Abstract
Background
No significant effect of psychological treatment has been reported from meta-analysis of subthreshold depression patients and control subjects at 1-year follow-up. However, behavioral activation is a simpler and more cost-effective treatment than cognitive behavioral therapy. The primary purpose of this study was to assess by comparison to an assessment-only control group whether the effects of behavioral activation program for depressive symptoms can persist up to 1-year follow-up without the use of antidepressants or other psychotherapy.
Patients and methods
Late adolescent students were the population targeted in this study. Participants were allocated randomly to an intervention group (n=62) or a control group (n=56). Treatment consisted of five-weekly 60-minute sessions. Participants underwent a structured interview and completed self-report scales at 1 year post-assessment.
Results
Late adolescent students receiving treatment had significantly lower mean Beck Depression Inventory, second edition scores at 1-year follow-up than control group students. The effect size (Hedges’ g) for between-group differences at 1-year follow-up was −0.41.
Conclusion
Our behavioral activation program is simple and short. Nevertheless, the results obtained at 1-year follow-up of the control group and late adolescent students receiving treatment indicated a significant difference in their Beck Depression Inventory, second edition scores. Our 5-week behavioral activation program based on behavioral characteristics for subthreshold depression might be promising for subthreshold depression. The sample examined for this study imposed some study limitations.
Introduction
Subthreshold depression is defined as the exhibition of clinically significant depressive symptoms that do not meet the diagnostic criteria for major depressive disorder (MDD).Citation1 Subthreshold depression is a major risk factor for subsequent development of more severe depressive symptoms.Citation2–Citation5 The probability of MDD is known to increase steadily during adolescence, that is, 12–20 years.Citation6 Although not meeting the full criteria, subthreshold depression has been associated with severe problems such as negative impact on academic performance and social activities,Citation7 which might be as severe as those associated with full depression.Citation8
An earlier report described that the use of antidepressant medication by adolescent patients is associated with a modestly increased risk of suicidality.Citation9 It is, therefore, especially important to assess the effectiveness of psychological treatment programs only, without antidepressants, for late adolescents with subthreshold depression. Several earlier reports of studies with longer follow-up (1 year) have described that cognitive behavioral therapy (CBT) can reduce the risk of MDD.Citation10–Citation12 Nevertheless, a meta-analysis of psychological treatments for subthreshold depression found no significant effect of psychotherapy for depressive symptoms at 1-year follow-upCitation13 and found no significant effect of CBT on the incidence of MDD at follow-up.Citation13
For adolescent and late adolescent patients with depression, earlier reports have described behavioral activation as an effective treatment.Citation14,Citation15 For university students with moderately depressive symptoms, behavioral activation was found to have significantly greater reduction in depressive symptoms from pretreatment to posttreatment.Citation16 Although the meta analysis of behavioral activation for children and adolescents reported that behavioral activation was effective from pretreatment to posttreatment, the long-term effect has not yet been elucidated for children and adolescent patients.Citation17 An earlier systematic review of behavioral activation programs for depression revealed an effect size of −0.35 (Hedges’ g) in comparison with control conditions at 6–9 months of follow-up.Citation18 The effectiveness of behavioral activation in follow-up might not have a sufficient effect. No report of the relevant literature describes a study that examined the long-term efficacy of brief behavioral activation for subthreshold depression. Recently, we conducted a randomized controlled trial (RCT) to examine the efficacy of a brief five-session behavioral activation program for late adolescent patients with subthreshold depression.Citation19 Results demonstrated that late adolescent students receiving this treatment exhibited significantly greater improvement in self-reported depressive symptoms than the assessment-only control group. The effect size was Hedges’ g of −0.90.Citation19 It has not been reported whether the effects of this behavioral activation program can be maintained over the long term.
Therefore, the primary purpose of this study was to assess whether a behavioral activation program without antidepressants for depressive symptom can be maintained for depressive symptoms up to 1 year and be compared with the assessment-only control group. The secondary aim was to explore whether the behavioral activation program can decrease the risk of developing MDD or not.
Patients and methods
Research design
Details of the study design of this RCT were presented in an earlier report (UMIN000011967).Citation19 The 1-year follow-up study was already planned in the original RCT. Furthermore, the same student sample as that examined in an earlier studyCitation19 was followed up 1 year later in the present study.
Procedures
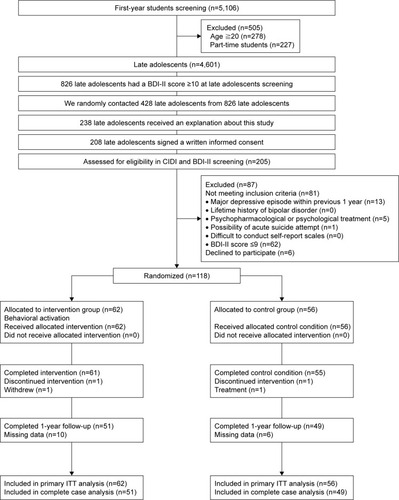
Details of procedures of this RCT were presented in an earlier report.Citation19 Participants were recruited from Hiroshima University over a 2-year period during 2013–2014 (). The Beck Depression Inventory, second edition (BDI-II) is administered annually to all first-year students of the university as a part of their health examination, which is conducted at the Health Service Center of Hiroshima University. We randomly selected the first-year students with a BDI-II score ≥10 using the Microsoft Excel randomization function. Recruitment took place through email at a public information sharing center. Then, we held a meeting to explain the study contents. After all the participants had signed a written informed consent form, participants received the Composite International Diagnostic Interview (CIDI) and completed self-report scales via the Internet. An expert of the Department of Clinical Research, who was independent of the research team that conducted this study, developed a sequential assignment list using computer-generated random numbers to allocate the participants to a treatment or a control group randomly at a 1:1 ratio. The random sequence was stratified by sex and depression severity during screening (BDI-II score ≤13, BDI-II score ≥14). The group allocation was masked in the entry and in the CIDI assessment. A psychiatrist interviewed the participants and assessed the risk of a future acute suicide attempt if a participant had a history of attempted suicide based on CIDI criteria. Furthermore, participants who met the criteria for a possible acute suicide attempt received counseling from a psychiatrist. Participants joined the RCT.Citation19 We contacted the participants by email and telephone 1 year later. Participants received telephone interviews by CIDI and completed self-report scales via the Internet 1 year after the assessment by blind testers who did not know the allocation. In CIDI assessment of 1-year follow-up, allocation to the treatment group or control group was masked.
Participants
We recruited late adolescent students with subthreshold depression during a 2-year period of 2013–2014 at Hiroshima University in Japan. For this study, the inclusion criteria were the following: 18–19-year-old first-year university student at Hiroshima University, BDI-II score ≥10 according to earlier studies,Citation20,Citation21 participants who did not have a major depressive episode during the previous year as determined by the structured clinical interview with the CIDI, and not undergoing psychopharmacological or psychological treatment. The exclusion criteria were the following: a lifetime history of bipolar disorder according to earlier studies,Citation20–Citation24 possibility of an acute suicidal attempt, difficulty understanding the study purpose, or having a severe physical disease and “difficulty in completing self-report scales”.
Intervention
Our behavioral activation program consisted of five-weekly 60-minute sessions. The program emphasized increased access to positive reinforcement activities to improve the rate of response-contingent positive reinforcement. Our behavioral activation program was modeled after the behavioral activation component of a CBT program developed based on earlier studies of adult depression in the USACitation25,Citation26 and which has been demonstrated in an RCT to be effective for subthreshold depression in the workplace in Japan.Citation21 Details of intervention of this RCT can be found in an earlier report.Citation19
Control group
The control group participants were examined for outcome measures. They received baseline, posttreatment, and follow-up assessments at approximately the same time as the intervention group did. The control group participants in this study received no medical treatment, usual care, or any educational information.
Measures
Primary outcome
The Japanese version of the BDI-II
BDI-II consists of 21 self-report items scored on a four-point scale. It is used to measure depressive symptoms.Citation27 Good reliability and validity have been reported for the Japanese version of BDI-II.Citation28 BDI-II was administered at baseline, at the end of treatment, and at 1-year follow-up. The primary outcome of this report is BDI-II scores at 1-year follow-up. The internal consistencies of the BDI-II in pretreatment, posttreatment, and 1-year follow-up were assessed using Cronbach’s α. The internal consistencies for all time BDI-II were also acceptable: pretreatment α=0.79, posttreatment α=0.74, and 1-year follow-up α=0.87.
Secondary outcome
Composite International Diagnostic Interview
The CIDI is a structured interview for assessing mental disorders.Citation29 Good reliability and validity have been reported for the Japanese ver 3.0 of the CIDI.Citation30 We used the Japanese 3.0 version of the CIDI in screening and 1-year follow-up. We assessed for 12-month history of MDD, generalized anxiety disorder, panic disorder, social phobia, and post-traumatic stress disorder. In addition, each participant was assessed for the lifetime history of bipolar disorder. Because earlier reports have described the comorbidity rate for depression and anxiety as high,Citation31 we included generalized anxiety disorder, panic disorder, social phobia, and post-traumatic stress disorder in screening for this study.
We administered CIDI to the participants before baseline and at 1-year follow-up. At the follow-up assessment, we limited the time frame to the previous year to ascertain the new incidence of MDD. The secondary outcome of this report is the incidence of MDD during 1 year of follow-up.
Sample size calculation
Sample size calculations were conducted at the study design stage.Citation19
An earlier report described a mean effect size of d=0.87 in behavioral activation group vs a control group at posttest.Citation32 The mean effect size found for psychotherapies for sub-threshold depression was d=0.42.Citation13 Because effect sizes suggest that d=0.5 indicates a medium effect,Citation33 we set the effect size in our study as a medium effect (d=0.50). We estimated a minimum of 64 participants in each group at the study design stage (power=0.80 and α=0.05, d=0.50 for an unpaired t-test). Therefore, the power might be insufficient to detect differences in incidence of MDD that occurs over 1 year.
Statistical analysis
All statistical analyses were conducted using software (SPSS Statistics 22; IBM Corp.).
Primary outcome analysis
The primary purpose of this study was exploratory examination of whether behavioral activation program effects persisted at 1-year follow-up. The primary point was estimation of the intervention effect on depressive symptoms between the original assigned groups at 1-year follow-up. Analysis of variance with repeated measures is limited to cases with complete data or with imputation of missing data. Some statistical approaches are useful for dealing with missing data that do not necessarily require formal imputation methods.Citation34 For example, the linear mixed model for repeated measure approach was used for analyzing outcomes measured repeatedly over time.Citation34–Citation36 To examine the effects of treatment on primary outcomes at 1-year follow-up, the primary analysis was conducted using a linear mixed model for repeated measures. The random effects of this model were intercepts. Therefore, because individual differences are explained as a variable effect, the mode of analysis of this research is a model showing change from the individual baseline. The model predictors were categorical time (pretreatment, post-treatment, 1-year follow-up), treatment condition, and time × treatment interaction as fixed effects. We applied intention-to-treat (ITT) analysis between the original assigned groups. We conducted post hoc analysis if an interaction was found. Effect sizes were calculated and reported as Hedges’ gCitation37 for between-group differences in 1-year follow-up, using the observed standard error (SE) at follow-up.
Some participants might not complete the full protocol of a longitudinal study. Sensitivity analyses can be conducted using different approaches to ascertain how robust the primary analysis is for the chosen method for handling missing data.Citation34 For sensitivity analysis, we conducted a complete case analysis to assess the discrepancy between ITT and complete case analysis.
Secondary exploratory outcome analysis
Next, we applied Cox proportional hazard analysis for exploratory assessment of the differences in time for the development of MDD between the intervention group and the control group to adjust for lifetime diagnosis of MDD. In CIDI, participants who met the criteria for MDD reported the time that participants developed depressive symptoms.
Ethics approval
Approval for the study was obtained from the ethics committee of Hiroshima University. All participants signed a written informed consent form.
Results
Participant enrollment
presents the study flow. Of the 208 students who gave their informed consent to participate, 205 (98.6%) completed screening. The mean score of BDI-II during screening was 13.53. Then, the 108 participants who satisfied all the eligibility criteria were allocated randomly to the intervention or control group (). The BDI-II average score of the sample consisting of 118 students was 13.02. One intervention group participant dropped out. One control group participant underwent psychopharmacological or psychological treatment during 5 weeks. At 1-year follow-up, seven intervention group participants did not complete the CIDI and self-report scales. Three intervention group participants had undergone psychopharmacological or psychological treatment during the follow-up period. Five control group participants did not complete the CIDI and self-report scales. One control group participant had undergone psychopharmacological or psychological treatment during the follow-up. Therefore, missing data of the intervention group were those of ten participants from posttreatment to 1-year follow-up. Missing data of the control group were those of six participants from posttreatment to 1-year follow-up. No significant difference was found in the rates of missing data (χ2 (1)=0.73, P=0.43).
Table 1 Descriptive data of groups
Depressive symptoms (primary outcome)
Results obtained from a linear mixed model
The primary point was estimation of the intervention effect on depressive symptoms between the original assigned groups at 1-year follow-up. To assess the effects of treatment on primary outcomes at 1-year follow-up, primary analysis was conducted using a linear mixed model for a repeated measures approach in the original assigned groups (62 participants in the intervention group and 56 participants in the control group). Significant interaction was found between groups and times (F value=9.01, degrees of freedom=216.45, P<0.01; ). Significant difference was found between the mean estimates for the intervention group and the control group at 1-year follow-up (intervention group, mean estimate=11.00, SE=0.89, 95% CI: 9.24 to 12.76; control group, mean estimate=13.83, SE=0.91, 95% CI: 12.00 to 15.61; estimated mean difference=2.83, 95% CI: 0.28 to 5.33, P=0.03), as shown in . The effect size (Hedges’ g) for between-group differences at 1-year follow-up was -0.41 (95% CI: −0.77 to −0.04). Additionally, a significant difference was found in the mean estimates between the intervention group and control group at posttreatment (intervention group, mean estimate=7.03, SE=0.84, 95% CI: 5.38 to 8.68; control group, mean estimate=12.77, SE=0.88, 95% CI: 11.03 to 14.51; estimate mean difference=5.74, 95% CI: 3.34 to 8.14, P<0.01). The effect size (Hedges’ g) for between-group differences in 1-year follow-up was −0.87 (95% CI: −1.24 to −0.49).
Table 2 Results of linear mixed model
Figure 2 Changes in BDI-II score from pretreatment to 1-year follow-up.
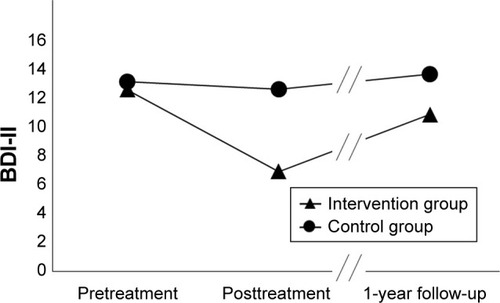
Next, because this study had missing data, we conducted complete case analysis (intervention group, n=51; control group, n=49) and then conducted sensitivity analysis and examined the discrepancy between ITT and complete case analysis. Significant interaction was found between groups and times (F value=9.42, degrees of freedom=196, P<0.01; ). Significant difference was found between the mean estimates for the intervention group and the control group at 1-year follow-up (intervention group, mean estimate=10.77, SE=0.93, 95% CI: 8.91 to 12.60; control group, mean estimate=13.83, SE=0.96, 95% CI: 11.90 to 15.65; estimated mean difference=3.01, 95% CI: 0.39 to 5.63, P=0.03). The effect size (Hedges’ g) for between-group differences at 1-year follow-up was −0.45 (95% CI: −0.85 to −0.05). Additionally, a significant difference was found in estimated means between the intervention group and the control group at posttreatment (intervention group, mean estimate=6.45, SE=0.93, 95% CI: 4.62 to 8.29; control group, mean estimate=12.77, SE=0.96, 95% CI: 10.95 to 14.69; estimated mean difference=6.37, 95% CI: 3.75 to 8.99, P<0.01). The effect size (Hedges’ g) for between-group differences at 1-year follow-up was −0.90 (95% CI: −1.33 to −0.51). No discrepancy was found between the results of ITT and complete case analysis.
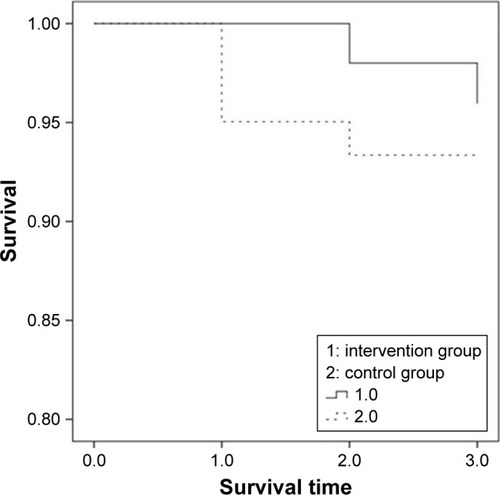
Prophylactic effects for onset of MDD
We assessed the significance of differences between the intervention group (n=51) and the control group (n=49) in developing MDD during the 1-year follow-up. In CIDI, participants who met the criteria for MDD responded that they had developed depressive symptoms. In addition, participants reported the time as 1) within 1 month, 2) between 2 and 6 months, and 3) between 7 and 12 months after baseline assessment.
Two participants in the intervention group developed MDD during 1-year follow-up (one participant within the previous 1 month, one participant in the previous 2–6 months: 2/51, 3.92%). Four control group participants developed MDD (one participant 2–6 months before, three participants 7–12 months before: 4/49, 8.16%). Three participants of the intervention group and eight participants in the control group had an MDD history longer than 1 year before the screening of this study. We applied Cox proportional hazard analysis to assess differences in survival probabilities between the intervention group and the control group. We used the MDD history as a covariate. No significant difference was found in these results (χ2=2.51, P=0.11; ).
Discussion
Results of linear mixed modeling for a repeated measures approach show that late adolescent students receiving treatment had significantly different BDI-II scores from those of the control group at 1-year follow-up. The effect size for between-group differences at 1-year follow-up was −0.41. Next, we conducted a complete case analysis and performed sensitivity analysis necessary to examine the discrepancy between ITT and a complete case analysis. The effect size of complete case analysis for between-group differences in 1-year follow-up was -0.45. Results showed no discrepancy between ITT analysis and complete case analysis. Sensitivity analysis can be done using a different approach to assess the robustness of the primary analysis to the chosen method for handling missing data.Citation34 Therefore, the primary analysis of this study is regarded as robust. An earlier study, a meta-analysis of psychological treatments for subthreshold depression, found no significant effect of psychotherapies for depressive symptoms between an intervention group and a control group at 1-year follow-up.Citation13 An earlier study of college students found no significant effect for the CBT group on depressive symptoms compared to either bibliotherapy or brochure controls at either 3- or 6-month follow-up.Citation38 Results of our earlier report indicated that late adolescents with subthreshold depression had a lower frequency of environmental rewards than healthy late adolescents.Citation39 Our behavioral activation program emphasized increased access to positive reinforcement activities to improve the rate of response-contingent positive reinforcement. These results demonstrate that late adolescent students receiving treatment had significantly different BDI-II scores from those of the assessment-only control group at 1-year follow-up.
However, the effect size for between-group differences at 1-year follow-up was −0.41. The effect size of intervention can be regarded as small. Our earlier study revealed the effect size of behavioral activation program as -0.90 for between-group differences in acute treatment.Citation19 Therefore, the behavioral activation program effect decreased during 1 year. Moreover, we attempted to ascertain whether a 5-week short-term behavioral activation program can decrease the risk of developing MDD compared to a control group or not. Results of Cox proportional hazard analysis revealed no significant difference between the intervention group and the control group in the incidence of MDD. Although a significant difference was found in the depressive symptoms at 1-year follow-up between the intervention group and the control group, one must interpret the results carefully. In terms of the considerable reduction in effects between posttreatment and follow-up, although some earlier studies conducted booster sessions or continuation sessions to maintain the effects of intervention,Citation40,Citation41 we conducted no such booster sessions. The knowledge that continued support would be provided via booster sessions might have reinforced participants’ confidence in managing depression or anxiety.Citation42 An earlier report described from a meta-analysis that CBT intervention with a booster session is more effective in terms of sustainability than CBT interventions without booster sessions.Citation42 To maintain behavioral activation effects, it is necessary to review activities in booster sessions. Moreover, it is very difficult to obtain large effects if baseline depressive symptoms are as low as they were in this study. Furthermore, the behavioral activation intervention was very brief. It can be regarded as a low-intensity intervention. Therefore, long-term effects of such treatment might be less likely to be apparent.
Some study limitations are related to the sample used for this study. The sample size calculations were conducted at the study design stage. However, this sample size was based on the study design of an earlier study.Citation19 An earlier report described that 200 participants per condition must be tested for a difference in the incidence rate.Citation40 Although we assessed differences in the incidence of MDD between the intervention group and the control group in a preliminary study, the sample size of this study was small. A future study using a large sample size must be undertaken to examine the incidence of MDD. Secondly, in this study, we confirmed whether the participants were undergoing psychopharmacological or psychological treatment in CIDI or not. Participants who were not undergoing psychopharmacological or psychological treatment were included in this study. We confirmed the current treatment in this study. Therefore, future studies must be conducted to target people who have never received psychopharmacological or psychological treatment. Despite the limitations described above, the results of this study show a significant difference in BDI-II scores between the intervention group and the control group at 1-year follow-up.
Conclusion
Although our behavioral activation program is simple and brief, the results obtained at 1-year follow-up indicate a significant difference between the BDI-II scores of the late adolescent control group students and the students receiving treatment. Our 5-week behavioral activation program based on behavioral characteristics for subthreshold depression appears to be promising for treating subthreshold depression.
Author contributions
All authors contributed to the design, acquisition of data, interpretation of data drafting, and critical revision of the paper, and agree to be accountable for all aspects of the work. All authors have approved the final article.
Acknowledgments
This study was supported by Grants-in-Aid for Scientific Research on Innovative Areas, Grant Numbers 16H06395 and 16H06399 from Japan Society for the Promotion of Science, and Grant Number 23118004 from the Ministry of Education, Culture, Sports, Science and Technology, Japan. No funding entity influenced the results or presentation of the study results. The authors would like to thank all participants.
Disclosure
The authors have no conflict of interest, financial or otherwise, related to this study.
References
- PincusHADavisWWMcqueenLE‘Subthreshold’ mental disorders. A review and synthesis of studies on minor depression and other brand namesBr J Psychiatry199917428829610533546
- BerthaEABalázsJSubthreshold depression in adolescence: a systematic reviewEur Child Adolesc Psychiatry2013221058960323579389
- FergussonDMHorwoodLJRidderEMBeautraisALSuicidal behaviour in adolescence and subsequent mental health outcomes in young adulthoodPsychol Med200535798399316045065
- JohnsonJGCohenPKasenSMinor depression during adolescence and mental health outcomes during adulthoodBr J Psychiatry2009195326426519721119
- JinninROkamotoYTakagakiKDetailed course of depressive symptoms and risk for developing depression in late adolescents with subthreshold depression: a cohort studyNeuropsychiatr Dis Treat201713253328053534
- RohdePBeeversCGSticeEO’NeilKMajor and minor depression in female adolescents: onset, course, symptom presentation, and demographic associationsJ Clin Psychol200965121339134919827116
- BalázsJMiklósiMKeresztényAAdolescent subthreshold-depression and anxiety: psychopathology, functional impairment and increased suicide riskJ Child Psychol Psychiatry201354667067723330982
- González-TejeraGCaninoGRamírezRExamining minor and major depression in adolescentsJ Child Psychol Psychiatry200546888889916033637
- HammadTALaughrenTRacoosinJSuicidality in pediatric patients treated with antidepressant drugsArch Gen Psychiatry200663333233916520440
- ClarkeGNHawkinsWMurphyMSheeberLBLewinsohnPMSeeleyJRTargeted prevention of unipolar depressive disorder in an at-risk sample of high school adolescents: a randomized trial of a group cognitive interventionJ Am Acad Child Adolesc Psychiatry19953433123217896672
- ClarkeGNHornbrookMLynchFA randomized trial of a group cognitive intervention for preventing depression in adolescent offspring of depressed parentsArch Gen Psychiatry200158121127113411735841
- ImamuraKKawakamiNFurukawaTADoes Internet-based cognitive behavioral therapy (iCBT) prevent major depressive episode for workers? A 12-month follow-up of a randomized controlled trialPsychol Med20154591907191725562115
- CuijpersPSmitFvan StratenAPsychological treatments of sub-threshold depression: a meta-analytic reviewActa Psychiatr Scand2007115643444117498154
- MccauleyEGudmundsenGSchloredtKThe Adolescent Behavioral Activation Program: adapting behavioral activation as a treatment for depression in adolescenceJ Clin Child Adolesc Psychol201645329130425602170
- WallisARoegerLMilanSWalmsleyCAllisonSBehavioural activation for the treatment of rural adolescents with depressionAust J Rural Health2012202959622435770
- GawrysiakMNicholasCHopkoDRBehavioral activation for moderately depressed university students: randomized controlled trialJ Couns Psychol2009563468475
- MartinFOliverTBehavioral activation for children and adolescents: a systematic review of progress and promiseEur Child Adolesc Psychiatry Epub2018223
- EkersDWebsterLvan StratenACuijpersPRichardsDGilbodySBehavioural activation for depression; an update of meta-analysis of effectiveness and sub group analysisPLoS One201496e10010024936656
- TakagakiKOkamotoYJinninRBehavioral activation for late adolescents with subthreshold depression: a randomized controlled trialEur Child Adolesc Psychiatry201625111171118227003390
- Allart-van DamEHosmanCMHHoogduinCALSchaapCPDRThe coping with depression course: short-term outcomes and mediating effects of a randomized controlled trial in the treatment of subclinical depressionBehav Ther2003343381396
- FurukawaTAHorikoshiMKawakamiNTelephone cognitive–behavioral therapy for subthreshold depression and presenteeism in workplace: a randomized controlled trialPLoS One201274e3533022532849
- ImamuraKKawakamiNFurukawaTAEffects of an Internet-based cognitive behavioral therapy (iCBT) program in Manga format on improving subthreshold depressive symptoms among healthy workers: a randomized controlled trialPLoS One201495e9716724844530
- SpekVNyklícekISmitsNInternet-based cognitive behavioural therapy for subthreshold depression in people over 50 years old: a randomized controlled clinical trialPsychol Med200737121797180617466110
- VázquezFLTorresABlancoVDíazOOteroPHermidaEComparison of relaxation training with a cognitive–behavioural intervention for indicated prevention of depression in university students: a randomized controlled trialJ Psychiatr Res201246111456146322939979
- SimonGELudmanEJTuttySOperskalskiBvon KorffMTelephone psychotherapy and telephone care management for primary care patients starting antidepressant treatment: a randomized controlled trialJAMA2004292893594215328325
- WangPSSimonGEAvornJTelephone screening, outreach, and care management for depressed workers and impact on clinical and work productivity outcomes: a randomized controlled trialJAMA2007298121401141117895456
- BeckATSteerRABrownGKBeck Depression Inventory: Manual2nd edAntonioSTexasThe Psychological Corp1996
- KojimaMFurukawaTJapanese Version of the Beck Depression Inventory2nd edTokyoNippon-Hyoron-sha Co2003
- KesslerRCÜstünTBThe World Mental Health (WMH) Survey Initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI)Int J Methods Psychiatr Res20041329312115297906
- KawakamiNTakeshimaTOnoYTwelve-month prevalence, severity, and treatment of common mental disorders in communities in Japan: preliminary finding from the World Mental Health Japan Survey 2002–2003Psychiatry Clin Neurosci200559444145216048450
- HirschfeldRMThe comorbidity of major depression and anxiety disorders: recognition and management in primary carePrim Care Companion J Clin Psychiatry20013624425415014592
- CuijpersPvan StratenAWarmerdamLBehavioral activation treatments of depression: a meta-analysisClin Psychol Rev200727331832617184887
- CohenJStatistical Power Analysis for the Behavioral Sciences2nd edHillsdale, NJErlbaum Associates1998
- ThabaneLMbuagbawLZhangSA tutorial on sensitivity analyses in clinical trials: the what, why, when and howBMC Med Res Methodol2013139223855337
- PetersSABotsMLden RuijterHMMultiple imputation of missing repeated outcome measurements did not add to linear mixed-effects modelsJ Clin Epidemiol201265668669522459429
- SonHFriedmannEThomasSAApplication of pattern mixture models to address missing data in longitudinal data analysis using SPSSNurs Res201261319520322551994
- HedgesLVDistribution theory for Glass’s estimator of effect size and related estimatorsJ Educ Stat198162107128
- RohdePSticeEShawHGauJMCognitive–behavioral group depression prevention compared to bibliotherapy and brochure control: nonsignificant effects in pilot effectiveness trial with college studentsBehav Res Ther201455485324655464
- TakagakiKOkamotoYJinninRBehavioral characteristics of subthreshold depressionJ Affect Disord201416847247525128753
- Allart-van DamEHosmanCMHoogduinCASchaapCPPrevention of depression in subclinically depressed adults: follow-up effects on the ‘Coping with Depression’ courseJ Affect Disord2007971–321922816860874
- GarberJClarkeGNWeersingVRPrevention of depression in at-risk adolescents: a randomized controlled trialJAMA2009301212215222419491183
- GearingRESchwalbeCSLeeRHoagwoodKEThe effectiveness of booster sessions in CBT treatment for child and adolescent mood and anxiety disordersDepress Anxiety201330980080823596102