Abstract
Purpose
The present retrospective study aimed to determine the medication profile and estimate the treatment costs from medical records of new outpatients with schizophrenia, bipolar disorder, depression, and anxiety disorders from a healthcare perspective at a national referral hospital in Indonesia from 2016 to 2018.
Methods
Medical records (including medical and administrative data) of 357 new outpatients with schizophrenia, bipolar disorder, depression, or anxiety disorders were collected from the hospital information system. The records of new outpatients with schizophrenia, bipolar disorder, depression, or anxiety disorders aged >18 years and had only received drugs for treatment were included. The medication profile was descriptively assessed, and estimated costs were calculated based on direct costs from a healthcare perspective.
Results
Overall, 173 medical records were further analyzed. The main drugs administered to the new outpatients were atypical and typical antipsychotics for schizophrenia, atypical antipsychotics and mood stabilizers for bipolar disorder, antidepressants and atypical antipsychotics for depression, and antidepressants and benzodiazepines for anxiety disorders. The average annual treatment costs per patient were IDR 3,307,931 (USD 236) for schizophrenia, IDR 17,978,865 (USD 1,284) for bipolar disorder, IDR 1,601,850 (USD 114) for depression, and IDR 1,190,563 (USD 85) for anxiety disorders.
Conclusion
The most commonly prescribed drugs for schizophrenia were haloperidol and risperidone; for bipolar disorders, sodium divalproex and risperidone; for depression, fluoxetine and sertraline; and for anxiety disorders, sertraline and lorazepam. Considering the high prevalence and estimated treatment costs for mental disorders, special attention is required to prevent an increase in their prevalence in Indonesia.
Introduction
According to the World Health Organization, one in four individuals globally will be affected by mental or neurological disorders at some point in their lives.Citation1 In 2018, the psychiatric disorders with the highest prevalence worldwide were depression (300 million individuals), bipolar disorder (60 million individuals), and schizophrenia and other psychoses (23 million individuals).Citation2 As of August 2018, Indonesia’s population aged >15 years included approximately 194 million individuals,Citation3 and in 2017 there were 67 million households.Citation4 The prevalence of schizophrenia in individuals aged >15 years according to basic health research (RISKESDAS) from the Ministry of Health, Indonesia, in 2018 was 7°/oo (7 of 1000 households have a member with schizophrenia, corresponding to approximately 470,000 individuals), and the prevalence of mental–emotional disorders including bipolar disorder, depression, and anxiety disorders was 9.8% (approximately 19 million).Citation5 Among this 9.8% of mental–emotional disorders, the prevalence of depression was 6.1% (approximately 11.8 million individuals).Citation5
Schizophrenia is a complex psychiatric disorder characterized by changes in inappropriate behavior, chaotic thought patterns, delusion, hallucination, and psychosocial dysfunction.Citation6 Antipsychotics are the main choice for schizophrenia therapy, and they are divided into typical and atypical antipsychotics.Citation6 According to the American Psychiatric Association, typical and atypical antipsychotics other than clozapine are recommended for the treatment of acute phase schizophrenia.Citation7 The choice of antipsychotics is influenced by several factors, such as side effects and cost.Citation7,Citation8 Cognitive behavioral therapy (CBT) was one of the first non-pharmacological interventions included in the treatment guidelines for schizophrenia.Citation9 CBT is an intervention that helps modify undesirable thought patterns, feelings, and behavior. Moreover, CBT is useful in reducing disorganized behavior, which affects daily life in individuals with schizophrenia.Citation9
Bipolar disorder is a mood disorder characterized by episodes of mania or hypomania that appear alternately or concurrent with depressive episodes.Citation10 Treatment for bipolar disorder typically focuses on acute stabilization, with the aim of improving the symptoms of mania or depression in a patient, thereby enabling a stable mood (euthymia) to be achieved.Citation11 The maintenance phase aims to prevent relapse, reduce subthreshold symptoms, improve social functioning, and reduce suicide risk and mood instability-related risk.Citation11,Citation12 The main therapies for episodes of mania in bipolar disorder are mood stabilizers, antipsychotic agents, or a combination of both agents, whereas the therapies for depressive episodes are mood stabilizers and certain antipsychotics.Citation13 Antidepressants can be used with mood stabilizers to reduce the risk of mood change to mania or can be used after a patient fails to respond to mood stabilizer therapy.Citation13 Non-pharmacological therapies, such as short-term psychotherapies, offer fairly consistent benefits to patients with bipolar disorder as an adjunctive therapy.Citation14 CBT, family-focused therapy, and psychoeducation offer the most robust efficacy in terms of relapse prevention.Citation14
Depression is a mental illness characterized by decreased mood, loss of interest, guilty feelings, decreased appetite, disturbed sleep, and low concentration.Citation15 Depressive disorders are typically treated with antidepressants, psychotherapy, or a combination of both.Citation16 There are four groups of antidepressants as follows: selective serotonin reuptake inhibitors (SSRIs), serotonin norepinephrine reuptake inhibitors (SNRIs), monoamine oxidase inhibitors (MAOIs), and tricyclic antidepressants (TCAs) and other heterocyclic agents.Citation17,Citation18 A systematic review published in 2017 revealed that in contrast to pharmacological treatment, most non-pharmacological interventions for treating patients with major depressive disorder are not evidence-based.Citation19 On the other hand, exercise therapy, bibliotherapy, CBT, short-term psychodynamic supportive psychotherapy, and interpersonal psychotherapy (IPT) are considered valid non-pharmacological treatments for adult patients with mild or moderate depression in Korea.Citation20
Anxiety disorders involve excessive fear and are irrational.Citation21 They are considered the most common psychiatric disorders, particularly in developed countries, and are characterized by physical symptoms, such as fatigue.Citation22 Therapy for anxiety disorder aims to prevent recurrence and improve the quality of life of patients.Citation23 The suggested first-line therapy includes a single SSRI or SNRI.Citation24 These drugs are effective for reducing anxiety symptoms according to randomized controlled trials.Citation25 TCAs are another drug choice; however, these drugs are rarely used owing to increased side effects and mortality risk associated with overdose.Citation26,Citation27 CBT has been proven to be effective as a non-pharmacological therapy for anxiety disorders.Citation28
The burden of disease (BOD), also known as the cost of illness (COI), encompasses various aspects of the disease impact on the health outcomes in a country, specific regions, communities, and even individuals.Citation29 COI studies traditionally stratify costs into three categories: direct, indirect, and intangible costs.Citation29 Direct costs most often refer to the “visible costs” associated with diagnosis and treatment in the healthcare system, such as those related to medication, physician visits, psychotherapy sessions, and hospitalization. Indirect costs refer to the “invisible costs” associated with income losses due to mortality, disability, and care seeking, including productivity losses due to work absence or early retirement.Citation30 COI studies can be performed from various perspectives, such as determining costs to society, the healthcare system, third-party payers, business sectors, the government, and the participants and their families.Citation29 From a healthcare perspective, only medical costs are included in such studies.Citation29
Mental health disorders are some of the main causes of the overall disease burden worldwide.Citation31 Approximately one-third of the BOD of mental health is associated with productivity losses, including those related to unemployment, disability, and low work performance.Citation32 According to the World Economic Forum in 2011, the economic burden of psychiatric disorders in 2010 was estimated at USD 2.5 trillion, and it is expected to increase to USD 6 trillion by 2030.Citation30,Citation33 In 2004–2005, the direct cost associated with schizophrenia in the UK reached GBP 2 billion and the indirect cost was GBP 4.7 billion, with a total cost of GBP 6.7 billion.Citation34 In a study conducted in the United States in 2009, it was estimated that the total cost of type I and II bipolar disorders was USD 151.1 billion, with a direct cost of approximately USD 30.7 billion and an indirect cost of approximately USD 120.3 billion.Citation35 In 2015, Cloutier et al estimated a total cost associated with bipolar disorder of USD 202.1 billion, with an average cost per patient of USD 81,559.Citation36 In 2017, the American Psychological Association reported that the cost of treating depression was approximately USD 71 billion in the United States.Citation37 Moreover, in Japan, the cost of treating anxiety disorders reached USD 20.5 billion in 2008.Citation38 We believe that these costs are high in Indonesia. The present study aimed to retrospectively determine the medication profile and estimate the treatment costs in from the medical records of new outpatients with schizophrenia, bipolar disorder, depression, and anxiety disorders from a healthcare perspective at one of the national referral hospitals in Indonesia from 2016 to 2018.
Methods
Study Design
This was an observational study with a cross-sectional design. Data were retrospectively collected from medical records, prescriptions, and administration records of outpatients at the mental clinic of one of the national referral hospitals in Indonesia from 2016 to 2018. New outpatients, in example, patients who were treated or registered in the hospital for the first time, with a diagnosis of schizophrenia (F20), bipolar disorder (F31), depression (F32 and F33), or anxiety disorders (F40–F43) according to the ICD-10 criteria, age more than 18 years, and had only received drugs for treatment were included. Patients with incomplete outpatient data, those who received only psychotherapy treatment, and those diagnosed with >1 mental disorders and had concomitant diseases that affect mental disorders, such as metabolic syndrome, endocrine disease, chronic disease, nervous system disorders, and cancer, were excluded.
Ethics
This study was approved by the ethics committee of Faculty of Medicine, Universitas Padjadjaran, Indonesia. Additionally, personal information was kept confidential by providing a numeric code for each medical record.
Medication Profile
The medication profile was analyzed according to patient characteristics and the types of drugs received by the patients during outpatient treatment. Each patient who received a drug type was recorded and then descriptively analyzed. One patient could receive more than one type of drug. Moreover, medication profiles were provided based on patient category (national insurance and uninsured).
Treatment Cost Estimation
Treatment cost estimation involved direct cost from a healthcare perspective. Direct costs consisted of drug cost, administrative cost, and doctor consultation fees. Each new outpatient data cost was recorded and calculated for 1 year. The sum of the annual direct cost for 1 year, was then divided by the total number of patients to obtain the average estimated annual cost for each patient. We estimated the annual direct costs deeming that the patients were adherent to the treatment. Cost data were obtained from the hospital information system.
Statistical Analysis
The medication profile was analyzed descriptively. The annual cost difference was analyzed by either the Kruskal–Wallis test or the Mann–Whitney test. The difference was considered significant at a p-value <0.05. All statistical analyses were performed using SPSS software version 22 for Windows (IBM Corp., Armonk, NY, USA).
Results
Data Collection
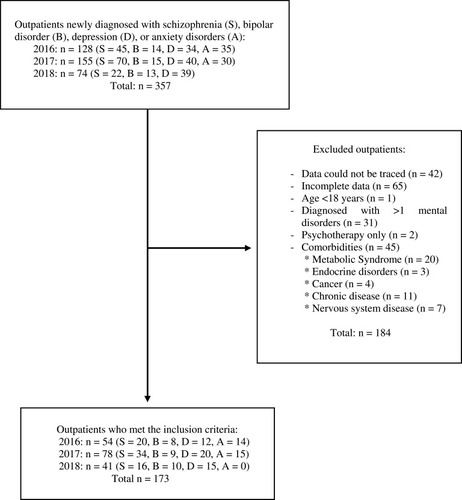
shows the process of data collection. Among 357 new outpatients from 2016 to 2018, we excluded 184. Thus, 173 outpatients met the inclusion and exclusion criteria and were eligible for further analysis.
Subject Characteristics
presents the characteristics of the new outpatients who visited the mental health department in 2016, 2017, and 2018, and who met the inclusion and exclusion criteria. Among the new outpatients, 59% (n=102) were male, 56.1% (n=97) were aged 26–45 years, and 56.6% (n=98) used insurance. The total number of visits was 422, and the average number of visits a year per patient was 2–3. Among the 173 outpatients selected, 40.5% (n=70) had schizophrenia, 15.6% (n=27) had bipolar disorder, 27.2% (n=47) had depression, and 16.7% (n=29) had anxiety disorders. Most patients with schizophrenia (48 of 70) and bipolar disorder (21 of 27) were insured, whereas most patients with depression (27 of 47) and anxiety disorders (20 of 29) were uninsured.
Table 1 Patient Characteristics
Schizophrenia Medication Profile
The medication profile of outpatients with schizophrenia is presented in . The first-line drugs administered to outpatients with schizophrenia who visited the mental health department were usually antipsychotic drugs (both typical and atypical types). Other drugs, such as anticholinergics, benzodiazepines, and antidepressants, were administered as adjunct drugs. The use of typical antipsychotics decreased from 35.8% of patients in 2016 to 14.3% in 2018, whereas the use of atypical antipsychotics increased from 22.6% in 2016 to 57.1% in 2018. Haloperidol was the most commonly used typical antipsychotic (16.0%), and risperidone was the most commonly used atypical antipsychotic (22.7%). The use of trihexyphenidyl decreased from 39.6% in 2016 to 7.1% in 2018, whereas the use of lorazepam increased from 1.9% in 2016 to 17.9% in 2018. Overall, 83.3% (40 of 48) of insured outpatients received atypical antipsychotic drugs.
Table 2 Medication Profile of Schizophrenia Patients
Bipolar Disorder Medication Profile
The medication profile of outpatients with bipolar disorder is presented in . Several classes of drugs were administered to the patients, including mood stabilizers, antipsychotics, antidepressants, benzodiazepines, and anticholinergics. Mood stabilizers were first-line drugs in patients with bipolar disorder, and they were used in 29.4% of patients. Sodium divalproex was the most commonly used mood stabilizer (27.9%). Atypical antipsychotics were used in 39.7% of patients. Risperidone was the most commonly used atypical antipsychotic (11.8%). All insured patients received at least one type of atypical antipsychotic drug, and 81% (17 of 21) received sodium divalproex for treatment.
Table 3 Medication Profile of Bipolar Disorders Patients
Depression Medication Profile
The medication profile of outpatients with depression is presented in . Antidepressants were commonly used for treatment (51.2%). Benzodiazepines, atypical antipsychotics, anticholinergics, and mood stabilizers were also used. The atypical antipsychotic risperidone was the most common drug (18%). The drugs used in both insured and uninsured patients did not show considerable difference.
Table 4 Medication Profile of Depression Patients
Anxiety Disorder Medication Profile
The medication profile of outpatients with anxiety disorders is presented in . Several classes of drugs were administered to the patients, including antidepressants, benzodiazepines, and antipsychotics. Antidepressants and benzodiazepines were dominantly used (both 47.6%). Sertraline was the most commonly used antidepressant (28.6%), and lorazepam was the most commonly used benzodiazepine (22.2%). Most of the insured patients received more than one benzodiazepine and antidepressant.
Table 5 Medication Profile of Anxiety Disorders Patients
Treatment Cost Estimation
presents the average estimated annual treatment costs from a healthcare perspective for outpatients with schizophrenia, bipolar disorder, depression, and anxiety disorders if the patients were adherent to regular medical treatment for 1 year. Among all the mental disorders, bipolar disorder had the highest average annual treatment cost of IDR 17,978,865 (USD 1,284) per patient. The average annual treatment costs for schizophrenia, depression, and anxiety disorders were IDR 3,307,931 (USD 236), IDR 1,601,850 (USD 114), and IDR 1,190,563 (USD 85) per patient, respectively. There was a significant difference (p =0.012) in the depression treatment cost owing to changes in the guideline in 2017. Based on patient category, the costs were not significantly different (p >0.05) between insured and uninsured patients with schizophrenia, depression, and anxiety disorders. However, the costs were significantly different (p =0.012) between insured and uninsured patients with bipolar disorder.
Table 6 Average Treatment Cost Estimation
Discussion
The present study provides an overview of the medication profile and estimated annual treatment costs of outpatients with schizophrenia, bipolar disorder, depression, and anxiety disorders, as well as the total estimated annual treatment cost for these disorders at one of the national referral hospitals in Indonesia from 2016 to 2018. The main drugs were atypical and typical antipsychotics for schizophrenia, atypical antipsychotics and mood stabilizers for bipolar disorder, antidepressants and atypical antipsychotics for depression, and antidepressants and benzodiazepines for anxiety disorders. The average annual treatment costs for schizophrenia, depression, and anxiety disorders were IDR 3,307,931 (USD 236), IDR 1,601,850 (USD 114), and IDR 1,190,563 (USD 85) per patient, respectively.
In patients with schizophrenia, our study found that haloperidol was the most commonly used typical antipsychotic and risperidone was the most commonly used atypical antipsychotic. These results are consistent with the findings in the 2017 study by Oktapaku in Nigeria, which reported that haloperidol was the most widely used antipsychotic among outpatients, and the 2018 study by Khan, which reported that the atypical antipsychotic risperidone was most widely used by patients with schizophrenia.Citation39,Citation40 The American Psychiatric Association states that the use of different types of antipsychotics depends on the clinical outcome desired. In addition, factors, such as patient response, hospital policy, drug availability, and cost influence the choice of antipsychotics.Citation7 In this study, the other drugs administered were anticholinergics (trihexyphenidyl), benzodiazepines (lorazepam), and antidepressants (fluoxetine). The anticholinergic trihexyphenidyl was mostly used in 2016 to reduce extrapyramidal side effects (dystonia, akathisia, pseudoparkinsonism, and tardive dyskinesia), and its use decreased with the decrease in typical antipsychotic use in 2017 and 2018. Benzodiazepines, such as lorazepam, when used together with antipsychotics can reduce the risk of extrapyramidal side effects.Citation7 The use of antidepressants in patients with schizophrenia is uncommon, and some studies suggest that the use of antidepressants in patients with schizophrenia is ineffective because not all patients recover from the depression symptoms experienced.Citation41
In this study, for the treatment of bipolar disorder, most patients received more than one type of drug other than mood stabilizers. They were also administered antipsychotics, antidepressants, benzodiazepines, and anticholinergics. This approach is common and has the purpose of preventing recurrence that cannot be avoided because the efficacy profiles of drugs differ and the needs for handling both episodes of bipolar disorder also differ.Citation42 Sodium divalproex is a type of mood stabilizer that was the most widely used drug among patients with bipolar disorder (27.9%) in this study. This finding is consistent with the finding in the 2012 study by Chawla et al, which reported that the most widely used drug among patients with bipolar disorder in India was sodium valproate (54.7%).Citation43 In addition, a 2009 study involving bipolar disorder outpatients in South Africa mentioned that most patients (83.8%) were prescribed at least one standard mood stabilizer and that sodium valproate was the most prescribed mood stabilizer (37.1%).Citation44 The National Institute for Health and Care Excellence (NICE) has recommended the use of valproate as first-line therapy in acute manic episodes. It can be combined with antidepressants for the treatment of acute depressive episodes and for prophylaxis.Citation45 In addition to mood stabilizers, antipsychotics, such as haloperidol, aripiprazole, and risperidone; benzodiazepines, such as lorazepam; and antidepressants, such as quetiapine, can be combined for treatment.Citation46 In this study, the most widely used atypical antipsychotic was risperidone. Antipsychotics are often used in the acute phase of bipolar disorder and are mostly used in patients who have psychotic symptoms.Citation47 Benzodiazepines, such as lorazepam, can also be used as an alternative therapy or as an adjunct therapy with antipsychotics in patients with acute manic episodes or those who cannot use mood stabilizers.Citation18
In this study, fluoxetine and sertraline were frequently administered in patients with depression (both 17%). A previous study at a hospital in Sragen, Indonesia, reported that 93.33% of patients were administered fluoxetine,Citation48 and another study at a hospital in Surakarta, Indonesia, reported that 64.4% of patients were administered this drug.Citation49 In addition to antidepressants, atypical antipsychotics and benzodiazepines were administered in patients with depression in the present study. Antipsychotics were frequently used for depression treatment because 80% of patients experienced psychotic symptoms in 2017. Antidepressants are widely used in combination with benzodiazepines to increase patient compliance and reduce the severity of depression.Citation50
The main drugs among patients with anxiety disorders in this study were antidepressants and benzodiazepines. Antidepressants with an SSRI mechanism were administered in 41.3% of patients with anxiety disorders, and the SSRI sertraline was administered in 28.6% of patients. An antidepressant with an SSRI mechanism is the first-line therapy recommended for most anxiety disorders, and it is typically started at a low dose to avoid side effects.Citation51 To provide additional efficacy for reducing symptoms, antidepressants are usually combined with benzodiazepines.Citation52 In the present study, the benzodiazepine lorazepam was administered in 28.6% of patients. However, benzodiazepines are not recommended for long-term treatment owing to side effects and potential addiction.Citation53 Benzodiazepines are usually administered for severe anxiety disorders and are administered at night to overcome insomnia.Citation54,Citation55
In our study, the estimated annual treatment cost for outpatients with schizophrenia from a healthcare perspective was USD 236 per patient. This cost is similar to the direct cost for outpatients with schizophrenia reported in Tianjin, China, in 2015 (USD 231 per patient annually)Citation56 and in Nigeria in 2012 (USD 349.6 per patient annually).Citation57 In 2013, the direct costs were USD 7247 in Japan, USD 154 in the UK, USD 10,635 in Germany, USD 774 in the Netherlands, and USD 4742–29,279 in the USA.Citation58
The annual treatment cost was the highest for bipolar disorder [IDR 17,978,865 (USD 1,284) per patient] among the mental disorders in this study. This finding is consistent with that obtained in the 2017 study by Sarkar, which reported that the treatment cost was the highest for bipolar disorder among mental disorders in South India.Citation59 In 2015, in the USA, the direct cost per individual for bipolar disorder type I was approximately 13 times higher than the cost in our study of USD 17,127 [21% of the total cost in the USA (USD 81,559)].Citation60 Furthermore, we found that the direct costs of insured and uninsured individuals with bipolar disorder significantly differed. This difference might have occurred because 80% of patients with national insurance (17 of 21) received sodium divalproex for treatment, whereas only 33% (2 of 6) of uninsured patients received sodium divalproex. Sodium divalproex was assumed to be the drug that contributed the most to the high costs of medication treatment.
The annual estimated direct costs for depression and anxiety disorders in our study were IDR 1,601,850 (USD 114) and IDR 1,190,563 (USD 85) per patient, respectively. The direct costs for depression were relatively lower than those per individual in Japan in 2008 (USD 689), in the UK in 2000 (USD 264), and in the USA in 1990–2000 (USD 1195–1400).Citation61 Moreover, the direct costs for anxiety disorders were lower than those in the USA, which were estimated to be USD 1657.52 per patient in 2009–2010.Citation62
Considering the absence of official data on the prevalence of bipolar and anxiety disorders, this prevalence can be estimated by subtracting the prevalence of depression from the prevalence of all mental–emotional disorders, which yields a value of 3.7%. To estimate treatment costs, the prevalence of bipolar disorder and anxiety disorders individually were determined as 1.85% (half of 3.7%), which corresponds to approximately 3.5 million individuals. Considering these prevalence estimations, if we estimated the annual direct costs based on our results, assuming that all patients adhered to medical treatment in 1 year, the estimated annual direct costs for schizophrenia, bipolar disorder, depression, and anxiety disorders were as follows: IDR 1.5 trillion (USD 110 million), IDR 62.9 trillion (USD 4.5 billion), IDR 18.9 trillion (USD 1.3 billion), and IDR 4.2 trillion (USD 297 million), respectively. Additionally, the total estimated annual direct costs for these four disorders are IDR 87.5 trillion (USD 6.2 billion). However, this cost determined might be overestimated as it is extremely high and almost six times higher than the cost for all catastrophic diseases, which was IDR 14.6 trillion according to BPJS financial data in 2016.Citation63
Although huge costs have been estimated based on the prevalence, the costs for mental health in Indonesia will be lower than the estimations because not all individuals with mental disorders in Indonesia seek help for their condition or are adherent to medication. In our study, the mean value obtained by dividing the total number of visits by the total number of patients was 2.4, indicating that each patient visits the hospital only 2–3 times a year. This finding was in accordance with the RISKESDAS data that reported that only 9% of patients with depression in Indonesia received treatment.Citation5 A systematic review published in 2017 revealed that patients with mental disorders discontinue or show non-adherence to their medication because of poor insight, negative attitude toward medication, distressing medication side effects, poor therapeutic alliance, and stigma.Citation64 Those factors might also affect the treatment adherence of patients with mental disorders in Indonesia.
Furthermore, our study showed that there are some differences in the number of cases detected in different years. Most of the increase occurred in 2017 for all disorders. It may be assumed that the increase in the number of cases detected occurred because of the increase in the prevalence of mental disorders. This finding was consistent with the basic health research report from the Ministry of Health, Indonesia, in 2018, which stated that the prevalence of mental–emotional disorders increased from 3.8%–6% in 2013 to 9.8% in 2018.Citation5 Second, in 2017, there were changes in national guidelines. Consequently, due to the new policy, medications were unavailable in primary and secondary healthcare in some cases, resulting in several patients being referred to the national referral hospital to continue their medication. In 2018, there were some improvements in the national guidelines to ensure that the patients could yet again receive their medications in primary or secondary hospitals.
The present study has limitations because data were collected from only one national referral hospital, included only new outpatient data, and some of the data were presented descriptively. Further analyses, such as analysis of the relationships between the medication profile and treatment cost considering community income per capita and cost from a societal perspective, are necessary, and they could explain nationally representative results with regard to the medication profile and estimation of BOD for mental disorders. This study provides information on the medication profile for mental disorders, and it could be the first step to estimate the annual cost for mental disorder treatment in Indonesia.
Conclusion
The most commonly administered drugs for schizophrenia treatment were haloperidol and risperidone, those for bipolar disorders were sodium divalproex and risperidone, those for depression were fluoxetine and sertraline, and those for anxiety disorders were sertraline and lorazepam. The average estimated annual treatment costs per patient from a healthcare perspective were IDR 3,307,931 (USD 236) for schizophrenia, IDR 17,978,865 (USD 1,284) for bipolar disorder, IDR 1,601,850 (USD 114) for depression, and IDR 1,190,563 (USD 85) for anxiety disorders. Considering the increasing prevalence each year and high costs, it is important for the government and all Indonesian citizens to work toward reducing the prevalence of mental disorders in Indonesia.
Disclosure
The authors declare there is no conflicts of interest in this work.
Additional information
Funding
References
- WHO. Mental disorders affect one in four people; 2001 Available from: https://www.who.int/whr/2001/media_centre/press_release/en/. Accessed 1031, 2019.
- World Health Organization. Mental disorders; 2018 Available from: https://www.who.int/news-room/fact-sheets/detail/mental-disorders. Accessed 1031, 2019.
- Statistics Indonesia. Population 15 years of age and over by age group and type of activity during the previous week, 2008–2018; 2019 Available from: https://www.bps.go.id/statictable/2016/04/04/1904/penduduk-berumur-15-tahun-ke-atas-menurut-golongan-umur-dan-jenis-kegiatan-selama-seminggu-yang-lalu-2008—2018.html. Accessed 1125, 2019.
- SI BPS. Statistical Yearbook of Indonesia. Sub-directorate of Statistical Compilation and Publication ed.; 2018.
- Ministry of Health Republic of Indonesia. National report basic health research 2018; 2018 Available from: http://labmandat.litbang.depkes.go.id/images/download/laporan/RKD/2018/Laporan_Nasional_RKD2018_FINAL.pdf. Accessed 312, 2020.
- DiPiro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey LM. Pharmacotherapy: A Pathophysiologic Approach. 8th ed. McGraw Hill; 2011.
- Work Group on Schizophrenia. Practice Guideline for the Treatment of Patients with Schizophrenia. 2nd ed. American Psychiatric Association; 2010.
- Miyamoto S, Miyake N, Jarskog LF, Fleischhacker WW, Lieberman JA. Pharmacological treatment of schizophrenia: a critical review of the pharmacology and clinical effects of current and future therapeutic agents. Mol Psychiatry. 2012;17(12):1206–1227. doi:10.1038/mp.2012.4722584864
- Ganguly P, Soliman A, Moustafa AA. Holistic management of schizophrenia symptoms using pharmacological and non-pharmacological treatment. Front Public Heal. 2018;6(166):1–9. doi:10.3389/fpubh.2018.00166
- Vieta E. Managing Bipolar Disorder in Clinical Practice: Third Edition; 2013. doi:10.1007/978-1-908517-94-4.
- Geddes JR, Miklowitz DJ. Treatment of bipolar disorder. Lancet. 2013;381(9878):1672–1682. doi:10.1016/S0140-6736(13)60857-023663953
- Grande I, De Arce R, Jiménez-Arriero MÁ, et al. Patterns of pharmacological maintenance treatment in a community mental health services bipolar disorder cohort study (SIN-DEPRES). Int J Neuropsychopharmacol. 2013;16(3):513–523. doi:10.1017/S146114571200040522717099
- Chisholm-Burns MA, Schwinghammer TL, Well BG, Malone PA, Kolesar JM, DiPiro JT. Pharmacotherapy Principles & Practice. 4th ed. McGraw Hill Education; 2016.
- Mirabel-Sarron C, Giachetti R. Non pharmacological treatment for bipolar disorder. Encephale. 2012;38(4). doi:10.1016/S0013-7006(12)70094-5
- Kumar KPS, Srivastava S, Paswan S, Dutta AS. Depression - symptoms, causes, medications and therapies. Pharm Innovation. 2012;1(3):37.
- Spijker J, Van Straten A, Bockting CLH, Meeuwissen JAC, Van Balkom AJLM. Psychotherapy, antidepressants, and their combination for chronic major depressive disorder: a systematic review. Can J Psychiatry. 2013;58(7):386–392. doi:10.1177/07067437130580070323870720
- Wang S-M, Han C, Bahk W-M, et al. Addressing the side effects of contemporary antidepressant drugs: a comprehensive review. Chonnam Med J. 2018;54(2):101. doi:10.4068/cmj.2018.54.2.10129854675
- Wells BG, DiPiro JT, Schwinghammer TL, Dipiro CV. Pharmacotherapy Handbook. 9th ed. New York: McGraw Hill Education; 2015.
- Gartlehner G, Wagner G, Matyas N, et al. Pharmacological and non-pharmacological treatments for major depressive disorder: review of systematic reviews. BMJ Open. 2017;7(6):e014912. doi:10.1136/bmjopen-2016-014912
- Park S-C, Oh HS, Oh D-H, et al. Evidence-based, non-pharmacological treatment guideline for depression in Korea. J Korean Med Sci. 2014;29(1):12–22. doi:10.3346/jkms.2014.29.1.1224431900
- Victoria Institute of Strategic Economic Studies. The economic cost of serious mental illness and comorbidities in Australia and New Zealand. R Aust New Zeal Coll Psychiatr. 2016:1–48. Available from: https://www.ranzcp.org/Files/Publications/RANZCP-Serious-Mental-Illness.aspx. Accessed March 12, 2020.
- Gariepy G, Nitka D, Schmitz N. The association between obesity and anxiety disorders in the population: A systematic review and meta-analysis. Int J Obes. 2010;34(3):407–419. doi:10.1038/ijo.2009.252
- Reinhold JA, Mandos LA, Rickels K, Lohoff FW. Pharmacological treatment of generalized anxiety disorder. Expert Opin Pharmacother. 2011;12(16):2457–2467. doi:10.1517/14656566.2011.61849621950420
- Lampe L. Drug treatment for anxiety. Aust Prescr. 2013;36(6):186–189. doi:10.18773/austprescr.2013.076
- Strawn JR, Geracioti L, Rajdev N, Clemenza K, Levine A. Pharmacotherapy for generalized anxiety disorder in adults and pediatric patients: an evidence-based treatment review. Expert Opin Pharmacother. 2018;19(10):1057–1070. doi:10.1080/14656566.2018.149196630056792
- Bystritsky A, Khalsa SS, Cameron ME, Schiffman J. Current diagnosis and treatment of anxiety disorder. Pharm Ther. 2013;38(1):30–57.
- Combs H, Markman J. Anxiety disorders in primary care. Med Clin North Am. 2014;98(5):1007–1023. doi:10.1016/j.mcna.2014.06.00325134870
- Cottraux J. Nonpharmacological treatments for anxiety disorders. Dialogues Clin Neurosci. 2002;4(3):305–319.22034140
- Jo C. Cost-of-illness studies: concepts, scopes, and methods. Clin Mol Hepatol. 2014;20(4):327–337. doi:10.3350/cmh.2014.20.4.32725548737
- Trautmann S, Rehm J, Wittchen H. The economic costs of mental disorders. EMBO Rep. 2016;17(9):1245–1249. doi:10.15252/embr.20164295127491723
- Vos T, Barber RM, Bell B, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386(9995):743–800. doi:10.1016/S0140-6736(15)60692-426063472
- Goetzel RZ, Roemer EC, Holingue C, et al. Mental health in the workplace: a call to action proceedings from the mental health in the workplace-public health summit. J Occup Environ Med. 2018;60(4):322–330. doi:10.1097/JOM.000000000000127129280775
- Bloom D, Cafero E, Jané-Llopis E, et al. The global economic burden of non-communicable diseases. Geneva: world Economic Forum; 2011 Available from: http://www3.weforum.org/docs/WEF_Harvard_HE_GlobalEconomicBurdenNonCommunicableDiseases_2011.pdf. Accessed 1125, 2019.
- Mangalore R, Knapp M. Cost of Schizophrenia. J Ment Health Policy Econ. 2007;10(1):23–41.17417045
- Dilsaver SC. An estimate of the minimum economic burden of bipolar i and II disorders in the United States: 2009. J Affect Disord. 2011;129(1–3):79–83. doi:10.1016/j.jad.2010.08.03020888048
- Cloutier M, Greene M, Guerin A, Touya M, Wu E. The economic burden of bipolar I disorder in the United States in 2015. J Affect Disord. 2018;226:45–51. doi:10.1016/j.jad.2017.09.01128961441
- Dieleman JL, Baral R, Birger M, et al. US spending on personal health care and public health, 1996–2013. JAMA. 2016;316(24):2627–2646. doi:10.1001/jama.2016.1688528027366
- Sado M, Takechi S, Inagaki A. et al. Cost of anxiety disorders in Japan in 2008: a prevalence-based approach. BMC Psychiatry. 2013:13. doi:10.1186/1471-244X-13-338.23297686
- Okpataku CI, Tawani D, Article O. Psychotropic prescriptions for the treatment of schizophrenia in an outpatient clinic. Trends Psychiatry Psychother. 2017;39(3):165–172. doi:10.1590/2237-6089-2016-008828876362
- Khan A, Iqbal Z, Sultan SM, Nazar Z, Tariq M. Antipsychotic prescription patterns and treatment costs of schizophrenia in northwestern Pakistan: a one-year observational study. Trop J Pharm Res. 2018;17:339–344.
- Irene M. A systematic review of instruments to measure depressive symptoms in patients with schizophrenia publisher’ s pdf, also known as version of record publication date. J Affect Disord. 2012;140(1):38–47. doi:10.1016/j.jad.2011.10.01422099566
- National Collaborating Centre for Mental H. Bipolar Disorder: The NICE Guideline on the Assessment and Management of Bipolar Disorder in Adults, Children and Young People in Primary and Secondary Care. Leicester: The British Psychological Society & The Royal College of Psychiatrists; 2014.
- Chawla S, Agarwal M, Sharma S, Jiloha RC. Drug utilization study of psychotropic drugs among psychiatric outpatients in a tertiary care hospital. Indian J Pharm Sci. 2017;79(6):1008–1013. doi:10.4172/pharmaceutical-sciences.1000319
- Holzapfel EM, Szabo CP. Pharmacotherapy prescribing patterns in the treatment of bipolar disorder in a South African outpatient population. Glob Psychiatry. 2018;1(2):39–51. doi:10.2478/gp-2018-0006
- National Institute for Health and Care Excelence. Bipolar disorder: assessment and management; 2014 Available from: https://www.nice.org.uk/guidance/cg185/chapter/1-Recommendations. Accessed 1125, 2019.
- Taylor D, Paton C, Kapur S. Prescribing Guidelines in Psychiatry. 11th ed. Wiley-Blackwell; 2012.
- Turner TL. The use of antipsychotics in maintenance treatment of bipolar disorder. Ment Heal Clin. 2013;2(12):412–415. doi:10.9740/mhc.n155513
- Rossatria E. Evaluation of Antidepressants Drug Prescribing for Depressed Patients at Pharmacy Installation Outpatient in Regional Hospital Dr. Soehadi Prijonegoro Sragen; 2016.
- Yuniastuti. Evaluation of Antidepressant Drug for Therapy Patient In Depression Mental Hospital Surakarta 2011–2012; 2013.
- Ogawa Y, Takeshima N, Hayasaka Y, et al. Antidepressants plus benzodiazepines for adults with major depression. Cochrane Database Syst Rev. 2019;2019(6). doi:10.1002/14651858.CD001026.pub2
- Bandelow B, Zohar J, Hollander E, et al. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the pharmacological treatment of anxiety, obsessive-compulsive and post-traumatic stress disorders - First revision. World J Biol Psychiatry. 2008;9(4):248–312. doi:10.1080/1562297080246580718949648
- Farach FJ, Pruitt LD, Jun JJ, Jerud AB, Zoellner LA, Roy-Byrne PP. Pharmacological treatment of anxiety disorders: current treatments and future directions. J Anxiety Disord. 2012;26(8):833–843. doi:10.1016/j.janxdis.2012.07.00923023162
- Tanguay Bernard MM, Luc M, Carrier JD, et al. Patterns of benzodiazepines use in primary care adults with anxiety disorders. Heliyon. 2018;4(7). doi:10.1016/j.heliyon.2018.e00688
- Crocco EA, Jaramillo S, Cruz-Ortiz C, Camfield K. Pharmacological management of anxiety disorders in the elderly. Curr Treat Options Psychiatry. 2017;4(1):33–46. doi:10.1007/s40501-017-0102-428948135
- Ellen S, Selzer R, Norman T, Blashki G. Depression and anxiety: pharmacological treatment in general practice. Aust Fam Physician. 2007;36(4):222–228.17392933
- Ye W. Health care resource use and direct medical costs for patients with schizophrenia in Tianjin, People’ s Republic of China. Neuropsychiatr Dis Treat. 2015;11:983–990.25897235
- Oloniniyi IO, Akinsulore A, ALoba OO, Mapayi BM, Oginni OA, Makanjuola R. Economic cost of schizophrenia in a Nigerian Teaching Hospital. J Neurosci Rural Pract. 2019;10(1):39–47. doi:10.4103/jnrp.jnrp_210_1830765969
- Chong HY, Teoh SL, Wu DB-C, Kotirum S, Chiou C-F, Chaiyakunapruk N. Global economic burden of schizophrenia: a systematic review. Neuropsychiatr Dis Treat. 2016;12:357–373. doi:10.2147/NDT.S9664926937191
- Sarkar S, Mathan K, Sakey S, Shaik S, Subramanian K, Kattimani S. Cost-of-treatment of clinically stable severe mental lilnesses in India. Indian J Soc Psychiatry. 2017;33(3):262. doi:10.4103/0971-9962.214600
- Cloutier M, Greene M, Guerin A, Touya M, Wu E. The economic burden of bipolar I disorder in the United States in 2015. J Affect Disord. 2018;15(226):45–51. doi:10.1016/j.jad.2017.09.011
- Okumura Y, Higuchi T. Cost of depression among adults in Japan. Prim Care Companion CNS Disord. 2011;13(3):PCC.10m01082. doi:10.4088/PCC.10m01082
- Shirneshan E, Bailey J, Relyea G, Franklin BE, Solomon DK, Brown LM. Incremental direct medical expenditures associated with anxiety disorders for the U.S. adult population: evidence from the medical expenditure panel survey. J Anxiety Disord. 2013;27(7):720–727. doi:10.1016/j.janxdis.2013.09.00924135257
- Ministry of Health Republic Indonesia. Heart disease is the highest cause of death, Ministry of Health reminds the CERDIK; 2017 Available from: https://www.depkes.go.id/article/view/17073100005/penyakit-jantung-penyebab-kematian-tertinggi-kemenkes-ingatkan-cerdik.html. Accessed 1030, 2019.
- Velligan DI, Sajatovic M, Hatch A, Kramata P, Docherty JP. Why do psychiatric patients stop antipsychotic medication? A systematic review of reasons for nonadherence to medication in patients with serious mental illness. Patient Prefer Adherence. 2017;11:449–468. doi:10.2147/PPA.S12465828424542