Abstract
The treatment of osteoporotic long bone fractures is difficult due to diminished bone density and compromised biomechanical integrity. The majority of osteoporotic long bone fractures occur in the metaphyseal region, which poses additional problems for surgical repair due to increased intramedullary volume. Treatment with internal fixation using intramedullary nails or plating is associated with poor clinical outcomes in this patient population. Subsequent fractures and complications such as screw pull-out necessitate additional interventions, prolonging recovery and increasing health care costs. The Photodynamic Bone Stabilization System (PBSS) is a minimally invasive surgical technique that allows clinicians to repair bone fractures using a light-curable polymer contained within an inflatable balloon catheter, offering a new treatment option for osteoporotic long bone fractures. The unique polymer compound and catheter application provides a customizable solution for long bone fractures that produces internal stability while maintaining bone length, rotational alignment, and postsurgical mobility. The PBSS has been utilized in a case series of 41 fractures in 33 patients suffering osteoporotic long bone fractures. The initial results indicate that the use of the light-cured polymeric rod for this patient population provides excellent fixation and stability in compromised bone, with a superior complication profile. This paper describes the clinical uses, procedural details, indications for use, and the initial clinical findings of the PBSS.
Introduction
Long bone fractures are a common and serious consequence of osteoporosis. The economic and health care burden of osteoporotic fractures in the European Union is estimated at €37 billion annually, with patients suffering significant pain, disability, and reduction in quality of life.Citation1–Citation3 Although fracture prevention remains at the forefront of the fight against osteoporosis, an estimated 9 million fractures occur worldwide every year.Citation1,Citation2 The prevalence of long bone fractures (eg, radius, tibia, humerus) in osteoporosis rivals that of vertebral fractures,Citation3,Citation4 and their repair presents a variety of clinical challenges not faced in the repair of other osteoporotic fractures. Chief among these are the restoration of proper bone length, rotation, and alignment; the management of delicate surrounding soft tissue; and the maintenance of postfracture patient mobility.
Surgical repair of osteoporotic long bone fractures is difficult due to the general weakness of the osseous tissue.Citation5 Conventional fixation techniques such as external fixation, plating, and intramedullary nails are often associated with poor outcomes in osteoporotic patients, as the diminished bone density prevents adequate anchoring of screws and implants.Citation5–Citation7 Furthermore, the majority of osteoporotic long bone fractures occur in the metaphyseal region, further complicating surgical repair, as the intramedullary volume is at its greatest in this region. As a result, surgical techniques that may be suitable for diaphyseal fractures are not necessarily appropriate for use in metaphyseal fractures, as they cannot anchor suitably in the widened metaphyseal space.Citation5–Citation7
To address the difficulties associated with surgical repair of osteoporotic long bone fractures, several techniques have been developed. One common approach has been to improve the bond between bone and implant through the use of resorbable bone cements. Initial innovation using polymethylmethacrylate-based (PMMA) resin was replaced with calcium–phosphate cement paste, as PMMA was found to bond the bone and implant to such a degree that revision procedures were impossible.Citation8 Calcium–phosphate cements have been shown to limit screw pull-out and screw migration following surgery; however, these procedures necessitate prolonged periods of nonweight bearing and unloading of the injured limb, requirements that prove difficult for elderly patients.Citation8–Citation10
The Photodynamic Bone Stabilization System (PBSS) is a minimally invasive surgical technique that has been developed to address the challenges associated with surgical repair of osteoporotic fractures of long bones. This novel technology allows clinicians to repair long bone fractures using a light-curable polymer contained within an inflatable balloon catheter (IlluminOss® Photodynamic Bone Stabilization System, IlluminOss Medical, Inc., East Providence, RI, USA). This method offers percutaneous, customized, intramedullary stabilization of osteoporotic fractures in long bones that combines the stability of intramedullary nailing with the versatility of balloon kyphosis techniques used in vertebral fracture repair. However, unlike vertebral kyphosis, the IlluminOss system maintains the monomer within the confines of the balloon, eliminating the risk of extravasation. This novel system thus offers a stabilization strategy which can be customized to accommodate both diaphyseal and metaphyseal fractures through a minimally invasive procedure. The purpose of this paper is to describe the clinical uses, procedural details, and indications for use of the IlluminOss PBSS technology in simple and complex long bone fractures.
Materials and methods
Device description
The PBSS is a new, minimally invasive surgical technique that allows clinicians to repair bone fractures using a light-curable polymer contained within an inflatable balloon catheter (IlluminOss Medical, Inc.). This unique system utilizes a light-cured, on-demand polymerizing mechanism that, unlike rapidly hardening bone cement, allows the surgeon the freedom and time to attain proper reduction of the fracture before hardening the polymer. PBSS has been approved by the United States Food and Drug Administration for investigation device use in the United States and is currently being used clinically in a number of European countries, including Germany, Austria, Switzerland, Italy, Turkey and the Netherlands, in addition to Spain, and Israel.
Procedural details and indications for use
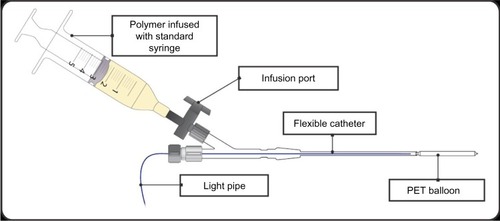
The PBSS is suitable for repair of long bone fractures in the diaphyseal and/or metaphyseal regions of the bone (). The device is introduced following reduction and stabilization of the fracture and consists of a balloon catheter and a light-cured polymer (). Following fracture reduction and stabilization, the customized intramedullary balloon is inserted through an 8 mm percutaneous incision and positioned in the intramedullary space, across the reduced fracture. The balloon is available in sizes ranging from 40 to 280 mm in length and 4 to 22 mm in diameter, with volume ranging from 5 to 51 mL. The implant is thus able to fully transit the fracture, providing longitudinal strength, and to ensure cortical wall contact for its entire length, providing rotational stability. Once the balloon is positioned appropriately in the intramedullary space, it is infused with the biocompatible photodynamic liquid monomer. After suitable alignment, rotational stability, and bone length have been established, the visible light curing system is introduced to quickly polymerize the liquid in the balloon to form a strong, hardened bone-stabilizing rod (). The light curing system comprises a fiber optic light pipe, an external light console, and a timer key, which collectively provide the surgeon with customized control over the curing process. The light pipe gains access to the balloon via an inner lumen, allowing for introduction and removal of the light source, which emits light along the length of the implant, curing the monomer internally (). Curing requires between 200 and 800 seconds, depending on polymer volume.
Figure 1 The PBSS utilized in a distal ulna fracture.
Abbreviation: PBSS, Photodynamic Bone Stabilization System.
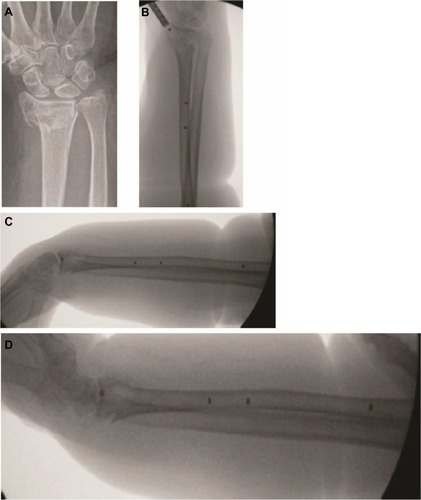
Figure 2 Schematic representation of the Photodynamic Bone Stabilization System.
Abbreviation: PET, polyethylene terephthalate.
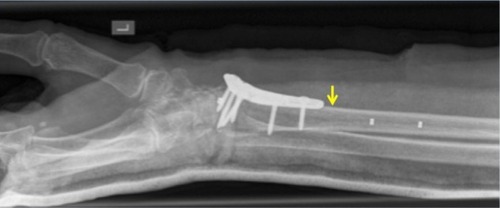
Osteosynthesis hardware can be used in conjunction with the PBSS, with screw size and placement limited only by proximity to the fracture line (). Hardware cannot be applied until the curing process is completed, but once hardened, the polymer provides an excellent substrate into which to insert screws. The PBSS does not interfere with osteosynthesis devices, and in some cases may serve to replace such implants. It is ideally suited to osteoporotic fractures, as it provides internal strength and stability to the weakened bone associated with osteoporosis.
Figure 3 The Photodynamic Bone Stabilization System implant in combination with standard compression plate hardware.
Abbreviations: PBSS, Photodynamic Bone Stabilization System; L, left.
Contraindications
The PBSS is contraindicated in patients where normal bone metabolism may be affected, including patients who are considered skeletally immature, patients with marked bone loss or resorption, patients with metabolic disorders which may impair bone formation, and patients with osteomalacia. It is also contraindicated in patients where infection is a concern, including those with an active or incompletely treated infection that could involve the implantation site and those with distant foci of infections which may spread to the implant site. Patients with an inappropriate fracture, such as open fractures with severe contamination or extremely comminuted fractures where insufficient holding power of the balloon on the intramedullary canal is probable are not suitable candidates for the PBSS. Patients with allergies to any of the implant materials or to dental glue are also contraindicated, as are uncooperative patients, those with a neurologic disorder, those incapable of following directions, and/or patients with vascular insufficiency, muscular atrophy, or neuromuscular disease. Finally, cases in which the delivery sheath is unable to cross the fracture site after proper fracture reduction and realignment and patients whose intramedullary canal at the site of the fracture measures smaller than the diameter of the sheath provided are also contraindicated.
Clinical outcomes
The PBSS implant has been evaluated in a representative group of patients and has shown excellent results in a variety of long bone fractures. From July 2012 to December 2013, 41 long bone fractures in 33 patients were treated using the PBSS. Patients were recruited from the orthopedic trauma ward at a major European hospital. The treatment group consisted of eight male and 25 female osteoporotic patients, with one female patient treated for two distal radius fractures at two separate time points. The patient ages ranged from 55 to 92 years; the majority were treated for an acute fracture (ie, less than 14 days from injury to assessment) or imminent fracture due to metastasis.
summarizes the distribution of fracture location. The majority of patients were treated for distal radius fractures, with or without concomitant ipsilateral distal ulnar fractures. The remaining patients were treated for fractures of the distal fibula, humerus, ulna alone, or femur. Two additional patients were treated for pseudoarthrosis.
Table 1 Summary of fracture characteristics
Results
Distal radius and ulna fractures
Twelve patients were treated for a distal radius and/or distal ulna fracture (AO Type 23-A2.1 to AO 23-A2.3). A total of 20 fractures were treated, 15 distal radius fractures and five ulnar fractures. One fracture from each group was categorized as an imminent fracture due to metastasis, with the remaining fractures a result of acute trauma (). All patients in this subgroup were treated with a polymeric rod alone, with no other osteosynthesis device added. Following surgery, patients were discharged with either a double bandage or a soft cast. No mobility restrictions were placed on these patients, and each patient took part in a standard postsurgical rehabilitation program.
Table 2 Distribution of fractures
No infections, secondary procedures, or delayed unions were reported from this group (). All demonstrated pain-free, satisfactory range of motion at follow-up, 3 months postsurgery.
Table 3 Summary of osteosynthesis device used and associated complications
Distal fibula
Eleven patients were treated for a unilateral distal fibular fracture (AO Type AO 44-A1-A3 and AO 44-A2-A3). With the exception of one fracture, all fractures were the result of acute trauma. Four patients were treated with the PBSS device alone; five patients were treated with a combination of the polymeric rod and stabilizing screws, and one patient was treated with a combination of the PBSS polymeric rod and a plate. The treatment provided was dependent upon the underlying density of the bone, with lower density bone requiring more comprehensive treatment.
Following the procedure, patients were discharged with removal of hardware at the medial malleolus and a soft cast. All reported full weight bearing within 2 weeks of discharge. One patient (age, 92 years) was discharged without a cast and suffered a subsequent screw pull-out and secondary dislocation of the ankle joint. This patient was subsequently treated with a soft cast for 6 weeks and was full weight bearing within 3 months. No other complications were reported in the distal fibula subgroup.
Humerus
Five patients were treated for unilateral humerus fracture (AO Type 12-A2-A3) under conditions of compassionate care, four of which were a result of acute trauma and one that was due to metastasis. The four acute fractures were treated with the polymeric rod with plate osteosynthesis, based on the fracture pattern and the density of bone. Three of these fractures were to the proximal humerus, with the fourth fracture located at the distal humerus. No infections or delayed unions were reported for this group of patients; one revision surgery was required. The fifth fracture in this group was due to metastasis. This fracture was treated with the PBSS polymeric rod alone with no reported complications.
Femur
Five patients with femoral fractures were treated with the PBSS device under conditions of compassionate use. One paraplegic patient, presenting with a distal femur pseudoarthrosis, had been referred for an above-knee amputation. This patient was treated with two polymeric rods and an angle stable plating system, which resulted in the full consolidation of the fracture and sparing of the limb. A second femur patient had been nonambulatory for several years due to extreme osteoporosis and soft tissue weakness. This patient’s fracture was treated with two intramedullary rods and angle stable plating. Due to the severity of osteoporosis, a new fracture of the femoral neck occurred intraoperatively. Following surgery, the angle stable plating fixed to the polymeric rods consolidated well; however, the cervical neck fracture not treated with the PBSS osteosynthesis failed.
Discussion
The treatment of osteoporotic long bone fractures is associated with significant challenges due to the inherent weakness of the osteoporotic bone and the limitations of standard fracture repair techniques in these patients. The minimally invasive PBSS is a novel technique for surgical repair of osteoporotic fractures in long bones that provides enhanced stability and excellent clinical results. Based on a preliminary case series, the PBSS device offers clinical efficacy comparable to current treatment options with a superior complication profile.
Inherent in the treatment of long bone fractures in osteoporotic patients is the difficulty in providing stability to the fracture site during the healing process, due to the bone fragility in these patients. Failure of internal fixation is common and is due largely to the structural weakness of the bone and not to failure of the device.Citation5,Citation10 Failure generally occurs due to either weakness in the cortical bone, which causes unsatisfactory anchoring of hardware, or the inability of current implants to adequately anchor in the expanded intramedullary space in the metaphyseal region.Citation11 Several techniques have been proposed to improve the bond between the device and the bone. These techniques, however, while increasing the stability of the implant–bone interface, fail to address the larger problem of internal bone weaknessCitation6,Citation8,Citation12,Citation13 and can limit the ability to revise the procedure when necessary.Citation8–Citation10,Citation13,Citation14
Current techniques for surgical fixation of osteoporotic long bone fractures are associated with two significant limitations: poor bonding of screws/hardware to the bone and poor anchoring of intramedullary nails due to enlarged intramedullary space. Methods to address the former have included increasing bond strength between screw and bone through the introduction of bone cements which are used to coat the screw and purport to increase the strength of the bone–screw interface.Citation8,Citation10,Citation12,Citation14–Citation16 Early versions of these bone cements provided extremely strong bonds; however, they hardened to such a degree as to limit the ability to perform revision surgery or safely remove stabilizing hardware.Citation8,Citation10,Citation15 Subsequent variations of bone cement have utilized bone substitutes such as calcium phosphate, which fuse with the injured bone, thus providing a strong bond while still allowing for revisions or hardware removal.Citation8,Citation9,Citation17,Citation18
Alternate strategies to improve the bone–hardware bond, such as pharmacologic augmentation and the use of compression plates in place of intramedullary rods, remain commonplace in orthopedics despite shortcomings. Pharmacologic augmentation utilizes the ability of compounds such as bisphosphonates or parathyroid hormone to influence the bone remodeling process, and while this approach has been associated with improved implant stability, there are concerns regarding potential adverse effects.Citation19 Local administration of bisphosphonates by coating the implant with a bisphosphonate–hydroxyapatite complex has been proposed to address this concern;Citation20–Citation22 however, this approach was found to be less effective than systemic administration in preclinical animal studies. Pharmacologic augmentation thus remains problematic.
Compression plates, historically proposed as a viable alternative to intramedullary nailing, provide superior fixation;Citation23 however, they have been associated with adverse effects such as decreased bone density under the plate due to stress shielding, thus compromising the structural integrity of the traumatized bone.Citation24,Citation25 Several studies have noted that local bone mineral density decreases significantly below the plate and can subsequently affect not only the bone-hardware interface but also the bone integrity itself.Citation26–Citation28 Use of PBSS in conjunction with compression plates limits these concerns; however, the superior stability provided by the PBSS system, due to its ability to completely fill the trabecular space, mitigates any weakness created as a result of plating or screws. Moreover, the mechanical properties of the hardened PBSS polymer mirror those of cancellous bone: the elastic modulus of the PBSS polymer is rated at 1.5 GPa, and thus falls within the range of cancellous bone (0.1–4.5 GPa).Citation29 Comparably, materials commonly used in orthopedic implants such as titanium alloy (115 GPa) and stainless steel (195 GPa) far exceed that of the cancellous bone cortical bone (15 GPa).Citation30 The PBSS polymer more closely matches the rigidity of cancellous bone, providing a more natural fit than other common materials, which dwarf the rigidity of either the cancellous or cortical bone and contribute to stress shielding.
While these innovations may have collectively improved implant–bone bonding, they fail to address the second challenge to adequate fracture healing: the expanded intramedullary space. Current intramedullary nails are unable to adequately fill this space, which necessitates additional screws and/or plates in an attempt to achieve satisfactory stability. In a recent systematic review of distal tibia fractures, Xue et alCitation7 found that intramedullary nails, while associated with good outcomes in functional ability and risk of infection, pain, complication rate, and time to union, were nonetheless shown to have a significantly higher malunion rate than did plating, which itself has been shown to be problematic, with a propensity towards complications and loss of reduction.Citation14,Citation31–Citation34 Thus, the current treatment options fail to adequately address the fundamental limitations of long bone surgical management in osteoporosis.Citation9,Citation10,Citation15
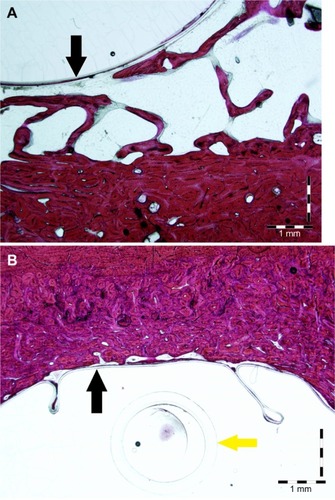
The PBSS system provides a viable alternative to current internal fixation options. The internal polymer system provides a customizable method for stabilizing metaphyseal fractures by filling the intramedullary space and providing additional stability to the cortical bone. Unique to this system, the balloon remains implanted in the medullar space, with the monomer contained within the confines of the balloon. This design provides stability and maintains alignment in a manner superior to other available methods. In in vivo testing, the implant has shown conformational filling of the medullary space with complete apposition to the cortical bone ().
Figure 4 Histologic images showing the Photodynamic Bone Stabilization System in situ.
The increased internal stability provided by the PBSS enhances the strength of adjunctive osteosynthesis devices such as screws or plates, and allows for better overall stability while eliminating many of the malunion issues associated with plates alone. PBSS provides an excellent combination of alignment and stability while decreasing the likelihood of revision surgery. Furthermore, it is associated with a much shorter and smaller thermal excursion than that of comparable systems such as PMMA (). As compared with the longer curing time and higher curing temperature of PMMA, the PBSS demonstrates superiority in ease of use and safety (). Patients with upper extremity fractures are discharged without the need for casting, which leads to faster improvements in mobility and decreased disability time, and patients with lower extremity fractures are able to bear weight faster and recover without the excessive restrictions placed on their mobility associated with conventional osteosynthesis devices.
Figure 5 A comparison of the thermal excursion and curing time of the PBSS monomer (blue) and PMMA (red).
Abbreviations: Illum, IlluminOss PBSS monomer; PMMA, polymethylmethacrylate.
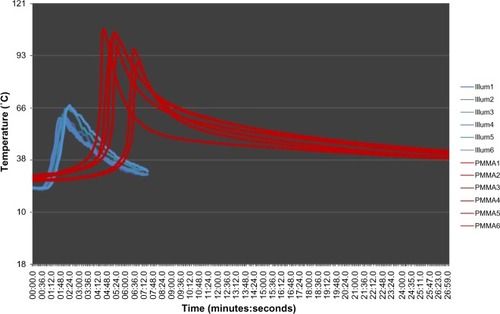
Table 4 Technical specifications regarding curing process in PBSS versus PMMA
Conclusion
The PBSS is a new, percutaneous, minimally invasive intramedullary rod that addresses some of the key challenges in treating osteoporotic fractures in the elderly. With the polymeric rod, extra-articular distal radius fractures can be treated without any postoperative cast, which is ideal for the elderly to achieve earlier self-supporting activities of daily living. Fibula bifocal fractures in the elderly can be treated with the polymeric rod system and 2 weeks in a soft cast that allows weight bearing from day 2 after surgery. In severe osteoporosis of the long bones, the IlluminOss polymeric rod system can be an augmentation for plate osteosynthesis. While further research is needed to evaluate the optimal use of this innovative technology, the early results are very promising.
Author contributions
JMM wrote the first manuscript draft. PV and JEB provided critical review and revision. All authors contributed toward conception and design, acquisition of data, or analysis and interpretation of data, read and approved the final manuscript, and agree to be accountable for all aspects of the work.
Disclosure
JMM and JEB received financial support from IlluminOss Medical, Inc. for assistance with manuscript development. The authors report no further conflicts of interest in this work.
References
- CostaAGWymanASirisESWhen, where and how osteoporosis-associated fractures occur: an analysis from the Global Longitudinal Study of Osteoporosis in Women (GLOW)PLoS One2013812e8330624349484
- JohnellOKanisJAAn estimate of the worldwide prevalence and disability associated with osteoporotic fracturesOsteoporos Int200617121726173316983459
- HernlundESvedbomAIvergårdMOsteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA)Arch Osteoporos201381–213624113837
- SvedbomAIvergårdMHernlundERizzoliRKanisJAEpidemiology and economic burden of osteoporosis in SwitzerlandArch Osteoporos2014918724970672
- LarssonSTreatment of osteoporotic fracturesScand J Surg200291214014612164513
- MarongiuGMastioMCaponeACurrent options to surgical treatment in osteoporotic fracturesAging Clin Exp Res201325Suppl 1S15S1724046046
- XueXHYanSGCaiXZShiMMLinTIntramedullary nailing versus plating for extra-articular distal tibial metaphyseal fracture: a systematic review and meta-analysisInjury201445466767624275358
- LarssonSCement augmentation in fracture treatmentScand J Surg200695211111816821654
- LarssonSBauerTWUse of injectable calcium phosphate cement for fracture fixation: a reviewClin Orthop Relat Res2002395233211937863
- LarssonSProcterPOptimising implant anchorage (augmentation) during fixation of osteoporotic fractures: is there a role for bone-graft substitutes?Injury201142Suppl 2S72S7621839441
- ThormannUEl KhawassnaTRaySDifferences of bone healing in metaphyseal defect fractures between osteoporotic and physiological bone in ratsInjury201445348749324332464
- MattssonPLarssonSStability of internally fixed femoral neck fractures augmented with resorbable cement. A prospective randomized study using radiostereometryScand J Surg200392321521914582545
- WähnertDLangeJHSchulzeMLenschowSStangeRRaschkeMJThe potential of implant augmentation in the treatment of osteoporotic distal femur fractures: a biomechanical studyInjury201344680881223000049
- AroraRLutzMHennerbichlerAKrappingerDEspenDGablMComplications following internal fixation of unstable distal radius fracture with a palmar locking-plateJ Orthop Trauma200721531632217485996
- GoetzenMNicolinoTHofmann-FliriLBlauthMWindolfMMetaphyseal screw augmentation of the LISS-PLT plate with polymethylmethacrylate improves angular stability in osteoporotic proximal third tibial fractures: a biomechanical study in human cadaveric tibiaeJ Orthop Trauma201428529429924296600
- WähnertDLangeJHSchulzeMGehweilerDKöstersCRaschkeMJA laboratory investigation to assess the influence of cement augmentation of screw and plate fixation in a simulation of distal femoral fracture of osteoporotic and non-osteoporotic boneBone Joint J201395-B101406140924078541
- LindnerTKanakarisNKMarxBCockbainAKontakisGGiannoudisPVFractures of the hip and osteoporosis: the role of bone substitutesJ Bone Joint Surg Br200991329430319258602
- MasalaSNanoGMarciaSMutoMFucciFPSimonettiGOsteoporotic vertebral compression fracture augmentation by injectable partly resorbable ceramic bone substitute (Cerament™|SPINESUPPORT): a prospective nonrandomized studyNeuroradiology201254111245125122391680
- RossRDHamiltonJLWilsonBMSumnerDRVirdiASPharmacologic augmentation of implant fixation in osteopenic boneCurr Osteoporos Rep2014121556424293098
- GaoYZouSLiuXBaoCHuJThe effect of surface immobilized bisphosphonates on the fixation of hydroxyapatitecoated titanium implants in ovariectomized ratsBiomaterials20093091790179619135249
- PeterBGauthierOLaïbSLocal delivery of bisphosphonate from coated orthopedic implants increases implants mechanical stability in osteoporotic ratsJ Biomed Mater Res A200676113314316254957
- StadelmannVAGauthierOTerrierABoulerJMPiolettiDPImplants delivering bisphosphonate locally increase periprosthetic bone density in an osteoporotic sheep model. A pilot studyEur Cell Mater200816101618671203
- RandJAAnKNChaoEYKellyPJA comparison of the effect of open intramedullary nailing and compression-plate fixation on fracture-site blood flow and fracture unionJ Bone Joint Surg Am19816334274427204443
- UhthoffHKPoitrasPBackmanDSInternal plate fixation of fractures: short history and recent developmentsJ Orthop Sci200611211812616568382
- PerrenSMEvolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biologyJ Bone Joint Surg Br20028481093111012463652
- UhthoffHKFinneganMThe effects of metal plates on post-traumatic remodelling and bone massJ Bone Joint Surg Br198365166716822605
- ZhuZADaiKRQiuSJRepair of regional osteoporosis after removal of rigid fixing plate. An experimental investigationChin Med J (Engl)199410753643677924578
- ClaesLKinzlLNeugebauerRExperimental studies on the influence of plate material on stress-relief and atrophy of the bone osteosynthesis plates (author’s transl)Biomed Tech (Berl)19812646671 German7236838
- GoldsteinSAThe mechanical properties of trabecular bone: dependence on anatomic location and functionJ Biomech19872011–12105510613323197
- The Engineering ToolboxModulus of elasticity – Young’s modulus for some common materials [webpage on the Internet] http://www.engineeringtoolbox.com/young-modulus-d_417.htmlAccessed October 7, 2014
- AroraRGablMGschwentnerMDemlCKrappingerDLutzMA comparative study of clinical and radiologic outcomes of unstable colles type distal radius fractures in patients older than 70 years: nonoperative treatment versus volar locking platingJ Orthop Trauma200923423724219318865
- AroraRLutzMFritzDZimmermannROberladstätterJGablMPalmar locking plate for treatment of unstable dorsal dislocated distal radius fracturesArch Orthop Trauma Surg2005125639940415891921
- FiglMWeningerPJurkowitschJHofbauerMSchauerJLeixneringMUnstable distal radius fractures in the elderly patient – volar fixed-angle plate osteosynthesis prevents secondary loss of reductionJ Trauma201068499299820065876
- FiglMWeningerPLiskaMHofbauerMLeixneringMVolar fixed-angle plate osteosynthesis of unstable distal radius fractures: 12 months resultsArch Orthop Trauma Surg2009129566166919225792
