Abstract
Objective
To study the pattern of psychotropic medication use and compare this pattern between inpatient and outpatient psychiatric settings in Saudi Arabia.
Method
This cross-sectional observational study was conducted between July 2012 and June 2014 on patients seeking psychiatric advice at major hospitals in five main regions of Saudi Arabia. Male (n=651) and female (n=594) patients who signed the informed consent form and were currently or had been previously using psychotropic medications, irrespective of the patient’s type of psychiatric diagnosis and duration of the disease, were included. A total of 1,246 patients were found to be suitable in the inclusion criteria of whom 464 were inpatients while 782 were outpatients.
Results
Several studied demographic factors have shown that compared with outpatients, inpatients were more likely to be male (P=0.004), unmarried (P<0.001), have less number of children (1–3; P=0.002), unemployed (P=0.001), have a lower family income (<3,000 SR; P<0.001), live in rural communities (P<0.001), have a lower body mass index (P=0.001), and are smokers (P<0.001); however, there were no differences with regard to age or educational levels. The current frequency of use of psychotropic medications in overall patients was antipsychotics (76.6%), antidepressants (41.4%), mood stabilizers (27.9%), and antianxiety (6.2%). However, compared to outpatients, the current use of medications for inpatients was more frequent (93.8% vs 89.9%, P=0.019) with inpatients more likely to be treated with multiple medications (2.1 vs 1.8 medications). A similar trend was observed in the case of antipsychotics, high potency first-generation antipsychotics, second-generation antipsychotics, mood stabilizers, and antianxiety medicines where inpatients were more frequently treated with these medications for all psychiatric diagnoses when compared with outpatients. On the contrary, in the case of antidepressant treatment, an opposite trend was observed with more number of treated outpatients in comparison to inpatients. Among elderly patients, 75.9% received antipsychotics, mainly second-generation formulations (67.2%), whereas only 41% received antidepressants and 13.8% received mood stabilizers.
Conclusion
Based upon the present study data, it is concluded that among all the psychotropic medications, antipsychotics were heavily used and the frequency was found to be significantly high in the case of inpatients compared with outpatients. Such a practice may lead to multiple negative consequences among the Saudi psychiatric patient population. Further, extensive use of sodium valproate in the case of bipolar disorder, and also among females either in childbearing age or during pregnancy is also the cause of concern and warrants logical use. Overall, this study may help in assessing the burden of psychiatric illness within specific patient demographics and might be effectively used to strategically plan health resources allocation, generate new treatment hypothesis, or be used as a source of evidence that could further integrate other observational studies.
Introduction
Psychotropic medications, such as phenothiazine, thioxanthene, or butyrophenone-type neuroleptics, lithium salts, tricyclic antidepressants, irreversible monoamine oxidase inhibitors, and benzodiazepines, have been used for more than 60 years in clinical practices. Most of the new generation of psychotropics have appeared after 1985 and, even more recently, atypical antipsychotics, antiepileptics as mood stabilizers, and antidementia medications. Compared with the old medications, the newer medications have similar efficacies but better tolerability and fewer side effects.Citation1,Citation2
Many international studies have directly or indirectly noted how clinical practice and actual psychotropic prescribing practices in both hospital and outpatient settings do not always agree with internationally recognized guidelines.Citation1–Citation4 A proper evaluation of the difference between actual practice and a theoretical, gold standard-oriented approach may help to avoid several erroneous trends that may negatively affect patient outcomes and other pharmacoeconomic issues. For example, some international studies have reported an increase in the practice of polypharmacy, that is, the use of four or more medications specially by the elderly population,Citation5 and the prescription of new and expensive medications and low-dose and off-label drugs to women and children.Citation4 Most of the studies that evaluated use of psychotropic drugs have reported a high rate of prescriptions for multiple drugs, which usually occurs when there was no improvement in clinical symptoms.Citation2 A UK survey found that more than 50% of hospitalized patients were receiving more than one type of antipsychotic medication.Citation6
Although hospitalization is often preferred in many major psychiatric diseases, such as schizophrenia or bipolar disorder, treatment as outpatients is also employed to maintain community ties and a patient’s autonomy,Citation7 thereby resulting in satisfactory treatment results while still reducing overall costs.Citation8 Outpatient psychiatric services often complement inpatient ones and limit the excessive use of mental health services; nonetheless, patient populations for whom substitution is possible should be accurately analyzed to avoid an overall reduction of care for patients who fail to follow-up with their treatment.Citation9,Citation10
The overall situation of mental health services and prescribing practices in Saudi Arabia has been previously investigated in other studies, but more data are still needed to successfully assess the trends and prescribing habits and to gain a broader view.Citation11 Studies with a larger scope have focused more on the mental health system’s general situation rather than on a detailed view of the current trends for inpatient and outpatient psychotropic medication prescriptions,Citation12 whereas other studies smaller in scope have only analyzed local data.Citation13 The objective of the current study was to study the pattern of psychotropic medication use and compare the frequency of prescribing psychotropic medications between inpatient and outpatient settings in Saudi Arabia.
Methods
Setting
The current study was conducted among patients seeking psychiatric advice at major hospitals in Saudi Arabia. The patients were recruited from a number of hospitals located in the Central, Eastern, Western, Northern, and Southern regions of Saudi Arabia. The hospitals included in the study were King Khalid University Hospital in Riyadh and Zulfi General Hospital (Central region), Jeddah Mental Health Hospital (Western region), Al Amal Complex for Mental Health – Dammam (Eastern region), Aljouf Mental Health Hospital (Northern region), and Abha Mental Health Hospital (Southern region). King Khalid University Hospital is a university-affiliated governmental hospital, whereas the other hospitals are government-funded hospitals under the authority of the Ministry of Health. All of the hospitals included in this study provide free psychiatric inpatient and outpatient health care services.
Study design
A cross-sectional observational study was conducted between July 2012 and June 2014. The study obtained all of the required ethical approvals from the Institutional Review Board at the Faculty of Medicine at King Saud University in Riyadh and administrative approvals from the respective hospitals. The study was funded by the National Plan for Science and Technology Strategic Grants Program.
Population
Male and female patients seeking psychiatric help from the included hospitals during the study period were asked to join the study. Those who signed the informed consent form and were currently or had been previously using psychotropic medications, irrespective of the patient’s type of psychiatric diagnosis and the duration of the disease, were included.
Data collection
A mini-interview form was developed, which included sociodemographic characteristics, detailed current and previous psychotropic medication use (including the name of the medication, dose, and duration), and current psychiatric diagnoses. The information was mainly obtained by reviewing each patient’s chart. Unclear/missing information was confirmed by interviewing the patient and/or his/her family. Trained psychiatric residents/staff were responsible for chart review and conducting interviews with the patients and/or their families.
Classification of psychotropic medications
Both the individual psychotropic medications and their pharmacologic groups were used in the analysis. These medications and groups include antidepressants (selective serotonin reuptake inhibitors, tricyclics, and others), antipsychotics (low potency first-generation and high potency first- and second-generation), antianxiety medications, and mood stabilizers.
Classification of psychiatric diagnosis
For the purpose of data analysis, the psychiatric diagnosis of the studied patients was classified under seven categories. “Primary psychotic disorders” included schizophrenia, schizoaffective disorder, delusional disorder, and brief psychotic disorder. “Primary bipolar disorders” included bipolar disorder and its features. “Primary depressive disorders” included major depressive disorder and dysthymic disorder. “Primary anxiety disorders” included generalized anxiety disorder, obsessive compulsive disorder, social anxiety disorder, specific phobias, panic disorder, post-traumatic stress disorder, and acute stress disorder. “Personality disorders” included mixed personality disorder, paranoid personality disorder, antisocial personality disorder, and borderline personality disorder. “Secondary psychiatric disorders” included psychotic disorder due to another medical condition, depression due to another medical condition, dementia, substance use disorder, and substance-induced depressive disorder. “Other disorders” included somatic symptom disorder, mental retardation, conversion disorder, attention deficit hyperactivity disorder, dissociative disorder, primary insomnia, adjustment disorder, enuresis disorder, trichotillomania, and anorexia nervosa.
Statistical analysis
The data are presented in frequencies and percentages for categorical data and mean values and standard deviations for continuous data. Individual psychiatric diagnosis and psychotropic medications were categorized into standard groups. Significant differences between inpatient and outpatient settings as they pertained to sociodemographics, psychotropic medication use, and psychiatric diagnosis were tested using the chi-square test or Fisher’s exact test (as appropriate) for categorical data and the Student’s t-test for continuous data. All P-values were two-tailed, and a P-value <0.05 was considered a significant value. SPSS software (release 20.0, SPSS Inc., Chicago, IL, USA) was used for the statistical analysis.
Results
A total of 1,246 patients (464 inpatients and 782 outpatients) were included in the current analysis.
Demographic characteristics
demonstrates the demographic characteristics of inpatients and outpatients studied. In terms of age, both types of patients were categorized into three categories, that is, <40, 40–60, and >60 years. Inpatients and outpatients were found to show similar trend with the average majority (58.9%) lying below the age of 40 followed by the age of 40–60 (35.9%) and >60 (5.2%). Similarly, no major sex difference was noticed with an average of 52.3% males and 47.7% females. Approximately 45.6% of the patients were married, and 54.4% were unmarried: single (44.1%), divorced (9.2%), or widowed (1.1%). However, significant difference (P<0.001) was obtained in this case where inpatients have a majority of single and divorced persons while outpatients have a maximum number of married and widowed persons.
Table 1 Demographic characteristics by type of patient setting (N=1,246)
Further, ~75.9% of the patients had children, in which the percentage of inpatients was more who possess one to three children in comparison with outpatients while the opposite was obtained where the number of children exceeds three.
All inpatients and outpatients were also recorded for their education level as illiterates, possess secondary education or less, and university level. No noticeable differences were observed in any of the education levels when compared between inpatients and outpatients, with an average majority (65.0%) falling in the category of less than secondary education.
When analyzed for their job status, partial variations were observed in patients who were in government job and unemployed persons. While more number of outpatients was recorded in the former condition, more number of inpatients was found in the latter status. However, overall among all the job status (private, government, business, or unemployed), the highest average (71.4%) belongs to unemployed patients. Approximately 61.9% of the total patients had a moderately low family monthly income (6,000 Saudi Riyal [SR] or less). Marked differences (P<0.001) were found with the number of inpatients comparatively more in low income category (<3,000 SR) and number of outpatients in high income category (>9,000 SR). The majority (80.9%) of the total patients reside in urban communities, with no major differences between the inpatient and outpatient count. The average body mass index was 28.6±7.6, and 67.1% of patients were either overweight or obese. Approximately 45.7% of patients were either current (33.7%) or previous (12.0%) smokers.
Overall, compared with outpatients, inpatients were more likely to be male (P=0.004), unmarried (P>0.001), have less number of children (1–3; P=0.002), unemployed (P=0.001), have a lower family income (>3,000 SR; P<0.001), live in rural communities (P<0.001), have a lower body mass index (P=0.001), and smokers (P<0.001); however, there were no differences with regard to age or educational levels.
Current and previous use of antipsychotic medications in inpatients and outpatients
illustrates the overall usage of psychotropic medications in current as well as in previous scenario and the following frequencies were recorded: antipsychotics (76.6% and 76.1%, respectively), antidepressants (41.4% and 38.5%, respectively), mood stabilizers (27.9% and 23.5%, respectively), and antianxiety medications (6.2% and 3.6%, respectively). Compared to outpatients, the current use of medications for inpatients was more frequent (93.8% vs 89.9%, P=0.019), whereas their previous medication use was approximately similar (76.3% vs 78.1%, P=0.452). Additionally, inpatients were more likely to currently (2.1±0.8 vs 1.8±0.7, P<0.001) and previously (2.0±0.8 vs 1.7±0.7, P<0.001) use multiple medications compared with outpatients.
Figure 1 Frequencies of current and previous uses of different psychotropic medications (N=1,246)
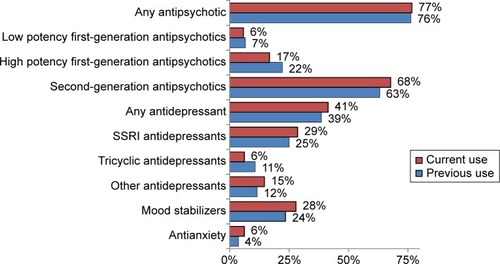
The current and previous uses of different psychotropic medications in inpatients and outpatients are shown in –. With very few exceptions, different groups of antipsychotic medications were both currently and previously more frequently used among inpatients compared with outpatients (). For example, antipsychotic medications were currently used for 94.3% of inpatients and 65.7% for outpatients (P<0.001). This trend was similarly observed in the heavily used second-generation group and less commonly used high potency first-generation groups (P<0.001 for all), but not in low potency first-generation group. However, the different groups of antidepressant medications were both currently and previously more frequently used among outpatients compared with inpatients (). For example, any antidepressant medications were currently used in 54.1% of outpatient settings and 20.9% of inpatient settings (P<0.001). This trend was similarly observed within the commonly used groups, such as selective serotonin reuptake inhibitors, and with the less commonly used tricyclics and other types of anti-depressants (P<0.001 for all). Current and previous uses of mood stabilizers and antianxiety medications were more frequently observed among inpatients compared with outpatients (). For example, mood stabilizers were currently used for 40.7% of inpatients and 20.1% of outpatients (P<0.001), and antianxiety medications were currently used for 13.3% of inpatients and 1.8% of outpatients (P<0.001).
Table 2 Current and previous uses of antipsychotic medications by type of patient setting (N=1,246)
Table 3 Current and previous uses of antidepressant medications by type of patient setting (N=1,246)
Table 4 Current and previous uses of other psychotropic medications by type of patient setting (N=1,246)
shows the current prevalence in the prescription of psychotropic medications according to psychiatric diagnosis in both inpatient and outpatient settings. Antipsychotic medications were heavily used (more than 85%) in almost all inpatient psychiatric diagnosis, with the exception of primary anxiety and depressive disorders. Additionally, antipsychotic use was more frequent among inpatients than outpatients for all psychiatric diagnosis, with the exception of personality and secondary psychiatric disorders. Antidepressant medications were heavily used (80% or more) in outpatient settings for primary anxiety disorders, primary depressive disorders, and personality disorders. Additionally, antidepressant use was more common for outpatients than for inpatients, especially for those with primary anxiety disorders and primary bipolar disorders. Mood stabilizers were frequently used for primary bipolar disorders among inpatients and outpatients (~75%), and their use was generally higher among inpatients than among outpatients. Antianxiety medications were largely administered (14%–27%) for primary bipolar disorders, primary anxiety disorders, and personality disorders, mainly among inpatients.
Table 5 Prevalence rates of current uses of psychotropic medications by psychiatric diagnoses and type of patient setting (N= 1,246)
Among all of the participants, lithium was only used by 2.6% of participants, compared to 26.7% of participants using various anticonvulsants (sodium valproate 18.6%, carbamazepine 5.8%, and lamotrigine 2.3%). Specifically, among women of childbearing age (18–45 years), sodium valproate was the most used mood-stabilizing agent (20.8%), whereas lithium was used only by 3.6%. Moreover, during pregnancy, there is a trend of preferring sodium valproate as a mood-stabilizing agent (7.7%) over lithium (0%), although the small sample size of the pregnant participants (15 participants, 2.5%) makes it difficult to attain statistically significant results.
Among elderly patients (older than 60 years), 75.9% received antipsychotics, mainly second-generation drugs (67.2%), whereas only 41% received antidepressants and 13.8% received mood stabilizers.
Discussion
The present study represented and analyzed data about the use of psychotropic medications in inpatients and outpatients from six hospitals in Saudi Arabia. These data clearly indicate that a large percentage of the total inpatient and outpatient participants (77%, ) received at least one antipsychotic drug while other drugs were prescribed in much smaller percentages, including antidepressants (41%), mood stabilizers (28%), and antianxiety drugs (6%). Further, it was also noticed that in comparison to outpatients (65.7%), almost all hospitalized patients (94.3%) were more often treated with at least one antipsychotic medication. On the contrary, a much larger percentage of outpatients were treated with antidepressants of any kind compared with inpatients (54.1% vs 20.9%, ). The use of antipsychotic medications for the treatment of several major psychiatric diseases, including depression,Citation5 is becoming common practice. The present data suggest that inpatients suffering from depression are more often managed by using psychotropic medications, which may necessitate a high level of care for their appropriate prescription and dosing.Citation3 It is to be noticed that treatment with antipsychotic medications (alone or in combination) showed a better response rate only if the patient suffers from major psychotic depression,Citation6 and these drugs may possess severe adverse side effects that could cause negative outcomesCitation7,Citation8 and could increase morbidity and mortality from a range of medical causes.Citation9 Considering the overuse of psychotropic medications as also indicated by the present study data, it is strongly recommended that great care and attention should be paid while prescribing these medications specifically for the agents which lack adequate scientific evidence.Citation4 A similar trend was also found in case of mood stabilizers and antianxiety drugs where frequency of prescription of these drugs was more in inpatients (40.7% and 13.3%) than outpatients (20.1% and 1.8%, ).
The present study also noticed that patients on antipsychotic medications in Saudi Arabia possess several risk factors, such as smoking, dyslipidemia, overweight, and obesity. As shown in the demographic characteristics in , ~45.7% of the patients were either current (33.7%) or previous (12.0%) smokers, and 67.1% of them were either overweight or obese. While these risk factors are reportedly associated with major mental illnesses, such as schizophrenia or bipolar disorder,Citation13,Citation14 they also lead to increased susceptibility for progression of diabetes, weight gain, and other metabolic and cardiovascular diseases.Citation11,Citation12 Further, association of other demographic factors was also studied for all the participants. The study findings revealed that more than half of the patients (54.4%, ) are unmarried – single (44.1%), divorced, (9.2%), or widowed (1.1%), although approximately three-quarters of them (75.9%) had at least one child. It is known that family support and social interactions play a crucial role in reducing psychotic episodes, and encourage patients to improve their compliance with drug treatments.Citation15,Citation16 Since a large percentage of Saudi Arabian psychiatric patients live in unstable family environments or alone, a series of health policies focusing on a more attentive follow-up treatment after discharge should be considered as a critical part of treatment. Further, a majority of these psychiatric patients were unemployed (71.4%), perhaps either due to being illiterate (21.5%) or with lowest education (65.0%), thereby living in poverty (29.7% of them had a monthly family income of <3,000 SR) (). It is still not clear whether these factors either contribute to the increased prevalence or outcome of psychiatric disorders; previous findings also reported a similar correlation between poverty and/or social vulnerability with mental illness in other countries.Citation17,Citation18
Second-generation antipsychotics are vastly preferred to both high- and low potency first-generation antipsychotics (68% total patients vs 6% and 17%, and ) due to their better safety profiles and improved tolerability.Citation19 However, a strong underuse of clozapine can be noted (only 3.1% of total inpatients and 2.4% of total outpatients, as shown in ), even though this drug is highly recommended among the other antipsychotics.Citation1 Clozapine underuse has also been reported in the USA and the UK, which may be caused by a tendency on the clinician’s part to overestimate the relevance and severity of side effects.Citation20–Citation22 Further, aggressive marketing of other second-generation antipsychotics from pharmaceutical companies may also be a reason why clozapine use is decreasing in hospitals all over the world, including in Saudi Arabia.Citation23 Several studies suggested that detailed marketing campaigns from pharmaceutical companies involved presentation of inaccurate or suppressed data and even more the criteria for mental disorders were in fact stretched to target a vast range of patients.Citation24,Citation25 Several pharmaceutical companies adopted aggressive sales strategies, such as, advertising directly to consumers, influencing prescribers, and paying physicians to market to their peers, presenting overly optimistic cost-effectiveness research, providing free drug samples, sponsoring medical education and patient advocacy groups, and publication of biased results, in order to push widespread usage of second-generation antipsychotics.Citation26
Our data also confirm that mood stabilizers (especially sodium valproate) are often used in addition to primary therapy with antipsychotics for the treatment of most cases of bipolar disorder (77.2%, ). Although this trend is positive, as prescribing sodium valproate in combination with antipsychotics provided better outcomes with mania than with antipsychotic medications alone, effectively lowering the antipsychotic medications’ dosages and consequently their side effects,Citation27 it should also be noted that valproate and carbamazepine are much more frequently used to treat bipolar disorder compared to lithium salt, which should be the current gold standard (343 and 130 total patients for valproate and carbamazepine, respectively, compared to just 55 total patients for lithium).Citation28 Other international studies have shown similar trends, suggesting that although lithium remains the gold standard of treatment, newer agents may sometimes be considered advances in treatment in local clinical practice and habits.Citation28,Citation29 Moreover, among women of childbearing age and even probably among pregnant women, sodium valproate was overused compared to lithium. Similar practices have also been noted in the UKCitation30 and the USA.Citation31 This practice is contrary to recent guidelines that recommend lithium use in this group, granting it higher efficacy data and a safer reproductive profile compared to sodium valproate.Citation32,Citation33 The use of sodium valproate during the first trimester has been associated with major malformations and long-term complications in the form of developmental delay, lower intelligence quotient, and a higher risk of the development of autism spectrum disorder.Citation32,Citation34,Citation35 It is worrisome that the majority of studied psychiatric patients in Saudi Arabia are receiving antipsychotic agents. Moreover, lithium is rarely used in women of childbearing age compared to valproate, which is linked to serious teratogenicity and other adverse effects.
In our study, 75.9% of elderly patients (older than 60 years) received antipsychotics, mainly second-generation drugs (67.2%), whereas only 41% received antidepressants and 13.8% received mood stabilizers. This overuse of antipsychotics among the elderly, despite warnings against this practice, can be explained by their off-label uses for behavioral disturbances that are associated with some mental disorders, such as dementia. Many factors play a role in increasing the risks associated with antipsychotic use among the elderly, including age, associated medical problems, and drug interactions. Thus, the use of antipsychotics for this population should follow recommendations and guidelines.Citation36
It is very interesting to note how in Saudi Arabia only a very small number of patients were prescribed antianxiety drugs. In contrast, alprazolam alone was the most prescribed psychiatric medication in the USA from 2005 to 2013, with 48,465,000 total prescriptions in 2013.Citation37 The greater legal restriction on psychotropic medication use within Saudi Arabian hospitals may be one of the reasons behind this trend, although it could also be that benzodiazepines may be overused in the private sector or as street drugs.Citation38,Citation39 Overall, the study findings indicate that the prescribing practices among psychiatric patients in Saudi Arabia do not conform well to international guidelines.Citation40–Citation42
Conclusion
Our study provides enough data to support and complement correct patient management and prescribing decisions for the use of psychotropic medications in both inpatient and outpatient settings. By investigating both previous and current treatments, we were able to produce an interesting, in-depth analysis that provides new point of view over a large and heterogeneous patient population from the five main regions of Saudi Arabia. Nevertheless, because of the use of convenience sampling, our results should be cautiously generalized to all psychiatric patients in Saudi Arabia. Another main limit is that the available data focus only on a small, 2-year time span (2012–2014); therefore, a more in-depth analysis of previous data may help to assess how prescriptions of psychotropic drugs have changed over the course of the last few years. This study may also help with assessing the burden of psychiatric illness in specific patient demographics and might be effectively used to strategically plan health resource allocation, generate new treatment hypotheses, or serve as a source of evidence that could further integrate other observational studies.
Acknowledgments
This project was funded by the National Plan for Science, Technology and Innovation (MAARIFAH), King Abdulaziz City for Science and Technology, Kingdom of Saudi Arabia, Award Number (MED3130).
Disclosure
The authors report no conflicts of interest in this work.
References
- DavidsEBunkCSpeckaMGastparMPsychotropic drug prescription in a psychiatric university hospital in GermanyProg Neuro-Psychopharmacology Biol Psychiatry200630611091116
- BowersLCallaghanPClarkNEversCComparisons of psychotropic drug prescribing patterns in acute psychiatric wards across EuropeEur J Clin Pharmacol2004601293514747883
- KurodaNSunSLinCKAttitudes toward taking medication among outpatients with schizophrenia: cross-national comparison between Tokyo and BeijingEnviron Health Prev Med200813528829519568916
- DeshmukhSAShaikhTShaikhEEvaluation of psychotropic drugs use pattern among out patients attending psychiatry department at government medical college and hospital, Nagpur: a cross sectional studyInt J Pharm Bio Sci201233428436
- YenilmezÇGüleçGBüyükkınacıABir üniversite hastanesinde yatarak tedavi gören hastalarda çoklu ilaç kullanımı: Geriye dönük bir çalışma [Polypharmacy among inpatients of a university psychiatry clinic: a retrospective study]Dusunen Adam J Psychiatry Neurol Sci2012254350 Turkish
- JordanovaVMaricNPAlikajVPrescribing practices in psychiatric hospitals in Eastern EuropeEur Psychiatry201126741441820828993
- CreedFBlackDAnthonyPOsbornMThomasPTomensonBRandomised controlled trial of day patient versus inpatient psychiatric treatmentBMJ19903006731103310372188696
- LeslieDRosenheckRShifting to outpatient care? Mental health care use and cost under private insuranceAm J Psychiatry199915681250125710450268
- MartinALeslieDPsychiatric inpatient, outpatient, and medication utilization and costs among privately insured youths, 1997–2000Am J Psychiatry2003160475776412668366
- GoldsteinJMHorganCMInpatient and outpatient psychiatric services: substitutes or complements?Hosp Community Psychiatry19883966326363042586
- ShahinSHDalyEBKnowledge, attitudes and beliefs about psychotropic medication among Saudi hospitalized psychiatric patientsInt J Nurs Stud1999361515510375066
- AlkhamisAHealth care system in Saudi Arabia: an overviewEast Mediterr Heal J2012181010781079
- Al-GhamdyYSQureshiNAAbdelghadirMHAl-HabeebTAAhmadSAPsychotropic drugs prescriptions in Al-Qassim Region, Saudi ArabiaEast Mediterr Health J199951273410793778
- CourtneyJA Review of: “Kalyna Z Bezchlibnyk-Butler and Adil S. Varani (2004)”Child Neuropsychol200511311313
- CorrellCUAntipsychotic use in children and adolescents: minimizing adverse effects to maximize outcomesJ Am Acad Child Adolesc Psychiatry200847192018174821
- SutherlandJESutherlandSJHoehnsJDAchieving the best outcome in treatment of depressionJ Farm Pract2003523201209
- De HertMDetrauxJvan WinkelRYuWCorrellCUMetabolic and cardiovascular adverse effects associated with antipsychotic drugsNat Rev Endocrinol20118211412622009159
- NewcomerJWSecond-generation (atypical) antipsychotics and metabolic effects: a comprehensive literature reviewCNS Drugs200519suppl 119315998156
- LlorenteMDUrrutiaVDiabetes, psychiatric disorders, and the metabolic effects of antipsychotic medicationsClin Diabetes2006241824
- HongCHOhBHInappropriate prescribing in the elderly patientsJ Korean Med Assoc20095219199
- AnonymousPractice guideline for major depressive disorder in adultsAm J Psychiatry19931504 Suppl1268465906
- TungarazaTEFarroqSClozapine prescribing in the UK: views and experience of consultant psychiatristsTher Adv Psychopharmacol201552889626240748
- RothschildAJChallenges in the treatment of major depressive disorder with psychotic featuresSchizophr Bull201339478779623599251
- SpielmansGIThe promotion of olanzapine in primary care: an examination of internal industry documentsSoc Sci Med20092769142019481322
- SpielmansGIParryPIFrom evidence-based medicine to marketing-based medicine: evidence from internal industry documentsJ Bioethical Inq201071329
- SpielsmanIGAtypical antipsychotics: overrated and overprescribedPharm J20152947851
- ElaineHJohnWMetabolic screening after the American diabetes association’s consensus statement on antipsychotic drugs and diabetesDiabetes Care2009321037104219244091
- ReviewCEFirst- and second-generation antipsychotics for children and young adultsComp Eff Rev201239
- LeuchtSCorvesCArbterDEngelRRLiCDavisJMSecond-generation versus first-generation antipsychotic drugs for schizophrenia: a meta-analysisLancet20093739657314119058842
- McCreaRLNazarethIEvansSJWLithium prescribing during pregnancy: a UK primary care database studyPLoS One201510318
- WinserKLLeckman-WestinEFinnertyMEssockSMValproate prescription prevalence among women of childbearing agePsychiatr Serv201162221822021285103
- GroverSAvasthiAMood stabilizers in pregnancy and lactationIndian J Psychiatry201557S308S323 Available from: http://search.ebscohost.com/login.aspx?direct=true&db=edb&AN=108714121&site=eds-liveAccessed December 31, 201526330649
- AdedinsewoDAThurmanDJLuoY-HWilliamsonRSOdewoleOAOakleyGPJrValproate prescriptions for nonepilepsy disorders in reproductive-age womenBirth Defects Res A Clin Mol Teratol201397640340823733498
- ArkiloDVaouEOAntiepileptic drug use during pregnancy: sodium valproate is associated with lower offspring IQEvid Based Nurs201518410925736074
- SinghSValproate use during pregnancy was linked to autism spectrum disorder and childhood autism in offspringAnn Intern Med20131594JC1324026277
- GareriPSegura-GarcíaCManfrediVGLUse of atypical antipsychotics in the elderly: a clinical reviewClin Interv Aging201491363137325170260
- FayekMFlowersCSignorelliDSimpsonGPsychopharmacology: underuse of evidence-based treatments in psychiatryPsychiatr Serv200354111453145414600298
- HodgeKJespersenSSide-effects and treatment with clozapine: a comparison between the views of consumers and their cliniciansInt J Ment Health Nurs20081712818211398
- Al-SabaieASAbdul-RahimFAOniGAHawariRAThe use of sedative-hypnotic drugs in a university hospital in Saudi ArabiaAnn Saudi Med199414537938217586949
- YathamLNKennedySHParikhSVCanadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) collaborative update of CANMAT guidelines for the management of patients with bipolar disorder: update 2013Bipolar Disord201315114423237061
- Association APAmerican Psychiatric Association Practice Guidelines for the Treatment of Psychiatric Disorders: Compendium 2006Arlington, VAAmerican Psychiatric Association2006
- TaylorDPatonCKapurSThe Maudsley Prescribing Guidelines in PsychiatryPortsmouthJohn Wiley & Sons2015
