Abstract
Background:
A burn injury can be a traumatic experience with tremendous social, physical, and psychological consequences. The aim of this study was to investigate the existence of post-traumatic stress disorder (PTSD) and predictors of PTSD Checklist score initially and 3 months after injury in burns victims admitted to the Sina Burn Center in north-west Iran.
Methods:
This prospective study examined adult patients aged 16–65 years with unintentional burns. The PTSD Checklist was used to screen for PTSD.
Results:
Flame burns constituted 49.4% of all burns. Mean PTSD score was 23.8 ± 14.7 early in the hospitalization period and increased to 24.2 ± 14.3, 3 months after the burn injury. Twenty percent of victims 2 weeks into treatment had a positive PTSD screening test, and this figure increased to 31.5% after 3 months. The likelihood of developing a positive PTSD screening test increased significantly after 3 months (P < 0.01). Using multivariate regression analysis, factors independently predicting PTSD score were found to be age, gender, and percentage of total body surface area burned.
Conclusion:
PTSD was a problem in the population studied and should be managed appropriately after hospital admission due to burn injury. Male gender, younger age, and higher total body surface area burned may predict a higher PTSD score after burn injury.
Introduction
Burns are among the leading causes of death and disability in most countries. About 265,000 fire-related deaths are reported each year, based on an earlier study report of global disease burden. According to the World Health Organization, 238,000 individuals died of fire-related burns in 2000, and 95% of these deaths occurred in low- and middle-income countries.Citation1,Citation2
A burn injury can be a traumatic experience, with tremendous social, physical, and psychological consequences.Citation3 Reading through the burn care literature, it appears that burn care and research has focused on medical issues rather than on psychological predictors, the psychological aftermath, and quality of life in burns patients. Moreover, the physical isolation needed during treatment for burns and the psychological burden of bodily disfigurement are other areas of importance in burn psychology that may not have attracted enough attention, especially in low- and middle-income countries.Citation3–Citation6
Patients suffering from burn injury may also lose their main job and need to pay for medical surgical, psychological, and rehabilitation care.Citation7 Many may also suffer from delirium, depression, anxiety, post-traumatic stress disorder (PTSD), and suffer from the loss of their normal appearance.Citation3
Primary hospitalization of burn victims may be a very short period of their long-term treatment, and most patients need several restorative surgeries and several years of medical referrals, as well as ongoing financial and psychological support. Any ignorance can lead to their incomplete recovery and can produce permanent disability or even death. Researchers have realized that the pain suffered by a burns victim not only originates from his/her joints and tissues, but may also have a psychological basis, and needs to be addressed to gain the patient’s cooperation in treatment.
Stress disorders, including PTSD, are reported to occur after burn injuries in 18%–33% of cases, with PTSD being more common. PTSD usually occurs 3–6 months after the burn injury or even a year or more later.Citation8–Citation10 Psychological problems in burn victims affect quality of life and also cooperation in rehabilitation activities. It is reported that anxiety is the common aftermath of physical and emotional trauma. Apart from anxiety and depression, PTSD is another important issue that some burn victims will encounter.Citation11 PTSD may appear after observing, experiencing, or even hearing about a severe stressful traumatic event. Severity of the stress disorder experienced after the triggering event may be unbearable for some people. It usually appears during war, torture, natural disasters, invasion, rape, fatal car accidents, or fire. No doubt, developing PTSD after injuries that need long-term medical care will exacerbate the problem and may affect the prognosis. Although one of the important psychological disorders that may appear after burn injuries is PTSD, very few studies in developing countries have addressed this.
Burns are also a major health problem in many areas in Iran, including the northwest region.Citation5,Citation12–Citation14 Except for studies of self-immolation, there is no adequate research published in the literature on the psychological aspects of burns in Iran, and investigation of its psychological risk factors and sequelae have been neglected. Even the studies of self-immolation are limited to epidemiology and geographical distribution, rather than its psychological aspects.Citation5 The aim of this study was to investigate the incidence and predictors of PTSD after burn injury in victims admitted to the Sina Burn Center in north-west Iran.
Methods
This prospective study examined adult patients with unintentional burn injuries who were admitted to Sina Burn Center in Tabriz, which is the burns referral center for the north-western provinces of Iran, during 2009–2010. Inclusion criteria were informed consent to participate in the study, age 16–65 years, residence in Tabriz for at least 3.5 months after the incident, and the injury being unintentional. Exclusion criteria were known psychotic or personality disorders and death in hospital or during follow-up. The study was approved by the ethics committee at Tabriz University of Medical Sciences. Informed consent was obtained from the participants and/or their legal guardians.
A total of 85 burns patients were sampled randomly and enrolled sequentially. They were interviewed on one occasion 2 weeks after their injury, and 53 of the patients were assessed 3 months later. In the literature, studies similar to ours usually screened patients for PTSD during hospitalization (often in the first 2 weeks) and 3 months afterwards. Although in some studies the checklist was completed during the early days of hospitalization, given that we were interested in PTSD and not just acute stress disorder, follow-up was scheduled for 3 months afterwards. Although our study was based on the PTSD Checklist (PCL), according to the Diagnostic and Statistical Manual-IV, Text Revision (DSM-IV-TR), signs should exist for more than 4 weeks to diagnose PTSD.Citation3,Citation15 The PCL is a 17-item inventory that assesses for specific symptoms of PTSD. The respondent is asked to rate how much the problem described in each statement has bothered him or her over a given time period on a five-point scale ranging from 1 (not at all) to 5 (extremely). The items of PTSD are prepared according to the DSM-IV-TR criteria for PTSD in the US by Weathers et al.Citation16 Of the 17 items, five describe signs and symptoms of re-experiencing PTSD, for example, the first item is recurring, disturbing memories, thoughts, or images of a stressful experience from the past; item seven covers signs and symptoms of mental numbness and avoidance; item five includes signs and symptoms of severe mental arousal. This test has been found to be valid and reliable in previous studies.Citation16–Citation18
Statistical analysis
Data were analyzed using the STATA 11 statistical software package (STATA Corporation, College Station, TX). Descriptive statistics regarding variables with continuous scales were reported as means and standard deviations or medians and interquartile ranges based on their distribution. A total PCL score above 44 was considered as a positive PTSD screening test. The cutoff was based on PCL assessments for civilians rather than military participants. Total body surface area burned (TBSA) was used as the main burn severity surrogate in assessing the association between PTSD and burn severity. Appropriate bivariate and multivariate analyses were done. A P value < 0.05 was considered as the cutoff for statistical significance. All tests were taken as two-tailed. Model assumptions for multivariate analysis were checked and model fit was assessed to improve appropriateness of multivariate analysis.
Results
Fifty-two percent of the burn victims were female. The mean age of the participants was 32.6 ± 11.1 years. The youngest victim was aged 16 years and the oldest was aged 65 years. In total, 56.5% of burns occurred at home. Forty-eight percent of the injuries happened in the kitchen. Median TBSA was 11% with an interquartile range of 8%. The median TBSA was 12% for those with a positive PTSD screening test versus 10% among those with a lower PTSD score. Flame burns constituted 49.4% of all burns. Scalds were the second most common cause of burns, accounting for 30% of cases.
Mean PTSD score was 23.8 ± 14.7 in the early hospitalization period and increased to 24.2 ± 14.3, 3 months after the burn injury. Twenty percent of victims had a positive PTSD test after 2 weeks of treatment in hospital, and this proportion increased to 31.5% after 3 months. The likelihood of developing PTSD increased significantly after 3 months (McNemar’s Chi-squared test = 7.4, P < 0.01). PTSD was more common among flame burn victims, but this finding was not statistically significant.
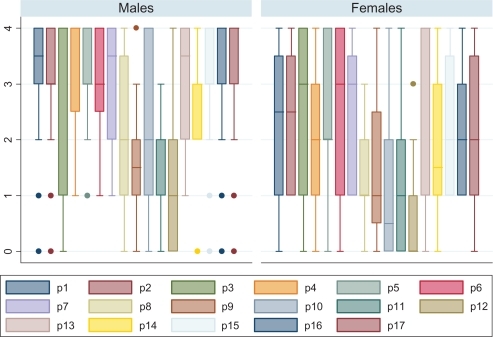
Using multivariate regression analysis, factors independently predicting PTSD score were age, gender, and percentage TBSA. Male gender, younger age, and higher TBSA was associated with a higher PTSD score. Box plots of PCL item scores in patients with a positive PTSD screening test were compared between males and females, and the results are shown in . Each box illustrates the first, second, and third quartiles of every item on the PCL, and shows which items are more affected.
Discussion
Of all injuries, burns are one of the most serious and often coexist with other illnesses and psychological disorders, leading to a range of signs and symptoms, including sleep problems, depression, acute stress disorder, and PTSD.Citation19,Citation20 It should be borne in mind that psychiatric symptoms do not always manifest themselves early in burns victims, and may appear up to several months after the injury.Citation21
In our study, 20% of burns victims had a positive PTSD test after 2 weeks in hospital, and this proportion increased to 31.5% after 3 months. According to the literature, 3%–58% of burns survivors develop PTSD symptoms and about 50% of them report suffering from at least one of the items on the PCL.Citation22–Citation25
Severe burn injuries are more likely to trigger PTSD,Citation20,Citation25,Citation26 which can impede the long-term rehabilitation of victims. Van Loey and Van Son reported that more than 90% of burns victims experience some symptoms of stress within the first week of the injury and more than 45% develop signs of chronic stress that can be categorized as PTSD after 1 year.Citation22
Millen et al considers personality to be the psychological equivalent of the immune system. Each of us lives in an environment of pathogens determining the characteristics of our immune systems.Citation27 A strong immune system can defeat infections while a weaker one predisposes to disease. Psychopathology follows a similar pattern, but there is no immune defense mechanism, and only our personality determines if we react, withstand, or succumb to our psychosocial environment and its stresses. From this point of view, personality characteristics play an important role in the capacity of a person to withstand stress. Therefore, each personality type can be considered as a coping style, and personality is a central regulator which expresses psychopathology. Victims suffering from PTSD at a young age may not benefit from powerful confronting strategies and need more time to be able to develop effective coping strategies and implement them.
In this study, younger age appeared to be associated with PTSD. It is difficult to explain this association fully. Several factors may be responsible, but at least one explanation that should be considered is that body image is more important at a young age and may be more affected by burn injuries. The findings of this study also show an association between PTSD and male gender. This may be explained by the higher prevalence of some types of burns in men, according to the literature.Citation28–Citation32 With regard to specific types of burns, eg, electrical and occupational burns, the male predominance is even higher, reaching up to 98% in some studies.Citation29,Citation33 Our study was not powered to assess if the observed gender association is in fact due to external factors, like type and mechanism of burn, or if it may be due to underlying biological or psychological differences between the genders. Future studies in this area should address these issues. It should be noted that the gender distribution of burn injuries can differ according to age group.
According to the recent research, there is a significant relationship between anxiety disorders and TBSA.Citation19 One finding in the present study was an association between burn severity and PTSD. Although this is in line with previous research,Citation19,Citation23 it needs to be clarified that the burn type (flame burn versus scald) or injury mechanism is also related to burn severity and may lead to a confounding effect.Citation34 Due to the limited statistical power of this study, we were unable to separate out the effects of burn severity and burn type, and this should be investigated in larger studies. Nevertheless, even if such a confounding effect exists, it seems to be partial, because injury severity is considered a plausible predictor for PTSD. Hospitalized patients should benefit from a psychological consultation as soon as possible, and these consultations should be continued even after discharge from hospital to decrease the risk of emotional disturbance.Citation35
The main limitation of this study was that it was not possible to use the DSM-IV-TR along with the PCL to make a definite diagnosis of PTSD and compare it with the results of PCL alone. Nevertheless, even the results of PCL could be beneficial in future research. PTSD was a problem after burn injuries in our study population and should be managed appropriately after admission for a burn injury. Male gender, younger age, and higher TBSA may predict a higher PTSD score after a burn injury.
Disclosure
The authors report no conflicts of interest in this work.
References
- World Health OrganizationInjury: A Leading Cause of the Global Burden of Disease, 2000Geneva, SwitzerlandWorld Health Organization2002
- MurrayCJLLopezADThe global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020Geneva, SwitzerlandWorld Health Organization1996
- TedstoneJETarrierNAn investigation of the prevalence of psychological morbidity in burn-injured patientsBurns1997237–85505549568322
- Aili-lowJIt’s not just a burn: physical and psychological problems after burns [thesis]Uppsala, SwedenUppsala University2007
- Sadeghi-BazarganiHMohammadiREpidemiology of burns in Iran during the last decade (2000–2010): review of literature and methodological considerations Unpublished work;2011
- Sadeghi-BazarganiHEpidemiology and statistical modeling in burn injuriesStockholm, SwedenKarolinska Institute Publications2011
- FauerbachJAEngravLKowalskeKBarriers to employment among working-aged patients with major burn injuryJ Burn Care Rehabil2001221263411227681
- DifedeJPtacekJTRobertsJAcute stress disorder after burn injury: a predictor of posttraumatic stress disorder?Psychosom Med200264582683412271114
- EhdeDMPattersonDRWiechmanSAWilsonLGPost-traumatic stress symptoms and distress following acute burn injuryBurns199925758759210563683
- EhdeDMPattersonDRWiechmanSAWilsonLGPost-traumatic stress symptoms and distress 1 year after burn injuryJ Burn Care Rehabil200021210511110752742
- FauerbachJALawrenceJWSchmidtCWJrMunsterAMCostaPTJrPersonality predictors of injury-related posttraumatic stress disorderJ Nerv Ment Dis2000188851051710972570
- MaghsoudiHPourzandAAzarmirGEtiology and outcome of burns in Tabriz, Iran. An analysis of 2963 casesScand J Surg2005941778115865123
- ArshiSSadeghi-BazarganiHMohammadiRPrevention oriented epidemiologic study of accidental burns in rural areas of Ardabil, IranBurns200632336637116529866
- ArshiSSadeghi-BazarganiHMohammadiRMohammad ZadehMSRouhiABarakMBurns comprising 3/4th of home injuries in pre-school children of rural areas of Ardabil province, IranJ Med Sci200772248251
- WillebrandMAnderssonGEkseliusLPrediction of psychological health after an accidental burnJ Trauma200457236737415345987
- WeathersFWLitzBTHermanDSHuskaJKeaneTThe PTSD Checklist (PCL). Reliability validity and diagnostic utilityAbstract presented at the ninth annual meeting of the International Society for Traumatic Stress StudiesSan Antonio, TX1993
- BlanchardEBJones-AlexanderJBuckleyTCFornerisCAPsychometric properties of the PTSD Checklist (PCL)Behav Res Ther19963486696738870294
- GoudarziMValidity and reliability of PTSD checklist [In Farsi]J Psychol2003722630
- PalmuRSuominenKVuolaJIsometsaEMental disorders among acute burn patientsBurns20103671072107920483541
- Ter SmittenMHde GraafRVan LoeyNEPrevalence and co-morbidity of psychiatric disorders 1–4 years after burnBurns2182011 [Epub ahead of print].
- YuBHDimsdaleJEPosttraumatic stress disorder in patients with burn injuriesJ Burn Care Rehabil199920542643310501332
- Van LoeyNEVan SonMJPsychopathology and psychological problems in patients with burn scars: epidemiology and managementAm J Clin Dermatol20034424527212680803
- SaxeGStoddardFChawlaNRisk factors for acute stress disorder in children with burnsJ Trauma Dissociation200562374916150668
- FalderSBrowneAEdgarDCore outcomes for adult burn survivors: a clinical overviewBurns200935561864119111399
- FauerbachJALawrenceJHaythornthwaiteJPreburn psychiatric history affects posttrauma morbidityPsychosomatics19973843743859217408
- TaalLAFaberAWPost-traumatic stress, pain and anxiety in adult burn victimsBurns1997237–85455499568321
- MillonTGrossmanSMillonCMeagherSRamnathRPersonality Disorders in Modern LifeHoboken, NJJohn Wiley & Sons Inc2004
- McKibbenJBEkseliusLGirasekDCEpidemiology of burn injuries II: psychiatric and behavioural perspectivesInt Rev Psychiatry200921651252119919204
- OthmanNKendrickDEpidemiology of burn injuries in the East Mediterranean Region: a systematic reviewBMC Public Health2010108320170527
- Sadeghi-BazarganiHMohammadiRSvanstromLEpidemiology of minor and moderate burns in rural Ardabil, IranBurns201036693393720171014
- SadeghiBHArshiSEkmanRMohammadiRPrevention-oriented epidemiology of burns in Ardabil provincial burn centre, IranBurns201137352152721131133
- ForjuohSNGuyerBStrobinoDMKeylPMDiener-WestMSmithGSRisk factors for childhood burns: a case-control study of Ghanaian childrenJ Epidemiol Community Health19954921891937798049
- MaghsoudiHAdyaniYAhmadianNElectrical and lightning injuriesJ Burn Care Res200728225526117351442
- ForjuohSNBurns in low- and middle-income countries: a review of available literature on descriptive epidemiology, risk factors, treatment, and preventionBurns200632552953716777340
- HerndonDTotal Burn CareLondon, UKWB Saunders2008