Abstract
Background
The objective of this study was to validate the novel integration of oscillometric (Vasotens®) technology into a BPLab® ambulatory blood pressure (BP) monitoring system to measure central BP, the aortic augmentation index, and pulse wave velocity (PWV) compared with the recommended and widely accepted tonometric method.
Methods
The ARTERY Society guidelines for comparison of PWV measurement techniques were used as the basis for recruitment of 99 individuals (mean age 44±19 years, 52 males). The standard for comparison was the conventional “classic” SphygmoCor device.
Results
Accordance of the two methods was satisfactory (r=0.98, mean difference of 2.9±3.5 mmHg for central systolic BP; r=0.98, mean difference of −1.1±2.3 mmHg for central diastolic BP; r=0.83, mean difference of −2.6%±13% for aortic augmentation index; r=0.85, mean difference of 0.69±1.4 for PWV).
Conclusion
The performance of Vasotens algorithms using an oscillometric ambulatory BP monitoring system is feasible for accurate diagnosis, risk assessment, and evaluation of the effects of antihypertensive drugs.
Introduction
The past decade has been characterized by increases in the prognostic value of ambulatory blood pressure monitoring (ABPM) and the role of ABPM in the diagnosis and management of hypertension. ABPM shows several advantages over conventional non-time-specific single blood pressure (BP) measurements, especially in routine clinical practice, such as improved accuracy, reduced observer error, elimination of office-induced pressor effects on BP, and offering a more standardized measurement technique using an automated oscillometric sphygmomanometer.Citation1–Citation3 ABPM devices measure not only systolic BP and diastolic BP but also mean BP and pulse pressure. Recently, ABPM monitors measure or calculate other parameters that provide information about vascular wall properties have been developed. Several oscillometric ABPM systems, for example, the BPLab® with Vasotens® technology (OOO Petr Telegin, Nizhny Novgorod, Russia), use specific algorithms to perform pulse wave analyses based on 24-hour recordings of ABPM data and to calculate central BP.Citation4–Citation7
The central BP waveform is a composite of the forward pressure wave produced by left ventricular contraction and a reflected wave.Citation8 Thus, the BP in the ascending aorta represents the actual pressure imposed on the heart, the large arteries, the brain, and the kidneys. The effect of wave reflection on the aortic systolic pressure peak can be described as an augmentation and can be estimated using the augmentation index. In principle, the augmentation index can be measured by calculating the quotient of the pressure peaks of the initial and reflected waves.
The central and brachial BP values are different because of superimposition and divergence of incoming and reflected waves along the arterial tree. Calculation of central BP in patients with hypertension has received increasing interest because central and brachial BP values were compared with respect to their predictive value for cardiovascular events and their utility for evaluation of the differential effects of antihypertensive drugs.Citation1 Some studies have shown that the central BP and augmentation index are independent predictors of mortality in several populations.Citation9,Citation10 Central BP and augmentation index measurements are recommended for routine clinical use in cases of isolated systolic hypertension among the young. In some of these individuals, central BP may be normal, while systolic BP at the brachial level may be elevated due to strong amplification of the central pressure wave.Citation1,Citation11
It is well known that wave reflection and stiffening of the aorta are crucial factors that mediate the increases in isolated systolic hypertension and pulse pressure accompanying aging.Citation12 Aortic stiffening results in increased propagation velocity of the pressure wave along the arterial tree (ie, increased pulse wave velocity [PWV]), which is associated with arterial distensibility.Citation8 Thus, the PWV can be used as a measure of aortic stiffness.Citation13 The PWV is increasingly being used in population studies. It has been demonstrated that the PWV has greater predictive value than traditional risk factors, such as the SCORE (Systematic COronary Risk Evaluation) and Framingham risk scores.Citation14,Citation15 PWV measurements are recommended by the European Society of Hypertension for the management of hypertension. A substantial proportion of patients with classifications of intermediate risk may be reclassified into categories of higher or lower cardiovascular risk when the PWV, used as a measure of arterial stiffness, exceeds 10 meters per second.Citation1
In recent years, several methods, such as applanation tonometry and transfer functions, have been developed to estimate central BP and the augmentation index.Citation13 When used with sequential electrocardiography-gated carotid and femoral artery tonometry via the SphygmoCor device, (software version 9; AtCor Medical, Sydney, Australia), the PWV can be measured noninvasively in parallel with central BP and the augmentation index. Carotid-femoral PWV, as measured by applanation tonometry, is presently considered to be the gold standard for noninvasive assessment of arterial stiffness and for validation of noninvasive hemodynamic measurement devices, such as ABPM monitors that include additional features estimating vascular wall properties.Citation13 In 2010, the ARTERY Society published widely recognized guidelines for the design of high-quality studies validating noninvasive hemodynamic measurement devices.Citation16 Thus, the objective of our study was to validate the novel integration of oscillometric (Vasotens) technology into a BPLab ABPM system to measure central BP, the aortic augmentation index, and the PWV compared with the recommended and widely accepted tonometric method according to these guidelines.
Materials and methods
Recruitment of participants
We used the guidelines of the ARTERY Society for comparisons between PWV techniques as the basis for our study comparing the measurements of central BP and the augmentation index using different devices.Citation16 The individuals recruited for the study were equally distributed across three age ranges (ie, 18–30 years, 30–60 years, and older than 60 years). At least 25 individuals were included in each age range, and each range included a minimum of 40% men and 40% women. Participants were excluded if they were under the age of 18 years, were pacemaker-dependent, were not in sinus rhythm, were pregnant, had a body mass index higher than 30 kg/m2, had known carotid or femoral artery stenosis, or the pulse at the site of measurement was impalpable. The study was approved by the local ethics committee.
Measurements
To ensure hemodynamic stability, the measurements were performed in the supine position after the participants had been resting in this position for a minimum of 15 minutes. All subjects were familiarized with the environment, the procedure, and the devices. Central BP, augmentation index, and PWV measurements were recorded in triplicate using each device. These three recordings from each device were averaged to produce a single value for each individual from each device.
The standard for comparison of the PWV measurements was the measurement of carotid-femoral PWV using a conventional or “classic” SphygmoCor device (AtCor Medical), which allows for sequential recording of the pulses at the carotid and femoral sites via applanation tonometry. These two signals are gated using the QRS complex from a simultaneously recorded electrocardiogram. The BP value entered into the SphygmoCor device for calibration of the pulse waves was measured using a BPLab device; this device is known to display an accuracy of class A/A.Citation17 The augmentation index was then initially determined using SphygmoCor software by calculating the central BP by a transfer function.Citation18 Two investigators performed this protocol, and restricted themselves to the use of a single device for each subject but alternated the device they used between subjects. The investigators were blind to the results obtained from the alternate device. The order of measurements for two sequential subjects was as follows.
Subject 1
First measurement, SphygmoCor, observer A; second measurement, BPLab, observer B; third measurement, SphygmoCor, observer A; fourth measurement, BPLab, observer B; fifth measurement, SphygmoCor, observer A; and sixth measurement, BPLab, observer B.
Subject 2
First measurement, BPLab, observer A; second measurement, SphygmoCor, observer B; third measurement, BPLab, observer A; fourth measurement, SphygmoCor, observer B; fifth measurement, BPLab, observer A; sixth measurement, SphygmoCor, observer B.
Vasotens technology
Vasotens technology involves an innovative method of pulse wave analysis based on oscillometric blood pressure measurements from the BPLab ABPM system (OOO Petr Telegin Company). The principle of the oscillometric method is based on plethysmography, where changes in the pulsatile pressure in the brachial artery are recorded. The recordings are performed in the supine position using a conventional brachial BP cuff for adults. During BP measurement, the pressure waveforms in the cuff are recorded, digitalized, and stored in the device while performing step-by-step deflation.
Thereafter, an aortic pulse wave is generated using a generalized transfer function that utilizes a modification in a certain frequency range within the acquired pulse signal to derive the aortic pressure wave. The modulus and phase characteristics of the Vasotens transfer function have been published previously.Citation19 The difference in time between the first wave and the second wave (ie, the reflected wave) correlates to the distance, according to the manufacturer’s instructions, and the resulting PWV is expressed as meters per second. The principle of PWV measurement using Vasotens technology has also been described previously.Citation7,Citation20
Statistical analysis
The statistical analysis was performed using Microsoft Excel software (Redmond, WA, USA). All results are presented as the mean ± standard deviation (SD) unless otherwise stated. We used Pearson correlations and the Bland–Altman method for analyses.Citation21 The R coefficient was calculated for assessment of bias. The accuracy of the test device was determined based on both the mean difference from the reference and the standard deviation of this difference. For example, we considered the accuracy of the PWV measurements to be excellent when the mean difference was ≤0.5 meters per second and the SD was <0.8 meters per second; the accuracy was considered to be acceptable when the mean difference was <1.0 meters per second and the SD was ≤1.5 meters per second; and the accuracy was considered to be poor when the mean difference was >1.0 meters per second or the SD was >1.5 meters per second.Citation16 To assess the accuracy of the BP measurements, we used the mean difference and SD thresholds recommended in international protocols.Citation22–Citation24
Results
Parameters of the study population
Ninety-nine individuals (including 52 males) of mean age 44±19 (18–77) years were recruited. They were evenly distributed across the three designated age groups, and were balanced with respect to sex (). Thus, this necessary condition for validation of noninvasive hemodynamic measurement devices according to the guidelines of the ARTERY Society protocol was satisfied. also includes the results of the measurements and comparison measurements for the entire group of study participants and each of the three age groups of participants.
Table 1 Demographics and results of measurements compared for the entire group of study participants and each of the three age groups of study participants
Central BP
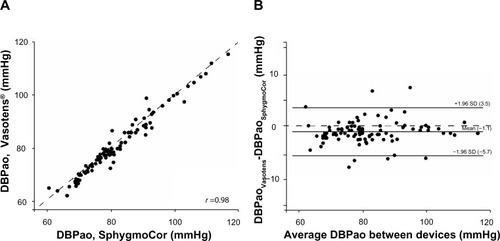
Across the study population, central systolic BP measured using the SphygmoCor device was 120±14 mmHg, and the central systolic BP calculated using the Vasotens device was 123±14 mmHg. The correlation between central SBP values measured using these two methods was significant (r=0.98, P<0.0001). The Bland–Altman plot of these data, as shown in , indicates excellent agreement (mean difference 2.9±3.5 mmHg) and no systematic bias. The central DBP values measured using the tonometer-based and one-cuff-based approaches were 68±11 mmHg and 67±11 mmHg, respectively. The correlation between these central DBP values was significant (r=0.98, P<0.0001). The Bland–Altman plot of these central diastolic BP data, as shown in , shows excellent agreement (mean difference of −1.1±2.3 mmHg) and no systematic bias.
Figure 1 Scatter plot containing the regression line (A) and Bland–Altman plot (B) comparing the SphygmoCor and Vasotens methods.
Abbreviations: SBPao, aortic systolic blood pressure; SD, standard deviation.
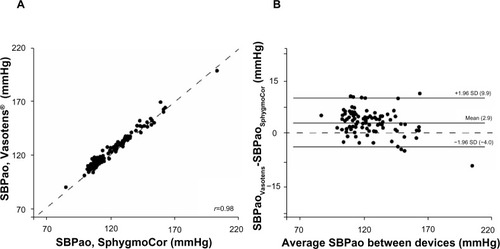
Figure 2 Scatter plot containing the regression line (A) and Bland–Altman plot (B) comparing the SphygmoCor and Vasotens methods.
Abbreviations: DBPao, aortic diastolic blood pressure; SD, standard deviation.
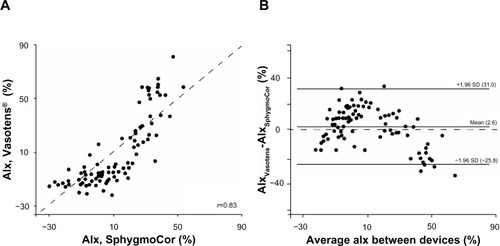
The mean aortic augmentation index values obtained using the SphygmoCor and Vasotens devices were 11%±11% and 13%±12%, respectively. The correlation between the aortic augmentation index values measured using these two methods was significant (r=0.83, P<0.001). The Bland–Altman plot of the aortic augmentation index values, as shown in , shows good agreement (mean difference −2.6%±13%) and no systematic bias.
Figure 3 Scatter plot containing the regression line (A) and Bland–Altman plot (B) comparing the SphygmoCor and Vasotens methods.
Abbreviations: AIx, augmentation index; SD, standard deviation.
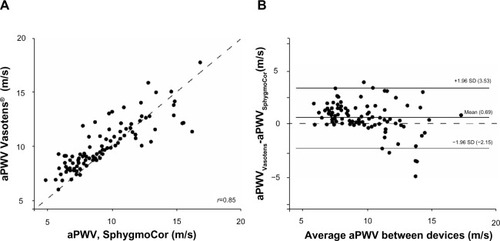
Pulse wave velocity
The mean aortic PWV measured by applanation tonometry was 7.03±1.88 meters per second and that using the one-cuff-based approach was 7.72±1.41 meters per second. The correlation between the PWV values measured using these two methods was significant (r=0.85, P<0.001). The Bland–Altman plot of these PWV data, as shown in , shows a mean difference of 0.69±1.4. According to the guidelines of the ARTERY Society, the accuracy of the Vasotens technology was “acceptable” (ie, the mean difference was less than 1.0±1.5 meters per second).
Figure 4 Scatter plot containing the regression line (A) and Bland–Altman plot (B) comparing the SphygmoCor and Vasotens methods.
Abbreviations: aPWV, aortic pulse wave velocity; SD, standard deviation.
Discussion
This study sought to validate a method of collecting additional “vascular” indices (ie, the central BP, the augmentation index, and the PWV) using the novel Vasotens technology and integration of these indices into the BPLab oscillometric ABPM system, which uses an original pulse wave analysis algorithm based on plethysmography. As recommended in the ARTERY Society guidelines, the tonometer-based assessment of these indices was chosen as the reference standard because this parameter has been used in the clinic setting and in large population studies.Citation16,Citation18,Citation25–Citation27 Thus, the equivalence of these data is a necessary requirement for oscillometric one-site-based measurements to be meaningful and useful for accurate diagnosis, risk assessment, and evaluation of the effects of antihypertensive drugs.
Other investigators have previously demonstrated that the brachial waveforms acquired using normal blood pressure cuffs can be used to calculate central BP.Citation28,Citation29 Our results also support the hypothesis that a generalized mathematical transfer function can be used to calculate central BP based on peripheral waveforms.Citation30 Our findings revealed levels of performance that are similar to those described in previous studies of oscillometric sphygmomanometers.Citation31 The mean difference and SD for central systolic BP were 2.9 and 3.5, respectively, which were far below the thresholds of ±5 (SD 8) mmHg for the mean difference and SD that are defining the highest levels of accuracy of conventional blood pressure measurements.Citation22–Citation24 The mean difference and SD for central diastolic BP were even lower.
The augmentation index values determined in our study were within the ranges that have been published for the SphygmoCor device, and the results of our comparisons of the aortic augmentation index measurements revealed sufficient accuracy.
The ability to obtain the data required to calculate PWV values using brachial waveforms acquired from a regular BP cuff has also been demonstrated previously.Citation4–Citation7 The accuracy of measurements produced using the Vasotens technology was “acceptable” according to the guidelines of the ARTERY Society, which were used as the basis of our study protocol.Citation16 Despite the wider range of PWV values compared with that reported in invasive and noninvasive validation studies, we obtained similar correlation coefficients, mean differences, and SDs.Citation4,Citation6,Citation7
For comparison of measurements between the different age groups, acceptable accuracy was detected for the entire group of study participants as well as for each of the three age groups.
There were limitations associated with this study. The aforementioned limits (±5 [SD 8] mmHg) recommended to define the levels of accuracy of BP measurements were designed to validate BP measurement devices for brachial BP but not for central BP. There is a need to develop formal recommendations to validate central BP measurements.
A further advantage of the Vasotens method that should be noted is its ability to collect 24-hour profiles of “vascular” indices. In fact, putative approaches to analyze 24-hour profile PWV data have already been proposed, and studies of the correlation between target organ damage in hypertension and the repeatability of the indices recorded using these approaches have been performed.Citation7,Citation32,Citation33
Conclusion
Our study revealed satisfactory accordance between the two methods. Thus, the performance of Vasotens algorithms using the oscillometric ABPM system represents a feasible approach to provide accurate diagnosis, risk assessment, and evaluation of the effects of antihypertensive drugs.
Disclosure
The authors have no conflicts of interest to report in this work.
References
- ManciaGFagardRNarkiewiczK2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC)Eur Heart J2013342159221923771844
- O’BrienEParatiGStergiouGon behalf of the European Society of Hypertension Working Group on Ambulatory Blood Pressure MonitoringEuropean Society of Hypertension position paper on ambulatory blood pressure monitoringJ Hypertens2013311731176824029863
- International Society for ChronobiologyAmerican Association of Medical Chronobiology and ChronotherapeuticsSpanish Society of Applied Chronobiology, Chronotherapy, and Vascular RiskSpanish Society of AtherosclerosisRomanian Society of Internal MedicineHermidaRCSmolenskyMHAyalaDE2013 ambulatory blood pressure monitoring recommendations for the diagnosis of adult hypertension, assessment of cardiovascular and other hypertension-associated risk, and attainment of therapeutic goalsChronobiol Int20133035541023517220
- BaulmannJSchillingsURickertSA new oscillometric method for assessment of arterial stiffness: comparison with tonometric and piezo-electronic methodsJ Hypertens20082652352818300864
- TrachetBReymondPKipsJNumerical validation of a new method to assess aortic pulse wave velocity from a single recording of a brachial artery waveform with an occluding cuffAnn Biomed Eng20103887688820127171
- HametnerBWassertheurerSKropfJMayerCEberBWeberTOscillometric estimation of aortic pulse wave velocity: comparison with intra-aortic catheter measurementsBlood Press Monit20131817317623571229
- PosokhovINPulse wave velocity 24-hour monitoring with one-site measurements by oscillometryMed Devices (Auckl)20136111523549868
- NicholsWO’RourkeMVlachopoulosCMcDonald’s Blood Flow in Arteries: Theoretical, Experimental and Clinical PrinciplesSixth EditionLondon, UKHodder Arnold2011
- SafarMEBlacherJPannierBCentral pulse pressure and mortality in end-stage renal diseaseHypertension20023973573811897754
- VlachopoulosCAznaouridisKO’RourkeMFSafarMEBaouKStefanadisCPrediction of cardiovascular events and all-cause mortality with central haemodynamics: a systematic review and meta-analysisEur Heart J2010311865187120197424
- O’RourkeMFAdjiAGuidelines on guidelines: focus on isolated systolic hypertension in youthJ Hypertens20133164965423412425
- SafarMELevyBIStruijker-BoudierHCurrent perspectives on arterial stiffness and pulse pressure in hypertension and cardiovascular diseasesCirculation20031072864286912796414
- LaurentSCockcroftJVan BortelLExpert consensus document on arterial stiffness: methodological issues and clinical applicationsEur Heart J2006272588260517000623
- SehestedtTJeppesenJHansenTWThresholds for pulse wave velocity, urine albumin creatinine ratio and left ventricular mass index using SCORE, Framingham and ESH/ESC risk chartsJ Hypertens2012301928193622871892
- BoutouyriePTropeanoAIAsmarRAortic stiffness is an independent predictor of primary coronary events in hypertensive patients: a longitudinal studyHypertension200239101511799071
- WilkinsonIBMcEnieryCMSchillaciGARTERY Society guidelines for validation of non-invasive haemodynamic measurement devices: Part 1, arterial pulse wave velocityArtery Res201043440
- KoudryavtcevSALazarevVMValidation of the BPLab® 24-hour blood pressure monitoring system according to the European standard BS EN 1060-4:2004 and British Hypertension Society protocolMed Devices (Auckl)2011419319622915946
- PaucaALO’RourkeMFKonNDProspective evaluation of a method for estimating ascending aortic pressure from the radial artery pressure waveformHypertension20013893293711641312
- RogozaANKuznetsovAACentral aortic blood pressure and augmentation index: comparison between Vasotens® and SphygmoCor® technologyResearch Reports in Clinical Cardiology201232733
- AgeenkovaOAPuryginaMACentral aortic blood pressure, augmentation index, and reflected wave transit time: reproducibility and repeatability of data obtained by oscillometryVasc Health Risk Manag2011764965622140314
- BlandJMAltmanDGStatistical methods for assessing agreement between two methods of clinical measurementLancet198613073102868172
- WhiteWBBersonASRobbinsCNational standard for measurement of resting and ambulatory blood pressures with automated sphygmomanometersHypertension1993215045098458649
- O’BrienEPetrieJLittlerWThe British Hypertension Society protocol for the evaluation of blood pressure measuring devicesJ Hypertens199311Suppl 2S43S62
- O’BrienEPickeringTAsmarRWorking Group on Blood Pressure Monitoring of the European Society of Hypertension: International Protocol for validation of blood pressure measuring devices in adultsBlood Press Monit2002731712040236
- Ben-ShlomoYSpearsMBoustredCAortic pulse wave velocity improves cardiovascular event prediction: an individual participant meta-analysis of prospective observational data from 17,635 subjectsJ Am Coll Cardiol225201463763664624239664
- McEnieryCMYasmin HallIRQasemAWilkinsonIBCockcroftJRNormal vascular aging: differential effects on wave reflection and aortic pulse wave velocity: the Anglo-Cardiff Collaborative Trial (ACCT)J Am Coll Cardiol2005461753176016256881
- MitchellGFHwangSJVasanRSArterial stiffness and cardiovascular events: the Framingham Heart StudyCirculation201012150551120083680
- ChengHMWangKLChenYHEstimation of central systolic blood pressure using an oscillometric blood pressure monitorHypertens Res20103359259920339373
- LiangFNumerical validation of a suprasystolic brachial cuff-based method for estimating aortic pressureBiomed Mater Eng2014241053106224211996
- WesterhofBEGuelenIStokWJIndividualization of transfer function in estimation of central aortic pressure from the peripheral pulse is not required in patients at restJ Appl Physiol20081051858186318845775
- WeberTWassertheurerSRammerMValidation of a brachial cuff-based method for estimating central systolic blood pressureHypertension20115882583221911710
- PosokhovINKulikovaNNStarchenkovaIVThe ‘pulse time index of norm’ highly correlates with the left ventricular mass index in patients with arterial hypertensionVasc Health Risk Manag20141013914424672245
- PosokhovINKonradiAOShlyakhtoEVMamontovOVOrlovAVRogozaANDay-to-day repeatability of the ‘pulse time index of norm’Med Devices (Auckl)20147293324600253
