Abstract
Background
Uncertainty exists regarding the prevalence and clinical features associated with the practice of polypharmacy in bipolar disorder (BD), warranting a systematic review on the matter.
Methods
Three authors independently searched major electronic databases from inception till September 2015. Articles were included that reported either qualitative or quantitative data about the prevalence and clinical features associated with polypharmacy in adult cases of BD.
Results
The operative definitions of polypharmacy adopted across varying studies varied, with concomitant use of two or more psychotropic medications or use of four or more psychotropic medications at once being the most common and the most reliable, respectively. Regardless of type or current mood episode polarity of BD, prevalence rates up to 85% and 36% were found using the most permissive (two or more medications at once) and the most conservative (four or more) operative definitions for polypharmacy, respectively. Point prevalence prescription rates of one or more antidepressant or antipsychotic as part of a polypharmacy regimen occurred in up to 45% or 80% of the cases, respectively, according to the most permissive definition of polypharmacy. In contrast, lithium prescription rates ranged from 13% to 33% in BD patients receiving polypharmacy according to conservative and permissive definitions, possibly suggesting a reduced need for augmentation of combination strategies for those cases of BD with a favorable lifetime lithium response and/or long-lasting treatment as well as less likelihood of lithium response over the time most severe cases possibly exposed to a more complex polypharmacy overall.
Limitations
“Apples and oranges” bias; publication bias for most recently introduced compounds.
Conclusion
Polypharmacy is common among people with BD across varying type and mood episode phases of illness. Special population, including BD patients at high risk of familial load for suicidal behavior, solicit further research as well as the plausible “protective” role of lithium toward polypharmacy in BD. The PROSPERO registration number is CRD42014015084.
Introduction
Bipolar patients include an eclectic mix of ages and diagnostic categories across varying states of health, often receiving complex and long-lasting pharmacological interventions. In a community study, up to 9% of psychiatric patients received polypharmacy.Citation1 These rates increase to 13% in general population and an alluring 90% in general psychiatric settings.Citation2 Polypharmacy point prevalence rates up to 40% (according to the definition of three or more medications at once) or 18% (in case of four or more concomitant medications) have been reported for bipolar disorder (BD) cases suffering from long-lasting and/or treatment-resistant depression and receiving antidepressant drugs.Citation3 Furthermore, most of the available information about psychiatric medications comes from drug development programs that lead to registration and marketing. These programs almost invariably study the new drug in isolation vs either placebo or a comparator agent.Citation4 Experience with any new psychiatric medication in combination with another intervention is therefore virtually limited to a few short-term drug–drug interaction studies that are usually conducted in carefully screened young healthy volunteers.Citation5 Nevertheless, the practice of polypharmacy in BD represents the rule rather than the exception in the clinical setting, regardless of the current polarity of mood episode.Citation3,Citation6–Citation8 A number of reasons endorse the clinical practice of polypharmacy, with failure to achieve remission being the most common one.Citation9 This reflects the findings from the most comprehensive “real-world” pharmacological trial on BD patients to date, the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD),Citation10 in which up to 42% of the symptomatic patients included at baseline did not achieve recovery within 2 years of follow-up, despite expert pharmacotherapy and psychotherapy.Citation11 Aimed at shedding light on the matter, a set of 12 useful criteria has been proposed for a rational polypharmacy, essentially focusing on pharmacokinetic and pharmacodynamics issues,Citation5 as previously done by other authors comparing different phases of BD.Citation12 Yet, it has not been investigated which bipolar patients were most exposed to polypharmacy. There is clinically sound predictive value for a past history of treatment. This is seen in cases that include resistant bipolar depression, sub- or full-threshold mixed features, rapid-cycling course, or affective temperaments (especially cyclothymic one). They represent a few potential clinical moderators of “hard-to-catch” issues for standard treatment of guidelines for BD.Citation13,Citation14 Standard treatment guidelines on BD pose little or no attention overall toward the matter of polypharmacy, especially in relationship to the past history of treatment, which includes resistant bipolar depression, sub- or full-threshold-mixed features, rapid-cycling course, or affective temperaments (especially cyclothymic one), despite their clinically sound predictive value overall.Citation13,Citation14 Both evidence in support ofCitation4,Citation15,Citation16 and in dispute againstCitation17–Citation19 the practice of polypharmacy have been advocated to date. However, data about the actual prevalence and clinical correlates of the practice beyond the essential pharmacological and neurobiological premises are limited.
Therefore, we conducted a systematic review to assess the prevalence rates and clinical correlates across varying definitions of polypharmacy and varying mood phases of adulthood BD.
Materials and methods
This systematic review adhered to the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) (http://www.prisma-statement.org/)Citation20 following a registered publically available protocol (PROSPERO number: CRD42014015084).
Eligibility criteria
We limited our search to those records including adult subjects with BD, published in peer-reviewed journals. Limits activated were species: humans, language: English, and all adult: 19+, with no publication date restriction.
Information sources and search strategy
Sources of information included the following databases last accessed on September 11, 2015: PubMed/MEDLINE, Scopus, PsycINFO, EMBASE, Cochrane library, and Google Scholar. Contact with study authors was planned in advance whenever needed. The following keywords or their combination were used in the search strategy: “Bipolar Disorder” AND “polypharmacy” either in the title or in the abstract (or in the keywords, if allowed to be specified). Therefore, the adopted PubMed string was “Bipolar Disorder AND polypharmacy” (any field). Finally, the terms “polypharmacy,” “polypharmacotherapy,” “polypharmacology,” “polytherapy,” and “copharmacy” were used interchangeably across multiple databases.
Study selection
Included papers were those reporting epidemiological data about the prevalence and clinical features associated with polypharmacy in course of BD, with no restriction on etiology, bipolar type, specifiers/features, phase of illness or pharmacological and/or nonpharmacological treatment, class, dose, or duration of the pharmacological trials. Papers covering cases of polypharmacy in BD comorbid with additional disorders (either psychiatric or medical disorders/diseases) were also accounted whenever available. When a title and/or an abstract appeared suggestive for inclusion, the full-text reprint was obtained and examined to assess its relevance according to our inclusion/exclusion criteria. Excluded papers were case reports, oral communications, papers not including BD cases (multidiagnostic samples were nonetheless allowed) receiving multiple psychopharmacological treatments at once (any indication), those merely focusing on neurobiological, genetic, or pharmacological aspects of either BD or polypharmacy, those including (only) children or adolescents, or without an accurate description of the operative constructs of polypharmacy.
Data collection process
Three authors (MF, BS, and DV) conducted a two-step literature search, examining all titles and abstracts, accessing the full texts of potentially relevant papers. On data collection and extraction, the appointed authors compared their own results with each other to reach a final consensus based on consensual inclusion and exclusion criteria. Any possible discrepancy between the principal investigators, blind to each other, was solved by consultation with three reviewing authors (ASK, DDB, and GP). Both autosearch and hand search for “type I” (duplicates among/across different databases) and “type II” (duplicate publications in different Journals/issues)Citation21 were performed using Thomson Reuters EndNote X7™ for Microsoft Windows™. Data were screened for the following characteristics: Participants, Interventions, Comparisons, Outcomes, and Study Design (PICOS) as well as funding sources. Specifically, the recorded variables for each article included in the review were author(s), year publication, study design, sample size, eventual follow-up or control group, sociodemographic status, concurrent psychotherapy or history of physical treatment for BD, outcome measures, conclusions, limitations, quality score, and quality differentiation.
Risk of bias in individual studies
Potential major confounding biases in the studies have been ascertained at study level focusing on the following: measurement/diagnostic bias (especially inconsistent/unreliable definitions of polypharmacy and/or lack of reliable diagnostic tools to make the diagnosis of BD), confounding bias (eg, lack of stratification and multivariate control for specific sociodemographic, vital, or clinical features), information (especially recall) bias, unrepresentativeness or inhomogeneity of the sample size or lack of control group, and selection by indication bias (nonrandom assignment of the exposure where applicable).Citation22
Summary measures
Summary measures were risk ratio for cohort studies, odds ratio (OR) for case–control studies, or difference in mean values. Cohen’s d effect sizes were reported, whenever available or anyway ascertainable.
Scoring and ranking of the studies
The assessed studies were rated for quality using the following eligibility criteria: 1) representativeness of the sample (0–1 point); 2) presence of BD patients only in the sample (0–2 points); 3) a priori study design with the goal of evaluating the epidemiology of polypharmacy in BD (0–2 points); 4) extension of the follow-up (longitudinal studies)/clinical records (retrospective studies) >1 year (0–2 points); 5) validation of the clinical diagnosis and definition of polypharmacy and the used treatment (if applicable) (0–2 points); 6) inclusion and control of all the available variables for potential confounders/effect modifiers that may had influenced outcome (if applicable) (0–2 points); 7) reliability of the information gathered for the identification of BD cases/recall bias (0–2 points); 8) accuracy of the study was to discern between manic, hypomanic, mixed, and depressive episodes in BD (0–2 points); and 9) appropriateness of the number of comorbid cases reported as results/sample size (0–2 points). Quality rating had 17 as the maximum score.
Studies were also differentiated in the following way: 1) good quality: most or all criteria being fulfilled, and even when they were not met, the study conclusions were thought to be very unlikely to alter (range: 10–17 points); 2) moderate quality: some criteria being fulfilled, and when they were not met, the study conclusions were thought to be unlikely to alter (range: 6–9 points); and 3) poor quality: few criteria fulfilled but the conclusions of the study were thought to be very likely to alter (range: 0–5 points).
Main clinical features at study
Among others, the following effect moderators were accounted for in the analysis: 1) illness duration; 2) ethnicity (in order to explore whether ethnic minorities may receive different care); 3) any kind of socioeconomic measure or a proxy for that, for example, education status; 4) a baseline psychiatric symptoms/general functioning score; 5) physical comorbidity; 6) psychiatric comorbidity; 7) differences in setting; 8) year of data collection (to reflect the time frame of introduction of different drugs, especially atypical antipsychotics); 9) geographical region; and 10) study design and duration of follow-up (taking into account that cross-sectional studies and those with shorter follow-up may have higher rates of polypharmacy, as it could be either part of cross-titration or transient).
Risk of bias across the studies
Any eventual bias affecting cumulative evidence (eg, publication bias, selective reporting within studies) was assessed through the study evaluation process and accounted in the discussion of the present manuscript.
Results
Study selection
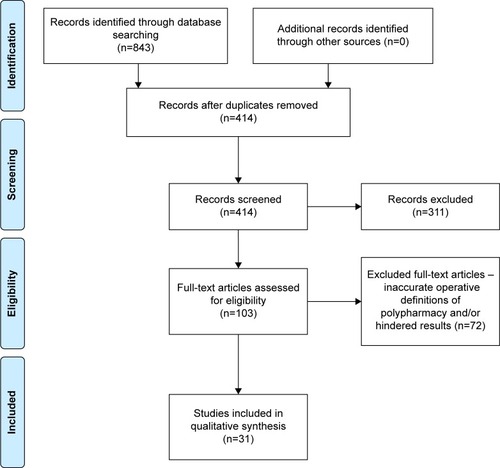
The search in PubMed generated 112 papers and 320 results in Scopus. Four hundred eleven additional results were obtained through search in Cochrane (n=7), PsycINFO (n=1), EMBASE (n=361), or Google Scholar (n=19 – including six edited books – out of 8,070 results initially obtained before limiting the Google Scholar search strategy to title and abstract, excluding patents or citations). Manual search allowed the identification of 23 additional results. Overall, the combined search strategy yielded a total of 843 results, of which 414 were removed after screening because they duplicated other articles. Three hundred eleven results were further screened; of those latter, 72 were excluded because they were not fully meeting the planned inclusion criteria (with a special reference to the operative definition of polypharmacy and the number of bipolar patients included). Therefore, 31 original studies were included in our qualitative analysis.Citation3,Citation23–Citation51 provides a synthetic flowchart of the multistep selection procedure. Overall, the combined search strategy yielded 843 results. Following screening for duplication, 414 articles were selected. On further evaluation, 311 studies were eliminated leaving 103 full-text articles. In all, 72 such articles were then excluded as they did not meet the planned inclusion criteria (especially, the operative definition of polypharmacy and the number of bipolar patients were included). Therefore, 31 original studies were included in our qualitative analysis.Citation3,Citation23–Citation51 provides a synthetic flowchart of a multistep selection procedure.
Quality score and quality differentiation results
Based on the quality differentiation, original studies were ranked as follows: poor (n=7, mean total score =3.5), moderate (n=13, mean total score =8.2), or good quality (n=11, mean total score =12.8). Additional details about pivotal cross-sectional, retrospective, and longitudinal studies have been outlined in –, respectively.
Table 1 Essential cross-sectional evidence
Table 2 Essential retrospective studies
Table 3 Essential prospective studies
Conceptual and operative definitions of polypharmacy across selected studies
Polypharmacy has been defined in at least 24 distinct conceptual ways, with “medication nonmatching a diagnosis” being the most commonly adopted conceptual definition,Citation52 capturing what could be both inappropriate therapy, that is, too many medications, and “evidence-based therapy that is inappropriate.”Citation53 The operative definitions of polypharmacy are also elusive and/or too broad,Citation54–Citation56 with the most commonly used definitions of psychiatric polypharmacy being the “use of two or more psychiatric medications in the same patient,”Citation2,Citation55 rather than “use of two or more medications of the same class or equivalent pharmacologic action to treat the same condition [BD].”Citation57 Nonetheless, “current use of four more psychotropic medications at once” was the most reliable operative definition for “complex polypharmacy” across the most pivotal studies.Citation3,Citation23,Citation27,Citation40,Citation42
Prevalence rates of polypharmacy in BD
A post hocCitation3 report based on the baseline data of the STEP-BD studyCitation10 indicated that only 12% of the patients (n=472 out 4,035) were taking none of the accounted medication at study entry, in contrast to 839 (21%) taking one vs 1,130 (28%) receiving two medications vs 883(22%) on three vs 711 (18%) taking four or more medications (complex polypharmacy). Of 2,159 females (53.5% of the total sample), 21% of whom (n=446) were received complex polypharmacy. With respect to the diagnostic type of BD, 2,666 patients were BD-I, of whom, 510 received complex polypharmacy, 2,156 received less than four medications; 1,084 were BD-II (complex polypharmacy, n=171 vs 913 not receiving complex polypharmacy); and 285 BD-not otherwise specified (NOS) cases, of whom just 30 received complex polypharmacy vs 255 who did not.
The operative definition of complex polypharmacy adopted for the STEP-BD post hocCitation3 was modified by independent authors conducting a chart-review study on 230 BD-I patients (of whom, 134 or 58% females) admitted to an inpatient or partial hospitalization, herein encompassing all classes of psychotropic and nonpsychotropic medications in order to better reflect routine clinical prescriptions for BD patients.Citation27 In all, 186 of the cases (81% of the total sample) received complex polypharmacy, while 122 (53%) reported taking medication for nonpsychiatric purposes. Polarity of mood episode on admission was as follows: depressed, n=85 (37%); manic, n=96 (42%); mixed state, n=44 (19%); and unspecified, n=5 (2%). Among those treated with pharmacotherapy for BD, patients reported taking an average of 3.31±1.46 psychotropic medications at the time of hospitalization. Average total medication usage (including both psychotropic and nonpsychotropic medications) was 5.94±3.78. One hundred twenty-six cases (55% of the sample) reported taking three or more psychotropic medications at the time of hospitalization, and 82 cases (36%) of the study met the operational criteria for complex polypharmacy. This figure represents 44% of those receiving any pharmacotherapy for BD at the time of hospital admission. Overall, even after accounting for 20% of patients who were not engaged in any pharmacologic treatment prior to hospitalization, 55% were on three or more psychotropic medications at the time of hospital admission and 36% were on four or more. The latter figure is exactly double than the rate reported from the outpatient STEP-BD sample,Citation3 although more consistent with rates of polypharmacy reported in voluntary BD registries.Citation41 Concordant with previous reports,Citation58,Citation59 additional analyses carried out by Weinstock et alCitation27 revealed that the average number of prescriptions almost doubled (from 3.3 to 5.9) when both psychotropic and nonpsychotropic medications were taken into account. The authors themselves also acknowledged that the discrepancy seen with respect to the STEP-BD post hoc reportCitation3 may be attributable to different operational criteria for complex polypharmacy, differential settings, and proportion of BD-I cases.
Data from the Arzneimittelüberwachung in der Psychiatrie (AMSP) European drug surveillance programCitation60,Citation61 involving 2,246 cases of bipolar depression followed over a 16-year period (1994–2009)Citation25 just relied on a “permissive” operative definition of polypharmacy, namely the use of two or more class of psychotropic substances. The prevalence rates of polypharmacy in European patients were therefore strikingly high, with almost 85% of the cases receiving polypharmacy in contrast to only 337 cases (or 15% of the total) receiving monotherapy (herein defined as the use of antidepressants or antipsychotics or anticonvulsants or lithium, including within-class prescriptions). Data about the practice of complex polypharmacy in European cases experiencing a current bipolar depressive episode were nonetheless made available by a 2012 report based on 2,231 inpatients (unspecified subtypes proportions) followed up in the context of the AMSP program between 1994 and 2009, which documented 137 patients (6.4% of the total) treated with at least four different psychotropic drugs at once, with rates steadily increasing, especially after year 2006.Citation33 Data about the practice of polypharmacy in Eastern European and Middle East patients just rely on post hoc cross-sectional analysis of the baseline records of a large (n=894) prospective study carried on manic patients prescribed with olanzapine (n=569 or 63.64%) or not (n=325 or 36.35%). While these data reflect a special population at study, the rates of polypharmacy were nonetheless very high (n=719 or 80.4%), although the authors adopted a permissive criterion of two or more psychotropic drugs at once.Citation31 Slightly lower prevalence rates in manic patients were also documented in Taiwanese inpatients approximately assessed within the same period (years 2000–2007). Specifically, out of 5,449 BD patients, 5,155 (95%) were BD-I cases, of whom 2,923 (57%) presenting with a manic episode at the time of hospitalization, 1,076 (21%) with depressed episode, 768 (15%) mixed episode, and 370 (7%) unspecified episode. Between-class vs within-class polypharmacy (according to the permissive criterion of two or more psychotropic drugs at once) occurred in 3,853 (71%) vs 941 (17%) patients, respectively.Citation28
Prescription trends and main clinical features associated with polypharmacy in BD
Quality receiver–operating characteristics post hoc analysis of the baseline records of the STEP-BD studyCitation3 also revealed that BD subjects had a 64% risk for receiving complex polypharmacy if they had ever taken any second-generation antipsychotic (SGA) drug, had six or more lifetime depressive episodes, ever attempted suicide (complex polypharmacy cases, n=686, vs noncomplex polypharmacy cases, n=1,105; P≤0.0001; Cohen’s d=0.05), and had an annual income of US$75,000 or higher (complex polypharmacy cases, n=158, vs noncomplex polypharmacy cases, n=747; P= nonsignificant [ns]; d=0.00). In contrast, complex polypharmacy was least often associated with lithium (n=41 vs 225 receiving lithium but not complex polypharmacy; d=0.03), divalproex (251 vs 934 noncomplex polypharmacy cases; d=0.11), and carbamazepine (219 vs n=548 noncomplex polypharmacy cases; d=0.13), whereas complex polypharmacy was most often associated with SGA use (complex polypharmacy cases, n=482, vs noncomplex polypharmacy cases, n=780; d=0.74), with antidepressants (684 vs n=1,251 noncomplex polypharmacy cases; d=0.78 – which is actually the largest effect size reported by the authors in their analyses). Contrary to expectations, a history of psychosis (complex polypharmacy cases, n=96, vs noncomplex polypharmacy, n=309; P=0.001; d=0.02), age at onset (complex polypharmacy mean age =16.4±3.3 vs noncomplex polypharmacy mean age of onset of 16.2±3.6; P=ns; d=0.03), BD-I vs BD-II subtype (no contrasts, P-value or d value reported), prior to hospitalization (no contrasts, P-value or d value reported), current illness state (no contrasts, P-value or d value reported), and history of substance use disorder (SUD) (complex polypharmacy, n=84, vs noncomplex polypharmacy, n=461; P=ns; d=0.05) did not significantly alter the risk profiles for receiving complex regimens, although concerns about the chance of a Berkson’s bias could be raised in these regards. Accounting of additional psychotropic and nonpsychotropic medications beyond the sole, seven-core medications regarded by the STEP-BD study (namely lithium, divalproex, carbamazepine, lamotrigine, and other anticonvulsants without definitely established thymoleptic properties as topiramate, gabapentin; oxcarbazepine, as well as SGA or any antidepressant) allowed Weinstock et al to provide additional insights about the clinical correlates of complex polypharmacy in BD.Citation27 Overall, according to this latter report, those BD-I cases receiving complex polypharmacy were significantly more likely to be female, depressed, have a comorbid anxiety disorder, and have a history of suicide attempt. Conversely, those receiving complex polypharmacy were significantly less likely to be manic and present with active psychosis at the time of hospital admission. Noteworthy, given that medication decisions may be especially driven by mood episode polarity, the authors decided on a priori basis to treat mood episode polarity as a covariate in any multivariate analysis to evaluate the demographic and clinical factors associated with complex polypharmacy and patterns of specific medication use, over and above any shared variance with mood episode. Therefore, controlling for mood episode polarity, female sex, B (standard error [SE])=0.58 (0.29), χ2(1)=3.88, P=0.049, OR =1.78; anxiety disorder comorbidity, B (SE)=0.72(0.32), χ2(1)=5.18, P=0.023, OR =2.05; and history of suicide attempt, B (SE)=0.79(0.34), χ2(1)=5.60, P=0.018, OR =2.21 remained significant predictors of complex polypharmacy for BD-I, whereas psychosis did not, B (SE)=−0.50 (0.32), χ2(1)=2.40, P=0.121, OR =0.61. Each psychotropic medication class was significantly associated with increased likelihood of complex polypharmacy. With respect to pattern of medication use by mood episode polarity, there was no statistically significant difference between depressed and mixed polarity patients (all P=0.11–0.94). As such, the authors combined these latter groups for purposes of comparison against patients presenting with pure mania. Use of antidepressants was significantly higher in the depressed/mixed polarity patients in comparison to patients presenting with pure mania (45% vs 20%; χ2(1)=15.49, P<0.001). This pattern of effects held for the use of selective serotonin reuptake inhibitors (26% vs 12%; χ2(1)=7.64, P=0.006), serotonin norepinephrine reuptake inhibitors (10% vs 2%; χ2(1)=5.65, P=0.017), and all other antidepressants (19% vs 7%; χ2(1)=5.93, P=0.015). Use of benzodiazepines (BDZs) was also significantly higher in the depressed/mixed polarity patients vs those presenting with mania (47% vs 33%; χ2(1)=4.42, P=0.036), while use of all remaining medications (ie, lithium, anticonvulsants, antipsychotics, stimulants, and hypnotics) did not differ as a function of episode polarity (all P-values=0.08–0.90). In addition, corresponding information about the use of varying classes of antidepressants for European BD inpatients receiving polypharmacy (yet herein adopting a permissive criterion of two or more drugs within different classes at once) was provided by Haeberle et al in 2012.Citation25 Olanzapine plus fluoxetine combination was found to be prescribed only in very few patients, as it was the case for the norepinephrine dopamine reuptake inhibitor bupropion, also possibly due to different drug policies and approval dates compared to the USA, despite the SGA quetiapine was found to be the second most frequently prescribed adjunctive therapy for bipolar depression during the period covered by the study, years 2006–2009, whereas lithium was the less common drug used in combination with any other class of substance (n=741 or 33% of the cases).Citation25 Owing to evidence pointing out that less than one-third of BD patients in the USA and about half of those in Europe received monotherapy,Citation3,Citation62–Citation65 Bauer et al planned a long-term naturalistic study in which patients with BD self-recorded mood, sleep, and drugs taken daily over a period of ∼6 months with the ultimate aim to further characterize the drug treatment patterns in 450 BD cases. Of these latter BD cases, 272 were BD-I cases (60%), 157 BD-II (35%), and 17 BD-NOS cases (5%). Noteworthy, the study adopted a permissive operative criterion for polypharmacy defined as the use of two or more psychotropic drugs at once.Citation34 Drug load was measured using the methodology developed by the World Health Organization (WHO) based on a measure of equipotency known as the defined daily dose.Citation66 Overall, 315 or 70% of the cases resided in the USA; n=53 or 11.8% resided in Germany; n=45 or 10% resided in Canada; and 37 or 8.2% resided elsewhere. Enrolled patients returned a total of 99,895 days of data (mean 222.0 days), with the most frequently taken drugs being mood stabilizers and 353 patients (78.4% of the total) taking a stable drug combination for half of days or longer. The majority of patients were taking polypharmacy, including 75% of those with a stable combination. Only a small number of drugs were commonly taken within each medication class, but there were a large number of unique drug combinations: 52 by medication class and 231 by specific drugs. Eighty percentage of patients with a stable combination were taking three or less drugs daily, although no specific report was documented in relationship with polypharmacy and lifetime hospitalization. Two previous chart-review studies on 457 BD-I cases suggested a positive correlation between the total number of current psychotropic medications and the number of hospitalization for depressive episodes, though not with suicidal attempt, neither lithium nor carbamazepine use in case of hospitalization due to mania.Citation40,Citation41 Finally, while most cross-sectional and longitudinal studies on the relationship between polypharmacy and the clinical features and/or prescription trends primarily focused on symptomatic cases of BD, evidence focusing just on 80 euthymic patients documented that those subjects self-reporting normal mood over a period of 3 consecutive months or longer usually received a lower number of drugs compared to nonlasting cases of euthymia, though a “selection by indication bias” would be prompted out considering that those cases receiving polypharmacy may already include the most severe and possibly rapid-cycling course cases of BD.Citation42
Personality features associated with polypharmacy in BD
A retrospective chart review of 89 treatment-seeking BD outpatients (F:M =48:41) assessed by the means of the revised NEO Five Factor Personality InventoryCitation67 about five personality dimensions, including neuroticism (the tendency to experience negative affect), extraversion (a tendency toward energy, positive emotions, and stimulation-seeking), conscientiousness (a tendency toward self-discipline and dutiful behavior), openness to experience (sometimes described as intellectual curiosity), and agreeableness (a tendency to be cooperative and compassionate) took into account 41 commonly prescribed psychotropic medications grouped in six classes (mood stabilizers, antidepressants, dopamine blockers, anxiolytic/sedative hypnotics, stimulants, and other) splitting the samples based on mean psychotropic medication use as follows: for current psychotropic medications: ≤3= low vs ≥4= high and for lifetime medications: ≤10= low vs ≥11= high. The subgroup with low openness had significantly more current psychotropic medications (3.7±1.9) than patients in the higher distribution of openness scores (2.8±1.8, P<0.005). There was no other comparison that reached statistical significance for either current or lifetime medications. Nonetheless, the subgroup using 18 or more lifetime psychotropic medications had significantly lower extraversion (21.8±8.9 vs 25.4±7.6, P≤0.005) and lower conscientiousness (21.9±8.2 vs 27.9±8.2, P<0.001) than those reporting lifetime usage of fewer than controls. Remarkably, the authors did not examine whether the duration of exposure to an ineffective medication would be correlated to reluctance to discontinue the ineffective agent, so that at present, conclusive statement about the potential moderator effect of personality traits in BD as measured by the means of the NEO Five Factor Personality Inventory could not be drawn.
Polypharmacy in suicidal behavior bipolar patients
Although different studies also accounted for suicidal cases of BD, the only quantitative evidence specifically addressing this issue involved 169 BD outpatients (most of whom being BD-I cases, n=145 or 85.7%) and used a permissive criterion for polypharmacy (two or more psychotropic medications), which actually occurred in 142 (84%) of the cases in contrast to just 27 patients (16%) receiving monotherapy. Polypharmacy with three or more medications occurred in 31 (19%) of the cases. Overall, rapid-cycling course was seen in up to 26.9% of the cases, which is a quite high rate, especially taking into account that most of the suicidal behavior outpatients were BD-I rather than BD-II cases.
Antipsychotic drugs prescription rates and polypharmacy in BD
The evidence about the use of antipsychotic polypharmacy in BD is also scarce and prone to publication bias considering the relatively novel introduction of most SGA drugs or their latter approval for BD and/or popularity as off-label prescriptions for BD patients, which nonetheless increased over the time.Citation68 Also, different prescription trends for SGA vs first-generation antipsychotics (FGAs) may depend on the geographical setting and resource settings, as Eastern European BD inpatients were less frequently prescribed with SGAs in comparison to their Western counterpart, with a 2010 report documenting 23.8% of them receiving two antipsychotics vs 28.6% receiving “complex antipsychotic polypharmacy.”Citation48 Indeed, much larger samples of BD patients prescribed with antipsychotic polypharmacy were documented by North American studies. For example, retrospective data on multistate Medicaid population for years 1998–2003 regarded 8,489 BD patients (unspecified proportion of BD subtypes), of whom 623 (7.3%) took antipsychotic polypharmacy (one or more antipsychotic drug) for at least 60 consecutive months (accountable SGAs at the time were olanzapine, quetiapine, risperidone, and the atypical antipsychotic clozapine).Citation44 Additionally, cross-sectional information on antipsychotic polypharmacy based on 1998 data (accounted SGAs could be olanzapine, quetiapine, risperidone, or clozapine) about US inpatients with psychotic disorders, of whom 36 were diagnosed with BD (unspecified subtypes), documented equal rates of antipsychotic polypharmacy (two or more drugs), and antipsychotic monotherapy (n=18 or 50% each group). It also documented the association of short-term treatment with multiple antipsychotics to major increase in drug exposure, adverse events, and time in the hospital, with no apparent gain in clinical benefit.Citation46 An updated 2008 report by Centorrino et al still based on 2004 records of antipsychotic polypharmacy in US inpatients documented very high rates of polytherapy including one antipsychotic drug (80%) or two or more antipsychotics (23%) at once for at least 3 consecutive days in the BD subset of the sample wherein BD subjects formed (n=37 out of 305 or 12.13%). Yet again, no clear-cut stratification between FGA and SGA was documented for, across varying BD subsets.Citation45 Concerning the antipsychotic prescribing patterns in US outpatients, a chart review of 2003–2004 data using a permissive operative definition of two or more antipsychotics involving also BD cases (n=511, no stratification of results across different BD subtypes) documented antipsychotic polypharmacy prevalence rates of 10% (53 cases), with accounted SGAs being risperidone, olanzapine, and quetiapine, although once again results were not stratified distinguishing between FGA vs SGA prescription trends.Citation47
Polypharmacy in special BD populations
Little is known about the practice of polypharmacy among special population of BD, and virtually no data exist about any eventual difference in care based on ethnicity in non-US samples. Sometimes, rates have been documented in qualitative but not quantitative way, as it was the case of BD inpatients with SUD reported to receive both higher number and doses of both conventional mood stabilizers and SGAs compared to non-SUD lifetime comorbidity.Citation69 Only a handful of studies have nonetheless provided essential quantitative data for alternative special settings/population of BD. Our knowledge is relatively limited even with respect to the practice of polypharmacy in BD inmates. Two longitudinal 12-week studies by Kamath et al documented strikingly high prevalence rates for polypharmacy (use of three or more psychotropic medications at one) in 84% of the cases (out of a total sample of 40 BD-I or BD-II cases, equal ratios for males and females)Citation43 urging the need for standard medication algorithms to reduce the polypharmacy in the correctional setting, with a special reference to antidepressant and antipsychotic drugs.Citation70 Similarly, despite the acknowledgment that pharmacological treatments for BD have historically been associated with neurocognitive side effects, especially in elderly subjects or otherwise possibly cognitively vulnerable subjects who would be particularly sensitive to polypharmacy,Citation71,Citation72 very little is known about these subjects, including bipolar subjects with intellectual disabilities (IDs). A report on 101 BD patients (F/M, n=59/41) aged 60 and older (mean age: 68.9±7.8 years), of whom 57 (56%) BD-I and 44 (44%) BD-II cases, with an onset of first affective symptoms before age 50 in 75.6% cases, was nonetheless studied with respect to polypharmacy (two or more psychotropic medications), which was documented in 31.7% of the cases (n=32), with equal daily median number of psychotropic medications in both BD-I and BD-II cases (median =2; interquartile range =3). Interestingly enough, among other classes of psychotropic drugs, lithium was the most frequently prescribed one in BD-I and BD-II cases: 63.2% vs 43.1%, respectively.Citation49 Regrettably, evidence about the practice of polypharmacy in BD outpatients with ID is even less conclusive, with the only available quantitative reports on the matter failing to provide any accurate stratification of results beyond the generic statement of similar polypharmacy rates occurring in ID (n=59) and non-ID (n=16) cases (range: 24%–38%) based on the operative criterion of two or more drugs rates in the ID (n=59)Citation50 or relying on unrepresentative subsets of BD cases,Citation73 despite the widespread and controversial clinical use of polypharmacy even for BD subjects with ID.Citation74 Similarly, only one study about the practice of polypharmacy involving pregnant bipolar women could meet our inclusion criteria.Citation32 Complete retrospective data ∼115 pregnancies, 75 of whom were followed throughout gestation while 40 had data for one certain gestational period, based on the Medicaid database of 5,000 women coded according to the International Classification of Diseases, Ninth Revision within years 2002–2004 indicated that the mean number of medications taken during pregnancy for manic BD-I cases was three (range: 0–10; mode =3), whereas 26.8% of the pregnant women filled prescriptions for six to ten medications during their pregnancy. Surprisingly, no dose change was made for the prescribed medications to accommodate changing metabolism across pregnancy. The most frequently prescribed psychotropic medications were from the opiate family, most likely due to comorbid diagnoses (especially SUD). However, the effects of taking multiple medications on pregnancy outcome and fetal development were unknown.Citation32 These findings are nonetheless compelling, especially considering that according to the clinical records of 53 fertile women with different mental illnesses (including 24 BD cases), about one-third (n=8 or 36%) were taking more than one psychotropic medication within the first trimester of an unplanned pregnancy.Citation75
Polypharmacy and treatment adherence in BD
The association between polypharmacy (two or more psychotropic medications at once) and self-reported adherence with daily dose of mood stabilizer (lithium, valproate, lamotrigine, carbamazepine, or oxcarbazepine) was obtained by Bauer et alCitation35 for 312 BD patients (BD-I, n=198; BD-II =100; and BD-NOS =14) over a 6-month period, accounting for the mean daily number of psychotropic drugs, which was 3.1±1.6 (7.0±4.2 pills daily). No significant association was found between the daily number of medications and the daily number of pills, although the smaller the dosage of mood stabilizer taken, the higher the self-reported adherence to overall psychotropic prescriptions.Citation35 In order to further characterize the factors associated with irregularity of daily dosage of antidepressants in BD, Bauer et al gathered self-reported information about medication dosage and mood ratings from 144 BD patients (BD-I, n=67 or 47.2%; BD-II, n=65 or 45.8%; and BD-NOS, n=10 or 7%) who received treatment as usual (of whom, 111 were also taking a mood stabilizer).Citation51 Regularity was measured using the “approximate entropy” (ApnEn), which is the tendency that values within a time series and remains the same on incremental comparisons.Citation76 The authors documented that although the mean percentage of days with missing doses was only 18.6%, there was a wide range of regularity in the daily antidepressant dosage. Drug holiday and polypharmacy (namely the use of two or more psychotropic drugs) were also significantly associated with irregularity (P=0.005), as it was the case for “pill burden” (P=0.005), and depression (P=0.015). Neither the percentage of days missing doses nor the drug holidays were associated with any demographic or clinical factors in the sample at study, which predominantly included female cases over male ones (F:M, n=108:36 or 75% vs 25%). Interestingly enough, the authors concluded that irregularity in daily dosage may be more dependent on the individual rather than on a specific drug, despite there being no assessment of temperamental or personality traits of the involved patients over the 100-day follow-up period. Nonetheless, conclusive evidence about the association of treatment nonadherence and polypharmacy in BD remains elusive, as a 2008 report by Baldessarini et al indicated that prevalent lack of treatment at 1 year was associated with sustained mood-stabilizer adherence (subgroup, n=620), with those patients on lithium or lamotrigine being more often adherent than those prescribed with valproate, carbamazepine, or oxcarbazepine (nonadherent subgroup, n=1,577; uncertain cases were excluded in secondary analyses).
Polypharmacy rates and concordance with standard treatment guidelines in BD
Polypharmacy accounted for nonconcordance with varying different guidelines for the pharmacological management of BD as documented by a Korean chart review using the permissive operative criterion of two or more psychotropic medications at once.Citation29 The study included 1,447 BD patients, including 990 BD-I cases (of whom, n=480 being currently manic inpatients; n=113 being depressive inpatients; and n=397 being outpatients) and 457 BD-II patients (of whom, n=190 being depressive inpatients and n=267 being outpatients. The authors concluded that varying degree of concordance rates across different guidelines essentially depended on the structure of heterogeneous guidelines themselves. For example, the 2009 edition of the Canadian Network for Mood and Anxiety Treatments (CANMAT)Citation77 and 2010 of the Korean Algorithm for Bipolar Disorder (KMAP-BP) guidelines had identical initial strategy for mania. In the manic inpatient group, the initial treatment strategy for 317 (66.0%) of 480 patients was equally concordant with both these latter guidelines. Nonconcordant initial treatment strategies included SGA polypharmacy (22.1%), mood-stabilizer polytherapy (9.6%), and use of carbamazepine (1.9%) or typical antipsychotics (0.4%). Approximately half of concordant cases at the initial step had continued the same strategy for the entire treatment period (176 of 317, 55.5%). The concordance rate was lower for the next step in the treatment. The overall concordance rate with the CANMAT guidelines was 48.7% (234 of 480), and the concordance rate with the KMAP-BP guidelines was 43.8% (210 of 480). Mean duration to proceed to the next treatment step (adding or discontinuing medication) was ∼15 days. In addition, the CANMAT guidelines provide an algorithm among bipolar depression only for bipolar I disorder (n=113). In the depressive inpatient group, only 30 cases (26.5%) were concordant with the initial treatment strategy of the CANMAT guidelines. More than half of the subjects were treated with the combination treatment, which was not included in the first step of the CANMAT algorithm. The overall concordance rate with the CANMAT guidelines was only 18.6% (21 of 113). Most nonconcordant subjects started two or more different medications concomitantly. The concordant rate for bipolar depression with the initial strategy of the KMAP-BP guidelines was 63.4% (192 of 303), as KMAP-BP included mood stabilizer plus SGA as one of the first options for bipolar depression. Nonconcordant initial treatment strategies essentially regarded SGA polytherapy and multiple mood stabilizers at once. The overall concordance rate with the KMAP-BP guidelines was 46.9% (142 of 303). When compared the concordance rate with the 2006 edition of the American Psychiatric Association (APA) practice guidelinesCitation78 and the 2009 edition of the World Federation Societies for Biological Psychiatry (WFSBP) guidelines,Citation79 the overall concordance rates for mania were only 7.3% and 2.1%, respectively. The authors concluded that nonconcordance occurred mainly because lithium is not recommended as the first line because of its potentially slower onset of action, and monotherapy should always proceed in the WFSBP guidelines. Finally, concerning the treatment of acute depression, the concordance rate with the APA or WFSBP guidelines was much lower, that is, 5.6% with the APA guidelines and 11.9% with the WFSBP guidelines. This latter quantitative evidence is in line with Western reports, pointing out a major impact of polypharmacy in determining poor adherence toward standard prescription guidelines, especially in the case of antipsychotic polypharmacy in the inpatient and/or the inmate units.Citation36
Discussion
Study limitations and implications and premises
Most of the limitations of the present systematic review are intrinsically related to the potential biases hampering the validity of the included studies and should be taken into account in the interpretations of the overall results presented herein. For example, given that medication decisions may be especially driven by mood episode polarity (eg, antidepressants prescribed for a depressive vs a manic episode), the fact that a number of included studies did not punctually stratify their own results using mood episode polarity as covariate in any multivariate analysis of significant univariate effect (if ever carried) should be considered. The inconsistency of the operative definitions of polypharmacy invariably affects the generalizability of the quantitative and qualitative results too, even if we strived to stratify our own results accordingly. Specifically, the ORs and risk ratios of the given studies included in the present review may differ across different studied samples according to the operative definitions of polypharmacy, sex, history of suicide attempt, associated medical and/or psychiatric clinical correlates, and Cohen’s d effect sizes could be documented or extracted whenever possible only. Publication and measurement (namely “diagnostic shift”) biases should also be regarded. Indeed, most of the recently introduced SGA or novel antidepressant drugs could not be assessed by previous studies. In addition, little is known about specific regional or cultural settings despite the potential impact of either cultural or pharmacoeconomic issues on prescription trends across different high resource regions,Citation80,Citation81 although strikingly high prevalence rates of polypharmacy were documented even in nonhigh resource settings worldwide, especially when permissive operative criteria were adopted.Citation28,Citation31,Citation82 With respect to low-income and/or non-Western regions, even when such information was available, it often came from outdated or generic reports. For example, low rates of “affective psychosis” in contrast to “schizophrenia” cases were documented in Nigeria based on pharmacological treatment records dating back to the late 1970s.Citation83 Yet, much higher prevalence rates of “affective disorders” was documented in the same region by a more recent multidiagnostic study focusing on polypharmacy.Citation84 In this regard, we speculate that a diagnostic shift from schizophrenia to “affective disorders”, in the broader sense, thus encompassing BD too, may reflect either differential settings (in- vs outpatient facilities) or the diagnostic revisions occurred within the past decades.Citation81,Citation85,Citation86 These are additional crucial issues in the interpretation of cumulative evidence on polypharmacy “in BD” obtained from studies published within a large time frame beyond the sole “regional setting” variable. Finally, it is worth mentioning that while the stringent selection criteria adopted through this qualitative and quantitative review greatly reduced the number of contributes considered of adequate quality, this systematic selection ideally emphasized just the most rigorous and clinically relevant results on the topic, which is also a critical issue for the topic at issue considering the discrepancy exiting between real-world practice and the standard treatment guidelines on the matter.
Final remarks and implications for the clinical practice
[…] Doctors are men who prescribe medicines of which they know little, to cure diseases of which they know less, in human beings of whom they know nothing.
This much pessimistic quote was attributed to François-Marie Arouet (1694–1778), best known by his nom de plume Voltaire. It was corroborated by the position of his countryman Philippe Pinel (1745–1826), who “was one of those physicians who reacted most strongly against the abuses of polypharmacy [multiple medications]” as René Semelaigne wrote in 1888, a later-born psychiatrist whose family had memories of Pinel.Citation87 This still reflects the attitude of many of modern prescribers toward BD polypharmacy.
Indeed, since 19th century, the practice of polypharmacy for what it is nowadays considered BD has spread consistently worldwide. It has been documented a tenfold increase in percentage of patients receiving three or more psychotropic medications at discharge between 1974 and 1995,Citation88 with much higher rates virtually occurring within the past 2 decades due to the increasing availability of novel pharmacological compounds, including antidepressant and SGA drugs, in the absence of any novel “silver bullet” drug for BD after the introduction of lithium.Citation7,Citation89,Citation90
While a firm position either in support or against the practice of polypharmacy in BD is out of the scope (and the possibility) of the present evidence-based qualitative and quantitative synthesis, it is nonetheless worth noting that polypharmacy for BD is an extremely common scenario, often poorly, scientifically sound. Not all of the polypharmacy routine follow a pharmacological and/or diagnostic rationale or the standard guidelines, with the ultimate risk of further burden on the patents rather than additional benefit. Thus, it is mandatory that future replication studies will expand the current knowledge about the prevalence and the clinical features of polypharmacy testing the reliability and validity of different operative definitions, ideally focusing on selective clinically sound potential moderators currently precluding any reliable quantitative extraction on the matter beyond the qualitative synthesis provided by a systematic review, with a special emphasis toward affective temperaments, history of suicidal behavior, and/or rapid cycling and mixed features, especially considering that the ultimate goal in the management of BD should be paving the ground for long-term stability (thus regarding efficacy, tolerability, sustainability, and adherence issues) rather than merely focusing on the acute phase management.
Author contributions
MF conceived the study. BS and DV assisted in study procedures. DDB, ASK, GP, and AV contributed to manuscript drafting and interpretation of the results. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- PattenSBBeckCMajor depression and mental health care utilization in Canada: 1994 to 2000Can J Psychiatry200449530330915198466
- KukrejaSKalraGShahNShrivastavaAPolypharmacy in psychiatry: a reviewMens Sana Monogr2013111829923678240
- GoldbergJFBrooksJO3rdKuritaKDepressive illness burden associated with complex polypharmacy in patients with bipolar disorder: findings from the STEP-BDJ Clin Psychiatry200970215516219210946
- ZarateCAJrQuirozJACombination treatment in bipolar disorder: a review of controlled trialsBipolar Disord20035321722512780875
- PreskornSHLaceyRLPolypharmacy: when is it rational?J Psychiatr Pract20071329710517414685
- McInerneySJKennedySHReview of evidence for use of antidepressants in bipolar depressionPrim Care Companion CNS Disord2014165
- FornaroMMartinoMDe PasqualeCMoussaouiDThe argument of antidepressant drugs in the treatment of bipolar depression: mixed evidence or mixed states?Expert Opin Pharmacother201213142037205122946746
- El-MallakhRSGaoYJeannie RobertsRTardive dysphoria: the role of long term antidepressant use in-inducing chronic depressionMed Hypotheses201176676977321459521
- ZigmanDBlierPA framework to avoid irrational polypharmacy in psychiatryJ Psychopharmacol201226121507151122767374
- SachsGSThaseMEOttoMWRationale, design, and methods of the systematic treatment enhancement program for bipolar disorder (STEP-BD)Biol Psychiatry200353111028104212788248
- PerlisRHOstacherMJPatelJKPredictors of recurrence in bipolar disorder: primary outcomes from the systematic treatment enhancement program for bipolar disorder (STEP-BD)Am J Psychiatry2006163221722416449474
- LinDMokHYathamLNPolytherapy in bipolar disorderCNS Drugs2006201294216396522
- PerugiGFornaroMBipolar disorder treatment guidelines and their limits in every day clinical practiceGiorn Ital Psicopat2011173261264
- VietaETreatment guidelines for bipolar disorder: a bit unrealistic, but indispensableGiorn Ital Psicopat201016380388
- GhaemiSNPolypharmacy in PsychiatryAbingdonTaylor & Francis2002
- NiculescuAB3rdPolypharmacy in oligopopulations: what psychiatric genetics can teach biological psychiatryPsychiatr Genet200616624124417106426
- HealyDPsychiatric Drugs Explained5th edLondonElsevier2009
- ParisJThe Use and Misuse of Psychiatric Drugs: An Evidence-Based CritiqueHoboken, NJJohn Wiley & Sons2010
- GallegoJABonettiJZhangJKaneJMCorrellCUPrevalence and correlates of antipsychotic polypharmacy: a systematic review and meta-regression of global and regional trends from the 1970s to 2009Schizophr Res20121381182822534420
- MoherDLiberatiATetzlaffJAltmanDGPRISMA GroupPreferred reporting items for systematic reviews and meta-analyses: the PRISMA statementPLoS Med200967e100009719621072
- QiXYangMRenWFind duplicates among the PubMed, EMBASE, and Cochrane Library Databases in systematic reviewPLoS One201388e7183823977157
- McGauranNWieselerBKreisJSchülerYBKölschHKaiserTReporting bias in medical research – a narrative reviewTrials2010113720388211
- SachsGSPetersATSylviaLGrunzeHPolypharmacy and bipolar disorder: what’s personality got to do with it?Int J Neuropsychopharmacol20141771053106124067291
- HowlandRHPharmacotherapy of inpatients with bipolar depressionAnn Clin Psychiatry1997941992029511942
- HaeberleAGreilWRussmannSGrohmannRMono- and combination drug therapies in hospitalized patients with bipolar depression. Data from the European drug surveillance program AMSPBMC Psychiatry20121215322998655
- KupferDJFrankEGrochocinskiVJClussPAHouckPRStapfDADemographic and clinical characteristics of individuals in a bipolar disorder case registryJ Clin Psychiatry200263212012511874212
- WeinstockLMGaudianoBAEpstein-LubowGTezanosKCelis-DehoyosCEMillerIWMedication burden in bipolar disorder: a chart review of patients at psychiatric hospital admissionPsychiatry Res20142161243024534121
- HungGCYangSYChenYLinSKPsychotropic polypharmacy for the treatment of bipolar disorder in TaiwanPsychiatr Serv201465112512824382766
- BaekJHHaKYathamLNPattern of pharmacotherapy by episode types for patients with bipolar disorders and its concordance with treatment guidelinesJ Clin Psychopharmacol201434557758725006813
- MauerSAlahmariRVohringerPAInternational prescribing patterns for mood illness: the International Mood Network (IMN)J Affect Disord201416713613924955565
- OkashaTAKucukalicANasrAALonger-term treatment of patients with bipolar disorder: a 9-month observational study in Central and Eastern Europe, the Middle East and AfricaCurr Med Res Opin20092581889190019538106
- PeindlKSMasandPMannelliPNarasimhanMPatkarAPolypharmacy in pregnant women with major psychiatric illness: a pilot studyJ Psychiatr Pract200713638539218032983
- GreilWHaberleAHaueisPGrohmannRRussmannSPharmacotherapeutic trends in 2231 psychiatric inpatients with bipolar depression from the International AMSP Project between 1994 and 2009J Affect Disord2012136353454222134044
- BauerMGlennTAldaMDrug treatment patterns in bipolar disorder: analysis of long-term self-reported dataInt J Bipolar Disord20131525505672
- BauerMGlennTGrofPThe association between concurrent psychotropic medications and self-reported adherence with taking a mood stabilizer in bipolar disorderHum Psychopharmacol2010251475420033908
- HuffmanJCChangTEDurhamLEWeissAPAntipsychotic polytherapy on an inpatient psychiatric unit: how does clinical practice coincide with Joint Commission guidelines?Gen Hosp Psychiatry201133550150821762994
- GazalleFKHallalPCTramontinaJPolypharmacy and suicide attempts in bipolar disorderRev Bras Psiquiatr2007291353817435926
- CorrellCUFredericksonAMKaneJMManuPDoes antipsychotic polypharmacy increase the risk for metabolic syndrome?Schizophr Res2007891–39110017070017
- BaldessariniRJPerryRPikeJFactors associated with treatment nonadherence among US bipolar disorder patientsHum Psychopharmacol20082329510518058849
- LevineJChengappaKNBrarJSGershonSKupferDJIllness characteristics and their association with prescription patterns for bipolar I disorderBipolar Disord200131414911256463
- LevineJChengappaKNBrarJSPsychotropic drug prescription patterns among patients with bipolar I disorderBipolar Disord20002212013011252651
- AdliMWhybrowPCGrofPUse of polypharmacy and self-reported mood in outpatients with bipolar disorderInt J Psychiatry Clin Pract20059425125624930922
- KamathJTemporiniHQuartiSBest practices: disseminating best practices for bipolar disorder treatment in a correctional populationPsychiatr Serv201061986586720810582
- MorratoEHDoddSOderdaGHaxbyDGAllenRValuckRJPrevalence, utilization patterns, and predictors of antipsychotic polypharmacy: experience in a multistate Medicaid population, 1998–2003Clin Ther200729118319517379060
- CentorrinoFCincottaSLTalamoAHospital use of antipsychotic drugs: polytherapyCompr Psychiatry2008491656918063043
- CentorrinoFGorenJLHennenJSalvatorePKelleherJPBaldessariniRJMultiple versus single antipsychotic agents for hospitalized psychiatric patients: case-control study of risks versus benefitsAm J Psychiatry2004161470070615056517
- AparasuRRJanoEBhataraVConcomitant antipsychotic prescribing in US outpatient settingsRes Soc Adm Pharm200953234241
- JordanovaVMaricNPAlikajVPrescribing practices in psychiatric hospitals in Eastern EuropeEur Psychiatry201126741441820828993
- DolsARhebergenDBeekmanAKupkaRSajatovicMStekMLPsychiatric and medical comorbidities: results from a bipolar elderly cohort studyAm J Geriatr Psychiatry201422111066107424495405
- HurleyADFolsteinMLamNPatients with and without intellectual disability seeking outpatient psychiatric services: diagnoses and prescribing patternJ Intellect Disabil Res200347pt 1395012558694
- BauerRGlennTAldaMAntidepressant dosage taken by patients with bipolar disorder: factors associated with irregularityInt J Bipolar Disord201312625505689
- BushardtRLMasseyEBSimpsonTWAriailJCSimpsonKNPolypharmacy: misleading, but manageableClin Interv Aging20083238338918686760
- GilletteCPruntyLWolcottJBroedel-ZauggKA new lexicon for polypharmacy: implications for research, practice, and educationRes Social Adm Pharm201511346847125280463
- JorgensenTJohanssonSKennerfalkAWallanderMASvärdsuddKPrescription drug use, diagnoses, and healthcare utilization among the elderlyAnn Pharmacother20013591004100911573845
- LinjakumpuTHartikainenSKlaukkaTVeijolaJKiveläSLIsoahoRUse of medications and polypharmacy are increasing among the elderlyJ Clin Epidemiol200255880981712384196
- Lopez-Torres HidalgoJCerda DiazRFernandez OlanoCRequena GallegoMFernández CasalderreyCOtero PuimeAFactors associated with chronic drug consumption in the elderlyMed Clin199710815572576
- KingsburySJYiDSimpsonGMPsychopharmacology: rational and irrational polypharmacyPsychiatr Serv20015281033103611474046
- KrishnanKRPsychiatric and medical comorbidities of bipolar disorderPsychosom Med20056711815673617
- KupferDJThe increasing medical burden in bipolar disorderJAMA2005293202528253015914754
- EngelRRGrohmannRRutherEHippiusHResearch methods in drug surveillancePharmacopsychiatry200437suppl 1S12S1515052510
- GrohmannREngelRRRutherEHippiusHThe AMSP drug safety program: methods and global resultsPharmacopsychiatry200437suppl 1S4S1115052509
- AzorinJMAubrunEBertschJReedCGerardSLukasiewiczMMixed states vs pure mania in the French sample of the EMBLEM study: results at baseline and 24 months – European mania in bipolar longitudinal evaluation of medicationBMC Psychiatry200993319500417
- BaldessariniRHenkHSklarAChangJLeahyLPsychotropic medications for patients with bipolar disorder in the United States: polytherapy and adherencePsychiatr Serv200859101175118318832504
- HayesJPrahPNazarethIPrescribing trends in bipolar disorder: cohort study in the United Kingdom THIN primary care database 1995–2009PLoS One2011612e2872522163329
- QuanteAZeugmannSRegenFEngelhardtAAnghelescuIGPsychopharmacological treatment status in outpatients with bipolar disorder: a clinical survey in GermanyPsychiatry Investig201073155162
- WHOWHO Collaborating Centre for Drug Statistics Methodology ATC/DDD Index 2011GenevaWorld Health Organization2013
- BarnettJHHuangJPerlisRHPersonality and bipolar disorder: dissecting state and trait associations between mood and personalityPsychol Med20114181593160421134316
- CorrellCUDetrauxJDe LepeleireJDe HertMEffects of antipsychotics, antidepressants and mood stabilizers on risk for physical diseases in people with schizophrenia, depression and bipolar disorderWorld Psychiatry201514211913626043321
- VincentiAVentriglioABaldessariniRJTalamoAFitzmauriceGCentorrinoFCharacteristics and clinical changes during hospitalization in bipolar and psychotic disorder patients with versus without substance-use disordersPharmacopsychiatry201043622523220652858
- KamathJWakaiSZhangWKestenKSheltonDTrestmanRAdaptation of the Texas implementation medication algorithm for bipolar disorder in adult female offendersInt J Offender Ther Comp Criminol Epub2015331
- DautzenbergGLansLMeestersPDThe care needs of older patients with bipolar disorderAging Ment Health Epub2015651926046823
- DiasVVBalanza-MartinezVSoeiro-de-SouzaMGPharmacological approaches in bipolar disorders and the impact on cognition: a critical overviewActa Psychiatr Scand2012126531533122881296
- GuilletteLMHollisKLMarkarianALearning in a sedentary insect predator: antlions (Neuroptera: Myrmeleontidae) anticipate a long waitBehav Processes200980322423220522313
- FornaroMCiampaGMostiNDel CarloACeraudoGColicchioSA case of treatment resistant depression and alcohol abuse in a person with mental retardation: response to aripiprazole and fluvoxamine therapy upon consideration of a bipolar diathesis after repetitive failure to respond to multiple antidepressant trialsCase Report Med20102010801514
- DesaiSDPandyaRHStudy of psychiatric comorbidity in patients with headache using a short structured clinical interview in a rural neurology clinic in Western IndiaJ Neurosci Rural Pract20145suppl 1S39S4225540537
- PincusSMGladstoneIMEhrenkranzRAA regularity statistic for medical data analysisJ Clin Monit1991743353451744678
- YathamLNKennedySHSchafferACanadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) collaborative update of CANMAT guidelines for the management of patients with bipolar disorder: update 2009Bipolar Disord200911322525519419382
- APAAmerican Psychiatric Association Practice Guidelines for the Treatment of Psychiatric Disorders: Compendium 2006Arlington, VAAPA2006
- GrunzeHVietaEGoodwinGMThe World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the biological treatment of bipolar disorders: update 2009 on the treatment of acute maniaWorld J Biol Psychiatry20091028511619347775
- FornaroMClementiNFornaroPMedicine and psychiatry in Western culture: Ancient Greek myths and modern prejudicesAnn Gen Psychiatry200982119811642
- BrometEJKotovRFochtmannLJDiagnostic shifts during the decade following first admission for psychosisAm J Psychiatry2011168111186119421676994
- DeshmukhSAIsmailTSEvaluation of psychotropic drugs use pattern among out patients attending psychiatry department at Government Medical College and Hospital, Nagpur: a cross sectional studyInt J Pharm Bio Sci201233428436
- OdejideAOA study of the inpatient service of a Nigerian Psychiatric HospitalCompr Psychiatry19802143023077398254
- AdeponleABObembeAOAdeyemiSOSuleimanGTPolypharmacy in psychiatric out-patient practice in northern NigeriaAfr J Psychiatry2007104215218
- LakeCRSchizophrenia Is a Misdiagnosis: Implications for the DSM-5 and the ICD-11BerlinSpringer Science & Business Media2012
- ChenYRSwannACBurtDBStability of diagnosis in schizophreniaAm J Psychiatry199615356826868615415
- RenéSPhilippe Pinel et son Oeuvre Au Point de Vue de la Médecine MentaleLondonForgotten Books2013130131 Original work published 1890
- FryeMAKetterTALeverichGSThe increasing use of polypharmacotherapy for refractory mood disorders: 22 years of studyJ Clin Psychiatry200061191510695639
- FornaroMAgugliaEDell’OssoLPerugiGCould the underestimation of bipolarity obstruct the search for novel antidepressant drugs?Expert Opin Pharmacother201112182817283122098226
- BlierPThe well of novel antidepressants: running dryJ Psychiatry Neurosci201035421922020569647