Abstract
Value is a key guiding principle in healthcare, yet value is defined in varying ways by different stakeholders. In this paper, we review evidence of the health and financial tolls of malnutrition or poor nutrition, report positive results from recent nutrition-focused quality improvement programs in hospitals, and discuss clinical and policy implications of realizing best-practice nutrition care. Hospitalized patients with malnutrition diagnoses have up to two-fold greater hospital costs for care compared to inpatient stays for adequately nourished patients. By contrast, implementation of nutrition care programs for hospitalized adults (nutrition status screening, assessment and diagnosis of malnutrition, oral nutritional supplements provided when indicated) is associated with substantial per-patient, per-episode healthcare savings approaching $4,000. Improved nutrition care has also been associated with fewer complications and faster recovery (shortened lengths of stay, lower readmission rates). Nutrition care thus delivers value, which is evidenced by better patient outcomes at cost savings to healthcare systems.
What is the “Value” of Therapeutic Nutrition in Healthcare?
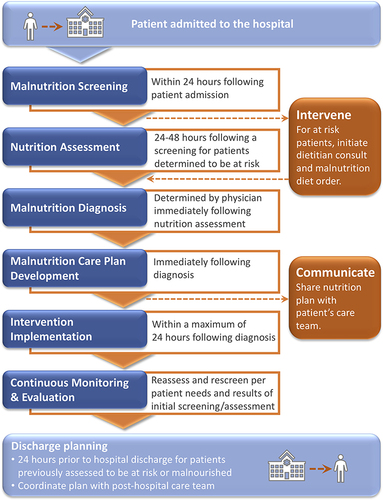
Value is a central aim for healthcare, yet value is defined in varying and sometimes conflicting terms by different stakeholders—providers, payers, and patients.Citation1 In terms of health economics, value is determined by outcomes relative to costs ().Citation2 The numerator of the value equation is outcome, while the denominator is cost. Depending on the stakeholder’s viewpoint, high value may be seen as reduced patient morbidity and mortality, cost containment, or profitability. Some aspects of value are important to patients and providers alike, eg, outcomes such as survival, fast recovery, few or no complications during hospitalization, and quality of life, as well as experience or satisfaction. To hospitals and healthcare systems, measurable outcomes that contribute to value include reduced length of stay (LOS) and lower readmission rates. Cost-effective treatments represent value to payers. Levels of patient-perceived satisfaction with care are being increasingly monitored as measures of healthcare quality, thus representing values shared by both patients and provider systems.Citation3 Like healthcare processes in general, nutrition care in hospitals and other healthcare settings is beneficial when it improves outcomes. The value of nutrition care is demonstrated when improved health outcomes for hospitalized patients are achieved at reasonable incremental costs for nutrition care and with reduced overall costs of care. Health economic studies support the concept that nutrition care can improve patient outcomes while reducing costs. Several years ago, a pivotal and large-scale data analysis by Philipson et al first raised awareness that therapeutic nutrition care during hospitalization—use of oral nutritional supplements (ONS) for inpatients identified as being at risk for malnutrition—could significantly improve health outcomes and lower costs of care.Citation4,Citation5 Specifically, ONS use was associated with a 2-day reduction in LOS in hospital and with cost savings for inpatient care estimated at over $4,700 per patient.Citation5 Based on this analysis and other work, healthcare decision-makers worldwide have likewise begun to realize that therapeutic nutrition plays important and cost-saving roles in overall care, ie, the value of nutrition care.Citation6–Citation10
Figure 1 For a hospitalized patient with malnutrition or its risk, the value of nutrition care is determined by improved health outcomes relative to cost of care.
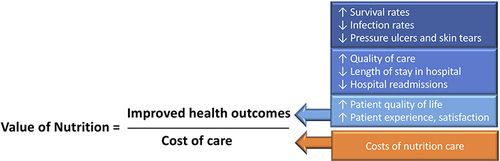
Table 1 Examples of US Hospital Quality Improvement Programs That Used ONS to Treat Malnutrition or Its Risk, Improve Health Outcomes, and Lower Costs of Care
To highlight value in nutrition care, this paper will review evidence of the health and financial tolls of disease-associated malnutrition in hospitals, report real-world results from nutrition-focused quality improvement programs (QIPs) in hospitals, and discuss clinical and policy implications of value in nutrition care for hospitalized patients with disease-associated malnutrition.
Definitions
As background for our discussion, definitions of terms relevant to malnutrition and its care are provided (Box 1).
Box 1 Malnutrition Care Definitions
The Cost Burden of Malnutrition
Disease-associated malnutrition is common and costly in healthcare settings. Financial costs of disease-associated malnutrition in the USA have been estimated as more than $147 billion per year,Citation13,Citation14 with $15.5 billion attributed to direct therapeutic costs.Citation15 US inpatients who also had a diagnosis of malnutrition had up to two-fold higher hospital costs compared to those for adequately nourished inpatients.Citation16 Similarly, the Canadian Malnutrition Task Force reported that 40% of patients were malnourished at hospital admission, and they cost between $1,500 and $2,000 more per hospital stay than an adequately nourished patient.Citation17 As such, the excess cost of malnutrition to Canadian hospitals was estimated at about $2 billion per year.Citation17
Cost Savings Attributed to Therapeutic Nutrition Support
The results of a wide range of studies (n=34) showed that the use of therapeutic nutrition—ONS, enteral nutrition (EN), and parenteral nutrition (PN)—plays an important role in the quality of care and in overall outcomes of care.Citation6 While nutrition care for patients with disease-associated malnutrition includes nutrition services/consultation, as well as food fortification, ONS, and EN or PN, most health economic studies to date have evaluated ONS value, as ONS beverages are often selected by nutrition professionals for individualized nutrition support. Numerous studies have compared ONS with routine care (no use of ONS) for hospitalized patients with malnutrition. In a comprehensive review of nutrition care in hospitalized patients, use of ONS led to median cost savings of 12.2% when quantitative data were available.Citation8 Savings were associated with fewer complications and shortened LOS in hospital.Citation8 Similarly, older people discharged from US hospitals experienced more quality-adjusted life years when they were given ONS; costs were well within standards of a cost-effective treatment.Citation18 These studies examined the effects of different ONS products on patients with a wide variety of diseases and conditions, underscoring the importance of medical nutrition therapy (MNT) advised by a nutrition professional. Notably, it has been estimated that every dollar spent for MNT provided under the care of a nutrition professional can yield five to 99 times that amount in savings on subsequent medical care.Citation19
Best-Practice Medical Nutrition Support Across the Continuum of Care
According to nutrition experts in the USA and Canada, optimal and patient-focused nutrition care is guided by key actions: screening patients for malnutrition risk; diagnosing those who are malnourished; implementing individualized nutrition interventions promptly and continuing to monitor for status changes; communicating nutrition plans with members of the patient’s care team; and developing a post-discharge nutrition and education plan for the patient ().Citation20–Citation22 The patient’s full hospital care team includes physicians, nurses and nursing assistants, dietitians and dietetic technicians, and pharmacists and pharmacy technicians. Registered Dietitian Nutritionists are recognized for the key roles they play in ensuring best-practice nutrition care during hospitalization, and they are recognized to add “value” by helping prevent hospitalizations and excess healthcare costs for people with chronic diseases.Citation23–Citation25 It has also been noted that nurses are ideally positioned to play critical roles in nutrition-related care since they are involved in the initial screening and they regularly observe and monitor the patients during hospitalization.Citation26 Post-discharge nutrition education may need to target the patient, his or her family members, and other caregivers, depending on each individual’s situation.
Quality Improvement Programs Translate Nutrition Care Value to Practice
We believe that the evidence clearly supports the value of optimal nutrition in healthcare settings, especially on admission to hospital. Specifically, disease-associated malnutrition predisposes patients and care systems to adverse clinical outcomes and excess costs, while early nutritional intervention can help achieve better outcomes and cut costs.
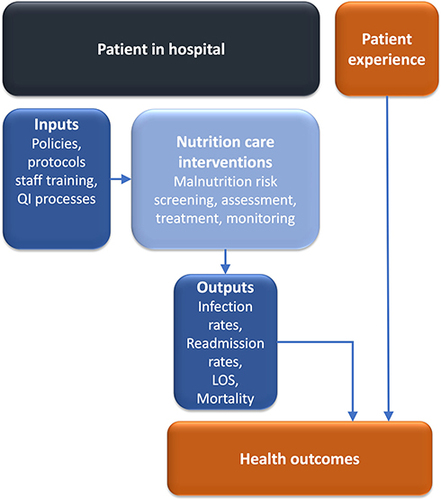
To put such actions into practice, QIPs have been applied. The quality improvement (QI) process is intended to combine the efforts of multiple stakeholders—healthcare professionals, planners and educators, and patients and their families—to implement changes that can lead to better patient outcomes (health and satisfaction with care), better system performance (care), and better professional development.Citation27 QIPs have been increasingly used for improving nutrition care processes, especially for increasing the effective use of ONS to treat malnutrition and those at risk. Such studies have been led by nurses, dietitians, and other nutrition-focused healthcare professionals in large healthcare systems. The QI process generally involves iterative cycles of process change with outcome measurements before and after changes are implemented (). An ever-growing number of QIPs have been implemented to help achieve best-practice nutrition care in hospital settings. Taken together, the findings of such studies provide compelling data showing that nutrition-focused QIPs can improve the identification of hospitalized patients with malnutrition or its risk, enhance nutrition practice and care (including use of ONS), and lower costs, mainly by reducing hospital LOS and readmission rates. Here, we summarize five recent studies that evaluated “value” in the use of ONS for care of patients with disease-associated malnutrition in US hospital settings (). Nutrition-focused QIP efforts have recently been extended to programs for home health care as well.Citation28
Figure 3 Policies and processes for improving the quality of nutrition care for hospitalized patients with malnutrition or its risk. A patient’s experience is a key component of the health outcome.
Quality Nutrition Care in Action: From Policy to Practice
Improved quality of care begins with effective policies—in both governmental and specific healthcare settings. In the US, The Joint Commission (TJC) is an independent organization that accredits, certifies, and provides disease management standards for healthcare organizations. TJC promotes effective and continuous improvements of quality and safety within healthcare. TJC’s standards state that nutritional and functional screenings are performed when warranted by the patient’s needs or condition. Each healthcare organization is expected to define in writing the criteria that identify when screenings and more in-depth assessments are needed. When applicable for the patient’s condition, nutrition screenings must be completed within 24 hours of inpatient admission.Citation29
To support nutrition care processes, the Academy of Nutrition and Dietetics, along with Avalere Health and other stakeholders recently developed a practical program to guide nutrition screening, assessment of nutrition status for malnutrition diagnoses, prompt initiation of treatment when needed, and ongoing monitoring of care—the Malnutrition Quality Improvement Initiative (MQii).Citation22,Citation30-Citation38 MQii offers tips for electronic Clinical Quality Measures (eCQMs) to be added to electronic health records, and it contains a toolkit to initiate such a program for nutrition-focused QI. Recent studies have shown that MQii can improve nutrition awareness and care in hospitals with remarkable cost-saving results.Citation30–Citation38
Take-Home Messages on the Value of Nutrition
Cost containment is important to healthcare providers, but cost cutting without regard for overall value—health and quality outcomes included—is perilous.Citation39 To bring the value of nutrition to healthcare, policies and practices supporting nutrition care during hospitalization and in post-discharge settings are essential. In this article, we have provided considerable evidence on the “value of nutrition” based on data from clinical studies and from real-world programs evaluating hospitalized patients who are malnourished or at risk for malnutrition.
Acknowledgment
We would like to thank Cecilia Hofmann of C. Hofmann & Associates for her help with manuscript review and editing.
Author Contributions
All authors made a significant contribution to the work reported, took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Financial support for preparation of this paper was provided by Abbott, USA.
Disclosure
S Sulo is an employee and stockholder of Abbott, USA. K Sriram has received consultancy fees in the past from Abbott, USA, not related to the present work. Leah Gramlich reports grants from, and speaker’s bureau and consultancy for, Baxter, Fresenius Kabi, and Abbott, outside the submitted work. Jan Powers reports personal fees from Abbott Nutrition, Avanos Medical, and Envizion Medical, outside the submitted work. Kristi Mitchell reports that the Malnutrition Quality Improvement Initiative, the national learning collaborative where participating sites in this study engaged, is sponsored by Abbott Nutrition. J Benjamin is an employee of Kaiser Permanente. S McCauley has no conflicts of interest. The authors report no other potential conflicts of interest in this work.
References
- Porter ME. What is value in health care? N Engl J Med. 2010;363(26):2477–2481. doi:10.1056/NEJMp1011024
- Philipson T, Linthicum MT, Snider JT. Tutorial on health economics and outcomes research in nutrition. JPEN J Parenter Enteral Nutr. 2014;38(2 Suppl):5S–16S. doi:10.1177/0148607114549770
- Centers for Medicare & Medicaid Services. Hospital inpatient quality reporting program. CMS. CMS.gov. 2017. Available from: https://www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/hospitalqualityinits/hospitalrhqdapu.html. Accessed April 17, 2020.
- Lakdawalla DN, Snider JT, Perlroth D, et al. Can oral nutritional supplements improve medicare patient outcomes in the hospital? Forum Health Econ Policy. 2014;17(2):131–151. doi:10.1515/fhep-2014-0011
- Philipson TJ, Snider JT, Lakdawalla DN, Stryckman B, Goldman DP. Impact of oral nutritional supplementation on hospital outcomes. Am J Manag Care. 2013;19(2):121–128.
- Walzer S, Droeschel D, Nuijten M, Chevrou-Severac H. Health economics evidence for medical nutrition: are these interventions value for money in integrated care? Clinicoecon Outcomes Res. 2014;6:241–252.
- Buitrago G, Vargas J, Sulo S, et al. Targeting malnutrition: nutrition programs yield cost savings for hospitalized patients. Clin Nutr. 2019;S0261–S5614(19):33213.
- Elia M, Normand C, Norman K, Laviano A. A systematic review of the cost and cost effectiveness of using standard oral nutritional supplements in the hospital setting. Clin Nutr. 2016;35(2):370–380. doi:10.1016/j.clnu.2015.05.010
- Tyler R, Barrocas A, Guenter P, et al. Value of nutrition support therapy: impact on clinical and economic outcomes in the United States. JPEN J Parenter Enteral Nutr. 2020;44(3):395–406. doi:10.1002/jpen.1768
- Khalatbari-Soltani S, Marques-Vidal P. Impact of nutritional risk screening in hospitalized patients on management, outcome and costs: a retrospective study. Clin Nutr. 2016;35(6):1340–1346. doi:10.1016/j.clnu.2016.02.012
- World Health Organization. Malnutrition. WHO. 2018. Available from: https://www.who.int/news-room/fact-sheets/detail/malnutrition. Accessed April 17, 2020.
- Academy of Nutrition and Dietetics. MNT versus nutrition education. 2020. Available from: https://www.eatrightpro.org/payment/coding-and-billing/mnt-vs-nutrition-education. Accessed April 17, 2020.
- Sulo S, Feldstein J, Partridge J, Schwander B, Sriram K, Summerfelt WT. Budget impact of a comprehensive nutrition-focused quality improvement program for malnourished hospitalized patients. Am Health Drug Benefits. 2017;10(5):262–270.
- Snider JT, Linthicum MT, Wu Y, et al. Economic burden of community-based disease-associated malnutrition in the United States. JPEN J Parenter Enteral Nutr. 2014;38(2 Suppl):77S–85S. doi:10.1177/0148607114550000
- Goates S, Du K, Braunschweig CA, Arensberg MB, Dowdy DW. Economic burden of disease-associated malnutrition at the state level. PLoS One. 2016;11(9):e0161833. doi:10.1371/journal.pone.0161833
- Barrett M, Baily M, Owens P. Non-maternal and non-neonatal inpatient stays in the United States involving malnutrition, 2016. In: US Agency for Healthcare Research and Quality 2018; 2018;1–29. Available from: www.hup-us.ahrq.gov/reports.jsp.
- Curtis LJ, Bernier P, Jeejeebhoy K, et al. Costs of hospital malnutrition. Clin Nutr. 2017;36(5):1391–1396. doi:10.1016/j.clnu.2016.09.009
- Zhong Y, Cohen JT, Goates S, Luo M, Nelson J, Neumann PJ. The cost-effectiveness of oral nutrition supplementation for malnourished older hospital patients. Appl Health Econ Health Policy. 2017;15(1):75–83. doi:10.1007/s40258-016-0269-7
- Howatson A, Wall CR, Turner-Benny P. The contribution of dietitians to the primary health care workforce. J Prim Health Care. 2015;7(4):324–332. doi:10.1071/HC15324
- Tappenden KA, Quatrara B, Parkhurst ML, Malone AM, Fanjiang G, Ziegler TR. Critical role of nutrition in improving quality of care: an interdisciplinary call to action to address adult hospital malnutrition. JPEN J Parenter Enteral Nutr. 2013;37(4):482–497. doi:10.1177/0148607113484066
- Keller HH, McCullough J, Davidson B, et al. The Integrated Nutrition Pathway for Acute Care (INPAC): building consensus with a modified Delphi. Nutr J. 2015;14:63–74. doi:10.1186/s12937-015-0051-y
- Fitall E, Pratt KJ, McCauley SM, et al. Improving malnutrition in hospitalized older adults: the development, optimization, and use of a supportive toolkit. J Acad Nutr Diet. 2019;119(9S2):S25–S31. doi:10.1016/j.jand.2019.05.024
- Kalantar-Zadeh K, Fouque D. Nutritional management of chronic kidney disease. N Engl J Med. 2018;378(6):584–585. doi:10.1056/NEJMc1715765
- Robbins JM, Thatcher GE, Webb DA, Valdmanis VG. Nutritionist visits, diabetes classes, and hospitalization rates and charges: the Urban Diabetes Study. Diabetes Care. 2008;31(4):655–660. doi:10.2337/dc07-1871
- Sikand G, Cole RE, Handu D, et al. Clinical and cost benefits of medical nutrition therapy by registered dietitian nutritionists for management of dyslipidemia: a systematic review and meta-analysis. J Clin Lipidol. 2018;12(5):1113–1122. doi:10.1016/j.jacl.2018.06.016
- Meehan A, Partridge J, Jonnalagadda SS. Clinical and economic value of nutrition in healthcare: a nurse’s perspective. Nutr Clin Pract. 2019;34(6):832–838. doi:10.1002/ncp.10405
- Batalden PB, Davidoff F. What is “quality improvement” and how can it transform healthcare? Qual Saf Health Care. 2007;16(1):2–3. doi:10.1136/qshc.2006.022046
- Riley K, Sulo S, Dabbous F, et al. Reducing hospitalizations and costs: a home health nutrition-focused quality improvement program. JPEN J Parenter Enteral Nutr. 2020;44(1):58–68. doi:10.1002/jpen.1606
- The Joint Commission. Standards FAQ details: nutritional and functional screening requirement. 2017. Available from: https://www.jointcommission.org/en/standards/standard-faqs/critical-access-hospital/provision-of-care-treatment-and-services-pc/000001652/. Accessed April 16, 2020.
- Academy of Nutrition and Dietetics. Malnutrition quality improvement initiative. Academy of Nutrition and Dietetics. 2016 [Updated 2018]. Available from: http://mqii.defeatmalnutrition.today. Accessed April 17, 2020.
- Arensberg MB, D’Andrea C, Khan M. Clinical leadership and innovation help achieve malnutrition quality improvement initiative success. J Acad Nutr Diet. 2019;119(9S2):S49–S55. doi:10.1016/j.jand.2019.05.021
- Danis K, Kline M, Munson M, et al. Identifying and managing malnourished hospitalized patients utilizing the malnutrition quality improvement initiative: the UPMC experience. J Acad Nutr Diet. 2019;119(9S2):S40–S43.
- McCauley SM, Mitchell K, Heap A. The malnutrition quality improvement initiative: a multiyear partnership transforms care. J Acad Nutr Diet. 2019;119(9S2):S18–S24. doi:10.1016/j.jand.2019.05.025
- Nepple KG, Tobert CM, Valladares AF, Mitchell K, Yadrick M. Enhancing identification and management of hospitalized patients who are malnourished: a pilot evaluation of electronic quality improvement measures. J Acad Nutr Diet. 2019;119(9S2):S32–S39. doi:10.1016/j.jand.2019.05.023
- Pratt KJ, Hernandez B, Blancato R, Blankenship J, Mitchell K. Impact of an interdisciplinary malnutrition quality improvement project at a large metropolitan hospital. BMJ Open Qual. 2020;9(1):e000735. doi:10.1136/bmjoq-2020-000924
- Silver HJ, Pratt KJ, Bruno M, Lynch J, Mitchell K, McCauley SM. Effectiveness of the malnutrition quality improvement initiative on practitioner malnutrition knowledge and screening, diagnosis, and timeliness of malnutrition-related care provided to older adults admitted to a tertiary care facility: a pilot study. J Acad Nutr Diet. 2018;118(1):101–109. doi:10.1016/j.jand.2017.08.111
- Valladares AF, Kilgore KM, Partridge J, Sulo S, Kerr KW, McCauley S. How a malnutrition quality improvement initiative furthers malnutrition measurement and care: results from a hospital learning collaborative. JPEN J Parenter Enteral Nutr. 2020.
- Doley J, Phillips W, Talaber J, Leger-LeBlanc G. Early implementation of malnutrition clinical quality metrics to identify institutional performance improvement needs. J Acad Nutr Diet. 2019;119(4):547–552.
- Bortoletto P, Little SE. Assess the ‘value’ of a healthcare intervention, not just its price: study design: economic evaluation. BJOG. 2019;126(4):525.
- Meehan A, Loose C, Bell J, Partridge J, Nelson J, Goates S. Health system quality improvement: impact of prompt nutrition care on patient outcomes and health care costs. J Nurs Care Qual. 2016;31(3):217–223. doi:10.1097/NCQ.0000000000000177
- Sriram K, Sulo S, VanDerBosch G, et al. A comprehensive nutrition-focused quality improvement program reduces 30-day readmissions and length of stay in hospitalized patients. JPEN J Parenter Enteral Nutr. 2017;41(3):384–391.
- Sriram K, Sulo S, VanDerBosch G, et al. Nutrition-focused quality improvement program results in significant readmission and length of stay reductions for malnourished surgical patients. JPEN J Parenter Enteral Nutr. 2018;42(6):1093–1098. doi:10.1002/jpen.1040
- Siegel S, Fan L, Goldman A, Higgins J, Goates S, Partridge J. Impact of nutrition-focused quality improvement on length of stay. J Nutr Care Qual. 2019;34(3):203–209. doi:10.1097/NCQ.0000000000000382