Abstract
Objective
To investigate the association of genetic polymorphisms of SIRT with postpartum depressive symptoms and analyze the risk factors for postpartum depressive symptoms in women following cesarean section.
Methods
A total of 368 Chinese woman undergoing cesarean section were enrolled in this study. A cutoff of ≥10 for the Edinburgh Postnatal Depression Scale identified postpartum depressive symptoms. Genotypes of SIRT1, SIRT2, and SIRT6 were determined using Sequenom MassArray single-nucleotide polymorphism (SNP) analysis. We analyzed the contribution of genetic factors (SNPs, linkage disequilibrium, and haplotype) to postpartum depressive symptoms and performed logistic regression analysis to identify all potential risk factors for postpartum depressive symptoms and define interactions between genetic and environmental factors.
Results
The incidence of postpartum depressive symptoms was 18.7% in this cohort. Univariate analysis suggested that SIRT2 polymorphism at rs2873703 (TT genotype) and rs4801933 ((TT genotype) and SIRT6 polymorphism at rs350846 (CC genotype) and rs107251 (TT genotype) were significantly correlated with the occurrence of postpartum depressive symptoms (p<0.05). Linkage disequilibrium was identified between SIRT6 polymorphisms rs350846 and rs107251. Incidence of postpartum depressive symptoms in cesarean-section parturients with SIRT2 haplotype CCC was decreased (OR 0.407, 95% CI 0.191–0.867; p=0.016). SIRT2 polymorphisms rs2873703 and rs4801933 were multiply collinear. Logistic regression analysis showed that SIRT2 polymorphism at rs2873703 (TT genotype) and rs4801933 (TT genotype), domestic violence, stress during pregnancy, and depressive prenatal mood were risk factors for postpartum depressive symptoms (p<0.05).
Conclusion
Pregnant women with SIRT2 genotypes rs2873703 TT and rs4801933 TT and experiencing domestic violence, stress during pregnancy, and prenatal depression are more likely to suffer from postpartum depressive symptoms.
Introduction
Postpartum depressive symptoms (PDSs) are serious psychiatric disorders that have a deep impact on maternal life quality. PDSs can be fatal: suicide accounts for approximately 20% of postpartum deaths.Citation1–Citation3 PDSs also have adverse effects on family relationships, including marital and maternal–infant interaction problems, which can result in poor physiological and psychological health of offspring.Citation4–Citation6 In recent decades, countries around the world have conducted extensive research on postpartum depression. The etiology and causes of PDSs are considered multifactorial, including hormonal changes, genetic risk factors, inflammation, and psychosocial stress, during pregnancy and the perinatal period.Citation7 However, the pathophysiology of the PDSs has still to be elucidated.
Mounting evidence suggests that epigenetic mechanisms, which induce stable and lasting changes in gene expression in response to environmental events and behavioral experiences, may play a role in processes that contribute to the pathophysiology of psychiatric disorders.Citation8 It is well known that histone deacetylation is one of the most important mechanisms of epigenetic modification and contributes a lot in regulating gene transcription and translation. Hobara et al described in their study that aberrant transcriptional regulation caused by the altered expression of HDAC was associated with the pathophysiology of mood disorders.Citation9 Interestingly, Hollis et al observed a trend toward decreased HDAC3 mRNA levels following social defeat exposure.Citation10 Schroeder et al showed in their study that the HDAC inhibitor sodium butyrate exerted antidepressant-like effects in the mouse.Citation11 Meanwhile, in a large and growing body of literature, some HDAC enzymes have been proposed as epigenetic targets involved in the pathophysiology of depression and antidepressant-like action.Citation12
Sirtuins are HDAC3s. They mediate histone deacetylation in an NAD+-dependent manner and can deacetylate proteins other than histones, which involves a variety of pathophysiological processes.Citation13 Recent studies have shown that SIRT plays an important role in the pathophysiology and treatment of depression. Clinical studies have shown that sirtuin is closely related to depression.Citation14 Animal experiments have suggested that stress and inflammation can affect the main subtypes of the sirtuin family, some of which are related to the pathogenesis of depression.Citation15 A recent large-scale genome-wide association study showed that genetic variants near the SIRT1 gene were significantly associated with major depressive disorders, suggesting that SIRT1 may participate in the pathogenesis of major depressive disorder.Citation16 Interestingly, a recent study reported that changes in SIRT1, SIRT2, and SIRT6 mRNA expression in peripheral blood cells may be a useful biomarker for mood disorders.Citation17 Numerous studies conducted by Kishi et al have shown that SIRT1 is associated with major depressive disorder in the Japanese population.Citation18 Recently, Liu et al found that SIRT2 is involved in the modulation of depressive behaviors.Citation19
Many studies have shown that tryptophan-metabolism disorder, induced by perinatal stress and inflammatory response, is one of the significant mechanisms of PDSs.Citation20,Citation21 As one of the end products of tryptophan metabolism, NAD+ is an important coenzyme of sirtuins. Studies have shown that SIRT participates in the pathophysiology and treatment of depression.Citation22–Citation24 Therefore, SIRT may be involved in the pathogenesis of PDSs, but it is not clear that it gene is involved in PDSs from the perspective of genetics. This study aimed to select parturients undergoing cesarean section to screen SIRT for single-nucleotide polymorphisms (SNPs) based on individual genes and genomes, explore the relationship between SIRT polymorphism and postpartum depression after cesarean section, provide a genetic basis for individual differences in postpartum depression, and to provide an important reference for predicting genetic susceptibility to postpartum depression. From the perspective of genetics, it provides new ideas for the pathogenesis and treatment of diseases.
Methods
Protocol
This study was approved by the local ethics committee (P2014/s155, February 20, 2014) and was nationally registered in the Chinese Clinical Trials Registry (CHICTR-ROC-17013357). All participants provided written informed consent before entering the study.
Study Participants
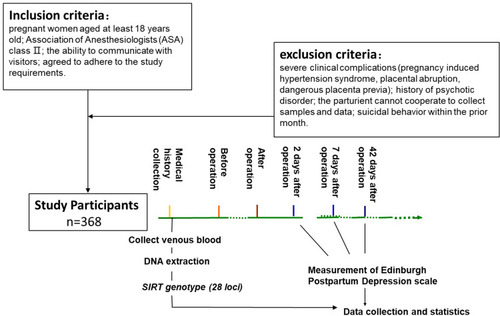
By using the sample size–calculation formula for a cohort study, 237 patients needed to be included to attain statistical significance (). A total of 368 participants who undergone cesarean sections at the Third Xiangya Hospital of Central South University were enrolled, and all agreed to postoperative intravenous analgesia. Eligibility criteria were pregnant and aged at least 18 years, American Association of Anesthesiologists class II status, ability to communicate with visitors, and agreement to adhere to the study requirements.Citation25 Exclusion criteria were severe clinical complications (pregnancy-induced hypertension syndrome, placental abruption, dangerous placenta previa), history of psychotic disorder, not cooperating with collection of samples and data, and suicidal behavior within the previous month.Citation2
Collection of General Data, Clinical Data, and Samples of Parturients
A preoperative questionnaire was used to collect basic information on all parturients, including age, height, weight, gestational age, whether unipara or not, education, employment and partner employment, monthly family income, artificial or natural pregnancy, and planned or unintended pregnancy. We used the Pregnancy Pressure Scale, and parturients were assessed on severe/moderate/ mild stress during pregnancy,Citation25 good/moderate/poor marital relationship, mood during pregnancy, and domestic violence during pregnancy, defined as one or more acts or threats of physical, sexual, or psychological/emotional violence reported by any family member ().Citation26 Additionally, prenatal depressive symptoms were assessed with the Edinburgh Postnatal Depression Scale (EPDS) by trained investigators.Citation27–Citation29 Finally, 2 mL venous blood was taken from each woman and marked with name and serial number in anticoagulant vessels containing EDTA, then stored in a freezer at −20°C.
Maternal Surgery, Postpartum Follow-Up, and Determination of Outcome Indicators
All women were admitted to the operating room after preoperative preparation. Monitoring was conducted using of electrocardiography, noninvasive blood pressure, and heart rate. Oxygen was administered by clear nasal catheter until delivery at a rate of 2L/minute. Subarachnoid block was performed with a disposable spinal–epidural anesthesia puncture bag (Tuoren Medical Devices, Henan, China). After skin disinfection and local anesthesia with lidocaine, a 25 G needle was inserted at the L3–L4 or L2–L3 interspace. When cerebrospinal fluid flowed, 1% ropivacaine 1.5 mL + 10% fentanyl 25 µg + 10% glucose solution 0.5 mL was administered into the subarachnoid space, aiming for a level of analgesia <T4. Attention was paid to observe and prevent supine hypotension syndrome.
After the anesthetic effect had met surgical conditions, the surgeon began the operation and performed cesarean section of the lower segment of the uterus. Changes of electrocardiography and output were closely observed during the operation. After the fetus had been removed, it was weighed to determine whether or not to transfer it to the neonatal intensive care unit according to maternal condition and birth quality. After the placenta had been removed by surgery and sutured layer by layer, it was decided whether to transfer the mother to postanesthesia care unit or back to the ward, according to the anesthesia resuscitation.
The parturients were evaluated with the EPDS at 2, 7, and 42 days after delivery. Scores ≥10 at 42 days after delivery were regarded as postpartum depression, and scores ≥10 on the day before delivery were rated as prenatal depression.Citation28,Citation30 Self-harm ideation (the last EPDS item) was assessed before childbirth on postpartum days 7 and 42, with parturients who gave a response of “yes, quite often”, “sometimes”, or “seldom”, being categorized as “yes”, with only a response of “never” being classified as “no”. If parturients could not be contacted on days 7 and 42 after delivery, the investigator could call them again within 2 days. If there were still no response, these cases were classified as lost.
Selection of SNP Loci
SNP loci were selected by querying the relevant literature to understand the SNP loci active in related SIRT research,especially those active in the field of psychosomatic medicine; querying relevant SNP sites in the dbSNP database so as to select SNP sites and coding sequences; (3) and querying the Ensembl website to download relevant files and import Haploview software so as to view and select SNP sites of the Beijing and southern populations. Loci selection also needed to meet a minimum allele frequency of >0.05. Genotypes of 28 SIRT loci were selected and gene polymorphisms of these analyzed with Sequenom MassArray (gene chip; ).
Table 1 Correlations between SIRT polymorphisms and postpartum depressive symptoms
Statistical Analysis
SPSS 23.0 was used to analyze all data. Measurement data are described as means ± SD, and counting and grade data as rate or constituent ratio. The relationship between the basic data of selected parturients and PDSs was assessed by χ2 and t-testsor . T^he Hardy–Weinberg equilibrium test was used for all SNP loci, and χ2 to analyze the relationship between the incidence of PDSs and SNPs. In addition, linkage-disequilibrium analysis and haploid analysis of SNPs were carried out on the SHEsis platform. Collinear analysis was used to find collinear factors and eliminate the list of multivariate analysis, and then logistic regression analysis was used to analyze the relationship between PDSs and various factors (forced-entry method). Factors with variance-inflation factor >10 and independent variables with tolerance <0.2 may have multiple collinearity. Interactions between genes and environment were analyzed with GMDR software. There was a statistical difference between the two sides if p<0.05.
Results
General Data and Analysis of Postpartum Depressive Symptoms
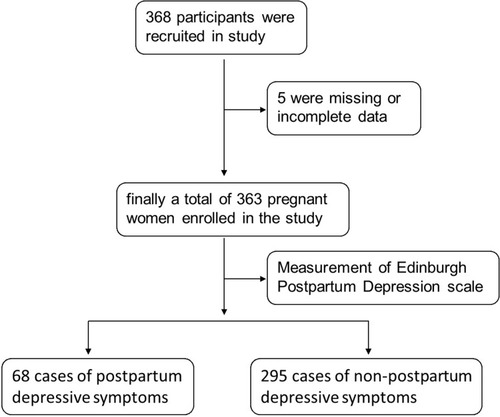
In this study, 368 participants were recruited, of which five were missing or had incomplete data, and finally a total of 363 pregnant women were enrolled in the study. Among the 363 pregnant women, there were 68 cases of PDSs, with an incidence of 18.7%. Among the 68 patients with PDSs, 39 had relatively low EPDS scores (<13) and 29 had relatively high EPDS scores (≥13).
Results showed that there was no significant difference in age (29.87±4.528 vs 30.28±4.513 years, t=0.682, df 360, Cohen’s p=0.092; p=0.495), height (1.59±0.047 vs.1.59±0.046 m, t=−0.173, Cohen’s p=−0.023, df 361; p=0.826), prepregnancy weight (53.85±7.908 vs 53.76±8.579 kg, t=−0.073, df 355, Cohen’s p=−0.010 p=0.942), prenatal weight (70.62±8.327 vs 70.34±9.727 kg, t=−0.220, df 361, Cohen’s p=−0.030 p=0.826), and preoperative BMI (27.83±2.970 vs 27.76±3.704, t=−0.146, df 361, Cohen’s p=−0.020; p=0.884) between PDSs and no PDSs (p>0.05). Therefore, the two groups were regarded as comparable in terms of age and body shape.
When using χ2 to compare general and clinical data of parturients, we found differences in pregnancy stress, domestic violence, and depressive prenatal mood between PDSs and no PDSs (p<0.05). Compared with ordinary cesarean section, incidence of PDSs in pregnant women suffering domestic violence was significantly higher (OR 7.02, 95% CI 1.92–25.60; p=0.004). Incidence of PDSs of parturients undergoing cesarean section was significantly higher than pregnant women with high stress and low stress and between moderate stress and low stress (OR 3.714, 95% CI 1.660–8.312 and OR 2.615, 95% CI 1.428–4.789, respectively). The likelihood of PDSs in pregnant women with prenatal depression was significantly higher than women without prenatal depression (OR 5.35, 95% CI 3.02–9.48; p=0; ).
Table 2 General information on parturients and incidence of PDSs, n (%)
Univariate Analysis of SIRT Polymorphisms and Postpartum Depressive Symptoms
All selected SNPs conformed to the Hardy–Weinberg equilibrium and were genetically representative and able to be used for gene analysis. IncidencePDSs after cesarean section in each genotype of SIRT polymorphisms rs350846, rs352492, rs107251, rs2873703, rs4801933, and rs2503071 was different. Further analysis and comparison showed that homozygous TT with rs2873703 mutation at SNP sites of SIRT2 had higher incidence of PDSs (OR 2.610, 95% CI 1.238–5.501; p=0.009) than wild-type homozygous CC and heterozygous CT. Compared with wild-type homozygote CC and heterozygote CT, homozygous TT with rs4801933 mutation at SNP sites of SIRT2 had higher incidence of PDSs (OR 2.307, 95% CI 1.091–4.876; p=0.025). SIRT6 gene SNP locus rs350846 wild homozygous CC has a higher incidence of PDSs than mutant homozygous GG and heterozygous CG (OR 2.539, 95% CI 1.122–5.749; p=0.021). SIRT6 SNP locus rs107251 wild homozygous TT had higher incidence of PDSs than mutant homozygous CC and heterozygous TC (OR 2.371, 95% CI 1.054–5.330; p=0.032; ).
Linkage-Disequilibrium Test and Haplotype Analysis of SIRT Loci
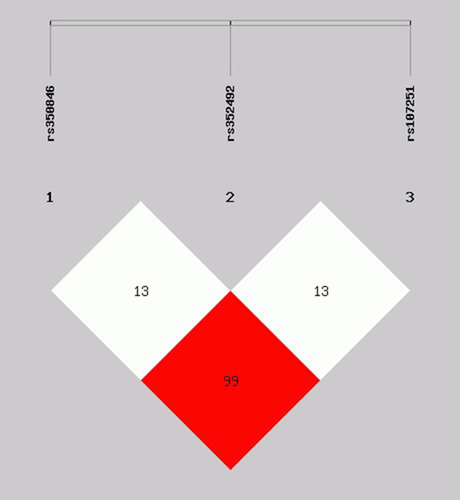
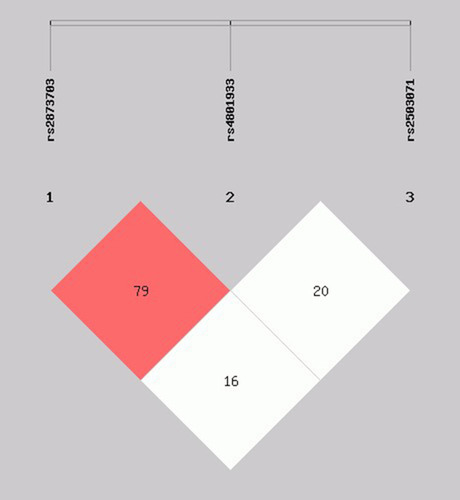
SHEsis software was used to detect linkage disequilibrium of rs2873703, rs4801933, and rs2503071 in SIRT2. R2>0.8 indicated that there was disequilibrium between the two loci. There was little linkage disequilibrium between rs2873703 and rs4801933 (). Haplotypes of SIRT2 rs2873703, rs4801933, and rs2503071 loci gene three haplotypes (CCC, TTC, TTG) with frequency >0.03 were analyzed. Haplotype analysis showed that incidence of PDSs after cesarean section was decreased in parturients with haplotype CCC (p<0.05, ).
Table 3 Haplotype analysis of SIRT2 and SIRT6 loci
Figure 3 Linkage-disequilibrium test of SIRT2 loci rs2873703, rs4801933, and rs2503071. The white square represents the weaker linkage disequilibrium between the two loci, and the red square stronger linkage disequilibrium.
SHEsis software was used to detect linkage disequilibrium of SIRT6 rs350846, rs352492, and rs107251 loci. R2>0.80 indicated that there was disequilibrium between the two loci. The results showed that there was linkage imbalance between rs350846 and rs107251 (). Haplotypes of SIRT6 rs350846, rs352492, and rs107251 lociand three haplotypes (CCT, GCC, GTC) with frequency >0.03 were analyzed. The results showed that the haplotypes of SIRT6 rs350846, rs352492, and rs107251 loci gene were not be associated with PDSs in parturients undergoing cesarean section (p>0.05, ).
Multivariate Analysis of SIRT Polymorphisms and Postpartum Depressive Symptoms
Before establishing the regression model, we first conducted a collinear analysis of all the variables. After assessing correlations between the two variables and the multiple collinearity test, the results showed that rs2873703 and rs4801933 and rs350846 and rs107251 had multiple collinearity. Therefore, rs4801933 and rs107251 were excluded and logistic multivariate analysis was carried out.Citation31
Finally, the variables selected were analyzed by logistic analysis, and results are shown in . Domestic violence (OR 6.59, 95% CI 1.47–29.61; p=0.014), stress during pregnancy (OR 1.67, 95% CI 1.09–2.56; p=0.020), prenatal depression (OR 5.11, 95% CI 2.73–9.55; p=0), and polymorphic rs2873703 genotype TT (OR 3.27, 95% CI 1.46–7.32; p=0.004) were risk factors for PDSs. Because of the multicollinearity and weak linkage disequilibrium between rs2873703 and rs4801933, rs4801933 was also associated with PDSs.
Table 4 Multivariate logistic analysis of risk factors for postpartum depressive symptoms
Interaction Between SIRT and Environment
Identification of gene–environment joint action is one of the most important and challenging topics in human genetics and genetic epidemiology. GMDR software was used to analyze the interaction between SIRT2 rs2873703 and environmental factors (stress during pregnancy and domestic violence) entering the regression equation. The results showed that there was no significant interaction among the three factors (the model did not pass the 10+10 cross-validation test; ).
Table 5 Interactive analysis of genetic polymorphisms and environmental factors
Discussion
The major findings in this study were that SIRT2 polymorphisms were associated with PDS incidence, compared to parturients carrying a CC or CT genotype, those carrying the the TT genotype in rs2873703 (SIRT2) were at higher risk of PDSs, and domestic violence, stress during pregnancy, and prenatal depression were risk factors for PDSs. In addition, we found that overall of PDS incidence based on EPDS score (cutoff ≥10) was 18.7%, which was basically consistent with other literature.Citation32
Sirtuins are a family of NAD+-dependent enzymes that regulate cellular functions through deacetylation of protein targets. The mammalian sirtuin family consists of seven sirtuins (SIRT1–7). SIRTs modulate major biological pathways, such as stress response, protein aggregation, and inflammatory processes, which are involved in neurodegenerative diseases.Citation33 SIRT2 is a major deacetylase that has some common substrates in both cytoplasm and nucleis.Citation17 It has been reported that the rs10410544 polymorphism of SIRT2 is associated with depression in Alzheimer’s disease patients.Citation23 In the present study, we found that SIRT2 polymorphism at rs2873703 and rs4801933 was associated with depression. Particularly, both TT genotypes were associated with a higher risk of developing PDSs. Kim et al demonstrated that infusion of the aspecific sirtuin agonist resveratrol promoted depression and anxiety-like behavioral deficits.Citation15 What is more, Ferland et al suggested that sirtuin inhibition is a therapeutic target for cognitive effects of depression.Citation34 A previous study showed that the SIRT2 inhibitor 33i reverted chronic mild stress–induced depressive-like behaviors,Citation24 whereas another study showed that inhibiting SIRT2 with tenovin D3 resulted in depression-like behavior.Citation19 As far as we know, rs2873703 is the first SIRT2 polymorphism found to be related to the incidence of postpartum depression. Because it is located in the noncoding region, we think that rs2873703 may be linked with rs4801933, which may cause changes in SIRT expression, then lead to the disease. Another assumption is that the single mutation of rs2873703 may affect gene transcription and translation, then result in disease. However, these conjectures need further confirmation.
SIRT6 plays a key role in sirtuin family, and is highly expressed in nuclei of skeletal muscle, brain, heart, liver, and thyroid. Michishita et al suggested that SIRT6 may regulate gene transcription by removing acetyl groups ofhistone H3, transcription factors, and cotranscription factors,Citation35 while Lappas et al and Wu et al reported that SIRT6 can regulate the expression of many inflammatory factors through NFκB and alleviate inflammatory injury.Citation36,Citation37 Considerable evidence suggests that SIRT6 is associated with neuropsychiatric diseases. We analyzed the influence of SIRT polymorphisms on the occurrence of PDSs, finding that the SIRT6 polymorphic rs350846 genotype CC and rs107251 genotype TT increased the incidence of postpartum depression (p<0.05). Mao et al reported that expression of SIRT6 in the hippocampus was increased in chronically stress rats with depression.Citation38 Iwata et al suggested that the inflammasome is a central mediator by which psychological and physical stressors can contribute to the development of depression.Citation39 Together, these studies have supported the view that SIRT6 may be involved in the occurrence of PDSs by regulating the expression of many inflammatory factors and inducing nerve-cell injury.
A series of previous studies have shown that environmental factors can modulate PDS occurrence.Citation40,Citation41 Our data indicated a role for pregnancy stress, domestic violence, and depressive prenatal mood in PDSs. Consistent with a systematic review,Citation42 multivariate analysis showed that depressive prenatal mood was a strong predictor of PDSs, and the risk of PDSs in women with depressive prenatal mood during cesarean section was five times that of women with no prenatal depression. It also suggested that in addition to genetic factors that cannot be interfered with, we need to pay attention not only to the postpartum psychological and emotional state but also to understanding the prenatal psychological and emotional state. Research has found that there is a correlation between pregnancy stress and PDSs.Citation43,Citation44 Abnormal stress regulation during pregnancy and changes in the hypothalamic–pituitary–adrenal axis may contribute to the occurrence of PDSs. This study also supports the view that domestic violence can increase the risk of PDSs.Citation45 In view of the composition of family relations in Chinese society, marriage bonds and the relationship between mother-in-law and daughter-in-law are worthy of attention. After calculation, there was a moderate correlation between these (r=0.501). The relationship between mother-in-law and daughter-in-law is extremely sensitive in the family. A study also found that compared with those living only with their husbands, women living with their parents-in-law had a higher risk of PDSs.Citation46 However, this association was not found in this study. Moreover, a previous study showed that perinatal stress events, suicidal tendencies, and lower socioeconomic status also increased the incidence of PDSs,Citation47 but this association was not found in this study. To account for this, it may be that maternal response to stress events and suicidal response are relatively evasive, with few total positive events causing statistical analysis results to be less objective. It is also of note that the socioeconomic evaluation should adopt some domestically and internationally recognized evaluation criteria, rather than just comparison of income levels.
PDSs are a complex multifactorial disease that involves chronic changes in the structure and function of neural circuits. As mentioned, environmental and genetic susceptibility play significant roles in the pathogenesis of depression.Citation7 Epigenetics is an important new field in depression research, and provides a mechanism for understanding the link between adverse environmental stimuli and changes in gene expression associated with depression.Citation48 This study also analyzed interactions between SIRT polymorphisms and the environment. We found that SIRT rs2873703 and rs4801933 had no significant interaction with pregnancy stress or domestic violence. Nevertheless, there was insufficient evidence to prove that the interaction between SIRT polymorphism and environmental factors was involved in the mechanism of PDSs.
There are some limitations in the present study. First of all, the population consisted of cesarean section patients only and not compared to normal deliveries. Secondly, this was a single-center study, and relevant research parameters should be investigated in future multicenter investigations. In addition, the sample of this study was relatively small, and some clinical observation indicators, such as husband–wife relationship and mother-in-law and daughter-in-law relationship are relatively lacking in objective and recognized evaluation criteria.
In summary, this study explored the related factors of PDSs in women after cesarean section. The results suggest that rs2873703 and rs4801933 in SIRT2 are factorsin susceptibility to PDSs. This study proposes for the first time that SIRT2 polymorphisms may play a certain role in the pathogenesis of PDSs, which provides a reference for promoting the genetic mechanism of SIRT in the pathogenesis of PDSs. Furthermore, adverse environmental stimulation and negative emotions werere also factors in susceptibility to PDSs after cesarean section. It is suggested that more attention be paid to the psychological state and living environment of women during pregnancy, in order to reduce the risk of PDSs and improve their quality of life.
Abbreviations
PDSs, postpartum depressive symptoms; EPDS, Edinburgh Postnatal Depression Scale; SNP, single-nucleotide polymorphism.
Data-Sharing Statement
The data sets used during thist study are available from the corresponding author on reasonable request.
Ethics and Consent
The study protocol was registered (Chinese Clinical Registry — CHICTR-ROC-17013357). The study was conducted in accordance with the Declaration of Helsinki (World Medical Association 2013) using procedures that had been approved by the ethics committee of the Third Xiangya Hospital of Central South University (P2014/s155, February 20, 2014). Informed consent was obtained from all participants.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval to the version to be published, and agree to be accountable for all aspects of the work.
Acknowledgment
We are deeply grateful to all the women who participated in this study and to all who collaborated.
Disclosure
The authors report no conflicts of interest for this work. There are no personal, organizational, or financial conflicts of interest.
Additional information
Funding
References
- O’Hara MW, McCabe JE. Postpartum depressive symptoms: current status and future directions. Annu Rev Clin Psychol. 2013;9(1):379–407. doi:10.1146/annurev-clinpsy-050212-18561223394227
- Duan K-M, Wang S-Y, Yin J-Y, et al. The IDO genetic polymorphisms and postpartum depressive symptoms: an association study in Chinese parturient-mothers who underwent cesarean section. Arch Women's Ment Health. 2019;22(3):339–348. doi:10.1007/s00737-018-0898-y30121843
- Lindahl V, Pearson JL, Colpe L. Prevalence of suicidality during pregnancy and the postpartum. Arch Women's Ment Health. 2005;8(2):77–87. doi:10.1007/s00737-005-0080-115883651
- Farías-Antúnez S, Xavier MO, Santos IS. Effect of maternal postpartum depressive symptoms on offspring’s growth. J Affect Disord. 2018;228:143–152. doi:10.1016/j.jad.2017.12.01329248820
- Hannigan LJ, Eilertsen EM, Gjerde LC, et al. Maternal prenatal depressive symptoms and risk for early-life psychopathology in offspring: genetic analyses in the Norwegian Mother and Child Birth Cohort Study. Lancet Psychiatry. 2018;5(10):808–815. doi:10.1016/S2215-0366(18)30225-630245187
- Plant DT, Pariante CM, Sharp D, Pawlby S. Maternal depression during pregnancy and offspring depression in adulthood: role of child maltreatment. Br J Psychiatry. 2015;207(3):213–220. doi:10.1192/bjp.bp.114.15662026045352
- Payne JL, Maguire J. Pathophysiological mechanisms implicated in postpartum depressive symptoms. Front Neuroendocrinol. 2019;52:165–180. doi:10.1016/j.yfrne.2018.12.00130552910
- Park C, Rosenblat JD, Brietzke E, et al. Stress, epigenetics and depression: a systematic review. Neurosci Biobehav Rev. 2019;102:139–152. doi:10.1016/j.neubiorev.2019.04.01031005627
- Hobara T, Uchida S, Otsuki K, et al. Altered gene expression of histone deacetylases in mood disorder patients. J Psychiatr Res. 2010;44(5):263–270. doi:10.1016/j.jpsychires.2009.08.01519767015
- Hollis F, Duclot F, Gunjan A, Kabbaj M. Individual differences in the effect of social defeat on anhedonia and histone acetylation in the rat hippocampus. Horm Behav. 2011;59(3):331–337. doi:10.1016/j.yhbeh.2010.09.00520851702
- Schroeder FA, Lin CL, Crusio WE, Akbarian S. Antidepressant-like effects of the histone deacetylase inhibitor, sodium butyrate, in the mouse. Biol Psychiatry. 2007;62(1):55–64. doi:10.1016/j.biopsych.2006.06.03616945350
- Martínez-Pacheco H, Picazo O, López-Torres A, et al. Biochemical and behavioral characterization of IN14, a new inhibitor of HDACs with antidepressant-like properties. Biomolecules. 2020;10(2):299. doi:10.3390/biom10020299
- Roomruangwong C, Anderson G, Berk M, et al. A neuro-immune, neuro-oxidative and neuro-nitrosative model of prenatal and postpartum depression. Prog Neuropsychopharmacol Biol Psychiatry. 2018;81:262–274. doi:10.1016/j.pnpbp.2017.09.01528941769
- Luo X-J, Zhang C. Down-regulation of SIRT1 gene expression in major depressive disorder. AJP. 2016;173(10):1046. doi:10.1176/appi.ajp.2016.16040394
- Kim H-D, Hesterman J, Call T, et al. SIRT1 mediates depression-like behaviors in the nucleus accumbens. J Neurosci. 2016;36(32):8441–8452. doi:10.1523/JNEUROSCI.0212-16.201627511015
- CONVERGE consortium. Sparse whole-genome sequencing identifies two loci for major depressive disorder. Nature. 2015;523(7562):588–591. doi:10.1038/nature14659.26176920
- Abe N, Uchida S, Otsuki K, et al. Altered sirtuin deacetylase gene expression in patients with a mood disorder. J Psychiatr Res. 2011;45(8):1106–1112. doi:10.1016/j.jpsychires.2011.01.01621349544
- Kishi T, Yoshimura R, Kitajima T, et al. SIRT1 gene is associated with major depressive disorder in the Japanese population. J Affect Disord. 2010;126(1–2):167–173. doi:10.1016/j.jad.2010.04.00320451257
- Liu R, Dang W, Du Y, et al. SIRT2 is involved in the modulation of depressive behaviors. Sci Rep. 2015;5(1). doi:10.1038/srep08415
- Duan K-M, Ma J-H, Wang S-Y, et al. The role of tryptophan metabolism in postpartum depression. Metab Brain Dis. 2018;33(3):647–660. doi:10.1007/s11011-017-0178-y29307018
- Anderson GM. Postpartum depression: psychoneuroimmunological underpinnings and treatment. NDT. 2013;277. doi:10.2147/NDT.S25320.
- Abe-Higuchi N, Uchida S, Yamagata H, et al. Hippocampal sirtuin 1 signaling mediates depression-like behavior. Biol Psychiatry. 2016;80(11):815–826. doi:10.1016/j.biopsych.2016.01.00927016384
- Porcelli S, Salfi R, Politis A, et al. Association between sirtuin 2 gene rs10410544 polymorphism and depression in alzheimer’s disease in two independent European samples. J Neural Transm. 2013;120(12):1709–1715. doi:10.1007/s00702-013-1045-623712749
- Erburu M, Muñoz-Cobo I, Diaz-Perdigon T, et al. SIRT2 inhibition modulate glutamate and serotonin systems in the prefrontal cortex and induces antidepressant-like action. Neuropharmacology. 2017;117:195–208. doi:10.1016/j.neuropharm.2017.01.03328185898
- Wang S-Y, Duan K-M, Tan X-F, et al. Genetic variants of the kynurenine-3-monooxygenase and postpartum depressive symptoms after cesarean section in Chinese women. J Affect Disord. 2017;215:94–101. doi:10.1016/j.jad.2017.03.02328319697
- Krug EG, Mercy JA, Dahlberg LL, Zwi AB. The world report on violence and health. Lancet. 2002;360(9339):1083–1088. doi:10.1016/S0140-6736(02)11133-012384003
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: development of the 10-item edinburgh postnatal depression scale. Br J Psychiatry. 1987;150(6):782–786. doi:10.1192/bjp.150.6.7823651732
- Lee DTS, Yip SK, Chiu HFK, et al. Detecting postnatal depression in Chinese women. Br J Psychiatry. 1998;6. doi:10.1192/bjp.172.5.433
- Hewitt C, Gilbody S, Brealey S, et al. Methods to identify postnatal depression in primary care: an integrated evidence synthesis and value of information analysis. Health Technol Assess. 2009;13(36):36. doi:10.3310/hta13360
- Lakkis NA, Mahmassani DM. Screening instruments for depression in primary care: a concise review for clinicians. Postgrad Med. 2015;127(1):99–106. doi:10.1080/00325481.2015.99272125526224
- Hidalgo B, Goodman M. Multivariate or multivariable regression? Am J Public Health. 2013;103(1):39–40. doi:10.2105/AJPH.2012.30089723153131
- Gelaye B, Rondon MB, Araya R, Williams MA. Epidemiology of maternal depression, risk factors, and child outcomes in low-income and middle-income countries. Lancet Psychiatry. 2016;3(10):973–982. doi:10.1016/S2215-0366(16)30284-X27650773
- Han S-H. Potential role of sirtuin as a therapeutic target for neurodegenerative diseases. J Clin Neurol. 2009;5(3):120. doi:10.3988/jcn.2009.5.3.12019826562
- Ferland CL, Hawley WR, Puckett RE, et al. Sirtuin activity in dentate gyrus contributes to chronic stress-induced behavior and extracellular signal-regulated protein kinases 1 and 2 cascade changes in the hippocampus. Biol Psychiatry. 2013;74(12):927–935. doi:10.1016/j.biopsych.2013.07.02924011821
- Michishita E, McCord RA, Berber E, et al. SIRT6 is a histone H3 lysine 9 deacetylase that modulates telomeric chromatin. Nature. 2008;452(7186):492–496. doi:10.1038/nature0673618337721
- Lappas M. Anti-inflammatory properties of sirtuin 6 in human umbilical vein endothelial cells. Mediators Inflamm. 2012;2012:1–11. doi:10.1155/2012/597514
- Wu Y, Chen L, Wang Y, et al. Overexpression of sirtuin 6 suppresses cellular senescence and NF-κB mediated inflammatory responses in osteoarthritis development. Sci Rep. 2015;5(1):17602. doi:10.1038/srep1760226639398
- Mao Q, Gong X, Zhou C, et al. Up-regulation of SIRT6 in the hippocampus induced rats with depression-like behavior via the block Akt/GSK3β signaling pathway. Behav Brain Res. 2017;323:38–46. doi:10.1016/j.bbr.2017.01.03528130175
- Iwata M, Ota KT, Duman RS. The inflammasome: pathways linking psychological stress, depression, and systemic illnesses. Brain Behav Immun. 2013;31:105–114. doi:10.1016/j.bbi.2012.12.00823261775
- Bernazzani O, Saucier J-F, David H, Borgeat F. Psychosocial predictors of depressive symptomatology level in postpartum women. J Affect Disord. 1997;46(1):39–49. doi:10.1016/S0165-0327(97)00077-39387085
- Da Costa D, Larouche J, Dritsa M, Brender W. Psychosocial correlates of prepartum and postpartum depressed mood. J Affect Disord. 2000;59(1):31–40. doi:10.1016/S0165-0327(99)00128-710814768
- English S, Steele A, Williams A, et al. Modelling of psychosocial and lifestyle predictors of peripartum depressive symptoms associated with distinct risk trajectories: a prospective cohort study. Sci Rep. 2018;8(1):12799. doi:10.1038/s41598-018-30874-z30143660
- Reid KM, Taylor MG. Social support, stress, and maternal postpartum depression: a comparison of supportive relationships. Soc Sci Res. 2015;54:246–262. doi:10.1016/j.ssresearch.2015.08.00926463547
- Caparros-Gonzalez RA, Romero-Gonzalez B, Strivens-Vilchez H, et al. Hair cortisol levels, psychological stress and psychopathological symptoms as predictors of postpartum depression. Slattery DA, ed. PLoS One. 2017;12(8):e0182817. doi:10.1371/journal.pone.0182817228846691
- Mahenge B, Stöckl H, Mizinduko M, Mazalale J, Jahn A. Adverse childhood experiences and intimate partner violence during pregnancy and their association to postpartum depression. J Affect Disord. 2018;229:159–163. doi:10.1016/j.jad.2017.12.03629310065
- Wang YY, Li H, Wang YJ, et al. Living with parents or with parents-in-law and postpartum depression: a preliminary investigation in China. J Affect Disord. 2017;218:335–338. doi:10.1016/j.jad.2017.04.05228494391
- Robertson E, Grace S, Wallington T, Stewart DE. Antenatal risk factors for postpartum depression: a synthesis of recent literature. Gen Hosp Psychiatry. 2004;26(4):289–295. doi:10.1016/j.genhosppsych.2004.02.00615234824
- Dalton VS, Kolshus E, McLoughlin DM. Epigenetics and depression: return of the repressed. J Affect Disord. 2014;155:1–12. doi:10.1016/j.jad.2013.10.02824238955