Abstract
This study explores sex differences in the outcomes of patients with schizophrenia (clinical/functional remission and recovery) across diverse regions of the world (Northern Europe, Southern Europe, Central and Eastern Europe, Latin America, East Asia, and North Africa and the Middle East). Data (n=16,380 for this post hoc analysis) were taken from the World-Schizophrenia Health Outcomes Study. In most regions, females had a later age at first service contact for schizophrenia, a lower level of overall/negative symptom severity, lower rates of alcohol/substance abuse and paid employment, and higher percentages of having a spouse/partner and independent living. Overall, females had slightly higher rates of clinical remission (58.0% vs 51.8%), functional remission (22.8% vs 16.0%), and recovery (16.5% vs 16.0%) at 36 months (P<0.001 for all). This pattern was consistently observed in Southern Europe and Northern Europe even after controlling for baseline sex differences, but not in other regions. In Central and Eastern Europe, rates of clinical remission were higher in females at 36 months, but those of functional remission and recovery were similar between males and females. The opposite was observed for Latin America. In East Asia, sex differences were rarely observed for these outcomes. Finally, in North Africa and the Middle East, sex differences in these outcomes were pronounced only in regression analyses. These regional variations shed light on the importance of psychosocial and cultural factors and their effects on sex in the prognosis of schizophrenia.
Introduction
Schizophrenia is a debilitating psychiatric condition, affecting ~1% of both males and females during their lifetime.Citation1 However, a number of studies have suggested that females with schizophrenia generally have a more favorable course and outcome than males. They tend to have higher rates of response, remission, and recovery, lower rates of rehospitalization, shorter lengths of stay, longer time to relapse, and better social adjustment.Citation2–Citation9 Recent findings from the Worldwide-Schizophrenia Outpatient Health Outcomes (W-SOHO) study, the largest prospective observational study on the outcomes of schizophrenia conducted in 37 countries across diverse regions of the world, also highlight a better course and outcome in females.Citation5,Citation7 In addition, a US study on the course of schizophrenia and other psychotic disorders in 97 patients also reported better global outcomes such as improvement in psychotic activity and functioning in females than in males over a 20-year period.Citation4
Several biological, psychosocial, and cultural factors have been suggested to explain these sex differences. These include the following tendencies in females: 1) later onset of illness,Citation10–Citation13 2) fewer negative symptoms,Citation14–Citation19 3) a less severe form of illness,Citation20 4) better premorbid functioning,Citation21–Citation23 5) better social functioning or social acceptance,Citation24,Citation25 6) better response to antipsychotics,Citation13,Citation26 7) lower frequency of socially undesirable behavior such as substance abuse and noncompliance to treatment,Citation27,Citation28 and 8) the potential protective role of estrogen.Citation29
Nevertheless, there are also some studies that have reported no sex differences in the outcomes of schizophrenia.Citation30–Citation32 For instance, recent findings from the “cross-sectional” European Group on Functional Outcomes and Remission in Schizophrenia study conducted in 12 centers in Europe with 276 stabilized patients with schizophrenia, schizoaffective, or delusional disorder indicated no sex differences in the rate of symptomatic and functional remission, despite the fact that females had a later onset of the illness, less severe negative symptoms, and less frequent alcohol abuse than males.Citation31
Further research is needed to better understand the complex role of sex in the prognosis of schizophrenia. A cross-cultural comparison will be particularly important since it will enhance our understanding of the relative importance of biological and sociocultural factors on the sex differences in the outcomes of schizophrenia. We thus aimed to extend the earlier findings of the W-SOHO to assess whether a more favorable course of illness observed in females is stable across different regions of the world. The specific objectives of this study were twofold: 1) to describe baseline clinical characteristics of both males and females in each of the six regions studied (Northern Europe, Southern Europe, Central and Eastern Europe, Latin America, East Asia, and North Africa and the Middle East), and 2) to explore whether males and females have a similar disease course over a 3-year period in terms of clinical remission, functional remission, and recovery across the regions.
Methods
Study design and patient sample
The Schizophrenia Outpatient Health Outcomes (SOHO) study was a 3-year, international, prospective, observational study on the outcomes of treatment with antipsychotics for schizophrenia. SOHO was conducted in ten Western European countriesCitation33 as well as in 27 countries across four continents as the Intercontinental SOHO.Citation34 Data from all 37 participating countries have been pooled to produce the W-SOHO dataset. A total of 17,384 patients were included in the W-SOHO dataset; the details of the study are available elsewhere.Citation35 This study followed the ethical standards of responsible local committees and regulations from the participating countries and was conducted in accordance with the ethical principles of the Declaration of Helsinki. This analysis was approved by the Ethics Committee of Fundació Sant Joan de Déu. Ethical Review Board approval was also obtained from the participating 27 countries wherever required by local law for observational studies. All patients provided either verbal or written informed consent for the provision and collection of data during the observational period.
Participating psychiatrists offered enrollment to adult patients (at least 18 years of age) initiating or changing antipsychotic medication for the treatment of schizophrenia, who presented within the normal course of care in the outpatient setting. The diagnosis of schizophrenia was made by the participating psychiatrists using standard diagnostic criteria (Diagnostic and Statistical Manual of Mental Disorders, fourth edition,Citation36 or International Classification of Diseases, tenth edition).Citation37
As the initial objective of SOHO was to compare the outcomes of patients starting olanzapine with other antipsychotics, the study was designed to provide two patient cohorts of approximately equal size: patients starting olanzapine, and those starting any other antipsychotic. Importantly, the antipsychotic treatment prescribed to each patient was wholly based on the opinion of the treating psychiatrist; patients were asked to participate in the study after they had received their medication prescription. In addition, changes in medication, dosing, and concomitant medication were possible at any time during follow-up as determined by the treating psychiatrist.
Data collection
Data collection for the study occurred during routine outpatient visits and was targeted for baseline, 3 months, and 6 months post baseline, and every 6 months thereafter.
Clinical severity was assessed by the treating psychiatrists at each visit using a scale based on the Clinical Global Impressions Severity Scale – Schizophrenia version (CGI-SCH),Citation38 which evaluates symptom severity across positive, negative, depressive, and cognitive subdomains as well as overall symptoms from 1 (normal, not ill) to 7 (extremely ill).
Other information collected at baseline or at follow-up visits include key demographic characteristics (eg, age, age at first contact, sex, and region), functional status (eg, relationships, housing conditions, work status, and social activities), clinical status (eg, weights [kg], alcohol/substance abuse/dependency, and suicide attempts), antipsychotic medication (drug name, formulation, dosage, and reasons for medication change if applicable), concomitant medication (anticholinergics, antidepressants, anxiolytics/hypnotics, and mood stabilizers), adverse events (eg, extrapyramidal symptoms, tardive dyskinesia, sexual dysfunction), quality of life, and health service use (eg, hospitalization, day care visits, and outpatient visits).
Regional classification and definition of outcomes
Regional classification
The 37 countries participating in the W-SOHO study were grouped into six regions as follows: Northern Europe (Denmark, France, Germany, Ireland, the Netherlands, and the UK); Southern Europe (Greece, Italy, Portugal, Spain, and Israel [Israel was included in the Southern Europe group based on ethnicity, economic and health care systems]); Central and Eastern Europe (Czech Republic, Hungary, Lithuania, Poland, Romania, Russia, Slovakia, and Slovenia); Latin America (Argentina, Chile, Colombia, Costa Rica, El Salvador, Guatemala, Honduras, Mexico, Peru, Puerto Rico, and Venezuela); East Asia (Korea, Malaysia, and Taiwan); and North Africa and the Middle East (Algeria, Egypt, Saudi Arabia, and Turkey).
Definition of clinical remission
Clinical remission was defined as achieving a score of 3 (mild severity) or less on the CGI-SCH overall severity score, the CGI-SCH positive symptoms score, the CGI-SCH negative symptoms score, and the CGI-SCH cognitive symptoms score for a period of 6 months or more (ie, at least two consecutive visits).Citation39 In addition, the patient should not have been hospitalized during the period. Given that two consecutive visits were considered, clinical remission was defined from the 12-month visit. This definition of clinical remission was based on the Andreasen criteria,Citation40 as presented and validated in a previous report from the SOHO study.Citation39
Definition of functional remission
Functional remission was defined from the 12-month visit as having good social functioning for a period of 6 months or more (ie, at least two consecutive visits). Good social functioning included those patients who had 1) a positive occupational/vocational status, ie, paid or unpaid full- or part-time employment, being a currently registered university student, or a housewife; 2) independent living; and 3) active social interactions, ie, having more than one social contact during the last 4 weeks or having a spouse or partner.
Definition of recovery
Recovery was defined from the 18-month visit as achieving functional remission at both current and previous visits (ie, two consecutive visits) and clinical remission at the current visit.
Statistical analysis
A total of 16,497 patients were prescribed antipsychotic monotherapy at baseline. Of these, 16,380 patients who had non-missing data for sex (male for female) were included in the current analysis. Approximately two-thirds (n=10,697; 65.3%) of these patients were available at the end of the study (65.0% in Northern Europe, 73.2% in Southern Europe, 73.6% in Central and Eastern Europe, 58.7% in Latin America, 39.9% in East Asia, and 53.0% in North Africa and the Middle East at 36 months).
Baseline characteristics of the study sample were described for each sex in each of the six regions. Differences in baseline characteristics between males and females in each region were compared using chi-square tests for categorical variables and Wilcoxon two-sample tests for continuous variables.
Rates of clinical remission, functional remission, and recovery were also described and compared between the sexes at follow-up visits in each of the six regions, using chi-square tests. In addition, generalized estimating equations with a logit link were used to examine the impact of sex on these outcomes, controlling for the following baseline variables: CGI-SCH overall scores, age at first service contact for schizophrenia, duration of illness, current alcohol or substance abuse, hospitalization in the 6 months prior to baseline, independent living at baseline, having a spouse or partner at baseline, being socially active in the 4 weeks prior to baseline, having paid employment at baseline, and visits. The unstructured covariance pattern was used to take into account the within-patient correlation.
All statistical analyses were performed using the SAS software (version 9.3), using PROC GENMOD for binomial outcome variables (SAS Institute Inc., Cary, NC, USA).
Results
Sex differences in the baseline patient characteristics across different regions
A total of 16,380 patients were included in the current analysis. The number of patients (female percentages) in each of the six regions was n=4,086 for Northern Europe (46.6%), n=5,585 for Southern Europe (38.9%), n=2,024 for Central and Eastern Europe (52.3%), n=2,396 for Latin America (41.5%), n=1,179 for East Asia (50.3%), and n=1,110 for North Africa and the Middle East (36.9%).
summarizes the baseline characteristics of the study sample by sex in each of the six regions. There were some differences in patient characteristics between the sexes as well as between the regions. The pattern of sex differences was, however, generally similar across the regions, except for North Africa and the Middle East. For example, the mean age at first service contact for schizophrenia was 2–4 years later in females in all regions except North Africa and the Middle East, where both males and females had their first service contact at similar mean ages (26.7 [standard deviation, SD =9.3] for females and 25.9 [SD =8.1] for males, P=0.412). Clinical symptom severity at baseline, as measured with the CGI-SCH overall scores, was also lower in females in most regions, but similar between males and females in North Africa and the Middle East (P=0.122) and in Latin America (P=0.750). Notably, the overall severity was highest in both sexes in North Africa and the Middle East (4.6 [SD =1.0] for both sexes). Moreover, positive symptom severity was also highest in this region, especially for females (mean CGI-SCH positive symptoms score: 4.5 [SD =1.3] for females and 4.2 [SD =1.4] for males, P=0.002). Nevertheless, the level of negative symptom severity was similar to that in other regions, and all regions including North Africa and the Middle East exhibited a lower level of negative symptom severity in females than in males. Meanwhile, depressive symptom severity was higher in females than in males in Northern Europe, Southern Europe, and Latin America, but similar between the two in other regions. There were no sex differences in cognitive symptom severity across all regions.
Table 1 Baseline patient characteristics by sex in each of the six regions
The percentage of current alcohol or substance abuse was also generally lower in females than in males across all regions. As for baseline functional status, a higher percentage of females than males had a spouse or partner and also lived independently in their own homes in all regions but North Africa and the Middle East; the opposite pattern was observed in this region albeit not statistically significant (29.0% for females and 33.4% for males for the former, P=0.145; 23.5% for females and 26.9% for males for the latter, P=0.208). However, the percentage being socially active was generally similar between the sexes across the regions except for Southern Europe, where a higher percentage of males than females were socially active (61.5% for females and 66.3% for males, P<0.001). The percentage in paid employment was also generally higher in males across the regions, especially in East Asia (13.0% for females and 20.2% for males, P<0.001) and North Africa and the Middle East (14.3% for females and 26.4% for males, P<0.001). Notably, the percentages for independent living and being socially active were generally higher for both males and females in Europe, especially in Northern Europe, compared with the other non-European regions.
Sex differences in rates of clinical remission, functional remission, and recovery across different regions
Overall, a higher percentage of females than males achieved clinical remission, functional remission, and recovery throughout the follow-up, although the differences were relatively small. More than half of both males and females achieved clinical remission at 36 months (58.0% vs 51.8%, P<0.001), and much fewer patients (in both sexes) achieved functional remission (22.8% vs 16.0%, P<0.001) and recovery (16.5% vs 11.7%, P<0.001) at 36 months.
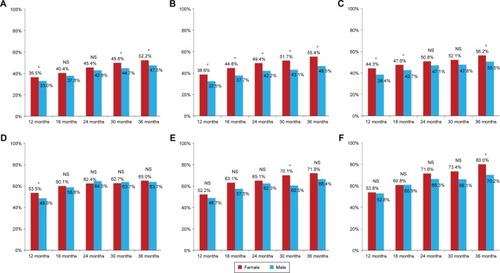
– show the rates of these outcomes by sex over the follow-up period in each of the six regions. While females generally achieved better outcomes than males across the regions, there were some inconsistencies in this pattern outside Europe, especially for functional remission and recovery. As for clinical remission (), a higher percentage of females than males achieved clinical remission at 36 months across the regions, but the sex difference was not statistically significant in Latin America (P=0.633) and East Asia (P=0.217). In addition, the sex difference in this rate became statistically significant only at 36 months, but not at other earlier visits, in North Africa and the Middle East. Notably, however, the rates of clinical remission were generally higher in both sexes outside Europe including Latin America and East Asia as well as North Africa and the Middle East.
Figure 1 Rates of clinical remission by sex in each region.
Abbreviation: NS, nonsignificant.
In contrast to clinical remission, the rates of functional remission were generally higher in Northern Europe and Southern Europe than in the other regions, and also a higher percentage of females than males still achieved functional remission in these regions and also in Latin America (). While a similar pattern was observed in Central and Eastern Europe (17.4% for females and 14.6% for males at 36 months), the sex difference did not reach statistical significance (P=0.151). No sex difference in the rates of functional remission was observed in East Asia (13.3% for females and 15.6% for males at 36 months, P=0.479) and also in North Africa and the Middle East (15.9% for females and 15.8% for males at 36 months, P=0.969).
Figure 2 Rates of functional remission by sex in each region.
Abbreviation: NS, nonsignificant.
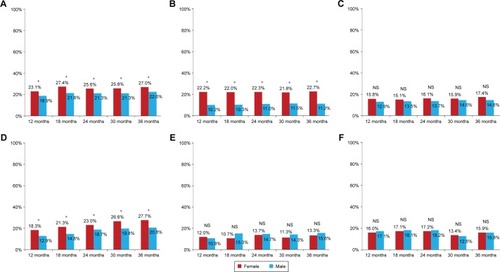
Figure 3 Rates of recovery by sex in each region.
Abbreviation: NS, nonsignificant.
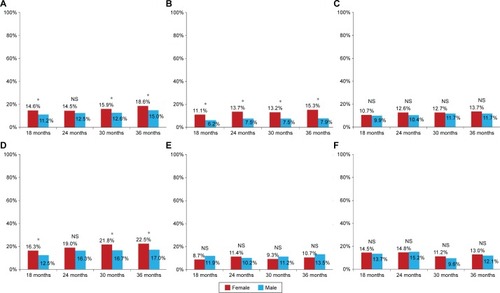
As for recovery (), the pattern by sex and region was very similar to that of functional remission; the sex difference at 36 months was only statistically significant in Northern Europe (18.6% vs 15.0%, P=0.014), Southern Europe (15.3% vs 7.9%, P<0.001), and Latin America (22.5% vs 17.0%, P=0.009), but not in Central and Eastern Europe (13.7% vs 11.7%, P=0.266), East Asia (10.7% vs 13.5%, P=0.344), and Africa and the Middle East (13.0% vs 12.1%, P=0.743).
The pattern of these outcomes by sex and region was largely maintained even after key baseline patient characteristics were controlled for (). There were, however, two broad exceptions. First, the sex difference in achieving clinical remission during follow-up was statistically significant only in Southern Europe (odds ratio [OR] of female vs male =1.45, P<0.001) and North Africa and the Middle East (OR =1.36, P=0.046) at a significance level of 0.05, and marginally significant at a significance level of 0.1 in Northern Europe (OR =1.15, P=0.056), Central and Eastern Europe (OR =1.19, P=0.057), and also in East Asia (OR =1.30, P=0.077). Second, unlike in the descriptive statistics for functional remission and recovery, females in North Africa and the Middle East appeared to be more likely than males to achieve functional remission and recovery during follow-up in regression analyses (OR =1.72, P=0.027 for functional remission; OR =1.81, P=0.022 for recovery). The other regions exhibited patterns of sex differences similar to those observed in descriptive statistics. As in clinical remission, the sex difference in achieving functional remission and recovery was greatest in Southern Europe (OR =2.47, P<0.001 for functional remission; OR =1.98, P<0.001 for recovery). In addition, the sex difference was statistically significant in Northern Europe (OR =1.51, P<0.001 for functional remission; OR =1.49, P<0.001 for recovery) and Latin America (OR =1.52, P=0.001 for functional remission; OR =1.40, P=0.013 for recovery), but not in Central and Eastern Europe (OR =1.14, P=0.366 for functional remission; OR =1.06, P=0.715) and East Asia (OR =1.00, P=0.985 for functional remission; OR =0.94, P=0.807 for recovery).
Table 2 GEE results: odds ratios of female vs male in achieving remission, functional remission, and recovery during follow-up in each region
Discussion
Sex differences in the prognosis of schizophrenia
The results of the W-SOHO study, the largest prospective observational study on the outcomes of schizophrenia in the outpatient setting, revealed the existence of sex differences in the prognosis of schizophrenia, with relevant regional differences. Consistent with the prevailing evidence, females had a higher frequency of clinical remission (58.0% vs 51.8%), functional remission (22.8% vs 16.0%), and recovery (16.5% vs 16.0%) at 36 months than males, although the differences were relatively small. Remarkably however, not all regions followed this pattern: a better course of illness in females was consistently observed for all three outcomes in Southern Europe and Northern Europe, but not in other regions. The sex differences in the former regions were maintained even after controlling for the potential mediators for the link between sex and outcomes, such as age at first service contact for schizophrenia, clinical severity, alcohol or substance abuse, and functional status at baseline.
This regional variation, despite the consistency of the study design and methodology in all of the participating countries of W-SOHO, may indicate the importance of psychosocial and cultural factors and their differential effects on sex in the prognosis of schizophrenia. However, the current analysis did not explore the relative contributions of both biological and psychosocial/cultural factors to the sex differences and their interplay, which clearly warrants further research.
Regional variation in sex differences in the patient characteristics and the prognosis of schizophrenia
As part of the World Health Organization (WHO) Collaborative Study on the Assessment and Reduction of Psychiatric Disability conducted over 25 years ago, Hambrecht et alCitation41 examined and compared the influence of sex on age at onset, symptomatology, and course of schizophrenia in patients with schizophrenia, paranoid, or unspecified psychosis from seven Western European (n=223), Balkan (n=156), and Islamic centers (n=141). Some regional differences emerged: an earlier onset in males was observed in all five European centers, but not in Islamic centers; similarly, sex differences in symptomatology were found in the former, but rarely in the latter. While the study did not make a cross-cultural comparison of sex differences in course of schizophrenia, the findings with the pooled sample showed that blunted affect, social withdrawal, alcohol abuse, and self-neglect were more frequent in males than in females at 1- and 2-year follow-ups. To our knowledge, there are no other published cross-national studies that have explored sex differences in the prognosis of schizophrenia.
The findings of W-SOHO, as mentioned previously, revealed some regional variation in the sex differences in the outcomes of schizophrenia in terms of clinical remission, functional remission, and recovery. Southern Europe and Northern Europe were the only regions where the sex differences were observed for all three outcomes in both descriptive and regression analyses, with higher rates of these outcomes in females than in males. Consistent with previous reports, females in these regions exhibited the following tendency, which might have contributed to higher rates of remission and recovery in females: a later age at first service contact for schizophrenia, a lower level of overall clinical severity, a lower level of negative symptom severity (but a higher level of depressive symptom severity), a lower percentage of alcohol or substance abuse at baseline, a higher percentage of having a spouse or partner, and a higher percentage of independent living. While similar patterns were also observed in other regions albeit with some exceptions, especially for North Africa and the Middle East, the mean age at first service contact, the percentage of independent living, and that of being socially active were generally higher in both males and females in Europe, compared to the other non-European regions. Notably, the sex differences in the rates of remission/recovery found in Southern and Northern Europe were not fully accounted for by the sex differences in these baseline patient characteristics.
The sex differences in the outcomes of schizophrenia were less pronounced and consistent in the other regions. For instance, in Central and Eastern Europe, rates of clinical remission were higher in females than in males at 36 months, but those of both functional remission and recovery were similar between males and females. On the contrary, in Latin America, the former was similar between males and females, but the latter rates were higher in females than in males.
In addition, sex differences in the outcomes of schizophrenia were rarely observed in East Asia (composed of Malaysia, South Korea, and Taiwan in this study). This finding does not seem consistent with the view that marriage can act as a protection against psychological breakdowns, given the fact that the rate of marriage was highest in East Asian females (56.4%) across both sexes of all regions. There is, however, some evidence suggesting an increased risk of suicide in young married females in South KoreaCitation42 and Taiwan.Citation43 Taken together, this may indicate no protective role of marriage in females against psychological breakdowns in this region where the role of females is changing fast. Moreover, the rate of paid employment was also lowest in these East Asian females, and unlike other regions, there was no sex difference in the rate of alcohol or substance abuse in this region (1.3% for females vs 2.0% for males, P=0.353). All of these might have diluted the sex differences in the outcomes of schizophrenia in this region, and also contributed to the lowest frequency of functional remission and recovery in East Asian females.
Finally, North Africa and the Middle East revealed some interesting patterns. First of all, there were no sex differences in the age at first service contact for schizophrenia (26.7 [SD =9.3] for females vs 25.9 [SD =8.1] for males, P=0.412) and in the percentage of having a spouse or partner (29.0% for females vs 33.4% for males, P=0.145). An earlier age at first service contact in males by 2–4 years was a phenomenon observed in all other regions. Nevertheless, this finding, ie, no sex difference in the age at first service contact in this region, is consistent with the earlier WHO Collaborative Study on the Assessment and Reduction of Psychiatric Disability, which also showed no sex difference in the onset of schizophrenia in Islamic centers but not in other European centers.Citation41 Notably, the level of positive symptoms, as measured with the CGI-SCH positive symptoms scores, was higher in females than in males in this region (4.5 [SD =1.3] vs 4.2 [SD =1.4], P=0.002), but similar between the two in other regions. In fact, the level of positive symptom severity was highest in this group of females across both sexes of all regions. It should also be noted that the level of overall symptom severity was also highest in both males (4.6 [SD =1.0]) and females (4.6 [SD =1.0]) in this region than in anywhere else. This may indicate that only those patients with more severe symptoms are likely to be diagnosed and treated for schizophrenia in North Africa and the Middle East. The role of positive symptoms in this sense might be particularly more important in this region, especially for females. No sex difference observed in the percentage of having a spouse/partner, unlike in other regions, may also be related to Islamic culture. Remarkably, this region showed a better course of illness in females than in males for all three outcomes only after controlling for the baseline patient characteristics. Otherwise, females had a greater frequency only for clinical remission at 36 months but neither at other earlier visits nor for other outcomes (ie, functional remission and recovery) at any visits.
These regional variations are likely to indicate the influence of biological, psychosocial, and cultural factors and their differential effects on sex in the course of schizophrenia. Among the biological factors, there may exist a protective role of estrogen.Citation29 Our study was, however, unable to test this hypothesis since its plasma level of estrogen was not examined in this observational study. Moreover, given that age at first service contact for schizophrenia and duration of illness were taken into account in our regression analyses, patient age was not controlled for as a separate variable in the analyses. The literature suggests that better outcomes of females with schizophrenia may decline over time, and eventually approximate that of males with schizophrenia due to a reduction in the level of estrogen in females.Citation44–Citation46 However, Grossman et alCitation4 did not find this pattern in a 20-year follow-up of patients with schizophrenia. In addition, although a shorter duration of illness was significantly associated with better outcomes across the regions in our study, similar associations were observed for both males and females (data not shown).
In summary, we found sex differences in the course of schizophrenia which were more marked in Europe. Continents that for cultural or religious differences have more marked sex inequalities did not show sex differences with a more favorable course in females. In these countries with higher sex inequality, the more favorable course in females, which is probably due to the protective role of estrogen, might have been diluted given the social situation of females. A recent study by Luhrmann et alCitation47 suggests that the clinical presentation of schizophrenia may be the result of an interaction between the pathological and cultural processes, a process which they name “social kindling”. Accordingly, sex differences will arise from the complex interactions among very different biological and environmental factors. However, since that study is descriptive, we cannot test the hypothesis that the lack of sex differences in these areas is due to cultural or religious factors.
Taken together, these findings also highlight the need for a more sex-sensitive approach in the treatment of schizophrenia. Moreover, psychosocial and cultural factors should also be fully taken into account, in addition to biological factors, in order to optimize both clinical and functional outcomes in schizophrenia.
Limitations
The current findings need to be interpreted in the context of the following limitations of the study. First, the W-SOHO studies were originally designed to assess the comparative costs and outcomes associated with treatment. The current findings as such emerged only from secondary analyses formulated to test sex differences in the outcomes of schizophrenia across diverse regions of the world. Second, the 37 countries included in the W-SOHO study were categorized into six regions, but they may not be representative of these regions and also had different sample sizes. Third, the sex differences in the outcomes of schizophrenia in each of the six regions were adjusted for clinical and sociodemographic characteristics of patients. However, data constraints on biological factors such as a family history of schizophrenia or plasma level of estrogen limited our ability to fully distinguish the influence of psychosocial and cultural factors from that of biological factors on the sex differences in the prognosis of schizophrenia. In addition, there could be other unobserved differences between the sexes and between the regional cohorts, which could confound our results. Fourth, we have not analyzed the role that differences in antipsychotic treatment response may have in these findings. Fifth, although there were no relevant differences in follow-up rate between males and females, there were some among the regions, with a higher dropout rate in Asia, Africa, and the Middle East.Citation5 Notably, these regions also had the lowest percentage of females participating in the study, and the severity of their cases was higher than the rest of the regions. This could be related to only the most severe cases being treated in those countries. If that is the case, this could partially explain the lack of sex differences: the less severe cases (especially for females) could have an even better preclinical outcome and do not enter in the study. In summary, there could be a number of unobserved differences between the sexes and between the regional cohorts that could confound our results. Finally, our definition of clinical remission required a low level of symptoms for at least 6 months, consistent with the definition proposed by Andreasen et al.Citation40 However, our definition of remission was based on the CGI-SCH, which is a valid but less specific measure of clinical severity than other scales such as the Positive and Negative Syndrome Scale.Citation48 Previous analyses have shown a good agreement between this and Andreasen’s definition.Citation49
Conclusion
The results of the W-SOHO study suggest sex differences in the patient characteristics and also in the outcomes of schizophrenia across diverse regions of the world. Consistent with previous findings, a later age at first service contact for schizophrenia, a lower level of overall/negative symptom severity, lower percentages of alcohol/substance abuse and paid employment, and higher percentages of having a spouse/partner and independent living in females were observed in most regions, but with some exceptions. Overall, females had slightly higher rates of clinical remission (58.0% vs 51.8%), functional remission (22.8% vs 16.0%), and recovery (16.5% vs 16.0%) than males at 36 months. This pattern was consistently observed in Southern Europe and Northern Europe even after controlling for the baseline sex differences, but not in other regions. These regional variations shed light on the importance of psychosocial and cultural factors and their differential effects on sex in the prognosis of schizophrenia. A more sex-sensitive approach relevant to each culture is required in the treatment of schizophrenia.
Acknowledgments
The findings of this paper were presented at the fourth Biennial Schizophrenia International Research Conference 2014 as a poster presentation with interim findings. The poster’s abstract was published in Schizophrenia Research Volume 153, Supplement 1, S1–S402 (http://www.schres-journal.com/issue/S0920-9964(14)X0004-6?page=19). The W-SOHO study was funded by Eli Lilly & Company.
Disclosure
DN, WM, and TT are employees of Eli Lilly and Company. JMH has acted as a consultant, received grants, or acted as a speaker in activities sponsored by the following companies: Astra-Zeneca, Eli Lilly and Company, Glaxo-Smith-Kline, and Lundbeck. MVM conducted the statistical analysis under a contract between Fundació Sant Joan de Déu and Eli Lilly and Company. The authors declare no other conflicts of interest in this work.
References
- RobinsLNHelzerJEWeissmanMMLifetime prevalence of specific psychiatric disorders in three sitesArch Gen Psychiatry198441109499586332590
- AngermeyerMCGoldsteinJMKuehnLGender differences in schizophrenia: rehospitalization and community survivalPsychol Med19891923653822762441
- GoldsteinJMGender differences in the course of schizophreniaAm J Psychiatry198814566846893369553
- GrossmanLSHarrowMRosenCFaullRStraussGPSex differences in schizophrenia and other psychotic disorders: a 20-year longitudinal study of psychosis and recoveryCompr Psychiatry200849652352918970899
- HaroJMNovickDBertschJKaragianisJDossenbachMJonesPBCross-national clinical and functional remission rates: Worldwide Schizophrenia Outpatient Health Outcomes (W-SOHO) studyBr J Psychiatry2011199319420121881098
- IniestaROchoaSUsallJGender differences in service use in a sample of people with schizophrenia and other psychosesSchizophr Res Treatment2012201236545222966434
- NovickDHaroJMHongJRegional differences in treatment response and three year course of schizophrenia across the worldJ Psychiatr Res201246785686422575332
- SalokangasRKPrognostic implications of the sex of schizophrenic patientsBr J Psychiatry19831421451516839067
- UsallJArayaSOchoaSGender differences in a sample of schizophrenic outpatientsCompr Psychiatry200142430130511458304
- AngermeyerMCKühnLGender differences in age at onset of schizophrenia. An overviewEur Arch Psychiatry Neurol Sci19882373513643053193
- FaraoneSVChenWJGoldsteinJMTsuangMTGender differences in age at onset of schizophreniaBr J Psychiatry199416456256297921712
- HäfnerHan der HeidenWBehrensSCauses and consequences of the gender difference in age at onset of schizophreniaSchizophr Bull1998241991139502549
- SzymanskiSLiebermanJAAlvirJMGender differences in onset of illness, treatment response, course, and biologic indexes in first-episode schizophrenic patientsAm J Psychiatry199515256987037726309
- GurREPettyRGTuretskyBIGurRCSchizophrenia throughout life: sex differences in severity and profile of symptomsSchizophr Res19962111128864248
- LewisSSex and schizophrenia: vive la differenceBr J Psychiatry19921614454501356575
- Riecher-RösslerAHafnerHGender aspects in schizophrenia: bridging the border between social and biological psychiatryActa Psychiatr Scand Suppl2000Suppl 1024075862
- SchultzSKMillerDDOliverSEArndtSFlaumMAndreasenNCThe life course of schizophrenia: age and symptom dimensionsSchizophr Res199723115239050124
- ShtaselDLGurREGallacherFHeimbergCGurRCGender differences in the clinical expression of schizophreniaSchizophr Res1992732252311390401
- WieselgrenIMLindströmELindströmLHSymptoms at index admission as predictor for 1–5 year outcome in schizophreniaActa Psychiatr Scand19969453113199124077
- WeiserMReichenbergARabinowitzJGender differences in premorbid cognitive performance in a national cohort of schizophrenic patientsSchizophr Res200045318519011042436
- ChildersSEHardingCMGender, premorbid social functioning, and long-term outcome in DSM-III schizophreniaSchizophr Bull19901623093182374886
- MorganVACastleDJJablenskyAVDo women express and experience psychosis differently from men? Epidemiological evidence from the Australian National Study of Low Prevalence (Psychotic) DisordersAust N Z J Psychiatry2008421748218058447
- NormanRMMallaAKManchandaRTownsendLPremorbid adjustment in first episode schizophrenia and schizoaffective disorders: a comparison of social and academic domainsActa Psychiatr Scand20051121303915952943
- AngermeyerMCMatschingerHHolzingerAGender and attitudes towards people with schizophrenia. Results of a representative survey in the Federal Republic of GermanyInt J Soc Psychiatry19984421071169675630
- UsallJHaroJMOchoaSMarquezMArayaSNeeds of Patients with Schizophrenia G. Influence of gender on social outcome in schizophreniaActa Psychiatr Scand2002106533734212366467
- LewineRRReflections on Saugstad’s “social class, marriage, and fertility in schizophrenia”Schizophr Bull1990162171174 discussion 175–1782374878
- BarnesTRMutsatsaSHHuttonSBWattHCJoyceEMComorbid substance use and age at onset of schizophreniaBr J Psychiatry200618823724216507965
- FotiDJKotovRGueyLTBrometEJCannabis use and the course of schizophrenia: 10-year follow-up after first hospitalizationAm J Psychiatry2010167898799320478874
- SeemanMVThe role of estrogen in schizophreniaJ Psychiatry Neurosci19962121231278820178
- CernovskyZZLandmarkJAO’ReillyRLSymptom patterns in schizophrenia for men and womenPsychol Rep1997803 pt 2126712719246891
- GalderisiSBucciPÜçokAPeuskensJNo gender differences in social outcome in patients suffering from schizophreniaEur Psychiatry201227640640821616645
- LabelleALightMDunbarFRisperidone treatment of outpatients with schizophrenia: no evidence of sex differences in treatment responseCan J Psychiatry200146653454111526810
- HaroJMEdgellETJonesPBThe European Schizophrenia Outpatient Health Outcomes (SOHO) study: rationale, methods and recruitmentActa Psychiatr Scand2003107322223212580830
- DossenbachMArango-DávilaCSilva IbarraHResponse and relapse in patients with schizophrenia treated with olanzapine, risperidone, quetiapine, or haloperidol: 12-month follow-up of the Intercontinental Schizophrenia Outpatient Health Outcomes (IC-SOHO) studyJ Clin Psychiatry20056681021103016086618
- KaragianisJNovickDPecenakJWorldwide-Schizophrenia Outpatient Health Outcomes (W-SOHO): baseline characteristics of pan-regional observational data from more than 17,000 patientsInt J Clin Pract200963111578158819780867
- American Psychiatric Association APA)Diagnostic and Statistical Manual of Mental DisordersFourth edWashington, DCAPA1994
- World Health Organisation (WHO)The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic GuidelinesGenevaWHO1992
- HaroJMKamathSAOchoaSThe Clinical Global Impression-Schizophrenia scale: a simple instrument to measure the diversity of symptoms present in schizophreniaActa Psychiatr Scand Suppl2003416162312755850
- HaroJMNovickDSuarezDSOHO Study GroupRemission and relapse in the outpatient care of schizophrenia: three-year results from the Schizophrenia Outpatient Health Outcomes studyJ Clin Psychopharmacol200626657157817110813
- AndreasenNCCarpenterWTJrKaneJMLasserRAMarderSRWeinbergerDRRemission in schizophrenia: proposed criteria and rationale for consensusAm J Psychiatry2005162344144915741458
- HambrechtMMaurerKHäfnerHGender differences in schizophrenia in three cultures. Results of the WHO collaborative study on psychiatric disabilitySoc Psychiatry Psychiatr Epidemiol19922731171211621135
- HongJKnappMImpact of macro-level socio-economic factors on rising suicide rates in South Korea: panel-data analysis in East AsiaJ Ment Health Policy Econ201417415116225599279
- YehJYXirasagarSLiuTCLiCYLinHCDoes marital status predict the odds of suicidal death in Taiwan? A seven-year population-based studySuicide Life Threat Behav200838330231018611128
- JonssonHNymanAKPredicting long-term outcome in schizophreniaActa Psychiatr Scand19918353423461853726
- LoydDSimpsonJCTsuangMTAre there sex differences in the long-term outcome of schizophrenia? Comparisons with mania, depression, and surgical controlsJ Nerv Ment Dis1985173116436494056778
- OpjordsmoenSLong-term clinical outcome of schizophrenia with special reference to gender differencesActa Psychiatr Scand19918343073132028808
- LuhrmannTMPadmavatiRTharoorHOseiAHearing voices in different cultures: a social kindling hypothesisTop Cogn Sci20157464666326349837
- KaySRFiszbeinAOplerLAThe positive and negative syndrome scale (PANSS) for schizophreniaSchizophr Bull19871322612763616518
- HaroJMAssessment of remission in schizophrenia with the CGI and CGI-SCH scalesActa Psychiatr Scand2008117215617970843
