Abstract
This systematic literature review investigates the use of technology for the coordination and management of mental health care with an emphasis on outcomes. Searches of MEDLINE/PubMed, Scopus, and EMBASE were conducted between January 1, 2003, and January 4, 2018, to identify articles that assessed patient outcomes associated with care coordination, evaluated technology to improve care, or discussed management of mental health care using technology. A total of 21 articles were included in a qualitative review based on the recommendations set forth by the PRISMA statement. Among the various health technologies, electronic health records were most commonly used for care coordination, with primary care being the most frequent setting. Care coordination was shown to provide easier patient access to health care providers and to improve communication between caregiver and patient, especially in cases where geographic location or distance is a challenge. Barriers to coordinated care included, but were not limited to, insufficient funding for health information technology, deficient reimbursement plans, limited access to technologies, cultural barriers, and underperforming electronic health record templates. In conclusion, many studies showed the benefit of coordinated and collaborative care through the use of technology; however, further research and development efforts are needed to continue technological innovation for advanced patient care.
Plain language summary
Use of technology is rapidly changing the health care landscape. In the field of mental health particularly, technology has the potential to overcome some of the barriers currently experienced by the inadequate and overburdened mental health care system in the United States. A systematic review of selected studies published between January 2003 and January 2018 was conducted to investigate the value of using technology for care coordination/collaborative care in mental health. Multiple studies have reported on the use of technologies such as electronic health records (EHRs), telemedicine, and Web-based communication for coordinating care, most frequently in primary care and community health centers. Among the various mental health conditions, coordinated care has most frequently been implemented for individuals with depression. Benefits of technology-based care coordination were evident across many areas, including screening, scheduling assessments, accessing patient information, facilitating communications, and improving treatment compliance. However, integration of technology into routine mental health care continues to remain challenging because of barriers including, but not limited to, cost, access, and usability of health technology. Although overall findings for collaborative care models have been encouraging, few studies have reported integration of technology into care models. Further studies are needed to realize the potential of technology in improving collaborative care for individuals with mental health disorders.
Introduction
Mental and behavioral health issues are leading causes of disability in adults,Citation1,Citation2 with depression being the leading cause of disability and suicide.Citation3 The treatment of patients with mental health conditions is an ongoing challenge that requires novel approaches. According to the 2017 National Council for Behavioral Health report, the number of practicing psychiatrists is declining, and by 2025, the demand may exceed supply by 6,090–15,600 psychiatrists.Citation4 It is well known that mental health care in the United States tends to be fragmented and inadequate for maintaining continuity of care, thereby impairing patient quality of life and potentially contributing to the high health care costs.Citation5 Mental health conditions can adversely affect adherence to therapy and associated medical outcomes,Citation6 further underscoring the need for a concerted effort among a patient’s various care providers. One approach to addressing these challenges has been to use coordinated care, which involves active organization of patient care and information sharing among all care participants.Citation7 Collaborative care has been shown to be effective at reducing symptoms and improving patient satisfaction with treatment,Citation8–Citation10 with particular benefits for patients with depression or substance abuse.Citation6,Citation11
One example of a well-studied collaborative care model was developed as part of the Improving Mood – Promoting Access to Collaborative Treatment (IMPACT) study.Citation8 Recognizing the need for a more comprehensive approach to the management of depression among older adults, the IMPACT investigators conducted a randomized trial of comprehensive vs usual care across 18 primary care clinics in the United States. The IMPACT program was based on prior evidence-based models, collectively promoting collaboration (among primary care physicians, specialists, and patients), personalized treatment plans, follow-up and outcomes assessment by a depression care manager, targeted referrals to specialists, and stepped care protocols. Patients randomized to usual care were to use their discretion in selecting any available primary care and specialist services. With a 12-month follow-up, the results showed that comprehensive care resulted in higher rates of antidepressant and psychotherapy use, greater satisfaction with care, significantly lower depression severity scores, and increased treatment response and complete remission rates. Additionally, the estimated cost was modest, at US$533 per patient for 1 year. The published experience with the IMPACT program for managing older adults with depression did not specify the type of technology used to facilitate the coordination of care among providers and between providers and patients, but it preceded the advent and widespread use of smart phones and other digital technology that has substantial potential to enhance patient monitoring and support ongoing communication. For example, telemedicine technology has been shown to improve outcomes in patients with depression who receive care from small primary care clinics that lack on-site specialized psychiatric services.Citation12 Results from the Clinical and Cost-Effectiveness of Collaborative Care for Depression in UK Primary Care Trial also show the benefits of a care coordination approach in patients with mental health conditions.Citation10 The objective of this multicenter, randomized controlled trial was to compare the effectiveness of collaborative care vs care as usual (CAU) in patients (n=581) with moderate to severe depression. Collaborative care was associated with a significant improvement in depression scores at 4 months compared with CAU, with benefits persisting through the 12-month follow-up.
A variety of technologies have been examined for their use in achieving interdisciplinary communication and coordination of care. Telemedicine aims to improve patient health through the use of real-time interactive communication between physicians and patients at distant sites using audio, video, or other electronic equipment.Citation13 EHRs can promote coordinated care by allowing clinicians to readily update patient health information and distribute it to other authorized providers in disparate care settings.Citation14 Web-based communication tools can aid in collaborative decision making and patient–provider communication by offering a means for patients to establish goals, view test results and medications, and identify care team members.Citation15 The agent-based simulation model was designed to help represent the complex modes of engagement between patients and care providers (the agents) and medical and social ecosystems and has been used to test and predict the effects of care coordination approaches.Citation16
Given the growing digitalization of health care and need for thoughtful and informed technology integration in mental health care, this systematic literature review was undertaken to evaluate the published literature regarding the role of technology as part of a care coordination approach compared with CAU in patients with mental health conditions. Specific objectives included determination of which technologies are being evaluated for their use as part of a coordinated care approach, how such technologies are being implemented, and benefits and barriers to these approaches for patients with mental health conditions compared with CAU.
Materials and methods
Information sources and literature search
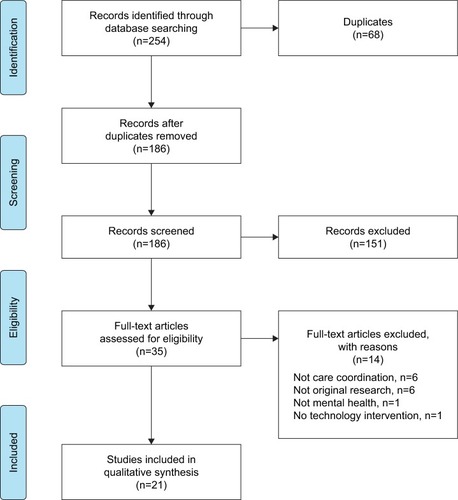
This systematic literature review was conducted based on recommendations outlined by the PRISMA statement.Citation17 Searches of MEDLINE/PubMed, Scopus, and EMBASE were used to identify articles published between January 1, 2003, and January 4, 2018. The initial search was conducted with an end date of May 20, 2015; subsequent to delays, updated searches were performed with end dates of January 10, 2017, and January 4, 2018. The search terms were derived from examination of known publications on the topic and iterative test searches to evaluate success in identifying known publications with minimal false positives. The following search terms were used: (“mental health” OR “mental healthcare” OR “psychiatric health” OR “psychiatric healthcare” OR “behavioral health” OR “behavioural health” OR “behavioral healthcare” OR “behavioural healthcare”) AND “technology” AND (“care coordination” OR “integrated care” OR “collaborative care” OR “care collaboration” OR “care integration” OR “coordinated care” OR “patient registries” OR “population health management”) AND (Electronic Health Record OR Disease management OR Health home OR Person Centered Medical Home OR Behavioral Health Home).
Article selection and data extraction
Inclusion criteria for the initial search were English-language articles providing data (preliminary or pilot data were not subject to exclusion) on outcomes associated with use of technology as part of a care coordination program in the care of patients with mental health issues, including, but not limited to, behavioral health, substance abuse, and high-risk populations. Exclusion criteria were congress abstract, review/opinion paper, lack of reporting on mental or behavioral health, and lack of inclusion of technology for care coordination intervention. Screeners used an Excel spreadsheet designed for this review that included exclusion criteria as drop-downs.
Following initial database searches, duplicates were removed, and the title and abstract of each retrieved article were screened against the inclusion and exclusion criteria by two randomly assigned authors. A third author screened articles for which assessments were discordant. Articles that passed this initial screening step then underwent full-text review against the same inclusion and exclusion criteria by all authors. Data were extracted using a spreadsheet prepopulated with the categories of information to be extracted. This was accomplished by two reviewers, one of whom extracted key data (eg, mental health diagnosis, location of study, patient population, type of technology, and type of care coordination center) and one of whom verified the extracted data, with any disagreements reconciled via discussion.
Results
Study selection
Study identification, screening, and eligibility are summarized in . In total, literature database searches retrieved 254 articles; after removing 68 duplicates, 186 articles were screened. During screening, 151 articles were excluded, resulting in 35 full-text articles that were assessed for eligibility. A total of 14 studies were excluded during full-text review, and the remaining 21 articles were included in the qualitative synthesis ().
Study characteristics
Overall, eight studies identified barriers to coordinated careCitation18–Citation25 (), and 13 studiesCitation9,Citation12,Citation16,Citation26–Citation35 () did not specifically mention challenges facing care coordination, five of whichCitation9,Citation12,Citation18,Citation34,Citation35 were specifically designed to compare the collaborative care model to CAU (). Mental health illnesses addressed in the reviewed articles included dementia (n=2),Citation18,Citation27 suicide (n=1),Citation28 substance abuse (n=4),Citation22,Citation24,Citation28,Citation31 posttraumatic stress disorder (PTSD; n=2),Citation32,Citation33 schizophrenia (n=1),Citation32 anxiety (n=1),Citation35 and depression, the most prevalent mental health condition assessed for collaborative care (n=9).Citation9,Citation12,Citation18,Citation20,Citation26–Citation28,Citation34,Citation35
Table 1 Characteristics of studies that identified barriers to care coordination
Table 2 Characteristics of studies not identifying barriers to care coordination
Technologies and health care models to implement coordination of care
The majority of studies used health information technologies to coordinate care among patients and providers, including computer cognitive behavior therapy,Citation35 agent-based simulation modeling,Citation16 density mapping technology,Citation27 telemedicine,Citation12,Citation26,Citation32,Citation33 and Internet Web-based communication.Citation9,Citation18,Citation20,Citation24,Citation25 EHRs were the most common health information technology used.Citation12,Citation18,Citation19,Citation21–Citation23,Citation26,Citation29,Citation30 A single study used the Aging Brain Care Medical Home model to facilitate care coordination.Citation18
Care coordination setting
A variety of health care centers were used to assist collaborative care efforts. The majority of care coordination took place within primary care centers (n=8),9,19,22,25,28,31,34,35 followed by community health centers (n=4),Citation19,Citation21,Citation22,Citation31 the veterans integrated health care system (n=5),Citation12,Citation26,Citation30,Citation32,Citation33 the correctional health system,Citation29 and independent living facilities.Citation27 Seven studies examined coordinated care in rural areas.Citation9,Citation12,Citation22,Citation24,Citation26,Citation31,Citation32 One studyCitation16 did not specify a care coordination setting.
Benefits of care coordination technologies
EHRs were the most commonly assessed technology for care coordination (n=9).12,18,19,21–23,26,29,30 In a survey of 101 collaborative care offices, 95% of primary care physicians and 87% of mental health clinicians used EHRs.Citation23 Across three studies, the identified advantages of using EHRs included increased shared access of patient information between providers;Citation22 high satisfaction with billing, scheduling, and screening for mental health;Citation23 and utility in promoting human rights for patients with mental illness in the correctional system.Citation29 A single study showed the utility of touch screen technology with wireless tablet computers for mental health screening.Citation28 Assessing mental illness and suicidality among youth with tablets and Web-based computer services allowed 74% of youth reporting suicidal thoughts (n=152/205) to be triaged on the same day for a mental health evaluation, with 65% receiving mental health service within 6 months.Citation28 A single study observed that compliance with an injury-specific template use by correctional health care providers increased by 25% when EHRs were modified, allowing more accurate injury surveillance in prisons.Citation29 A retrospective case-by-case study demonstrated the benefits of density-mapping technology to coordinate mental health assessments and interventions using motion density mapping and infrared motion sensors in patients with dementia.Citation27 In an agent-based simulation model, the inclusion of care coordination across medical and social systems (with an increase in patient handoff success rate between providers that ranged from 5%–15%) resulted in increased rates of compliance with medication by 3.5%–5.5% and patient appointment by 3%–12%.Citation16
The benefits of facilitating coordinated care over a distance using telemedicine technologies was shown in several studies (n=4).Citation12,Citation26,Citation32,Citation33 A study of distant telemedicine-based collaborative care for depression management found that patients receiving collaborative care (n=177) were more adherent at 6 months (OR, 2.1; P=0.04) and 12 months (OR, 2.7; P=0.01) and more satisfied at both time points (6 months: OR, 1.8 [P=0.01]; 12 months: OR, 1.7 [P=0.03]) when compared with CAU (n=218).Citation12 Implementing care coordination using a Web-based tracking and decision aid for major depression in primary care centers also showed favorable outcomes; collaborative care (n=101) was more effective for achieving treatment response (50% reduction in depressive symptom score) than CAU (n=49) at 3 months (OR, 5.2 [95% CI, 1.41–16.09]) and 9 months (OR, 5.6 [95% CI, 1.40–22.58]).Citation9
Care coordination among the military veteran population was examined in six studies.Citation12,Citation24,Citation26,Citation30,Citation32,Citation33 Among the veterans involved in a study of individualized telemedicine technology, 94% reported satisfaction with their technology device at 12 months, and 88% reported improved communication with their health care provider.Citation32 Coordinated care for veterans with substance abuse via Internet-based interventions showed a decrease in days of alcohol use from 2.8 to 1.5 days (P=0.038); patients on parole, from 42% to 30% (P=0.005); and duration of depression, from 11.6 to 8.2 days (P=0.024) during the program.Citation24 Integrating mental health care within a primary care facility using technology to coordinate care for patient assessment was shown to be effective for veterans, with 75% of referred patients receiving all of their treatments within the primary care clinic itself; reducing new appointment wait times, improving adherence to evidence-based treatments for depression, and increasing patient satisfaction.Citation30
Barriers to using technology in care coordination
The implementation of coordinated care for mental health continues to face challenges, especially related to cost, usability, and integration of EHRs. Eight studies identified barriers to implementing care coordination ();Citation18–Citation25 these barriers were related to provider setting (n=7)Citation18–Citation23,Citation25 and patient engagement (n=3).Citation18,Citation24,Citation25
The challenges to implementing technology in coordinated care as a result of barriers within a provider setting included lack of financial resources and investments for health information technology (n=2),Citation18,Citation21 inadequate reimbursements (n=2),Citation21,Citation22 and poor EHR templates.Citation19 Two studies mentioned the poor interdisciplinary integration of EHRs and their steep learning curves.Citation19,Citation23 In an observational, cross-case comparative study of 11 health care centers, Cifuentes et al found many challenges to integrating EHRs, including lack of templates supporting shared care plans between primary and behavioral health providers, limited interoperability between EHRs and tablet devices, and double documentation with duplicate data entry for practices using two different EHRs.Citation19 Zeman et al described similar experiences when implementing computerized behavioral health assessment in four primary clinics.Citation25 Challenges related to technology included determining what type of technology to use for assessments and software version issues between devices.Citation25 In an Assessment of Behavioral Health Services survey evaluating integrated care, of the 390 health center responses, only one in five (20%) reported joint conferences, and co-management of care between primary and behavioral health staff was reported in only 35% of institutions.Citation22 The barriers to patient engagement in other studies included limited access to technologies and poor Internet connections (n=1),Citation24 along with cultural barriersCitation18 and lack of patient willingness and engagement in completing psychiatric evaluations (n=1).Citation25
Benefits of care coordination technology for specific mental health conditions
Fortney et al enrolled a large patient population (n=395), 82% of whom reported major depression, to evaluate telemedicine-enhanced collaborative care for depression management in a rural setting.Citation26 As mentioned previously, those randomized to telemedicine-enhanced care had better medication adherence and better outcomes at the 6- and 12-month time points when compared with CAU.Citation12 In a separate article, the development of a Web-based decision aid was proposed with the goal of facilitating coordinated care by enhancing patient registries, patient scheduling, and clinical decisions for patient encounters with automated progress note generation.Citation20 Results from a randomized controlled trial of collaborative care delivered by telephone and coordinated through EHRs demonstrated favorable outcomes in highly anxious patients. At the 12-month follow-up, patients who received this intervention (n=250) had improved mental health–related quality of life (effect size [ES], 0.38 [95% CI, 0.13–0.63]; P=0.003), improved anxiety (ES, 0.30 [0.05–0.55]; P=0.02), and improved mood (ES, 0.45 [0.19–0.71]; P=0.001) when compared with CAU (n=79).Citation35 In an observational study over 36 months, use of a distant Internet-based monitoring program found that patients with traumatic brain injury and PTSD reported more frustration and poorer independence than those with traumatic brain injury alone.Citation33
The implementation of a technology-supported collaborative care program for patients with Alzheimer’s dementia disease (n=153) led to patients having fewer symptoms at 12 months and rating their primary physician more favorably when compared with CAU.Citation18 For patients with substance abuse disorders, coordination of care in federally qualified health centers was proposed, with the goals of eHealth integrated technology via mobile devices improving the cost-effectiveness of treatment and the lives of these patients.Citation31 Furthermore, using health information technology for patients with substance abuse was shown to markedly decrease the need for outpatient treatment (P=0.001) at the 6-month follow-up.Citation24 Wodarski and Green reported that a program that incorporated text or e-mail reminders and communications, online counseling and recovery support, and virtual community and peer support was effective in improving outcomes for patients with substance abuse problems in a rural community.Citation24 A two-arm randomized controlled study of adults with comorbid depression and obesity (target n=404) showed increased weight loss and reduced depression severity in patients receiving integrated care via health monitoring, including Fitbit and mobile devices, compared with CAU.Citation34
Discussion
This literature review has identified both benefits and challenges to implementing technology for care coordination for patients with mental health conditions. The application of technology helps fill a gap in communication between health care providers and allows patients more comfort in disclosing their mental health issues.Citation28 By integrating mental health care and technologies, a collaborative approach can allow physicians structured patient assessment, improved patient care, and increased monitoring of patient health. Studies of coordinated care vs CAU have shown that coordinated mental health care and implementation of technology allow patients to be more involved in their health care decisions and have greater control of their treatment and progress, especially for depressive disorder.Citation8,Citation9 Moreover, the use of technology to facilitate coordinated care can result in greater adherence to guidelines and standards by health care providers when compared with CAU.
Establishing coordinated care with technology for patients at high risk, including individuals who are in prison and veterans, can be of added value to address mental health in these demographics. People in prisons face a high degree of morbidity related to mental illness, including psychosis, depression, anxiety, substance abuse, and PTSD.Citation36 With nearly 10 million imprisoned individuals worldwide, one in seven faces a mental illness, increasing their chances for suicide, violence, self-harm, and victimization. Additionally, there remains a lack of psychopharmacologic research in treatment outcomes for this patient group.Citation37 Patients with mental illness tend to face high rates of incarceration,Citation38 and implementing health information technology to correctional health systems with modified EHR templates can help identify vulnerable patients in this setting and allow enhanced documentation of their mental health and injuries while protecting their human rights.Citation29 The veteran population similarly requires attention, and the RAND Center for Military Health Policy Research reports that 18.5% of returning military personnel meet the criteria for PTSD or depression and 19.5% face traumatic brain injury. This figure estimates that nearly 600,000 veterans returning from active duty may be experiencing mental health issues. Moreover, there remains a gap in patient care for this group because 50% of patients who meet the criteria for mental health illness do not receive treatment or do not seek care. Of those receiving care, only half receive adequate treatment, and there remains lack of health monitoring, placing a high burden of cost on the health system.Citation39
The application of technology can be especially beneficial for populations living in rural areas that lack adequate access to mental health care. The US Department of Health and Human Services has identified 4,000 underserved areas without adequate mental health professionals,Citation40 which is substantial considering that depression and anxiety affect 2.6 million and 1.1 million rural patients, respectively.Citation41
A notable barrier to care coordination has been the financial constraints associated with investing in the technology needed to strengthen a facility’s ability to coordinate care,Citation18 particularly in rural areas where patients have limited access to computers, laptops, and adequate Internet connection.Citation24 Federal initiatives like the Health Information Technology for Economic and Clinical Health Act of 2009Citation42 and added financial assistance to community health centers have resulted in increased and faster adoption of health information technology like EHRs.Citation21
As observed throughout this review, primary care facilities are the most prevalent centers in organizing collaborative care efforts and therefore are vital for care coordination of mental health conditions. The rate of mental health diagnosis and treatment among primary care physicians has increased for children and adults.Citation38 Furthermore, examination of primary care centers finds that patients with depression tend to have persistent symptoms despite adequate treatment from their primary care physician. By increasing education and frequency of visits by a psychiatrist, collaborative care can increase a patient’s medication adherence, improve their quality of life,Citation43 and improve their mental health status and depression symptomology.Citation44
This systematic review showed a number of research gaps. The majority of studies identified focused on EHRs to coordinate care, and our review suggests a knowledge gap regarding newer e-health technologies such as mobile devices and cell phone apps to facilitate coordinated care. New technologies, including mobile devices and cell phone applications, can be of added value for modern day coordinated care and clinical decision-making efforts.Citation45 Given the broad range of mental health illnesses, there were limited articles found to encompass the full range of disease pathology to collaborate coordinated care, with a majority of articles focusing on depression. Other potentially serious mental health conditions that could benefit from collaborative care outside of depression include eating disorders, anxiety disorders, psychotic disorders, personality disorders, and obsessive-compulsive disorders. Many studies focused on EHRs, but several studies also focused on telemedicine to coordinate care. Although these modes of collaborative care are useful, there is a need for greater inclusion of and research into new wearable device technology, including accelerometers, gyroscopes, smart fabrics,Citation46 and health monitors. The nearly US$25 billion global market for digital health technologiesCitation47 such as mobile health apps and biometric sensors reflects the growing influence of technology on modern medicine. With the global shift toward digitalization, it is important for clinicians to take an active role in evaluating health care technologies with respect to their ability to provide effective coordinated care and optimize treatment outcomes for their patients.
Our systematic review had several limitations. The search was limited to articles written in English; potentially relevant articles published in other languages were not captured. The selected studies could not be directly compared because of varying designs, endpoints, and attitude evaluation methods. A broader definition of type of technology or center could facilitate comparisons. In addition, comparisons were limited owing to varying technologies and differing mental health diseases. This review did not attempt to assess or evaluate the efficacy for any disease technology but rather provided an overview of the technologies and quality of research available in addressing coordinated care for mental health patients.
Conclusion
This literature review has demonstrated that although many studies have reported positive findings in collaborative care models, limited studies refer to new digital technologies to coordinate care for patients with mental health conditions. Primary care centers remain strategic partners in the health care system for collaborative care initiatives, especially in managing care coordination for mental health. The overall use of technology has shown positive strides in management of mental health care, and technology can be used not only for collaborative efforts but also to help patients with medication adherence and chronic disease management. Advances and portability of technologies will further enhance the positive efforts of care coordination.
Acknowledgments
This research was supported by ODH, Inc. (Princeton, NJ, USA). Editorial support for the preparation of this manuscript was provided by Mayur Kapadia, MD, of C4 MedSolutions, LLC (Yardley, PA, USA), a CHC Group company, with funding from ODH, Inc.
Disclosure
Erin Falconer is an employee of ODH, Inc.; David Kho was an employee of ODH, Inc. at the time the work was done. John P Docherty is an employee of Otsuka America Pharmaceutical, Inc. The authors report no other conflicts of interest in this work.
References
- AndersonPJané-LlopisEHosmanCReducing the silent burden of impaired mental healthHealth Promot Int201126Suppl 1i4i922079936
- World Health OrganizationThe Global Burden of Disease: 2004 UpdateGeneva, SwitzerlandWorld Health Organization2008
- World Health OrganizationDepression and Other Common Mental Disorders: Global Health EstimatesGeneva, SwitzerlandWorld Health Organization2017
- National Council Medical Director InstituteThe Psychiatric Shortage – Causes and SolutionsWashington, DCNational Council for Behavioral Health2017
- FalconerEEl-HayTAlevrasDIntegrated multisystem analysis in a mental health and criminal justice ecosystemHealth Justice201751428332099
- UnutzerJHarbinHSchoenbaumMDrussBThe collaborative care model: an approach for integrating physical and mental health care in Medicaid health homes2013 Available from: https://www.chcs.org/media/HH_IRC_Collaborative_Care_Model__052113_2.pdfAccessed July 25, 2018
- AHRQ [webpage on the Internet]Care Coordination2016 Available from: http://www.ahrq.gov/professionals/prevention-chronic-care/improve/coordination/index.htmlAccessed July 25, 2018
- UnützerJKatonWCallahanCMCollaborative care management of late-life depression in the primary care setting: a randomized controlled trialJAMA2002288222836284512472325
- HuijbregtsKMde JongFJvan MarwijkHWA target-driven collaborative care model for major depressive disorder is effective in primary care in the Netherlands. A randomized clinical trial from the depression initiativeJ Affect Disord2013146332833723068021
- RichardsDAHillJJGaskLClinical effectiveness of collaborative care for depression in UK primary care (CADET): cluster randomised controlled trialBMJ2013347f491323959152
- WoltmannEGrogan-KaylorAPerronBGeorgesHKilbourneAMBauerMSComparative effectiveness of collaborative chronic care models for mental health conditions across primary, specialty, and behavioral health care settings: systematic review and meta-analysisAm J Psychiatry2012169879080422772364
- FortneyJCPyneJMEdlundMJA randomized trial of telemedicine-based collaborative care for depressionJ Gen Intern Med20072281086109317492326
- Medicaid [webpage on the Internet]Telemedicine2018 Available from: https://www.medicaid.gov/medicaid/benefits/telemed/index.htmlAccessed July 25, 2018
- BurtonLCAndersonGFKuesIWUsing electronic health records to help coordinate careMilbank Q200482345748115330973
- DalalAKDykesPCCollinsSA web-based, patient-centered toolkit to engage patients and caregivers in the acute care setting: a preliminary evaluationJ Am Med Inform Assoc2016231808726239859
- KaltonAFalconerEDochertyJAlevrasDBrannDJohnsonKMulti-agent-based simulation of a complex ecosystem of mental health careJ Med Syst20164023926590977
- MoherDLiberatiATetzlaffJAltmanDGPRISMA GroupPreferred reporting items for systematic reviews and meta-analyses: the PRISMA statementPLoS Med200967e100009719621072
- CallahanCMBoustaniMAWeinerMImplementing dementia care models in primary care settings: the Aging Brain Care Medical HomeAging Ment Health201115151220945236
- CifuentesMDavisMFernaldDGunnRDickinsonPCohenDJElectronic health record challenges, workarounds, and solutions observed in practices integrating behavioral health and primary careJ Am Board Fam Med201528Suppl 1S63S7226359473
- FortneyJCPyneJMStevenCAA Web-based clinical decision support system for depression care managementAm J Manag Care2010161184985421348556
- JonesEWittieMAccelerated adoption of advanced health information technology in Beacon community health centersJ Am Board Fam Med201528556557526355128
- JonesEBKuLSharing a playbook: integrated care in community health centers in the United StatesAm J Public Health2015105102028203426270310
- ReitzRCommonKFifieldPStiasnyECollaboration in the presence of an electronic health recordFam Syst Health2012301728022429079
- WodarskiJSGreenPDHealth information technology: an expanded care coordination in rural TennesseeSoc Work Public Health201530543144226156399
- ZemanLLJohnsonDArfkenCSmithTOpokuPLessons learned: challenges implementing a personal digital assistant (PDA) to assess behavioral health in primary careFam Syst Health2006243286298
- FortneyJCPyneJMEdlundMJRobinsonDEMittalDHendersonKLDesign and implementation of the telemedicine-enhanced antidepressant management studyGen Hosp Psychiatry2006281182616377361
- GalambosCSkubicMWangSRantzMManagement of dementia and depression utilizing in-home passive sensor dataGerontechnology201311345746824049513
- GardnerWKlimaJChisolmDScreening, triage, and referral of patients who report suicidal thought during a primary care visitPediatrics2010125594595220385642
- Glowa-KollischSAndradeKStazeskyRData-driven human rights: using the electronic health record to promote human rights in jailHealth Hum Rights201416115716525474604
- PomerantzASShinerBWattsBVThe White River model of colocated collaborative care: a platform for mental and behavioral health care in the medical homeFam Syst Health201028211412920695670
- QuanbeckARGustafsonDHMarschLAIntegrating addiction treatment into primary care using mobile health technology: protocol for an implementation research studyImplement Sci201496524884976
- RyanPKobbRHilsenPMaking the right connection: matching patients to technologyTelemed J E Health200391818812699611
- SiddharthanKThe effect of post traumatic stress disorders on rehabilitation among combat-wounded veteransStud Health Technol Inform201218211412423138086
- MaJYankVLvNResearch aimed at improving both mood and weight (RAINBOW) in primary care: a type 1 hybrid design randomized controlled trialContemp Clin Trials20154326027826096714
- RollmanBBelnapHBRothenbergerDSOnline treatments for mood and anxiety disorders in primary care: a randomized controlled trialJ Gen Intern Med2016312S316S317
- BebbingtonPJakobowitzSMcKenzieNAssessing needs for psychiatric treatment in prisoners: prevalence of disorderSoc Psychiatry Psychiatr Epidemiol201752222122927878322
- FazelSHayesAJBartellasKClericiMTrestmanRMental health of prisoners: prevalence, adverse outcomes, and interventionsLancet Psychiatry20163987188127426440
- GliedSAFrankRGBetter but not best: recent trends in the well-being of the mentally illHealth Aff2009283637648
- TanielianTJaycoxHLSchellT webpage on the InternetInvisible wounds: mental health and cognitive care needs of America’s returning veterans2008 Available from: https://www.rand.org/pubs/research_briefs/RB9336.htmlAccessed April 6, 2018
- LycetteJNeglected – cancer care and mental health in rural AmericaN Engl J Med2016375232220222127959671
- ProbstJLaditkaSMooreGCHarunNPowellP webpage on the InternetDepression in rural populations: prevalence, effects on life quality, and treatment-seeking behavior2005 Available from: https://www.ruralhealthresearch.org/publications/226Accessed April 6, 2018
- GovernmentUSTitle XIII – Health Information Technology for Economic and Clinical Health ActWashington, DC111th Congress2009
- KatonWvon KorffMLinEStepped collaborative care for primary care patients with persistent symptoms of depression: a randomized trialArch Gen Psychiatry199956121109111510591288
- HedrickSCChaneyEFFelkerBEffectiveness of collaborative care depression treatment in Veterans’ Affairs primary careJ Gen Intern Med200318191612534758
- VentolaCLMobile devices and apps for health care professionals: uses and benefitsP T201439535636424883008
- AppelboomGCamachoEAbrahamMESmart wearable body sensors for patient self-assessment and monitoringArch Public Health20147212825232478
- DuggalRBrindleIBagenalJDigital healthcare: regulating the revolutionBMJ2018360k629335296