Abstract
Purpose
The aim of this study was to examine the effectiveness of a combined cognitive-behavioral therapy for insomnia (CBT-I) and hypnotherapy for insomnia (HT-I) program for insomnia patients with or without additional depression regarding depressive symptoms and various sleep parameters.
Patients and methods
A sample of 63 patients suffering from insomnia received a six-session sleep intervention, which combined cognitive-behavioral and hypnotherapeutical elements. Due to violating exclusion criteria, data of 37 patients were analyzed. Ten patients had insomnia comorbid with depression, whereas 27 patients had insomnia only. Sleep diaries were implemented to measure various sleep parameters, whereas depressive symptomatology was assessed with the anxiety and depression scale and Symptom-Checklist-90-R at baseline, before and after the intervention, as well as at 3-months follow-up.
Results
Depressive symptoms decreased from pre to post measurement and follow-up for patients with insomnia comorbid with depression, whereas scores of patients with only insomnia remained relatively on a low level. Both groups showed a significant increase of sleep efficiency and a significant decrease of the duration of wake after sleep onset. However, only patients with insomnia and depression revealed a significant reduction of sleep-onset latency and a higher level of regeneration. Nondepressive insomniacs, on the other hand, showed a significant increase of performance from post measurement to follow-up. For both groups, no change over time was found for number of wake after sleep onset, total sleep time, mood in the morning and evening.
Conclusion
Combining CBT-I and HT-I is effective in reducing depressive symptoms and improving sleep. Therefore, nonresponders to other forms of therapy, eg, pharmacological, interpersonal, or cognitive-behavioral therapy, might benefit from the combined CBT-I/HT-I intervention.
Introduction
Research showed that insomnia is a widespread disorder among individuals in industrial nations and is associated with various negative consequences, like health problems, increase of medication, job problems, accidents, and a decreased level of quality of life.Citation7 The lifetime prevalence of insomnia is estimated at 24.6%, and ~40% develop a more chronic form of insomnia.Citation6,Citation8 While 2.3% of the people aged 20 suffer from insomnia, this number increased to 13.9% at age 35, and dropped again to 5.5% at age 41.Citation8
Due to the close bidirectional relationship between insomnia and affective disorders, it is not surprising that in 40% of the cases comorbidities with insomnia occurred regularly.Citation13,Citation22 Especially, an association between insomnia and affective disorders was confirmed in various samples.Citation13 Up to 50% of patients with insomnia developed a major depressive disorder.Citation8,Citation25 Even after controlling for other symptoms, the odds ratio for a major depression associated with insomnia is 2.1.Citation6 Hereby, no age effects could be detected.Citation2 Conclusively, insomnia is one of the most important risk factors for developing a depression and prevents remission.Citation12,Citation16 Qualitative predictors for recurrence of depression are subjective sleep disturbances and anxiety, though higher levels of sleep disturbances occurred several weeks prior to recurrence.Citation34,Citation36
Vice versa, 90% of depressive patients reported complaints about their sleep quality and two-thirds of them will meet the criteria for insomnia.Citation16,Citation25 Patients with affective disorders showed an increased level of sleep-onset latency (SOL) and percentage of rapid eye movement (REM) sleep, whereas total sleep time (TST), sleep efficiency (SE), slow wave sleep (SWS), and REM latency decreased.Citation41 Luik et al, however, found that longer REM sleep latency and higher REM density were associated with depressive symptoms.Citation28 Yet, after excluding patients using medication, only REM density remained related to depressive symptoms.Citation28
Cognitive-Behavioral Therapy for Insomnia (CBT-I)
Cognitive-behavioral therapy became a standard treatment for primary insomnia, as well as insomnia comorbid with medical or psychiatric disorders.Citation37,Citation38,Citation40 Several studies showed that CBT-I influenced various subjective sleep parameters.Citation19,Citation24,Citation29,Citation44 After CBT-I intervention, often SOL, wake after sleep onset (WASO), insomnia severity, and use of sleep medication declined, whereas SE, TST, and sleep quality increased. Effect sizes fluctuated from small (TST) to large effects (sleep quality) depending on the sleep variable and measurement method.Citation24 However, younger adults and patients with higher values of sleep self-efficacy showed the greatest improvement of SE at post measurement and follow-up.Citation27 Besides improving sleep after using a CBT-I intervention, Trauer et al reported improved sleepiness, self-efficacy, motoric vigilance, health status, beliefs and attitudes about sleep, and daytime functioning.Citation44 These improvements are independent of age, gender, type, or duration of complaints.Citation46
Comparing regular CBT-I with other forms of therapy, eg, pharmacotherapy, relaxation training, and sleep hygiene education, showed that CBT-I was superior.Citation1,Citation3,Citation33,Citation35,Citation43 A meta-analysis by Okajima et al reported that CBT-I was more effective than a control group regarding SOL, WASO, time in bed (TIB), and SE.Citation35 Effect sizes ranged from small to medium for post measurement and from medium to large for follow-up. Differences between subjective and objective measurements were found for SOL and TST, which only improved in the sleep diaries. A level of good sleep at follow-up was achieved by 38% in the CBT-I group, whereas none achieved a good level of sleep in the control group.Citation47 Ashworth et al reported a rate of 67% for clinical remission of insomnia (vs 11% for self-help CBT-I), and 78% for those with additional comorbid depression (vs 17% for self-help CBT-I).Citation1 Furthermore, patients with insomnia and comorbid diseases reported the poorest sleep hygiene practice compared to a group of insomnia only patients, and to good sleepers, who reported the best sleep hygiene.Citation45 Comparing a CBT-I intervention with a sleep hygiene education revealed a reduction of SOL and WASO, as well as an improvement of SE for the CBT-I group.Citation14 The same effects account for a relaxation training, whereby sleep quality, early morning awakening, and TST were equal for both groups.Citation33 Nevertheless, effectiveness of a CBT-I intervention was mediated by the change of depression severity, as well as the content of the intervention rather than the comorbidity.Citation1,Citation14 Finally, adding CBT-I to a treatment, as usual, leads to higher quality-adjusted life years without a significant increase in cost.Citation48
Focusing on insomnia treatments for depressive patients seems to be highly relevant due to the high comorbidity of insomnia with depression and their negative influence on affective symptoms. Koffel et al reported reduced scores for depression from pre to post treatment and to follow-up.Citation24 In addition, normalized depressive symptoms were shown in 87.5% of treatment completers and normalized sleep patterns in 100% of patients with insomnia and depression.Citation42 Furthermore, SOL and WASO decreased, while TST, SE, and sleep quality increased with medium to large effect sizes.Citation5,Citation42 On the other hand, higher scores for depression were associated with shorter sleep duration and shorter TIB.Citation18 Additionally, comorbidity reduced anxiety and depressive symptoms in patients of the CBT-I group, though this effect could not be found in the only cognitive therapy and the only behavioral therapy groups.Citation4
The higher reduction of insomnia symptoms, when using an insomnia treatment instead of a treatment for depression, has proved that insomnia is not just a symptom of depression, but rather needs separate treatment.Citation5 Blom et al compared patients with insomnia and depression receiving either an insomnia (CBT-I) or depression intervention.Citation5 Patients from the CBT-I group showed a distinctive increase of SE and decrease of SOL and use of sleep medication with medium to large effects. Depressive symptoms were unaffected by the type of intervention.
Hypnotherapy for insomnia
Adding hypnotherapeutical elements to a CBT-I program might improve sleep parameters even more, because insomniacs often respond to this kind of therapy and relaxation.Citation32 A meta-analysis by Lam et al found that hypnotherapy increased various subjective sleep parameters from baseline to posttreatment.Citation26 In comparison to a waitlist-control group, participants receiving hypnotherapy showed decreased SOL. However, the number of nighttime awakenings did not differ between those two groups. Additionally, a hypnotic suggestion led to an extension of SWS in 81% of young females and 57% of older females compared with a control group.Citation9,Citation10 This enhanced activity led to a better prefrontal cognitive functioning. However, this effect was significant only for high and middle suggestible participants.Citation10 Besides improving sleep, Holdevici et al investigated the effect of an intervention, which was based on hypnosis and relaxation, on depressive and anxiety symptoms.Citation21 Both men and women showed a significant reduction of symptoms for anxiety and depression immediately after the intervention and at a 3-months followup.Citation21 Thereby, hypnotherapy seems to be more effective than waitlist-control groups, cerebral electrotherapy, and pharmacological therapy in improving sleep and reducing depressive symptoms.Citation26
Research question
The aim of this study was to examine the effectiveness of a combined cognitive-behavioral and hypnotherapeutical program for depressive and nondepressive patients. We assumed that patients suffering from insomnia without depression report less sleep problems after 3-months follow-up to a sleep intervention than patients suffering from insomnia with depression. Furthermore, we assumed that depressive symptoms will decrease for both groups, however, more predominantly in the group of depressive patients.
Patients and methods
Procedure and sample
This longitudinal pilot study included 74 participants between the age of 18 and 65 years suffering from insomnia: difficulties falling or staying asleep for at least 1 month. Patients were informed via our webpage of the outpatient clinic, newspaper, and information sheets in care practices. Prior to participation, information about diagnostic procedure, post-diagnostic measurement, and treatment content was given. Furthermore, they were informed that they could quit at any time without any negative consequences. After information about procedure and treatment, participants gave their written informed consent. In a further step, participants completed questionnaires regarding their demographic background, current life style, medication, sleep problems, as well as somatic and psychological impairments; selected participants were assessed 8 weeks prior to the treatment (baseline, t0). This assessment included a sleep log for 14 days and further questionnaires for mental health. To evaluate effects of waiting time, another assessment with the same instruments was conducted right before the 6-week intervention (t1) and after the intervention (t2), and at 3-months follow-up (t3). This six-session sleep intervention combined cognitive-behavioral (CBT-I), eg, psychoeducation, progressive muscle relaxation, stress management, and problem-solving, and hypnotherapeutical elements for insomnia (HT-I) in the form of different trances for each session. Each group session lasted for 120 minutes and consisted of four to seven patients and two to three trainers in a face-to-face setting. Exclusion criteria for data analysis were additional psychotherapy at the same time (n=11) leading to a participating sample of 63 adults. Furthermore, data sets with >30% of missing data on the post measurement (n=26) were excluded from analysis. Thus, 37 participants with a mean age of 43.86 (SD=13.08; 25 females, 12 males) were included for statistical analyses. shows sample description at baseline. The study was approved by the ethical board of the University of Tuebingen and carried out in accordance with national law and the Helsinki Declaration of 1975 (in its current, revised form).
Table 1 Sample description at baseline
Instruments
Sleep log
Sleep logs are an essential tool in the assessment of sleep problems and sleep disorders. Based on the sleep logs of the German association for sleep medicine, each sleep log assesses participants’ bedtime, wake-up time, SOL, subjective regeneration, daytime functioning, performance, medication, and substance consumption over a period of 2 weeks.Citation11 Participants are asked to complete these sleep logs, but only the second week data will be used for statistical analysis to avoid bias of adaption and irritation in the first week. For statistical analysis, the following sleep parameters are used: SOL, number and duration of WASO, TST, SE, mood in the morning and evening, performance, and regeneration (“How restful/tired do you feel at the moment?”). Mood, performance, and regeneration are measured on a six-point Likert scale from 1 (“very good”) to 6 (“very bad”).
General Depression Scale (ADS)
This 20-item self-report instrument gathers information about impairment regarding depressive affect, somatic complaints, motoric inhibition, and negative thought patterns. Participants rate the frequency of their impairment on a four-point scale referring to the last week. It can be used for adults between the age of 14 and 80 years in clinical and nonclinical samples. Sum score above 23 is an indicator of a depressive disorder. With an internal consistency of α=0.89 and a split-half reliability of r=0.81. This instrument shows adequate psychometric properties.Citation20
Symptom-Checklist-90-R (SCL-90-R)
Subjective impairment of somatic and psychological symptoms was assessed with the SCL-90-R, which gathers information retrospectively over a period of 1 week and consists of 90 items, which are rated on a four-point scale from “not at all” to “very intense”. Adolescents’ (from the age of 12) and adults’ psychological distress is classified on nine subscales: somatization, obsessive-compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism. Three global indices give information about participant’s response: Global Severity Index, Positive Symptom Distress Index, and Positive Symptom Total. Internal consistencies for each subscale are between α=0.74 and α=0.97 for clinical and nonclinical samples. The instrument has demonstrated acceptable retest reliabilities between 0.69 and 0.92.Citation15
Data analysis
Statistical analyses were carried out with IBM SPSS Statistics 23. The P-value was set to P<0.05. For testing the longitudinal effects of this intervention, analyses of variances with repeated measures were used. In case of significance of the Mauchly test of sphericity, data were corrected using the Greenhouse–Geisser correction. Post hoc analyses of significant main and interactions effects included Bonferroni corrected pairwise comparisons for normally distributed data and Wilcoxon tests for non-normally distributed data. The effect size Cohen’s d will be reported for group comparisons and partial eta squared (ηp2) for the analyses of variance. An effect size of d=0.2 and ηp2=0.01 shows a small effect, d=0.5 and ηp2=0.06 a medium effect, and d=0.8 and ηp2=0.14 a large effect.
Results
Group comparisons at baseline
Analyzing the effect of an intervention in depressive and nondepressive patients on various variables required a comparison at baseline. Thus, t-tests for independent samples were conducted which showed that nondepressive patients reported a significant better mood in the morning and evening, felt more regenerated, more efficient, and less psychologically stressed prior to treatment (). Age, duration of sleep problems, SOL, WASO, TST, and SE did not differ significantly between the two groups. However, depressive patients exceeded the cutoff scores for SOL with 36 minutes (cutoff 30 minutes), duration of WASO of 38 minutes (cutoff 30 minutes), and TST with 357 minutes (cutoff 390 minutes) according to literature.
Table 2 Group comparisons of depressive vs nondepressive participants at baseline
A chi-squared test showed no significant difference between depressive and nondepressive patients regarding gender, χ2 (1, N=37)=1.93, P=0.16, and medication, χ2 (1, N=37)=0.01, P=0.92. Patients who completed did not differ regarding age, sleep problems, or depression in comparison to those who did not complete (all P>0.05).
Sleep parameters
According to our hypothesis, it was assumed that various sleep parameters from the sleep diary would improve over time for both groups; however, these improvements will be less distinctive for insomnia patients with comorbid depression.
SOL of depressive patients decreased significantly from 36 minutes at baseline to 21 minutes at post measurement, which is under the clinical cutoff, but increased again to 30 minutes at follow-up, whereas no significant change occurred for nondepressive patients. No significant interaction was found, F (3, 105)=1.818, P=0.168. Also, the number of WASO showed no significant main or interaction effects for neither depressive nor nondepressive patients. On average, patients woke up one to two times per night. However, duration of WASO decreased from 33 minutes before treatment to 17 minutes at follow-up in nondepressive patients. For depressive patients, this main effect was marginally significant with 37 minutes at premeasurement to 17 minutes at follow-up, though no significant interaction occurred, F (3, 105)=1.112, P=0.336; however, the change is clinically significant. SE increased from 76% to 82% for nondepressive patients; similarly from 75% to 84% for depressive patients. Both groups did not differ regarding SE after treatment, F (3, 105)=1.315, P=0.275. Nevertheless, a significant increase of SE could be revealed only from pre-measurement to follow-up in nondepressed, P=0.04.
Regeneration was significantly influenced by the presence of a depression, meaning that depressive patients improved their scores for regeneration from premeasurement to follow-up, P=0.008, whereas no change occurred for nondepressed insomnia patients. The interaction of time and group was marginally significant, F (3, 105)=2.281, P=0.084, ηp2=0.061. Regarding performance, nondepressive patients showed a significant improvement over time, especially from post measurement to follow-up, P=0.036. However, changes over time for depressive patients, and the interaction were not significant, F (3, 105)=0.327, P=0.806.
Concerning TST, no significant main or interaction effects were found, F (3, 105)=1.312, P=0.275, mood in the morning, F (3, 105)=0.377, P=0.77, and in the evening, F (3, 105)=0.474, P=0.701, meaning that depressive and nondepressive patients remained stable over time and did not differ among each other. shows the effects over time for depressive and nondepressive patients.
Table 3 Descriptives and analysis of variance for depressive and nondepressive patients
Depressiveness
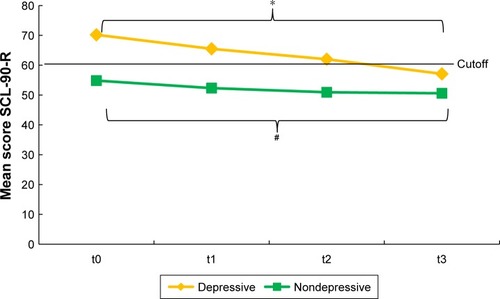
Analyses of variance revealed a significant decrease of depressive symptoms measured with the anxiety and depression scale (ADS) for depressive, F (3, 27)=9.063, P<0.001, ηp2=0.502, and nondepressive insomnia patients, F (3, 78)=5.208, P=0.002, ηp2=0.167. The interaction of time and group was significant, F (3, 105)=6.183, P=0.001, ηp2=0.15, which indicated a significant difference between depressive and nondepressive patients and their depressiveness over time. Remarkably, depressive patients reported an ADS mean score of 31.30 at baseline and 16.84 at follow-up, which is below the cutoff score for indicating a depressive disorder. Post hoc analysis showed a significant decrease from baseline to post measurement, P=0.028, and follow-up, P=0.003, for depressive patients. For nondepressive patients, only marginally significant decreases were revealed between baseline and follow-up, P=0.052, and premeasurement to post measurement, P=0.083, and follow-up, P=0.071 ().
Figure 1 Mean scores of ADS scale for depressive and nondepressive patients over time.
Abbreviation: ADS, anxiety and depression scale.
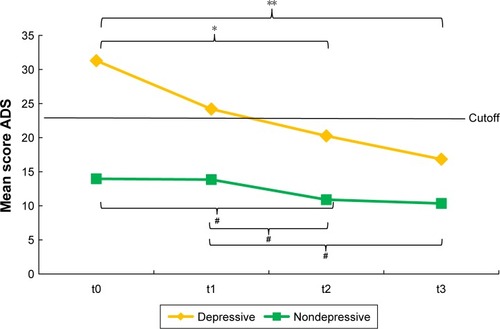
Severity of depression measured with the SCL-90-R showed a main effect of time for depressive, F (3, 27)=5.912, P=0.003, ηp2=0.369, and nondepressive patients, F (3, 78)=2.428, P=0.072, ηp2=0.085, as well as a significant interaction, F (3, 105)=6.183, P=0.001, ηp2=0.15. Post hoc analyses revealed a significant decrease of depressive symptoms between baseline and follow-up, P=0.029, for depressive and a marginally significant decrease for nondepressive patients, P=0.076 ().
Discussion
The main goal of this study was to examine the effects of a sleep intervention, which combines CBT-I and HT-I techniques, to treat insomnia patients with and without depression. Data of 37 patients were implemented for statistical analyses, in which 10 patients suffered additionally from depression. Sleep parameters, depression, and psychological distress were assessed at four measurement times: 8 weeks before intervention (baseline), right before (premeasurement) and after the intervention (post measurement), and 3 months later (follow-up).
Patients suffering from insomnia and comorbid depression responded differently to this intervention regarding several sleep parameters than insomnia patients without depressive symptoms. Whereas the latter group’s SOL remained firm under the clinical cutoff of 30 minutes for all four measurement points, depressive patients showed a decrease in SOL from baseline to post measurement and a slightly elevated score at follow-up. These results are in line with previous studies such as Taylor et al and Trauer et al, who also reported a reduction in SOL.Citation42,Citation44 Although both groups did not significantly differ at baseline, patients with insomnia and comorbid depression exceeded the clinical cutoff, supposedly due to their comorbidity, which might lead to more thoughts that are negative and rumination, as well as a higher presleep arousal.Citation23 In the study by Hsu et al, an intervention contributed to the reduction of patients’ presleep arousal and an improvement of sleep parameters.Citation23 Furthermore, anticipation and hope for therapy seemed to play a major role for these changes in depressive patients, due to a tremendous decline from baseline to pre and post measurement.Citation30 Nondepressed patients did not show these effects of anticipation; however, a higher level of psychological distress in the group of depressives might explain the clinical difference at baseline. Patients with insomnia and depression might be more pleased because of the opportunity of a therapy and the attention regarding their impairment.
For both groups, duration of WASO decreased and SE increased significantly, which is in line with results of Blom et al, Koffel et al, and Trauer et al;Citation5,Citation24,Citation44 SE raised up to >80% at posttreatment and follow-up. Even duration of WASO decreased by almost 50%, which then influences mood, SE, and regeneration. For depressive patients, regeneration enhanced significantly from baseline to follow-up, whereas this was not found for nondepressives. One explanation can be the significant difference between these two groups at baseline and the comorbidity of insomnia and depression. Finally, mood in the morning and evening, as well as TST remained stable over time for both groups. Koffel et al found elevated TST after treatment, though, only small effects were reported.Citation24 For depressive patients, TST increased from 357 minutes at baseline to 405 minutes at follow-up. Due to the high level of variance, this difference was not significant.
Furthermore, depressive symptomatology over time differed for depressive patients in contrast to the nondepressive group. Depressive insomnia patients decreased their ADS score from baseline to post and follow-up significantly, whereas nondepressed patients showed no such changes. This result is in line with results from Bélanger et al, Holdevici, and Koffel et al.Citation4,Citation21,Citation24 Importantly, after CBT-I treatment, depressive patients scored below the cutoff score, indicating no clinical abnormality. This result is very important, meaning that such a sleep intervention reduces sleep parameters as well as depressive symptoms in patients suffering from both disorders.
Limitations
However, several limitations have to be listed. For example, the implementation of further insomnia-specific questionnaires as the Insomnia Severity Index would be helpful to evaluate more precisely insomnia-specific outcomes. Besides, more detailed dropout analysis might enhance the quality of the results. However, most participants reported at the end of the treatment an enhancement regarding their sleep quality and mental health, but not all filled in the full set of questionnaires and sleep logs for a further measurement. Therefore, future research should add either treatment costs or award systems for every completed data set.
Besides, future research could investigate the issue that different parts of an intervention have different effects on sleep behavior, especially focusing on patients suffering from insomnia and comorbidities.Citation31 On the one hand, components like stimulus control and sleep deprivation appeared to be more effective, whereas sleep hygiene alone showed no effect on sleep. Furthermore, the use of cognitive strategies rather than focusing on the physiological arousal seemed superior.Citation31 A meta-analysis by Friedrich and Schlarb about psychological sleep interventions for college students with sleep problems revealed that CBT elements were most effective, whereas relaxation, which includes hypnotherapy, showed a high level of variance regarding effect sizes.Citation17 Furthermore, the course of insomnia and depression might be mediated by various other variables, eg, presleep arousal, self-efficacy, and sleep-related beliefs.Citation39 Gałuszko-Węgielnik et al reported a decrease in psychophysiological arousal after CBT-I, but did not investigate the impact of arousal on treatment success regarding sleep parameters.Citation19 The level of stress vulnerability, though, did not influence this effect.Citation19 All these factors should be taken into account in further studies addressing insomnia patients with comorbid disorders or symptoms.
Conclusion
An intervention combining CBT-I and HT-I is effective in reducing depressive symptoms and improving various sleep parameters in adults with insomnia comorbid with depression, whereas patients with isolated insomnia showed these enhancements on less sleep parameters. Therefore, nonresponders to other forms of therapy, eg, pharmacological, interpersonal, or cognitive-behavioral therapy, could benefit from a combined therapy including hypnotherapy. The additional effect of hypnotherapy itself should be part of future research. Mediator variables influencing the course of insomnia should be considered.
Acknowledgments
We acknowledge support for the Article Processing Charge by the Deutsche Forschungsgemeinschaft and the Open Access Publication Fund of Bielefeld University.
Disclosure
The authors report no conflicts of interest in this work.
References
- AshworthDKSlettenTLJungeMA randomized controlled trial of cognitive behavioral therapy for insomnia: an effective treatment for comorbid insomnia and depressionJ Couns Psychol201562211512325867693
- BaglioniCBattaglieseGFeigeBInsomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studiesJ Affect Disord20111351–3101921300408
- BaglioniCNanovskaSRegenWSleep and mental disorders: A meta-analysis of polysomnographic researchPsychol Bull2016142996999027416139
- BélangerLHarveyAGFortier-BrochuÉImpact of comorbid anxiety and depressive disorders on treatment response to cognitive behavior therapy for insomniaJ Consult Clin Psychol201684865966726963600
- BlomKJernelövSKraepelienMInternet treatment addressing either insomnia or depression, for patients with both diagnoses: a randomized trialSleep201538226727725337948
- BreslauNRothTRosenthalLAndreskiPSleep disturbance and psychiatric disorders: a longitudinal epidemiological study of young adultsBiol Psychiatry19963964114188679786
- BrunelloNArmitageRFeinbergIDepression and sleep disorders: clinical relevance, economic burden and pharmacological treatmentNeuropsychobiology200042310711911015028
- BuysseDJAngstJGammaAAjdacicVEichDRösslerWPrevalence, course, and comorbidity of insomnia and depression in young adultsSleep200831447348018457234
- CordiMJHirsigerSMérillatSRaschBImproving sleep and cognition by hypnotic suggestion in the elderlyNeuropsychologia20156917618225660206
- CordiMJSchlarbAARaschBDeepening sleep by hypnotic suggestionSleep20143761143115224882909
- Deutsche Gesellschaft für Schlafmedizin und Schlafforschung (DGSM) [German Association for Sleep Medicine]Fachinformationen: Fragebögen. Schlaftagebücher in der Diagnostik von Insomnien [Technical information: questionnaires. Sleep diaries for the diagnosis of insomnia] Available from: http://www.dgsm.de/fachinformationen_frageboegen_schlaftagebuecher.phpAccessed July 27, 2018 German
- DoerrJPHirscherVRiemannDVoderholzerUStörungen des Tiefschlafs und psychische Erkrankungen [Deep sleep disorders and mental disorders]Nervenarzt2018813347354 German
- DrakeCLRoehrsTRothTInsomnia causes, consequences, and therapeutics: an overviewDepress Anxiety200318416317614661186
- EdingerJDOlsenMKStechuchakKMCognitive behavioral therapy for patients with primary insomnia or insomnia associated predominantly with mixed psychiatric disorders: a randomized clinical trialSleep200932449951019413144
- FrankeGHDie Symptom-Checkliste von Derogatis: Manual. SCL-90-R; Deutsche version [The Symptom-Checklist by Derogatis. German version. Manual]GöttingenBeltz Test GmbH1995 German
- FranzenPLBuysseDJSleep disturbances and depression: risk relationships for subsequent depression and therapeutic implicationsDialogues Clin Neurosci200810447348119170404
- FriedrichASchlarbAALet’s talk about sleep: a systematic review of psychological interventions to improve sleep in college studentsJ Sleep Res201827142228618185
- FurihataRUchiyamaMSuzukiMAssociation of short sleep duration and short time in bed with depression: A Japanese general population surveySleep Biol Rhythms2015132136145
- Gałuszko-WęgielnikMJakuszkowiak-WojtenKWigluszMSCubałaWJLandowskiJThe efficacy of Cognitive-Behavioural Therapy (CBT) as related to sleep quality and hyperarousal level in the treatment of primary insomniaPsychiatr Danub201224Suppl 1S51S5522945187
- HautzingerMBailerMDie Allgemeine Depressionsskala. Manual. [The General Anxiety Scale ADS]GöttingenBeltz Test GmbH1993
- HoldeviciIRelaxation and Hypnosis in Reducing Anxious-depressive Symptoms and Insomnia among AdultsProcedia Soc Behav Sci2014127586590
- Jansson-FröjmarkMLindblomKA bidirectional relationship between anxiety and depression, and insomnia? A prospective study in the general populationJ Psychosom Res200864444344918374745
- HsuHMChouKRLinKCChenKYSuSFChungMHEffects of cognitive behavioral therapy in patients with depressive disorder and comorbid insomnia: A propensity score-matched outcome studyBehav Res Ther20157314315026313621
- KoffelEAKoffelJBGehrmanPRA meta-analysis of group cognitive behavioral therapy for insomniaSleep Med Rev20151961624931811
- KrahnLEPsychiatric disorders associated with disturbed sleepSemin Neurol2005251909615798941
- LamTHChungKFYeungWFYuBYYungKPNgTHHypnotherapy for insomnia: a systematic review and meta-analysis of randomized controlled trialsComplement Ther Med201523571973226365453
- LovatoNLackLWrightHKennawayDJPredictors of improvement in subjective sleep quality reported by older adults following group-based cognitive behavior therapy for sleep maintenance and early morning awakening insomniaSleep Med201314988889323871260
- LuikAIZuurbierLAWhitmoreHHofmanATiemeierHREM sleep and depressive symptoms in a population-based study of middle-aged and elderly personsJ Sleep Res201524330530825581509
- MarotiDFolkesonPJansson-FröjmarkMLintonSJDoes Treating Insomnia With Cognitive–Behavioural Therapy Influence Comorbid Anxiety and Depression? An Exploratory Multiple Baseline Design With Four PatientsBehaviour Change20112804195205
- MohrDCHoJHartTLControl condition design and implementation features in controlled trials: a meta-analysis of trials evaluating psychotherapy for depressionTransl Behav Med20144440742325584090
- MorinCMCulbertJPSchwartzSMNonpharmacological interventions for insomnia: a meta-analysis of treatment efficacyAm J Psychiatry19941518117211808037252
- NgBYLeeTSHypnotherapy for sleep disordersAnn Acad Med Singapore200837868368818797562
- Norell-ClarkeAJansson-FröjmarkMTillforsMHolländareFEngströmIGroup cognitive behavioural therapy for insomnia: Effects on sleep and depressive symptomatology in a sample with comorbidityBehav Res Ther201574809326433466
- NuttDWilsonSPatersonLSleep disorders as core symptoms of depressionDialogues Clin Neurosci200810332933618979946
- OkajimaIKomadaYInoueYA meta-analysis on the treatment effectiveness of cognitive behavioral therapy for primary insomniaSleep Biol Rhythms2011912434
- PerlisMLGilesDEBuysseDJTuXKupferDJSelf-reported sleep disturbance as a prodromal symptom in recurrent depressionJ Affect Disord1997422–32092129105962
- RiemannDPerlisMLThe treatments of chronic insomnia: a review of benzodiazepine receptor agonists and psychological and behavioral therapiesSleep Med Rev200913320521419201632
- RiemannDBaumECohrsSS3 Leitlinie Nichterholsamer Schlaf/Schlafstörungen – Kapitel “Insomnie bei Erwachsenen” (AWMF-Registernummer 063-003) [German S3 guidelines for nonrestorative sleep and sleep disorders – Chapter “Insomnia in Adults”]; Update 2016Somnologie201721244 German
- SchwartzDRCarneyCEMediators of cognitive-behavioral therapy for insomnia: a review of randomized controlled trials and secondary analysis studiesClin Psychol Rev201232766467522935473
- SmithMTPerlisMLWho is a candidate for cognitive-behavioral therapy for insomnia?Health Psychol2006251151916448293
- SpiegelhalderKRegenWNanovskaSBaglioniCRiemannDComorbid sleep disorders in neuropsychiatric disorders across the life cycleCurr Psychiatry Rep201315636423636987
- TaylorDJLichsteinKLWeinstockJSanfordSTempleJRA pilot study of cognitive-behavioral therapy of insomnia in people with mild depressionBehav Ther2007381495717292694
- TaylorHLRybarczykBDNayWLeszczyszynDEffectiveness of a CBT Intervention for Persistent Insomnia and Hypnotic Dependency in an Outpatient Psychiatry ClinicJ Clin Psychol201571766668325907406
- TrauerJMQianMYDoyleJSRajaratnamSMCunningtonDCognitive Behavioral Therapy for Chronic Insomnia: A Systematic Review and Meta-analysisAnn Intern Med2015163319120426054060
- TsaiY-LChenC-WChengH-CChangC-HChenC-YYangC-MCognitive and behavioral factors in insomnia comorbid with depression and anxietySleep Biol Rhythms2013114237244
- van HoudenhoveLBuyseBGabriëlsLvan den BerghOTreating primary insomnia: clinical effectiveness and predictors of outcomes on sleep, daytime function and health-related quality of lifeJ Clin Psychol Med Settings201118331232121629999
- WagleyJNRybarczykBNayWTDanishSLundHGEffectiveness of abbreviated CBT for insomnia in psychiatric outpatients: sleep and depression outcomesJ Clin Psychol201369101043105523109266
- WatanabeNFurukawaTAShimoderaSCost-effectiveness of cognitive behavioral therapy for insomnia comorbid with depression: Analysis of a randomized controlled trialPsychiatry Clin Neurosci201569633534325205008