Abstract
Introduction
Postoperative delirium (POD) is a common complication of cardiac surgery associated with increased mortality, morbidity, and long-term cognitive dysfunction. Diabetic patients, especially those with poor diabetes control and long-standing hyperglycemia, may be at risk of developing delirium. The aim of this study was to analyze whether the occurrence of POD in cardiac surgery is associated with diabetes or elevated preoperative glycated hemoglobin (HbA1c) level.
Materials and methods
We performed a cohort analysis of prospectively collected data from a register of cardiac surgery department of a university hospital. Delirium assessment was performed twice a day during the first 5 days after the operation based on Diagnostic Statistical Manual of Mental Disorders, fifth edition criteria.
Results
We analyzed a cohort of 3,178 consecutive patients, out of which 1,010 (31.8%) were diabetic and 502 (15.8%) were diagnosed with POD. Patients with delirium were more often diabetic (42.03% vs 29.86%, P<0.001) and on oral diabetic medications (34.66% vs 24.07%, P<0.001), no difference was found in patients with insulin treatment. Preoperative HbA1c was elevated above normal (≥6%) in more delirious than nondelirious patients (44.54% vs 33.04%, P<0.001), but significance was reached only in nondiabetic patients (20.44% vs 14.86%, P=0.018). In univariate analysis, the diagnosis of diabetes was associated with an increased risk of developing POD (OR: 1.703, 95% CI: 1.401–2.071, P<0.001), but only for patients on oral diabetic medications (OR: 1.617, 95% CI: 1.319–1.983, P<0.001) and an association was noted between HbA1c and POD (OR: 1.269, 95% CI: 1.161–1.387, P<0.001). Multivariate analysis controlled for diabetes showed that POD was associated with age, heart failure, preoperative creatinine, extracardiac arteriopathy, and preoperative HbA1c level.
Conclusion
More diabetic patients develop POD after cardiac surgery than nondiabetic patients. Elevated preoperative HbA1c level is a risk factor for postcardiac surgery delirium regardless of the diagnosis of diabetes.
Introduction
Postoperative delirium (POD) is an acute central nervous system pathology commonly occurring after cardiac surgery.Citation1,Citation2 Delirium can be defined as an acute brain dysfunction manifested by fluctuation of mental status compared with baseline, inattention, altered level of consciousness, and disorganized thinking.Citation3 Both POD and intensive care unit (ICU) delirium have been linked to serious negative consequences, including postoperative cognitive dysfunction, prolonged mechanical ventilation, and prolonged hospital and ICU stay, as well as increased health care costs and long-term cardiovascular events after cardiac surgery.Citation4–Citation8 There are many modifiable and non-modifiable risk factors associated with delirium in critically ill patients.Citation9 A number of predisposing and accelerating risk factors contributed to postcardiac surgery delirium in previous studies.Citation10,Citation11 Getting more knowledge about risk factors in ICU delirium is important to increase our understanding of the pathophysiology and identification of patients at risk to prevent the condition and ultimately improve results.
Hyperglycemia is an important factor associated with increased mortality in critically ill patients in ICU and undergoing cardiac surgery.Citation12 It has been shown that insulin resistance and stress-induced hyperglycemia reflect the risk of death in critically ill patients.Citation13 Major randomized controlled trials aimed at proving that maintaining normoglycemia with targeted insulin therapy reduces morbidity and mortality were performed in surgical ICU patients.Citation14 Hyperglycemia during the perioperative period is common, particularly in patients undergoing cardiac surgery due to specific factors: administration of heparin, use of dextrose-containing cardioplegia solutions, cardiopulmonary bypass, and hypothermia.Citation15–Citation17
Based on previous studies of diabetes, glycemic variability, and mortality in critically ill patients, it can be assumed that diabetes and glycemic dysregulation identified by elevated preoperative glycated hemoglobin (HbA1c) level may be identified as a risk factor postcardiac surgery. Moreover, HbA1c is regarded as a good indicator of long-term (3 months) glycemic control and is the most commonly used biomarker to diagnose prediabetes and diabetes.Citation18–Citation20
For many years, diabetes has been reported to be associated with cognitive dysfunction, including vascular dementia and Alzheimer’s disease, yet the exact underlying pathology was not entirely elucidated.Citation21 Cognitive dysfunction in relation to brain glucose levels may be caused by one of the following causes: insulin resistance, altered glucose metabolism, vascular lesions, and/or β-amyloid and tau metabolism.Citation22 Similarly, it has been suggested that both hyperglycemia and hypoglycemia can be identified as risk factors associated with ICU delirium, but this was found in studies that were subject to various methodological limitations.Citation23,Citation24
Therefore, the hypothesis of this study was that the diagnosis of diabetes and/or elevated preoperative HbA1c level may be associated with the occurrence of POD in cardiac surgery.
Materials and methods
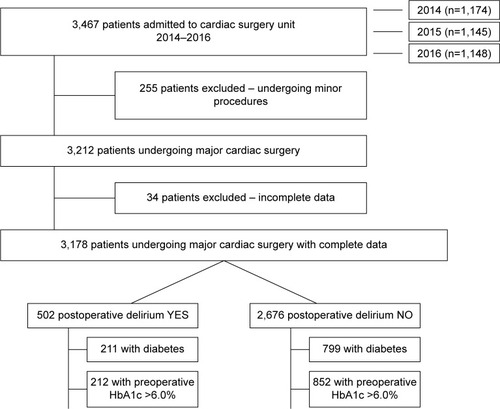
Prospectively collected data from a register of cardiac surgery department of a university hospital of Pomeranian Medical University in Szczecin, Poland, acquired during 3 consecutive years (2014–2016) were analyzed retrospectively. From the general cohort of patients undergoing cardiac surgery at our department during that time, we analyzed data regarding all patients for the presence or absence of POD and further analyzed only the diabetic cohort (). Finally, we included all patients undergoing major cardiac surgery (3,178 patients), irrespective of the type of surgery or case priority.
Prospectively collected database contains information regarding demographic data and concomitant medical conditions (coronary artery disease, congestive heart failure, hypertension, arrhythmia, diabetes mellitus or impaired glucose tolerance, renal disease, COPD, and smoking). Perioperative risk was calculated according to the EuroSCORE Logistics II scale.Citation25 Preoperative anesthetic assessment, as well as intraoperative surgical and anesthetic approach, was performed according to local guidelines and protocols. Standard pre- and postoperative laboratory blood analysis was performed, including preoperative HbA1c level. The dataset covered all major cardiac procedures performed under general anesthesia: coronary artery bypass grafting (CABG), CABG with concomitant valve operations (CABG + valve), isolated or multiple valve replacement and/or valve repair, transthoracic aortic valve implementation, ascending aorta aneurysm (AAA) surgery, and CABG with AAA surgery. All patients were anesthetized according to a local protocol, using a standard set of drugs and doses for each patient. After the operation, each patient remained intubated and mechanically ventilated and was transferred to the postoperative cardiac ICU. For postoperative pain control, multimodal analgesia was used. The postoperative outcome measures were ICU length of stay, hospital length of stay, and postoperative mortality at 30 days after the operation.
We used the following criteria for HbA1c level according to the American Diabetes Association: HbA1c <5.7% was regarded as normal, HbA1c 5.7%–6.4% was defined as prediabetes, and HbA1c >6.5% was defined as diabetes.Citation18 We also used the level >6.0% as the cutoff for the upper limit of the laboratory value for HbA1c at our institution.
In the postoperative period, all patients admitted to the postcardiac surgery ICU and cardiac surgery ward were screened for the presence of delirium by ICU physicians, cardiac surgeons, consultant neurologist, and nurses according to standard criteria of Diagnostic Statistical Manual of Mental Disorders, fifth edition (DSM-5) criteria for delirium, during the first 5 days after the operation.Citation3 The time frame of 5 days was chosen as it is the average hospitalization time and reflects early postcardiac surgery delirium. Standard delirium screening tools were not in use at the facility during data collection; delirium diagnosis was based on clinical assessment guided by DSM-5 criteria. DSM-5 diagnostic criteria for delirium are as follows: 1) disturbance in attention (ie, reduced ability to direct, focus, sustain, and shift attention) and awareness (reduced orientation to the environment); 2) disturbance developed over a short period of time (hours to days), changed from baseline, and fluctuated in severity during the course of a day; 3) additional disturbance in cognition (eg, memory deficit, disorientation, language, visuospatial ability, or perception). Moreover, criteria from 1 and 2 could not have been better explained by another condition, preexisting, established, or evolving neurocognitive disorder or coma, and there was no evidence from medical history, physical examination, and/or laboratory findings that the disturbance is a direct physiological consequence of another medical condition, substance intoxication or exposure to toxin, substance withdrawal, or because of multiple etiologies.Citation3 Delirium evaluation was performed twice daily by at least two health care professionals (doctor and/or nurse) after the patient has been weaned off mechanical ventilation and extubated. Data regarding delirium were further extracted from detailed nursing and medical staff charts.
Ethical statement
Retrospective nature of the analysis was the basis for a waiver from the Bioethical Committee of the Pomeranian Medical University in Szczecin, Poland, decision no KB-0012/79/01/18. Prospective data collection was performed according to the guidelines of the Declaration of Helsinki. Written informed consent for general anesthesia and surgery was obtained from each patient as part of routine preoperative document workup and included consent for data collection and medical record review. Patient confidentiality was ensured with the use of anonymous, dehumanified data.
Statistical analysis
We used descriptive statistics to characterize the study population, categorical variables were presented as proportions and analyzed using the chi-squared test, and continuous variables were presented as mean with SD. The incidence of delirium was calculated for patients with and without diabetes and Chi-square test or Chi-square test with Yates correction was used for comparison between both groups. The Shapiro–Wilk test was used to check normality of distribution. Data analysis for two groups was performed using a Mann–Whitney U test. Univariate logistic regression analysis for each variable was performed and presented as OR with 95% CIs. Multivariate logistic regression analysis was performed for risk factors that were significant in univariate analysis and presented with narrow CIs. All data were analyzed using licensed software Statistica 12 (StatSoft, Inc., Tulsa, OK, USA). P-value of <0.05 was regarded as statistically significant.
Results
We analyzed a cohort of 3,178 patients, out of which 1,010 (31.8%) were diabetic and 502 (15.8%) were diagnosed with POD. Study group characteristics regarding demographic data, concomitant diseases, and pre-, intra-, and postoperative parameters are shown in . Patients with POD were older (70 vs 65 years, P<0.001), more often had ischemic heart disease (P=0.026), diabetes (P<0.001), arterial hypertension (P=0.007), internal carotid artery stenosis (P<0.001), COPD (P<0.006), chronic (P<0.001) and acute renal failure (P=0.022), ejection fraction <30% (P<0.001), New York Heart Association III and IV (P<0.001), and extracardiac arteriopathy (P<0.001). When looking at preoperative data, HbA1c was significantly higher in patients with delirium (6.18±1.15 vs 5.91±0.95, P<0.001), as was creatinine level (P<0.001).
Table 1 Preoperative and perioperative characteristics of patients
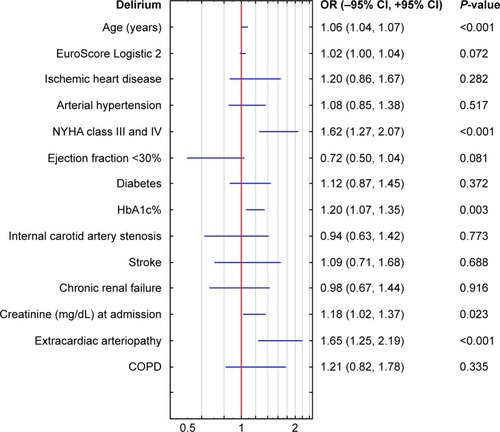
The univariate analysis confirms a relationship between chosen preoperative factors and postcardiac surgery delirium (). For diabetic patients, the OR for developing delirium was 1.703 (CI: 1.401–2.071, P<0.001). Moreover, an association was noted between HbA1c and POD (OR: 1.269, CI: 1.161–1.387, P<0.001). Multivariate analysis controlled for diabetes has shown that POD was associated with increasing age, heart failure, preoperative creatinine, extracardiac arteriopathy, and preoperative HbA1c level (OR: 1.20, 95% CI: 1.07–1.35, P=0.003) ().
Table 2 Univariate analysis including all preoperative variables associated with postoperative delirium after cardiac surgery
Therefore, we decided to perform a further analysis between HbA1c and different types of diabetes and the occurrence of POD after cardiac surgery. In the whole group of patients, preoperative HbA1c was elevated >6% more often in delirious than nondelirious patients (44.54% vs 33.04%, P<0.001), but significance was reached only in nondiabetic patients (20.44% vs 14.86%, P=0.018, ).
Table 3 Preoperative diabetes-related data and glycated hemoglobin for patients with and without delirium
Diabetes was associated with an increased risk of developing delirium (OR: 1.703, CI: 1.401–2.071, P<0.001), but only for patients on oral diabetic medications (OR: 1.617, CI: 1.319–1.983, P<0.001). Moreover, HbA1c level, elevated above 6.5%, was an independent risk factor for postcardiac surgery delirium (OR: 1.817, CI: 1.449–2.278, P<0.001), as seen in .
Table 4 Univariate diabetes-related variables associated with postoperative delirium after cardiac surgery
We aimed to look at the characteristics and outcome of diabetic patients and what factors determine the occurrence of postcardiac surgery delirium in diabetics. provides a summary of demographic and pre-, intra-, and postoperative factors.
Table 5 Preoperative and perioperative characteristics of diabetic patients
When analyzing postoperative complications (), in diabetic delirious patients, there were more episodes of stroke or TIA (7.11% vs 3.50%, P=0.021), atrial fibrillation (28.91% vs 17.77%, P<0.001), respiratory failure (22.27% vs 6.76%, P<0.001), pneumonia (9.00% vs 2.13%, P<0.001), but not sepsis. Interestingly, the mortality rate did not differ between the two groups (6.64% vs 5.26%, P = not significant). Both ICU length of stay (3.77±6.22, P<0.001) and hospital length of stay (15.61±18.34 vs 9.41±12.27, P<0.001) were longer in diabetics with delirium.
Table 6 Postoperative complications and outcome for diabetic patients with and without postcardiac surgery delirium
Discussion
The pathophysiology of postoperative and ICU delirium is not entirely understood, yet it is obvious that multiple predisposing conditions and precipitating factors are involved. In this study, we found that diabetes mellitus was associated with the development of POD in a large cohort of patients undergoing cardiac surgery. Moreover, patients who developed POD presented with elevated preoperative levels of HbA1c, regardless of the diagnosis of diabetes. To our knowledge, this is the first analysis to report on association between HbA1c level and delirium and to analyze the outcome of diabetic patients and nondiabetic patients in the light of POD occurrence.
The number of studies investigating the possible interplay between glucose, diabetes, HbA1c, and the incidence of postoperative or ICU delirium is very limited. Diabetes mellitus has been identified as a significant independent predictor of higher postoperative morbidity, increased incidence of delirium, and prolonged hospital stay after cardiac surgery.Citation26 There are three observational studies that reported hyperglycemia as a factor worsening the risk of delirium.Citation27–Citation29 Heymann et al aimed at finding an association between ICU delirium and blood glucose levels and performed a retrospective analysis and contrary to our results reported that diabetes had no influence on the onset of hyperactive delirium.Citation27 A retrospective analysis done by Ganai et al suggested a relationship between hyperglycemia and delirium in patients after abdominal surgery.Citation29
Factors associated with delirium include an upregulation of sympathetic tone and downregulation of parasympathetic tone due to surgical stress, impaired cholinergic function, reversible impairment of cerebral oxidative metabolism involvement of multiple neurotransmitter pathway abnormalities, and neuroinflammation.Citation30 Hyperglycemia is a known factor inducing inflammation (neuroinflammation) at the cellular level and a physiological response to inflammation, whereas the effect of insulin both endogenous and exogenous during treatment is not only to normalize glycemia but also anti-inflammatory.Citation31,Citation32 It has been shown that maintaining normoglycemia with insulin therapy improves survival and reduces morbidity in surgical ICU patients.Citation33 In critically ill patients undergoing cardiac surgery, the influence of abnormal blood glucose concentrations in the perioperative period on morbidity and mortality cannot be overestimated.Citation34,Citation35
Furthermore, it has been hypothesized that tight glucose control with insulin treatment would be a useful strategy to reduce the risk of POD. van Keulen et al performed a study to test the hypothesis that patients without diabetes who experienced glucose dysregulation (hypo- or hyperglycemia, or both) to be at higher risk of developing ICU delirium than patients with diabetes.Citation24 Contrary to our results, van Keulen et al reported that the diagnosis of diabetes mellitus was not associated with the development of ICU delirium. The authors found that hyperglycemia or both hypo- and hyperglycemia was associated with ICU delirium, yet only in nondiabetic patients.
Saager et al did a study in cardiac surgery patients aimed at testing the hypothesis that tight glucose control with a hyperinsulinemic strategy may reduce the risk of POD.Citation36 Contrary to their own hypothesis, the authors found that tight intraoperative glucose control with the use of normoglycemic hyperinsulinemic clamp actually increased the incidence but not severity of postcardiac surgery delirium. It is important to note that the authors recruited both patients with and without diabetes into their study, and within the diabetic group, both insulin and noninsulin-controlled diabetics. Similar to our results, there were more insulin-controlled diabetics in their study who did not develop delirium and more noninsulin-controlled diabetics in the group with delirium.Citation36
In must be noted that the HbA1c level assessment as a monitor for antecedent glycemia has been under discussion for some time. Several studies looked at HbA1c as a risk factor for postoperative complications in cardiac surgery because the number of diabetic patients presenting with coronary artery disease continues to rise. Nicolini et al performed a study aimed to assess whether elevated HbA1c level is associated with adverse outcome in patients undergoing CABG.Citation37 In this study, HbA1c identified patients at risk of sternal wound infection, but no other postoperative outcomes.Citation37 A study by Narayan et al is associated with HbA1c level of 6.5% or higher with a significant increase in the incidence of sternal wound infection and respiratory complications in patients undergoing CABG.Citation38 van den Boom et al have shown that although the HbA1c level was positively associated with perioperative glucose, it was not associated with increased 30-day mortality in cardiac procedures. The authors concluded that perioperative glucose control is related to surgical outcomes, yet the HbA1c, that reports preoperative glycemia control, is a less useful predictor.Citation39 Importantly, none of the above studies looked at postcardiac surgery delirium as a postoperative outcome after cardiac surgery.
It must also be underlined that in our study the internal carotid artery stenosis, but not stroke or transitory ischemic attack, was associated with POD after cardiac surgery. This is contrary to the findings of Cereghetti et al.Citation40 On the contrary, our study showed that in diabetic delirious patients, there were more episodes of stroke or TIA postoperatively.
Our study is not without limitations. We would like to underline that our study was a single-center retrospective analysis; therefore, it was merely associative and not predictor of causality research, and therefore, further prospective, multicenter activities are necessary to deepen our knowledge of diabetes and ICU delirium. Although the number of patients included was relatively high, as mentioned above the nature of the analysis was retrospective; therefore, some data may not be retrievable. We did not have the information regarding the type of delirium for all patients in our database nor regarding its severity. For a better understanding of the matter under discussion in diabetic and nondiabetic patients, a prospective study should be performed with a thorough examination of cognitive function and delirium severity assessment, as well as HbA1c and perioperative glycemia. Moreover, we used only HbA1c as a measure for the assessment of diabetes control, yet other and newer tests are available, including fructosamine, 1,5-anhydroglucitol, glycated albumin, or fetuin-A.
Conclusion
Occurrence of POD after cardiac surgery is associated with the diagnosis of diabetes and an elevated preoperative level of HbA1c. More diabetic patients develop POD after cardiac surgery than nondiabetic patients. Elevated preoperative level of HbA1c was an independent risk factor for postcardiac surgery delirium regardless of the diagnosis of diabetes.
Author contributions
All authors contributed toward data analysis, drafting and critically revising the paper, gave final approval of the version to be published and agree to be accountable for all aspects of the work.
Acknowledgments
The authors thank the patients who provided the data and staff of Department of Cardiac Surgery and Department of Anesthesiology, Intensive Therapy and Acute Intoxications of the Pomeranian Medical University in Szczecin for their kind help during this study.
Disclosure
The authors report no conflicts of interest in this work.
References
- McPhersonJAWagnerCEBoehmLMDelirium in the cardiovascular ICU: exploring modifiable risk factorsCrit Care Med201341240541323263581
- HollingerASiegemundMGoettelNSteinerLAPostoperative delirium in cardiac surgery: an unavoidable menace?J Cardiothorac Vasc Anesth20152961677168726456271
- American Psychiatric AssociationDiagnostic and Statistical Manual of Mental Disorders: DSM-55th edArlington, VAAmerican Psychiatric Association2013
- ElyEWShintaniATrumanBDelirium as a predictor of mortality in mechanically ventilated patients in the intensive care unitJAMA2004291141753176215082703
- KotfisKMarraAElyEWICU delirium – a diagnostic and therapeutic challenge in the intensive care unitAnaesthesiol Intensive Ther201850216016729882581
- MilbrandtEBDeppenSHarrisonPLCosts associated with delirium in mechanically ventilated patientsCrit Care Med200432495596215071384
- WoltersAEvan DijkDPasmaWLong-term outcome of delirium during intensive care unit stay in survivors of critical illness: a prospective cohort studyCrit Care2014183R12524942154
- OgawaMIzawaKPSatomi-KobayashiSImpact of delirium on postoperative frailty and long term cardiovascular events after cardiac surgeryPLoS One20171212e019035929287124
- ZaalIJSlooterAJDelirium in critically ill patients: epidemiology, pathophysiology, diagnosis and managementDrugs201272111457147122804788
- BurkhartCSDell-KusterSGamberiniMModifiable and non-modifiable risk factors for postoperative delirium after cardiac surgery with cardiopulmonary bypassJ Cardiothorac Vasc Anesth201024455555920227891
- OgawaMIzawaKPSatomi-KobayashiSPreoperative exercise capacity is associated with the prevalence of postoperative delirium in elective cardiac surgeryAging Clin Exp Res2018301273428243862
- LangoucheLVan den BergheGGlucose metabolism and insulin therapyCrit Care Clin20062211912916399023
- BisschopPHde RooijSEZwindermanAHvan OostenHEvan MunsterBCCortisol, insulin, and glucose and the risk of delirium in older adults with hip fractureJ Am Geriatr Soc20115991692169621883119
- van den BergheGWoutersPWeekersFIntensive insulin therapy in critically ill patientsN Engl J Med2001345191359136711794168
- WerbMRZinmanBTeasdaleSJHormonal and metabolic responses during coronary artery bypass surgery: role of infused glucoseJ Clin Endocrinol Metab1989695101010182677036
- LessenRDiCapuaJPekmezarisROur experience with two cardioplegic solutions: dextrose versus non-dextrose in adult cardiac surgeryJ Extra Corpor Technol201244313413823198393
- CarvalhoGMooreAQizilbashBLachapelleKSchrickerTMaintenance of normoglycemia during cardiac surgeryAnesth Analg200499231932415271698
- American Diabetes Association6. Glycemic targets: standards of medical care in diabetes-2018Diabetes Care201841Suppl 1S55S6429222377
- DorcelyBKatzKJagannathanRNovel biomarkers for prediabetes, diabetes, and associated complicationsDiabetes Metab Syndr Obes20171034536128860833
- HalkosMEPuskasJDLattoufOMElevated preoperative hemoglobin A1c level is predictive of adverse events after coronary artery bypass surgeryJ Thorac Cardiovasc Surg2008136363164018805264
- BordierLDoucetJBoudetJBauduceauBUpdate on cognitive decline and dementia in elderly patients with diabetesDiabetes Metab201440533133724703603
- ShinoharaMSatoNBidirectional interactions between diabetes and Alzheimer’s diseaseNeurochem Int201710829630228551028
- SechterbergerMKBosmanRJOudemans-van StraatenHMThe effect of diabetes mellitus on the association between measures of glycaemic control and ICU mortality: a retrospective cohort studyCrit Care2013172R5223510051
- van KeulenKKnolWBelitserSVDiabetes and glucose dysregulation and transition to delirium in ICU patientsCrit Care Med20184691444144929957712
- NashefSARoquesFSharplesLDEuroSCORE IIEur J Cardiothorac Surg201241473474522378855
- BuceriusJGummertJFWaltherTImpact of diabetes mellitus on cardiac surgery outcomeThorac Cardiovasc Surg2003511111612587082
- HeymannASanderMKrahneDHyperactive delirium and blood glucose control in critically ill patientsJ Int Med Res200735566667717900406
- GandhiGYNuttallGAAbelMDIntraoperative hyperglycemia and perioperative outcomes in cardiac surgery patientsMayo Clin Proc200580786286616007890
- GanaiSLeeKFMerrillAAdverse outcomes of geriatric patients undergoing abdominal surgery who are at high risk for deliriumArch Surg2007142111072107818025336
- AdamisDTreloarAMartinFCGregsonNHamiltonGMacdonaldAJAPOE and cytokines as biological markers for recovery of prevalent delirium in elderly medical inpatientsInt J Geriatr Psychiatry200722768869417203511
- HyunERamachandranRHollenbergMDVergnolleNMechanisms behind the anti-inflammatory actions of insulinCrit Rev Immunol201131430734021899513
- DandonaPChaudhuriAMohantyPGhanimHAnti-inflammatory effects of insulinCurr Opin Clin Nutr Metab Care200710451151717563472
- Van den BergheGWilmerAHermansGIntensive insulin therapy in the medical ICUN Engl J Med2006354544946116452557
- NasrawaySAHyperglycemia during critical illnessJPEN J Parenter Enteral Nutr200630325425816639074
- IngelsCDebaveyeYMilantsIStrict blood glucose control with insulin during intensive care after cardiac surgery: impact on 4-years survival, dependency on medical care, and quality-of-lifeEur Heart J200627222716272416608860
- SaagerLDuncanAEYaredJPIntraoperative tight glucose control using hyperinsulinemic normoglycemia increases delirium after cardiac surgeryAnesthesiology201512261214122325992877
- NicoliniFSantarpinoGGattiGUtility of glycated hemoglobin screening in patients undergoing elective coronary artery surgery: prospective, cohort study from the E-CABG registryInt J Surg20185335435929665452
- NarayanPKshirsagarSNMandalCKPreoperative glycosylated hemoglobin: a risk factor for patients undergoing coronary artery bypassAnn Thorac Surg2017104260661228274522
- van den BoomWSchroederRAManningMWSetjiTLFiestanG-ODunsonDBEffect of A1c and glucose on postoperative mortality in noncardiac and cardiac surgeriesDiabetes Care201841478278829440113
- CereghettiCSiegemundMSchaedelinSIndependent predictors of the duration and overall burden of postoperative delirium after cardiac surgery in adults: an observational cohort studyJ Cardiothorac Vasc Anesth20173161966197328711314