Abstract
An approach viewing anxiety and depression as extensions of normal adaptive biologic drives is discussed. Anxiety is viewed as the result of an underlying biological drive to preserve and maintain our wellbeing. At the extremes, if unresolved, this drive can be maladaptive, particularly if activated over prolonged periods of time. This paper proposes that depression is the result of a biological drive that mediates the effects of maladaptive levels of anxiety. These two processes are thought to be acting simultaneously. When operating in the normal range, these drives are helpful; in the extremes, they are associated with impairment. Over time, if unresolved, symptoms of anxiety will begin to become associated with increasing levels of depression.
Keywords:
Plain Language Summary
This article offers another way of thinking about anxiety and depression. Both are viewed as extensions of normal biological drives that work in parallel to keep us safe, healthy, and functioning well. But when pushed to the extremes these same adaptive drives are responsible for anxiety and depression. We are constantly faced with stressors great and small, ranging from requirements to meet basic physical, social, and emotional needs such as aquiring food or finding a partner, to making less imperative decisions such as selecting a pair of socks to wear in the morning. Normally we are able to effectively and effeciently manage the stressors that are encountered. However, if these stressors, when combined, are too great and beyond the individual's ability to manage, impairment in functionng begins to occur. Initially, the stressors cause anxiety, but if they remain unresolved, over time symptoms of depression may begin to appear in increasing number and intensity.
Adaptive Affect
Adaptive characteristics, meaning those that are helpful to us, are retained in the general population. As such, the continued presence of anxiety and depression suggests the processes reflect something beneficial. While the adaptive role anxiety plays in preserving and protecting us is not difficult to see (eg, avoiding potential harm), at the extremes of severity and duration, anxiety can become problematic (eg, clinically significant impairment). The adaptive role of depression is less clear. On the surface, it does not seem plausible that depression would be adaptive, as a hallmark feature is impairment in functioning. Yet, depression is present across cultures and has been preserved over time.Citation1–Citation3 This manuscript describes a slightly different perspective on the origin and relationship between anxious and depressive mood states.
Affective symptoms caused by stressors both internal and external have been the subject of a tremendous amount of study over the last century, and documented for several millennia.Citation3 During this time, any number of models explaining the development of affective symptoms have been presented;Citation3–Citation14 as these models have increased in accuracy and relevance, they have also become more complex. The goal of this manuscript is to provide a simple model explaining the natural development of affective symptoms over time. The approach described is straight forward. Individuals are constantly under stress to adapt to the environment (internal and external), required to maintain an adaptive balance between action and non-action. The thought being stress produces anxiety that is adaptive when the individual is able to respond and alter themselves or the environment, but in situations that a satisfactory response is not possible it is maladaptive to remain in a highly activated state for prolonged periods of time. In these situations it would be beneficial to reduce the call to action, to decrease the anxiety response. It is possible that some of the symptom presentations we associate with clinical depression are the result of the extension of an adaptive biological mechanism that mediates the effects of prolonged anxiety. If we associate anxiety with activation and depression with deactivation at the extremes, the idea can be displayed in a diagram (see ).
Figure 1 Phase diagram showing stress outcomes from the resolution of biological drives.
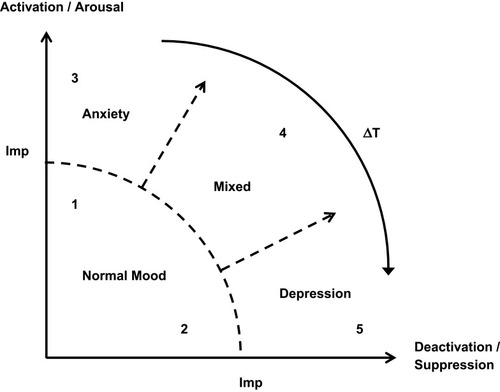
is a “temporal” phase diagram that allows for activation and deactivation to occur simultaneously over time. The axes “y” (Activation/Arousal) and “x” (Deactivation/Suppression) display the interaction between underlying biological drives that are responsible for symptom presentation at the extremes. Clinically significant impairment and/or distress define the boundary for normal mood states and those requiring treatment (expressed as dashed line “Imp” in ). The lines displaying boundaries between normal, anxiety, depression, and mixed are dashed, indicated they are imprecise and individualized. The lines between anxiety, depression, and mixed presentations were included to illustrate the progression of symptoms, with ∆T indicating the direction of change over time. Holding severity constant, the natural progression over time is indicated as (A→D)∆T (anxiety yields depression over time).
If these underlying biological drives are developed, the question of why would activation and deactivation occur simultaneously remains, as it would appear to be more efficient simply to reduce or stop the activation process rather than initiate a mediating process. There is an advantage associated with being able to reduce the effects of anxiety-producing stimuli while maintaining a level of arousal that does not impair functioning.Citation15 In the individual that is functioning normally, this may achieve this balance and create a space to process (conscious and nonconscious) as needed, increasing positive outcomes. In the person who is experiencing clinically significant distress and/or impairment, this space may appear symptomatic, replete with maladaptive levels of anxiety and depression.Citation16,Citation17
While, in general, if stressors remain constant, the relationship (A→D)∆T would be expressed.Citation9–Citation12 Key prognostic features, such as the rate at which the symptom presentation moves from being predominantly anxious to including symptoms of depressed mood, and the magnitude of stressors required for impairment to occur are unique to the individual (genetic vulnerability and resiliency factors,Citation18–Citation21 as well as characteristics that moderate disease burden and coarse of illness,Citation22–Citation26 have been identified). A person’s present state (position on the diagram) is the result of a summation of multiple inputs (internal and external) calling for action and non-action simultaneously. The specific symptom presentation would depend upon the individual’s location on the time line (anxiety-mixed-depression).
Disorders associated with primary physiologic hyperarousal (panic and phobic disorders) would be located close to the y-axis of , and those associated with neurovegetative symptoms would be close to the x-axis (atypical depression).Citation27,Citation28 Disorders showing symptoms of both anxiety and depression, such as melancholic depression,Citation27–Citation30 would be located in the middle portion of the diagram in the mixed section. This approach addresses normal mood and affective symptoms of anxiety and depression; mania and psychosis are thought to involve additional underlying systems and are not included in this model. Normal mood such as being excited or relaxed would be below the impairment line, close to the y- and x-axis, respectively. In most patients, exposure to sustained levels of unresolvable anxiety-producing stressors leads to depression.Citation9–Citation12 However, patients with disorders hallmarked by brief episodic hyperarousal experience clinical anxiety as discrete events, and may lack the sustained exposure to stressors required to develop clinical depression.
An adaptive affect approach offers a slightly different perspective on what we currently understand about anxiety and depression. By looking at the summation of concurrent activating and deactivating drives, the model explains much of the broad spectrum of symptom presentations associated with affective disorders, and based upon trajectory, provides a framework for understanding the progression of an individual’s affective states over time. The approach is simple, and the information required is generally gathered as part of a standard clinical interview within or outside of a research protocol. Whether in clinical practice or research, this perspective provides a simple way to interpret a person’s history and current functioning, as well as a “common sense” model that is easy to understand.
Disclosure
The author reports no conflicts of interest in this work.
References
- Whiteford HA, Degenhardt L, Rehm J, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382(9904):1575–1586. doi:10.1016/S0140-6736(13)61611-623993280
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age of-onset distributions of DSM-IV disorders in the National Comorbidity Survey replication. Arch Gen Psychiatry. 2005;62:593–602. doi:10.1001/archpsyc.62.6.59315939837
- Hippocrates. Omni opera Hippocratis. Venice: Aldus Manutius, 1526.
- Solomon RL, Corbit JD. An opponent-process theory of motivation: I. Temporal dynamics of affect. Psychol Rev. 1974;81(2):119–145. doi:10.1037/h00361284817611
- Clark LA, Watson D. Tripartite model of anxiety and depression: psychometric evidence and taxonomic implications. J Abnorm Psychol. 1991;100(3):316–336. doi:10.1037/0021-843X.100.3.3161918611
- Watson D, Tellegen A. Toward a consensual structure of mood. Psychol Bull. 1985;98(2):219–235. doi:10.1037/0033-2909.98.2.2193901060
- Leary T. Interpersonal Diagnosis of Personality. New York: Ronald Press; 1957:59–87.
- Posner J, Russell J, Peterson B. The circumplex model of affect: an integrative approach to affective neuroscience, cognitive development, and psychopathology. Dev Psychopathol. 2005;17:715–734. doi:10.1017/S095457940505034016262989
- Gold PW, Goodwin FK, Chrousos GP. Clinical and biochemical manifestations of depression. Relation to the neurobiology of stress. N Engl J Med. 1988;319(6):348–353. doi:10.1056/NEJM1988081131906063292920
- Chrousos GP, Gold PW. The concepts of stress and stress system disorders. Overview of physical and behavioral homeostasis. JAMA. 1992;267(9):1244–1252.1538563
- Gold PW. The organization of the stress system and its dysregulation in depressive illness. Mol Psychiatry. 2015;20(1):32–47. doi:10.1038/mp.2014.16325486982
- Gold PW, Chrousos GP. Organization of the stress system and its dysregulation in melancholic and atypical depression: high vs low CRH/NE states. Mol Psychiatry. 2002;7:254–275. doi:10.1038/sj.mp.400103211920153
- Krishnan V, Nestler EJ. The molecular neurobiology of depression. Nature. 2008;455:894–902. doi:10.1038/nature0745518923511
- Martin EI, Ressler KJ, Binder E, Nemeroff CB. The neurobiology of anxiety disorders: brain imaging, genetics, and psychoneuroendocrinology. Psychiatr Clin North Am. 2009;32(3):549–575. doi:10.1016/j.psc.2009.05.00419716990
- Yerkes RM, Dodson JD. The relation of strength of stimulus to rapidity of habit-formation. J Comp Neurol Psychol. 1908;18(5):459–482. doi:10.1002/(ISSN)1550-7149
- Cannon WB. The Wisdom of the Body. New York: W. W. Norton; 1932:177–201.
- Anselme P. The uncertainty processing theory of motivation. Behav Brain Res. 2010;208(2):291–310. doi:10.1016/j.bbr.2009.12.02020035799
- Feder A, Nestler EJ, Charney DS. Psychobiology and molecular genetics of resilience. Nat Rev Neurosci. 2009;10:446–457. doi:10.1038/nrn264919455174
- Krishnan V, Han MH, Graham DL, et al. Molecular adaptations underlying susceptibility and resistance to social defeat in brain reward regions. Cell. 2007;131:391–404. doi:10.1016/j.cell.2007.09.01817956738
- Caspi A, Sugden K, Moffitt TE, et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003;301:386–389. doi:10.1126/science.108396812869766
- Kendler KS, Kuhn JW, Vittum J, Prescott CA, Riley B. The interaction of stressful life events and a serotonin transporter polymorphism in the prediction of episodes of major depression: a replication. Arch Gen Psychiatry. 2005;62:529–535. doi:10.1001/archpsyc.62.5.52915867106
- Morris DW, Budhwar N, Husain M, et al. Depression treatment in patients with general medical conditions: results from the CO-MED trial. Ann Fam Med. 2012;10(1):23–33. doi:10.1370/afm.131622230827
- Trivedi MH, Morris DW, Pan J, Grannemann BD, Rush AJ. What moderator characteristics are associated with better prognosis for depression? Neuropsychiatr Dis Treat. 2005;1(1):51–57. doi:10.2147/nedt.1.1.51.5229818568124
- Trivedi MH, Morris DW, Wisniewski SR, et al. Increase in work productivity of depressed individuals with improvement in depressive symptom outcomes. Am J Psychiatry. 2013;170(6):633–641. doi:10.1176/appi.ajp.2012.1202025023558394
- Rush AJ, Trivedi MH, Stewart JW, et al. Combining medications to enhance depression outcomes (CO-MED): acute and long-term outcomes of a single-blind randomized study. Am J Psychiatry. 2011;168(7):689–701. doi:10.1176/appi.ajp.2011.1011164521536692
- Trivedi MH, Kocsis JH, Thase ME, et al. REVAMP – research evaluating the value of augmenting medication with psychotherapy: rationale and design. Psychopharmacol Bull. 2008;41(4):5–33.
- Fava M, Kendler KS. Major depressive disorder. Neuron. 2000;28(2):335–341. doi:10.1016/S0896-6273(00)00112-411144343
- Rush AJ. The varied clinical presentations of major depressive disorder. J Clin Psychiatry. 2007;68(Suppl 8):4–10.
- Morris DW, Rush AJ, Jain S, et al. Diurnal mood variation in outpatients with major depressive disorder: implications for DSM-V from an analysis of the sequenced treatment alternatives to relieve depression study data. J Clin Psychiatry. 2007;68:1339–1347. doi:10.4088/JCP.v68n090317915971
- Morris DW, Trivedi MH, Fava M, et al. Diurnal mood variation in outpatients with major depressive disorder. Depress Anxiety. 2009;26:851–863. doi:10.1002/da.v26:919306304
