Abstract
Coronary stents represent a key development for the treatment of obstructive coronary artery disease since the introduction of percutaneous coronary intervention. While drug-eluting stents gained wide acceptance in contemporary percutaneous coronary intervention practice, further developments in bare-metal stents remain crucial for patients who are not candidates for drug-eluting stents, or to improve metallic platforms for drug elution. Initially, stent platforms used biologically inert stainless steel, restricting stent performance due to limitations in flexibility and strut thickness. Later, cobalt chromium stent alloys outperformed steel as the material of choice for stents, allowing latest generation stents to be designed with significantly thinner struts, while maintaining corrosion resistance and radial strength. Most recently, the introduction of the platinum chromium alloy refined stent architecture with thin struts, high radial strength, conformability, and improved radiopacity. This review will provide an overview of the novel platinum chromium bare-metal stent platforms available for coronary intervention. Mechanical properties, clinical utility, and device limitations will be summarized and put into perspective.
Introduction
Coronary artery disease (CAD) is the leading cause of death in the world and is responsible for 7.4 million deaths in 2012.Citation1 Major advances in treatment and technology have led to a reduction in age-related cardiovascular deaths over the past 25–30 years.Citation2 Paradoxically, however, the prevalence of CAD is expected to further increase as a result of the continuously growing epidemic of obesity and its consequences, including hypertension, dyslipidemia, and diabetes.Citation2
The introduction of percutaneous coronary catheter interventions has revolutionized the field of coronary revascularization, and key developments in percutaneous coronary intervention (PCI) have significantly contributed to improve outcomes in patients with CAD: coronary bare-metal stents (BMSs) provided an answer to acute vessel closure, caused by dissection or elastic recoil after balloon angioplasty.Citation3 While BMS prevented late lumen narrowing owing to vascular remodeling, they simultaneously triggered neointimal proliferation, ultimately leading to in-stent restenosis.Citation3 Drug-eluting stents (DESs) virtually eliminated restenosis, providing controlled antiproliferative drug release from BMS carriers.Citation4 While the latest revolution in interventional cardiology introduced fully resorbable scaffolds with a promise of vessel restoration, lumen enlargement, and regained vasomotion,Citation5 versatile engineering of permanent metallic implants represents a unique opportunity to improve stent delivery, conformability and radial strength, both for BMS and DES.
Position of bare-metal coronary stents in current interventional practice
BMSs are currently used in 15%–20% of coronary stent implantations,Citation6 despite being significantly less effective than DES at inhibiting neointimal proliferation in response to strut-associated vascular injury and inflammation.Citation7 Continued interest in BMS and further developments in the field have three clear explanations.
First, the initial enthusiasm of neointimal growth control with DES was tempered by reports of incomplete endothelialization and late-stent thrombosis.Citation8 Animal studies demonstrated incomplete healing with DES at 180 days, whereas BMS uniformly showed complete endothelialization at 28 days.Citation9 Despite a somewhat longer endothelialization process in humans,Citation10 BMSs in stable CAD require therefore short duration (1 month) dual antiplatelet treatment (DAPT), while guidelines continue recommending prolonged (>6 months) DAPT with DES, even with latest-generation products.Citation11 Consequently, concerns about compliance to prolonged DAPT and bleeding risk, especially in an aging population, represent the primary reason to use BMS in a subgroup of patients with CAD.Citation12 Similarly, planned non-cardiac surgery within 12 months, need for anticoagulation, and finally cost may also play a role in the choice of BMS over DES.Citation12,Citation13
Second, the benefit of DES in reducing neointimal hyperplasia and restenosis seems to be most pronounced in patients with diffuse CAD, small vessels, and diabetics, whereas restenosis rates with BMS in nondiabetic patients with large vessels (≥3 mm) and discrete short stenoses (≤15 mm) are similar to DES.Citation13–Citation15 Moreover, the benefit of DES seems to be mostly limited to the prevention of restenosis and reintervention, while patients treated with BMS or DES have similar rates of death and acute myocardial infarction (MI).Citation16
Finally, latest generation (bare)-metallic stents are a formal part of contemporary DES technology. Indeed, in addition to developments in antiproliferative drug and polymer coating for DES, key improvements in design and metal alloy composition of the BMS platform have been shown to affect acute stent performance and clinical outcome.Citation17–Citation19
Platinum chromium bare-metal stents
Acute clinical performance of BMS is determined by a complex interplay of metal alloy and stent design. In an ideal setting, a coronary stent should be highly deliverable, owing to a thin strut and low-profile flexible design, while providing appropriate radial strength, near-absent recoil, and high radiopacity.Citation17
The platinum chromium alloy
Stainless steel (SS) (316L) was for many years the preferred alloy for coronary stents, combining excellent biocompatibility with adequate mechanical behavior, but suboptimal corrosion resistance.Citation20–Citation22 Further reduction of SS strut thickness to 130–140 µm occurred at the expense of stent visibility, while improving stent trackability, flexibility, and deliverability. These design changes did not affect stent recoil and radial strength, and ultimately lead to reduced restenosis rates.Citation20 Loss of stent visibility was initially compensated by the introduction of gold coatings and highly radiopaque gold markers on SS stents. However, overall poor clinical performance and higher incidence of in-stent restenosis with these coatings, together with the relatively moderate yield strength of 316L SS, created the need for superior strength metal alloys.Citation18,Citation23,Citation24
The introduction of a significant amount of cobalt and chromium in stent alloys (CoCr) allowed to significantly reduce strut thickness (80–90 µm), while simultaneously modestly improving radiopacity (eg, density of 8.0 g/cm3 for 316L SS vs 9.1 g/cm3 for the CoCr L605 Vision stent [Abbott Vascular, Santa Clara, CA, USA] and 8.4 g/cm3 MP35N Driver stent [Medtronic, Minneapolis, MN, USA]). Reduced strut thickness with CoCr equally favorably affected elastic characteristics (flexibility/deliverability/conformability) of stents, however, at the expense of more pronounced acute recoil as compared with 316L SS alternatives.Citation18,Citation23
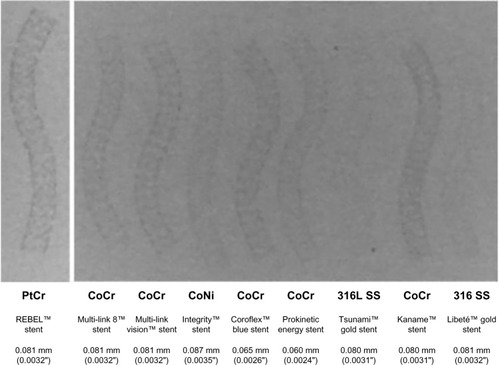
Different from cobalt, platinum (Pt) represents an attractive metal compound for stent alloys, owing to its superior strength, corrosion resistance, chemical stability, and biocompatibility. In combination with Cr, Pt-containing stent alloys were specifically created and tested for coronary applications.Citation18 Of the different alloy compositions tested, those using a fraction of 33% Pt seemed to offer the best equilibrium between processability, strength, stability, and radiopacity.Citation17 The improved strength of PtCr (480 MPa) compared to SS (275 MPa) allowed a further reduction in strut thickness compromising neither radial strength, mechanical properties, nor radiopacity (Pt density of 9.9 g/cm3) ().Citation17 Available PtCr stent platforms consist of Pt (33%), Cr (18%), iron (37%), nickel (9%), molybdenum (3%), and a trace of manganese, thereby reducing iron and nickel content when compared to 316L SS.Citation23 Details of stent processing have been described elsewhere.Citation17,Citation23,Citation25
Figure 1 Visibility bench test comparison of distinct stent alloys.
Abbreviations: PtCr, platinum chromium; CoCr, cobalt chromium; CoNi, colbalt nickel; SS, stainless steel.
Biovascular compatibility of the PtCr alloy has been extensively assessed in a nondiseased swine model: 30 days, 90 days, and 180 days after implantation of PtCr, 316L SS, and L605 CoCr BMS all three stent types showed indistinguishable histological findings and a similar clinical safety profile.Citation17
Clinical implications of stent alloy modifications
Thin-strut stents have been shown to improve stent crossing profile, contributing to superior trackability, a lower risk of occlusion of side branches, and related periprocedural MI.Citation17 Thinner stent struts equally favorably impact on in-stent restenosis and thrombosis, likely due to reduced vascular injuryCitation17,Citation19 and early and complete strut endothelialization.Citation26
High radiopacity inherently improves procedural precision and safety by enhancing immediate stent visibility, a feature that is particularly valuable during complex PCI. Clinical scenarios clearly benefiting from improved stent radiopacity are fluoroscopy in extreme caudal projections, in obese patients, or when differentiating severe calcifications from stent edges. Likewise, proper stent imaging is fundamental when precise stent positioning determines the completeness and degree of stent overlap in long lesions in order to avoid geographical miss or long double-layered stent segments, respectively. Inappropriate stent overlap may indeed lead to target vessel failures, likely related to uncovered areas or excessive local drug-delivery and inflammation. Finally, appropriate visualization of stent edges facilitates precise high pressure noncompliant balloon postdilatation avoiding unintentional balloon damage beyond stent margins.Citation17
Radial strength is a quantitative measure of stent scaffolding strength, and its resistance to extrinsic compression, maintaining vessel patency. This feature is of particular importance during PCI of aorto-ostial or highly fibrocalcific lesions.Citation17
Low recoil, the ability of a stent to maintain its initial expansion diameter, is known to be associated with reduced risk of malapposition and late-stent thrombosis and restenosis.Citation17
Finally, conformability is defined as the ability of a stent to adapt and support a tortous vascular anatomy without inducing vessel straightening. It may be one of the main predictors to avoid stent-induced injury and stent-edge dissections in complex vessel anatomies. Stent rigidity, the opposite of conformability, restricts the adaptive capability of stents in tortuous anatomies, potentially inducing a hinge effect and putting the patient at increased risk for restenosis.Citation23
Available platinum chromium stent designs
The Element stent concept for DES and BMS
Coronary stents using the improved mechanical properties and radiopacity of the Pt-enhanced alloy were initially launched as the revolutionary Element (Boston Scientific, Natik, MA, USA) BMS platform for everolimus or paclitaxel elution (Promus Element and Taxus Element series, respectively).
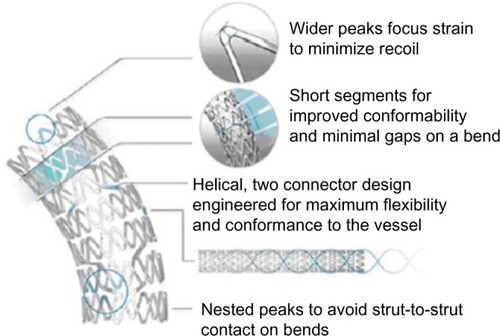
The Element portfolio includes stent models with lengths and diameters ranging from 8 mm to 38 mm and from 2.25 mm to 4.0 mm, respectively. Strut thickness of 81 µm, and a unique design of interconnected serpentine segments contribute to an excellent flexibility, deliverability, and conformability.Citation25 Improved stent behavior is further enhanced by a limited number of connectors (n=2) between segments, while connectors arranged in a kind of double helix configuration facilitate independent stent segment motion, while balancing forces in the stent (). A particular design feature of the Element platform is the nested orientation of stent segment peaks, hereby avoiding strut-to-strut contact during stent tracking in tortuous anatomies, or during deployment in a bend. Finally, wider segment peaks and shorter segment lengths redistribute expansion strain in the longitudinal direction, hereby increasing radial strength, while simultaneously improving conformability.Citation23,Citation25
Figure 2 Design structure of the element PtCr stent platform.
Abbreviation: PtCr, platinum and chromium.
In contrast with most other latest generation stents, often available in two models mounted on a wider range of balloon sizes, the Element stent platform was developed in four sizes to accommodate for an optimal surface-to-artery ratio ().Citation23,Citation25 Such tailored design reduces the risk of plaque prolapse, by allowing more uniform scaffolding and contact with the vessel wall, hereby insuring a uniform drug release. The smaller 2.25 mm model stent has even a more individualized design with shorter (and thus more) segments per stent as compared with the larger diameter models as well as a lower system profile, optimizing the conformability and deliverability in small and often more tortuous vessels.Citation23
Figure 3 PtCr stent models according to vessel size.
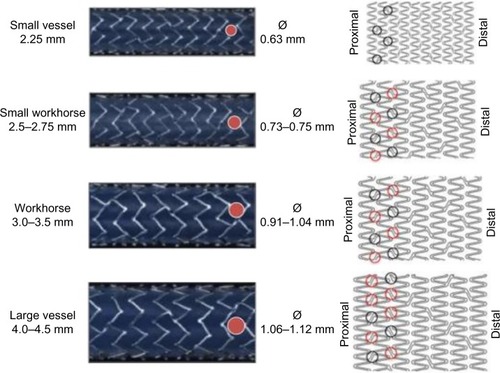
Finally, stent performance in Element was optimized by implementation of a tailored stent delivery system, similar to the Apex balloon catheter (Boston Scientific), using a bisegment inner lumen technology to offer maximal distal shaft and balloon flexibility as well as proximal shaft pushability.Citation23,Citation25
The Element platform was consequently released as the Omega BMS (Boston Scientific), with identical mechanical properties without drug elution. These stent characteristics have been shown to translate into superior performance as compared with competitive BMS designs both in terms of conformability and recoil.Citation23 The Omega portfolio offers BMS ranging in diameter from 2.25 mm to 4.50 mm and lengths of 8 mm to 32 mm.
Further refinements: Promus Premier and Rebel
The last generation PtCr platform for the Rebel BMS (Boston Scientific) and Promus Premier DES (Boston Scientific) is based on the Omega/Element stent. It introduces additional connectors within the proximal end of the stent to increase axial strength and resistance to stent deformation. Moreover, it uses an improved delivery system for increased resistance to compression while maintaining flexibility and deliverability.Citation27 The customized stent architecture consists of two additional connectors between the first and second and between the second and third proximal segment for the 2.50–3.5 mm platforms for Rebel and Premier and three additional connectors for the 4.00–4.50 mm versions, enhancing in this way the axial strength (). The length of each segment has been shortened at the expense of an increasing number of stent segments, to improve conformability, and to minimize gaps on a bend. The segment peaks were also widened to focus radial strength and minimize stent recoil.
Improvements in the mechanical characteristics of the stent delivery system for the Rebel BMS intend to reduce frictional force and enable precise stent delivery in challenging lesions. The catheter shaft uses a ZGlide coating, identical to the one used in the Emerge balloon (Boston Scientific). This hydrophilic coating is applied on the catheter between the wire port and the proximal balloon and increases lubricity as compared with the bioslide coating (Boston Scientific) on the Omega stent. The inner lumen catheter has a bisegment customized design, with a pushable proximal segment and a flexible distal segment. The proximal hypotube is polytetrafluoroethylene coated for improved stent deliverability. Finally, the stent platform is mounted on a dual-layer pebax balloon (Boston Scientific), providing an optimal compliance with minimal balloon growth, in order to avoid stent overexpansion while maintaining appropriate stent apposition.
Efficacy studies with platinum chromium stents
Efficacy of the PtCr stent platform has been extensively tested for the everolimus-eluting version in randomized comparisons to CoCr stents eluting everolimus (PLATINUM)Citation28 or zotarolimus (HOST-ASSURE),Citation29 but detailed analysis of these results is beyond the scope of this review. For the PtCr BMS, the OMEGA Clinical Trial evaluated the safety and efficacy of the Omega stent in a prospective, single-arm fashion, comparing results to a prespecified performance goal.Citation27 A total of 328 patients with de novo CAD in vessels of 2.5–4.5 mm in diameter were enrolled. The primary endpoint at 9 months was a composite of target lesion failure defined as any ischemia-driven target lesion revascularization (TLR), MI related to the target vessel or cardiac death. The Omega stent was superior to a prespecified performance goal based on prior generation BMS (target lesion failure 11.5% vs 21.2%, P<0.0001). Cardiac death at 9 months occurred in 1.2% of patients, MI in 3.7%, TLR in 7.4% and definite or probable stent thrombosis was as low as 0.6%. While clinical restenosis leading to TLR was 7.4% at 9 months with Omega, angiographic binary restenosis (diameter stenosis >50%) was reported in 8.6% at 9 months and 9.9% at 1 year, thus at the lower end of the restenosis ranges commonly reported with BMS (5%–35%).Citation27 These rates are in line with those observed in the Driver registry (Driver stent restenosis 8.1% at 9 months),Citation30 DaVinci Registry (Multilink Vision 9.7% at 9 months),Citation31 and the bare metal arm of the Endeavor II randomized trial (Driver stent 14.1% at 12 months).Citation32 In these trials, patients receiving a Driver stent had a larger vessel diameter and a shorter lesion length. In contrast, patients treated with Omega had the most complex lesion subset, with an average vessel diameter of 2.77 mm and lesion length of 12.49 mm.
Safety and tolerability of platinum chromium bare-metal stents
The biocompatibility of the Pt alloy has been assessed in accordance with the usual battery of ISO 10993–1 tests and in a variety of porcine implant studies, as previously mentioned. However, from a vascular biomaterials perspective, endothelialization studies provide a better insight into cellular response to the surface characteristics. The importance of surface endothelialization has been well demonstrated for coronary stents, with poor endothelialization being associated with increased risk of thrombus formation and increased proliferation of smooth muscle cells.Citation10 Endothelial cell assays showed comparable results for PtCr to 316L-SS, one of the best materials in terms of supporting endothelial cell growth and migration. While this cell assay is of relatively short duration (14 days) it does address the most critical stage after implantation, when rapid endothelial cell coverage is desired.Citation18 In addition, the presence of Pt would not be expected to impair endothelialization, as histological investigations on Pt embolism coils have shown endothelialization as early as 2 weeks after aneurysm treatment.Citation33
The surface thrombogenicity and vascular healing process induced by the bare Element PtCr stent were also compared to the durable second-generation polymer coating polyvinylidene fluoride-co-hexafluoropropene used in the XienceV (Abbott Vascular) and Promus (Boston Scientific) everolimus-eluting stents. PtCr surfaces in contact with blood seem to be more biocompatible compared with polyvinylidene fluoride-co-hexafluoropropene-coated surfaces, since the latter tend to induce more thrombus, and subsequently, more neointima as well as a more delayed endothelialization.Citation34 This last finding is equally supported by autopsy studies, suggesting that the permanent presence of these polymers may elicit chronic arterial inflammation, resulting in delayed healing and late thrombotic events.Citation35,Citation36 However, large comparative studies with DES with durable vs bioresorbable polymers failed to convincingly show a clinical benefit for DES with bioresorbable coatings.Citation37,Citation38
Finally, low rates of definitive stent thrombosis were reported with the PtCr Omega stent in the SCAAR registry, including 174,703 BMS and DES implanted since 2007 to October 2013 ().Citation39
Figure 4 SCAAR stent thrombosis rates with various bare-metal stents.
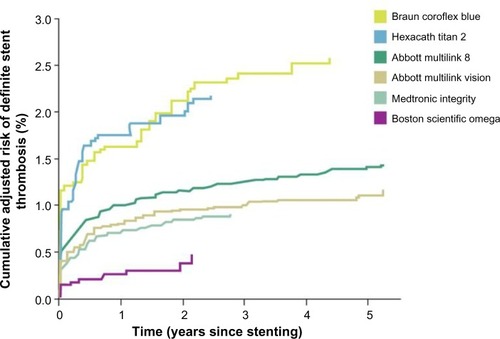
Besides biovascular compatibility, the improved radiopacity/visibility of the PtCr platform may have led to improved procedural technical outcome at the lesion level, hence reducing the risk for stent thrombosis.Citation40
Longitudinal stent deformation
Longitudinal stent deformation (LSD) has been recently recognized as a complication of coronary stent deployment, resulting from the elongation, shortening, or distortion of a stent in the longitudinal axis as a consequence of inadvertent device manipulation, and resulting in the need for additional measures, including repeat dilatation of the stent, deployment of another stent, and/or surgical intervention.Citation41–Citation43 This complication is expected to be rare, with an incidence estimated at 0.1%–1%, although the first dedicated study identified LSD in 1.3% of the procedures.Citation41,Citation44 Mechanisms contributing to this complication are not completely clear. In almost all cases reporting LSD, a direct force was applied at the level of the proximal stent segment, by compression by the guide catheter or guide extension, or when attempting to cross the freshly implanted stent with a secondary device (intravascular ultrasound catheters, additional undeployed stent, distal protection device and postdilatation balloon).Citation44,Citation45 Immediate outcome was usually uneventful, but correction of LSD often required considerable time and effort due to difficult crossing, while failure to reexpand the deformed stent may put the patient at risk for stent thrombosis.Citation44
Significant differences in longitudinal strength between available stent platforms have been identified in recent engineering analyses as potential contributors to LSD.Citation46,Citation47 While LSD has been reported with at least eight stent designs, it appears to occur more frequently with the PtCr Element stent platform. A retrospective review of the FDA MAUDE database for device malfunctions reported LSD with the Element platform in 2010–2011 in 45 of the 57 (79%) cases with stent deformation.Citation43 Moreover, a recent retrospective and observational study of 450 consecutive procedures suggested that LSD is specific to the platform used (3.1% with the Promus Element stent vs <1% with the Biomatrix [Biosensors Europe, Morges, Switzerland), Resolute Integrity (Medtronic, Minneapolis, MN, USA] and XienceV [Abbott Vascular, Santa Clara, CA, USA] platforms).Citation44 In contrast, a systematic independent analysis, specifically directed toward LSD in 2403 stents implanted in the PERSEUS and PLATINUM trials, did not identify cases with severe stent distortion among three different stent platforms with variable design, alloy composition (CoCr, PtCr, and 316L SS), and strut thickness (81–132 µm). However, only 21% of all lesions treated in these trials were classified as ACC/AHA type C.Citation48 Occurrence of LSD may, therefore, have been underestimated in this analysis, since lesions typically favoring stent distortion, such as chronic total occlusions, heavily calcified and tortuous vessels, and ostial lesions were excluded in these trials.Citation45,Citation48 Finally, in the most recent PE-prove trial, the occurrence of two cases of LSD out of 1,679 PtCr stents implanted in this study, highlights the low frequency of this procedural complication. These two cases, which were detected by angiography during the index procedure, represent classic examples of stent deformation resulting from interaction between an ancillary device and a stent that were easily treated without severe adverse consequences.Citation49
The intentional improvement of stent radiopacity with the PtCr alloy used in Element ensures optimal stent visualization and parallely early detection of LSD.Citation41 While the alloy composition on itself has been shown to provide superior tensile strength and density as compared with other alloys, the mechanical susceptibility to LSD with Element is primarily related to an off-set peak-to-peak design and a limited (n=2) number of connectors between different stent rings.Citation17,Citation45 This limitation has recently been addressed by inclusion of additional end connectors in the latest generation Rebel bare metal and in the everolimus-eluting Promus Premier and derived Synergy (Boston Scientific) stents, in order to optimize longitudinal robustness (). A recent report confirmed an increased longitudinal strength of the Promus Premier stent in bench testing.Citation50
Finally, awareness for the potential occurrence of LSD, irrespective of the stent platform used, should incite operators to implement a preventive behavior toward this entity. Indeed, optimal target lesion preparation and stent expansion, minimizing stent contact with guide catheter or guide catheter extension, and use of finesse rather than force when recrossing a freshly deployed stent, have been shown to minimize the risk of LSD.Citation25
Conclusion
Thin-strut PtCr coronary stent platforms combine improved acute mechanical performance in terms of flexibility, deliverability, conformability, radial strength, and visibility, with favorable long-term clinical results in both BMS and DES versions. Recent alterations in stent design have successfully addressed concerns of longitudinal stent distortion by adding a limited number of stent segment connectors for increased proximal robustness. Improvements in stent design with PtCr stent series therefore illustrate the delicate balance between optimal stent concept and clinical failure. Growing evidence in a wide variety of clinical scenarios can truly position latest generation PtCr stent platforms for BMS and DES among best-in-class for contemporary PCI practice.
Disclosure
CD has received institutional grants from Abbott Vascular, Medtronic, Biosensors International, and Boston Scientific. CD is member of the Scientific Medical Advisory Board of Boston Scientific. The authors report no other conflicts of interest in this work.
References
- The World Health OrganizationThe Top Ten Causes of Death Fact Sheet 20122015 Available from: http:/www.who.int/mediacentre/factsheets/fs310/en/Accessed February 1, 2015
- FusterVMearnsBMThe CVD paradox: mortality vs prevalenceNat Rev Cardiol200961166919851344
- BautersCMeuriceTHamonMMcFaddenELablancheJMBertrandMEMechanisms and prevention of restenosis: from experimental models to clinical practiceCardiovasc Res19963168358468759238
- NabelEGBraunwaldEA tale of coronary artery diease and myocardial infarctionN Engl J Med20123661546322216842
- TamburinoCLatibAvan GeunsRJContemporary practice and technical aspects in coronary intervention with bioresorbable scaffold a European perspective.pdfEuroIntervention201510116
- AlfonsoFByrneRARiveroFKastratiACurrent treatment of in-stent restenosisJ Am Coll Cardiol201463242659267324632282
- MoliternoDJHealing achilles – sirolimus versus paclitaxelN Engl J Med2005353772472716105991
- McFaddenEPStabileERegarELate thrombosis in drug-eluting coronary stents after discontinuation of antiplatelet therapyLancet200436494441519152115500897
- TsimikasSDrug-eluting stents and late adverse clinical outcomes lessons learned, lessons awaitedJ Am Coll Cardiol200647102112211516697332
- GrewePHDenekeTMachraouiABarmeyerJMüllerKMAcute and chronic tissue response to coronary stent implantation: pathologic findings in human specimenJ Am Coll Cardiol200035115716310636274
- WindeckerSKolhPAlfonsoF2014 ESC/EACTS guidelines on myocardial revascularization: the task force on myocardial revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS)Eur Heart J201435372541261925173339
- MoriceMCUrbanPGreeneSSchulerGChevalierBWhy are we still using coronary bare-metal stents?J Am Coll Cardiol201361101122112323333139
- AminAPSpertusJACohenDJUse of drug-eluting stents as a function of predicted benefit: clinical and economic implications of current practiceArch Intern Med2012172151145115222777536
- PfistererMBrunner-La RoccaHPRickenbacherPBASKETLong-term benefit-risk balance of drug-eluting vs bare-metal stents in daily practice: does stent diameter matter? Three-year follow-up of BASKETEur Heart J2009301162419033260
- TuJVBowenJChiuMEffectiveness and safety of drug-eluting stents in OntarioN Engl J Med2007357141393140217914040
- GreenhalghJHockenhullJRaoNDundarYDicksonRCBagustADrug-eluting stents versus bare metal stents for angina or acute coronary syndromesCochrane Database Syst Rev20105CD00458720464732
- MenownIBNoadRGarciaEJMeredithIThe platinum chromium element stent platform: from alloy, to design, to clinical practiceAdv Ther201027312914120437213
- O’BrienBJStinsonJSLarsenSREppihimerMJCarrollWMA platinum-chromium steel for cardiovascular stentsBiomaterials201031143755376120181394
- TurcoMAThe integrity® bare-metal stent made by continuous sinusoid technologyExpert Rev Med Devices20118330330621542702
- KastratiAMehilliJDirschingerJIntracoronary stenting and angiographic results: strut thickness effect on restenosis outcome (ISAR-STEREO) trialCirculation2001103232816282111401938
- GotmanICharacteristics of metals used in implantsJ Endourol19971163833899440845
- MesserRLMickalonisJLewisJBInteractions between stainless steel, shear stress, and monocytesJ Biomed Mater Res A200887122923518092353
- AlloccoDJJacoskiMVHuibregtseBMickleyTDawkinsKDCoronary stents platinum chromium stent series – the TAXUS™ Element™ (ION™), PROMUS Element™ and OMEGA™ stentsIntervent Cardiol201162134141
- KastratiASchömigADirschingerJIncreased risk of restenosis after placement of gold-coated stents: results of a randomized trial comparing gold-coated with uncoated steel stents in patients with coronary artery diseaseCirculation2000101212478248310831521
- BennettJDuboisCA novel platinum chromium everolimus-eluting stent for the treatment of coronary artery diseaseBiologics20137114915923818756
- SoucyNVFeyginJMTunstallRStrut tissue coverage and endothelial cell coverage: a comparison between bare metal stent platforms and platinum chromium stents with and without everolimus-eluting coatingEuroIntervention20106563063721044918
- WangJCCarriéDMasottiMPrimary endpoint results of the OMEGA Study: one-year clinical outcomes after implantation of a novel platinum chromium bare metal stentCardiovasc Revasc Med2015162656925576273
- StoneGWTeirsteinPSMeredithITPLATINUM Trial InvestigatorsA prospective, randomized evaluation of a novel everolimus-eluting coronary stent: the PLATINUM (a prospective, randomized, multicenter trial to assess an everolimus-eluting coronary stent system [PROMUS Element] for the treatment of up to Two de Novo CorJ Am Coll Cardiol201157161700170821470815
- ParkKWKangS-HKangH-JA randomized comparison of platinum chromium-based everolimus-eluting stents versus cobalt chromium-based Zotarolimus-Eluting stents in all-comers receiving percutaneous coronary intervention: HOST-ASSURE (harmonizing optimal strategy for treatment of corJ Am Coll Cardiol201463252805281624814486
- SketchMHBallMRutherfordBPopmaJJRussellCKereiakesDJEvaluation of the medtronic (Driver) cobalt-chromium alloy coronary stent systemAm J Cardiol200595181215619386
- NefHMMöllmannHWeberMCobalt-chrome MULTI-LINK VISION-stent implantation in diabetics and complex lesions: results from the DaVinci-registryClin Res Cardiol2009981173173719697076
- FajadetJWijnsWLaarmanGJLong-term follow-up of the randomised controlled trial to evaluate the safety and efficacy of the zotarolimus-eluting driver coronary stent in de novo native coronary artery lesions: five year outcomes in the ENDEAVOR II studyEuroIntervention20106556256721044908
- IshiharaSMawadMEOgataKHistopathologic findings in human cerebral aneurysms embolized with platinum coils: report of two cases and review of the literatureAJNR Am J Neuroradiol200223697097412063226
- EppihimerMJSushkovaNGrimsbyJLImpact of stent surface on thrombogenicity and vascular healing: a comparative analysis of metallic and polymeric surfacesCirc Cardiovasc Interv20136437037723899869
- VirmaniRFarbAGuagliumiGKolodgieFDDrug-eluting stents: caution and concerns for long-term outcomeCoron Artery Dis200415631331815346088
- FinnAVNakazawaGJonerMVascular responses to drug eluting stents: importance of delayed healingArterioscler Thromb Vasc Biol20072771500151017510464
- SmitsPCHofmaSTogniMAbluminal biodegradable polymer biolimus-eluting stent versus durable polymer everolimus-eluting stent (COMPARE II): a randomised, controlled, non-inferiority trialLancet2013381986765166023374650
- NatsuakiMKozumaKMorimotoTNEXT InvestigatorsBiodegradable polymer biolimus-eluting stent versus durable polymer everolimus-eluting stent: a randomized, controlled, noninferiority trialJ Am Coll Cardiol201362318119023684673
- SCAARSwedish Coronary Angiography and Angioplasty Registry2015 Available from: http://www.ucr.uu.se/swedeheart/index.php/forskning-scaar/in-english/stent-reportsAccessed April 1, 2015
- TamburinoCCapodannoDErglisAOne-year outcomes in unselected patients treated with a thin-strut, platinum-chromium, paclitaxel-eluting stent: primary endpoint results from the TAXUS element European post-approval surveillance study (TE-PROVE)EuroIntervention201510111261126625572023
- WilliamsPDMamasMAFraserDGHow serious an adverse event is longitudinal stent deformation? Incidence and severityExpert Rev Med Devices20129544945123116069
- HanrattyCGWalshSJLongitudinal compression: a “new” complication with modern coronary stent platforms – time to think beyond deliverability?EuroIntervention20117787287721970984
- MamasMAWilliamsPDLongitudinal stent deformation: insights on mechanisms, treatments and outcomes from the Food and Drug Administration Manufacturer and User Facility Device Experience databaseEuroIntervention20128219620422381263
- ArnousSShakhshirNWiperAIncidence, and mechanisms of longitudinal stent deformation (LSD) associated with biomatrix, resolute, element and xience stents: angiographic and case-by-case review of 1,800 PCIsCatheter Cardiovasc Interv2014
- LeibundgutGGickMTomaALongitudinal compression of the platinum-chromium everolimus-eluting stent during coronary implantation: predisposing mechanical properties, incidence, and predictors in a large patient cohortCatheter Cardiovasc Interv2013815206214
- PrabhuSSchikorrTMahmoudTJacobsJPotgieterASimontonCEngineering assessment of the longitudinal compression behaviour of contemporary coronary stentsEuroIntervention20128227528122057097
- OrmistonJAWebberBWebsterMWIStent longitudinal integrity bench insights into a clinical problemJACC Cardiovasc Interv20114121310131722136972
- KereiakesDJPopmaJJCannonLALongitudinal stent deformation: quantitative coronary angiographic analysis from the PERSEUS and PLATINUM randomised controlled clinical trialsEuroIntervention20128218719522445912
- ThomasMRBirkemeyerRSchwimmbeckPOne-year outcomes in 1,010 unselected patients treated with the PROMUS element everolimus-eluting stent: the multicentre PROMUS element European Post-Approval Surveillance StudyEuroIntervention201510111267127125631367
- OrmistonJAWebberBUbodBWhiteJWebsterMWIStent longitudinal strength assessed using point compression: insights from a second-generation, clinically related bench testCirc Cardiovasc Interv201371626924368821
