Abstract
Purpose
There is limited knowledge on the relationship between postnatal depression and childbirth pain characteristics associated with childbirth. We investigated whether the characteristics of childbirth pain, as assessed by Short-form-McGill Pain Questionnaire-2 (SF-MPQ-2), were associated with postnatal anxiety and depressive disorders.
Patients and Methods
Nulliparous parturients who received labor epidural analgesia (LEA) and delivered in our institution were invited to have a Mini-International Neuropsychiatric Interview (MINI) assessment following their 5–9 weeks post-delivery follow-up phone survey of a larger study. Parturients’ demographics, pre-delivery questionnaires on pain and psychological vulnerabilities, LEA data, maternal and neonatal outcomes, postnatal follow-up survey on pain and psychological vulnerabilities, pain and breastfeeding were collected accordingly. The primary outcome was the binary variable (yes/no) of the presence of postnatal depression and/or anxiety disorders based on the post-delivery MINI assessment.
Results
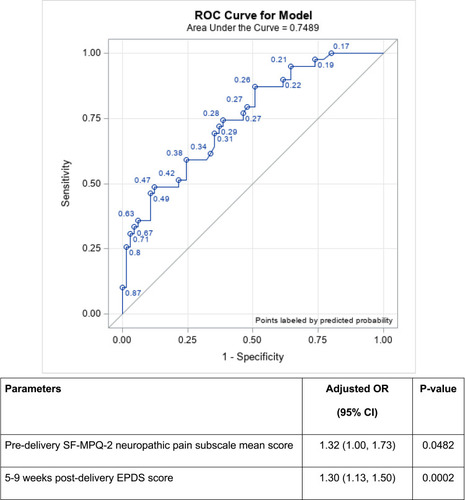
Among the 107 parturients who participated in the post-delivery MINI assessment, a total of 40 (42.5%) patients were found to have postnatal anxiety and depressive disorders. A greater pre-delivery SF-MPQ-2 neuropathic pain mean subscale score (adjusted odds ratio (OR) 1.32, 95% CI 1.00–1.73, p=0.0482) and greater post-delivery Edinburgh Postnatal Depression Scale (EPDS) at 5–9 weeks post-delivery (adjusted OR 1.30, 95% CI 1.13–1.50, p=0.0002) were independently associated with the presence of postnatal anxiety and/or depressive disorders (receiver operating characteristic (ROC) = 0.7489).
Conclusion
Patients with greater pre-delivery neuropathic pain and higher EPDS scores at 5–9 weeks post-delivery are more likely to have postnatal depression and/or anxiety disorders, suggesting possible associations between pain and psychological vulnerability in the development of postnatal mental disorders.
Introduction
Postnatal depression (PND) is associated with significant long-term psychological and socio-economic implications in mothers, their offspring, and families. The reported incidence of PND after childbirth may vary from 27% to 32% in the Asian population,Citation1–Citation4 and well-established risk factors of PND include but are not limited to pain severity, analgesic technique and psychological susceptibility during childbirth and delivery.Citation5–Citation7
Anxiety disorders are phenomenologically heterogeneous in nature, and these can be categorized into several groups predominantly characterized by: i) anxiety (generalized anxiety disorder (GAD)), ii) fear-related obsessional thoughts and behavioral compulsions (obsessive-compulsive disorder (OCD)), and iii) fear (phobias, panic disorder, etc.).Citation8 Similar to PND, postnatal anxiety may lead to detrimental maternal and neonatal outcomes; however, it has received less attention despite being a common co-morbidity with depression.Citation9 Postnatal anxiety has been associated with disengaged, negative and over-controlling maternal and parenting behaviors, highlighting the need to inform screening and treatment efforts.Citation9,Citation10
Neuropathic pain, as defined by the International Association for the Study of Pain (IASP), is “the pain caused by a lesion or dysfunctional nervous system”.Citation11 Neuropathic pain has been reported during the peripartum and postpartum periods, and could reduce functional status and health-related quality of life in pregnant women.Citation12 Interestingly, both depression and anxiety are well-known co-morbidities with neuropathic pain, especially in chronic pain patients. A recent animal study showed that neuropathic pain state may promote adaptations in gene expressions responsible for anxiety and depressive symptoms.Citation13 While pain elements, such as breakthrough pain during labor epidural analgesia (LEA) and acute pain after childbirth have been found to be significantly associated with increased Edinburgh Postnatal Depression Scale (EPDS) scores, there is limited knowledge on the association of specific childbirth pain characteristics on postnatal mental disorders.Citation7,Citation14
In this study, we investigated whether characteristics of childbirth pain, especially in the context of neuropathic pain, were associated with postnatal anxiety and depressive disorders. We also investigated the association of perinatal factors (demographic, pain, LEA, maternal and neonatal outcomes, psychological) with presence of postnatal anxiety and/or depressive disorders.
Patients and Methods
Patient Recruitment
This was a prospective cohort study from a secondary analysis of a randomized controlled trial that investigated the performance of different regimens for LEA maintenance. Approval was obtained from SingHealth Centralized Institutional Review Board (2014/670/D; 2018/3128) and registered at ClinicalTrials.gov (NCT02278601). Written informed consent was obtained prior to any study activity. This study adheres to the applicable Strengthening the Reporting of Observational studies in Epidemiology (STROBE) guidelines.
We recruited parturients in KK Women’s and Children’s Hospital, Singapore, between January 2015 and March 2019. We included nulliparous parturients aged 21–50 years old, ≥36 gestational weeks with singleton pregnancy, and in early labor (cervical dilation <5 cm) requesting LEA. Parturients with non-cephalic fetal presentation, obstetric complications and contraindications to LEA, received parenteral opioids within two hours prior to LEA initiation or suspected inadvertent dural puncture during LEA initiation, were excluded.
All LEA were performed following descriptions as stated in Zeng et al.Citation7 Once the patient received LEA and felt comfortable (ie not in pain or in distress), the following questionnaires (English or Chinese) were self-administered before delivery:
Short-form-McGill Pain Questionnaire-2 (SF-MPQ-2) is designed specifically and validated in the context of pain syndromes to differentiate different qualities of neuropathic and non-neuropathic pain in four subscales: continuous pain (throbbing pain, cramping pain, gnawing pain, aching pain, heavy pain, tender), intermittent pain (shooting pain, stabbing pain, splitting pain, electric-shock pain, piercing), neuropathic pain (hot-burning pain, cold-freezing pain, pain caused by light touch, itching, tingling or pins and needles, numbness), and affective descriptors (tiring-exhausting, sickening, fearful, punishing-cruel).Citation15 In this study, SF-MPQ-2 questionnaire was administered to measure pre-delivery neuropathic and non-neuropathic pain on an 11-point scale, with 0 being none and 10 being the worst possible intensity. The four subscale scores are calculated as the mean of items in each subscale, whereas the total score is the mean of all 22 items;
EPDS, a 10-item validated self-reported screening tool for antenatal/postnatal depression with a total score of 0–30. With a cut-off score of 10, this would encompass a range of probable postnatal depressive states;Citation16,Citation17
EuroQol-5-dimension-3-level (EQ-5D-3L), a widely used instrument to measure health-related quality of life;Citation18
Pain Catastrophizing Scale (PCS), a validated 13-item instrument to evaluate the processes of negative thoughts when encountering actual/anticipated pain or painful experiences. A cut-off score of 25 was used based on previous studies on intrapartum parturients;Citation7,Citation19
Cohen’s Perceived Stress Scale (PSS), a 10-item questionnaire to quantify the perception of stress. We used a cut-off score of 20 as suggested by previous studies, which illustrated good internal consistencies (Cronbach’s alpha 0.78–0.91);Citation20,Citation21
Spielberger’s State Trait Anxiety Inventory (STAI) that comprises 40 items to assess transient anxiety (state) during questionnaire administration, the dispositional anxiety (trait) and anxiety in general.Citation22 In this study, STAI and its subscales were measured as continuous variables as there are no reliable cut-off scores established thus far in the perinatal population.Citation23 Nevertheless, STAI is still considered the most robust and specific instrument to measure perinatal anxiety as compared with other anxiety measures.Citation23
Childbirth processes for all parturients were managed by a team of multidisciplinary staff including obstetricians, nurses and midwives, with each patient being in a single-room delivery suite in our institution. Parturients’ demographics (BMI, race, age, gravida, gestation, indirect morbidities, drug allergy), LEA data (pain scores-numerical rating scale (NRS) 0–10), number of LEA attempts, total time taken for LEA initiation, number of anesthetist(s), depth of space, loss of resistance, catheter in space, incidence of breakthrough pain, post-LEA complications, satisfaction with LEA), maternal and neonatal outcomes (use of oxytocin, labor onset, mode of delivery, duration of labor, infant body weight and length, infant sex and head circumference) were collected. Postnatal follow-up survey was conducted via phone by the study team members at 5–9 weeks post-delivery to administer questionnaires on EPDS, EQ-5D-3L, STAI, and questions pertaining to pain and breastfeeding.
MINI Assessment
During the 5–9 weeks post-delivery follow-up phone survey, women were invited to be interviewed by the study's research coordinator, who was trained and supervised by investigators (T Chua, H Chen) in the use of the Mini-International Neuropsychiatric Interview (MINI). The MINI is a brief, structured psychiatric interview developed to assess the most common psychiatric disorders as listed in the Diagnostic and Statistical Manual of Mental Disorders (DSM)-III-R, DSM-IV, DSM-5, and International Classification of Diseases-10th revision (ICD-10).Citation24 Based on the diagnostic categories, the MINI may be divided into modules for further assessment, of which five modules were used in the present study: major/minor depressive disorder, GAD, panic disorder, agoraphobia, and OCD to encompass the possible co-morbidity of both depression and anxiety in postpartum women.
Statistical Analysis
The study's goal was to understand the childbirth pain experience of women with defined clinical postnatal depression and/or anxiety disorders, rather than general measures of depressive symptoms. Hence, the primary outcome was defined as the presence of postnatal depression and/or anxiety disorders based on the post-delivery MINI assessment (including any anxiety disorders in GAD, depressive disorders that affected daily life activities, lifetime panic disorder, obsession/compulsions, and/or current agoraphobia) and was treated as binary data with status “yes” or “no”. The primary objective was to evaluate the association between pre-delivery neuropathic pain, as measured by the mean of six items in SF-MPQ-2 neuropathic subscale, and the presence of postnatal anxiety and/or depressive disorders.
The continuous and categorical variables were summarized as mean ± standard deviation (SD), median [interquartile range (IQR)] or frequency (proportion) where appropriate. Univariate and multivariable logistic regression analyses were performed to find association between postnatal anxiety and/or depressive disorders and independent variables. Quantitative association from logistic regression was expressed as odds ratio (OR) with corresponding 95% confidence interval (95% CI). Variables, with P < 0.10 in the univariate logistic regression were chosen for the multivariable model, and a stepwise variable selection method was used to finalize the multivariable model. Area under the curve (AUC) from receiver-operating characteristics (ROC) based on the final multivariable model was reported to check the robustness and predictive ability of the model. All tests were two-sided, with P < 0.05 considered as statistically significant. SAS software (version 9.4, SAS Institute; North Carolina, USA) was used for all analyses.
Results
One hundred and seven women were invited to participate in the MINI assessment that took place after the 5–9 weeks post-delivery phone follow-up (median [IQR] duration between post-delivery follow-up and MINI: 23 [24] days) with no drop-out. There were 67 (57.5%) without and 40 (42.5%) patients with postnatal anxiety and depressive disorders (). The study cohort had a mean age of 29.5 ± 4.3 years old (age range: 21 to 43 years old), a mean BMI of 27.9 ± 4.7 kg/m2, and a mean gestation of 37.6 ± 1.8 weeks. There were no significant differences in demographic characteristics (), LEA data () nor maternal and neonatal outcomes () between those with and without postnatal anxiety and/or depressive disorders. We also found no significant univariate association (P < 0.05) in the SF-MPQ-2 subscales and postnatal anxiety and/or depressive disorders (). A separate analysis on SF-MPQ-2 subscales showed that they had no significant associations with postnatal anxiety and postnatal depressive disorders, respectively (Supplementary Table 1).
Figure 1 Study flowchart.
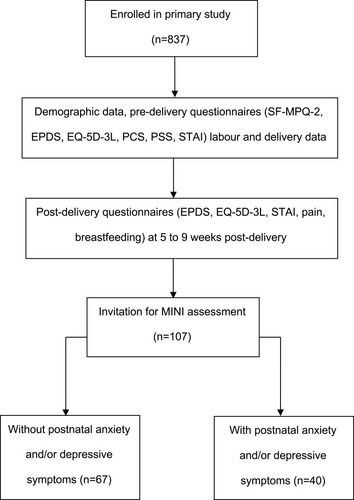
Table 1 Demographic Characteristics in Patients with or without Postnatal Anxiety and/or Depressive Disorders
Table 2 Pain Characteristics in Patients with or without Postnatal Anxiety and/or Depressive Disorders
Table 3 Maternal and Neonatal Characteristics in Patients with or without Postnatal Anxiety and/or Depressive Disorders
On univariate analysis, pre-delivery EPDS score was greater in those with postnatal anxiety and/or depressive disorders (7.6 ± 3.8) as compared with those without (5.8 ± 3.7; OR 1.13, 95% CI 1.02–1.26, p=0.0223) (). A pre-delivery PSS score of ≥20 was found to be associated with presence of postnatal anxiety and/or depressive disorders (OR 2.74, 95% CI 1.07–7.05, p=0.0359). At 5–9 weeks post-delivery follow-up phone survey, all measured psychological characteristics were significantly associated with postnatal anxiety and/or depressive disorders: EPDS (OR 1.29, 95% CI 1.13–1.48, p=0.0003), EQ-5D-3L health status (OR 0.92, 95% CI 0.87–0.97, p=0.0038), and STAI state anxiety (OR 1.08, 95% CI 1.03–1.13, p=0.0020) ().
Table 4 Psychological Characteristics in Patients with or without Postnatal Anxiety and/or Depressive Disorders
Follow-up survey at 5–9 weeks post-delivery demonstrated that mood affected by post-delivery pain (OR 2.93, 95% CI 1.17–7.33, p=0.0214) () and unsatisfactory delivery experience (OR 5.76, 95% CI 1.07–31.01, p=0.0414) () was significantly associated with presence of postnatal anxiety and/or depressive disorders. There were no significant associations found of breastfeeding with postnatal anxiety and/or depressive disorders ().
A greater pre-delivery SF-MPQ-2 neuropathic pain mean subscale score (adjusted OR 1.32, 95% CI 1.00–1.73, p=0.0482) and greater post-delivery EPDS at 5–9 weeks post-delivery (adjusted OR 1.30, 95% CI 1.13–1.50, p=0.0002) were independently associated with the presence of postnatal anxiety and/or depressive disorders (). The AUC of ROC based on the multivariable analysis was 0.7489.
Discussion
Women with greater pre-delivery neuropathic pain, as determined by the neuropathic subscale of SF-MPQ-2, and higher EPDS scores at 5–9 weeks post-delivery were more likely to have postnatal anxiety and/or depressive disorders categorized as major/minor depressive disorder, GAD, panic disorder, agoraphobia, and OCD as listed in the MINI assessment.
Neuropathic pain complaints, such as carpal tunnel syndrome, meralgia paresthetica, and scar pain associated with previous cesarean delivery, are associated with pregnancy.Citation25 During labor, neuropathic pain may arise from direct pressure on the lumbosacral plexus, which is left exposed to the pelvic area, and the pain may usually be resolved after the childbirth process.Citation25 Previous studies have suggested an association between the intensity of labor pain and PND development;Citation26,Citation27 a prospective observational study in 72 women showed that increased pain at each perinatal time point (pre-delivery, labor, post-delivery) was independently associated with increased EPDS scores at 6 weeks after delivery. However, whether the pain syndrome is of neuropathic nature is unknown.Citation27 The SF-MPQ-2 was used in Cesarean delivery to evaluate for post-delivery chronic neuropathic pain; however, there is limited information on its use in those undergoing labor process.Citation28 We demonstrated that pre-delivery neuropathic pain, as measured by SF-MPQ-2, was associated with postnatal anxiety and/or depressive disorders. To our knowledge, this association is relatively unexplored and suggests that a closer look based on pathophysiology of pain characteristics may be important, particularly in relation to postnatal mental health status.
While EPDS was previously validated as a screening tool for depression and anxiety with regard to MINI assessment, EPDS has demonstrated high sensitivity (82–84%) for detecting MINI mental disorders.Citation29 While it is possible to use EPDS as a preliminary screening tool in busy maternal-fetal units, further psychiatric assessment via DSM-5, the gold standard for diagnosing PND, is recommended. Our previous study showed that EPDS may yield false positives and has low positive predictive value (PPV) for both major and any depression (23.68% and 36.84%, respectively) in high-risk pregnancies, and this suggests that the clinical use of the EPDS is more suitable for screening, than being used as a confirmatory tool.Citation29 Hence, EPDS should retain its clinical utility as a screener to identify women requiring further assessment. In the absence of clinical diagnostic assessment, a structured DSM-5 interview, such as the MINI, can help to further assess the specific diagnostic conditions in those having elevated EPDS scores.Citation29
Rosseland et al demonstrated that negative birth experience was significantly associated with PND at 8 weeks post-delivery.Citation30 Conversely, previous study compared the incidence of PND among those who received LEA, and found that there was no difference in the PND rate between those who were satisfied with LEA and those among women who were not satisfied with LEA.Citation31 This is in line with our findings where a significant association was found between overall delivery experience and postnatal anxiety/depressive disorders, but not LEA satisfaction, suggesting that there could be potential confounders other than childbirth pain and treatment for childbirth pain that may affect the maternal outcomes.
Increased stress during labor is known to have adverse maternal consequences, including prolonged labor, reduced uterine contractions, and delayed wound healing.Citation32 In the postpartum setting, Razurel et al showed a significant positive correlation between perceived stress and postnatal anxiety and depressive symptoms. However, we found that pre-delivery PSS≥20 was a significant univariate factor but not an independent risk factor in the multivariable model.Citation33 This may be attributed to the use of different questionnaire (Antenatal Perceived Stress Inventory (APSI)), smaller sample size in our study, or the utilization of a different cut-off that may differ in different cultural and obstetric practice context.Citation33 Similarly, Grant et al demonstrated that an increase in both pre-delivery (37 gestational weeks) and 32 weeks post-delivery STAI trait anxiety was associated with postnatal depressive and anxiety disorders, but not pre-delivery state anxiety.Citation34 In this study, however, we did not find a significant association between pre-delivery anxiety and postnatal mental disorders, and only STAI state anxiety was significant with postnatal depression/anxiety disorders at 5–9 weeks post-delivery period. The differing findings could be related to different patient demographics and different time-point on follow-up, but possibly due to this study recruiting women who all received LEA. To date, there are only a few anxiety-related instruments (eg, Pregnancy-related Anxiety Scale (PAS), Perinatal Anxiety Screening Scale (PASS)) specifically designed for pregnant population and one for postnatal anxiety (Postpartum Specific Anxiety Scale (PSAS)). Hence, further validation is required for the clinical relevance of these instruments.Citation35–Citation37
There were several limitations in this study. First, the inclusion criteria on nulliparous Asian parturients may result in different perceptions and psychological characteristics, which may not be generalized to other obstetric populations. Secondly, we recruited only parturients who requested LEA, and hence would not be able to provide generalized data for those who did not opt for LEA. The intended study design, however, allowed a more homogenous cohort to reduce potential confounding factors and evaluate independent risk factors. Thirdly, we recruited only English and/or Chinese-speaking patients for the questionnaire administration; language and cultural differences may influence the findings. Factors such as education, income, occupation, social/partner support, motherhood transition, and pain history that were previously associated with postnatal depression/anxiety disorders were also not taken into account.Citation9,Citation38,Citation39 Fourthly, anxiety and depression often co-exist in postpartum women, as unpredictable challenges are associated with anxiety, and difficulties with coping are associated with depressive symptoms. We were unable to examine the potential reverse causality between anxiety and depression as there were only two time points of measure. The sample size was limited and not able to control for the impact of depression on anxiety and vice versa. Finally, we only included a few types of anxiety (GAD, panic disorder, agoraphobia) disorders during the MINI assessment since they are more prevalent in pregnant patients. Future studies may include investigating other types of mental disorders, eg, post-traumatic stress disorder for more comprehensive analyses.
Conclusion
Women with greater pre-delivery neuropathic pain and higher EPDS scores at 5–9 weeks post-delivery were associated with an increased risk of postnatal depression/anxiety disorders. This suggests that pain and psychological vulnerability are important factors associated with postnatal mood disorders. Future studies to validate the above findings are needed to confirm the suggested model and refine the role of neuropathic pain in childbirth, so that risk stratification and early interventions can be instituted to reduce maternal postnatal depression and anxiety.
Abbreviations
APSI, Antenatal Perceived Stress Inventory; AUC, area under the curve; BMI, body mass index; CI, confidence interval; EPDS, Edinburgh Postnatal Depression Scale; EQ-5D-3L, EuroQol-5-dimension-3-level; GAD, Generalized anxiety disorder; IASP, International Association for the Study of Pain; LEA, labor epidural analgesia; OCD, obsessive-compulsive disorder; OR, odds ratio; MINI, Mini-International Neuropsychiatric Interview; NRS, numerical rating scale; PAS, Pregnancy-related Anxiety Scale; PASS, Perinatal Anxiety Screening Scale; PCS, Pain Catastrophizing Scale; PND, postnatal depression; PPV, positive predictive value; PSAS, Postpartum Specific Anxiety Scale; PSS, Perceived Stress Scale; ROC, receiver operating characteristic; SD, standard deviation; SF-MPQ-2, Short-form-McGill Pain Questionnaire-2; STAI, Spielberger’s State Trait Anxiety Inventory; STROBE, Strengthening the Reporting of Observational studies in Epidemiology.
Data Sharing Statement
The datasets generated and analyzed in this work are available for anyone who wishes to access the data by contacting the corresponding author.
Ethics Approval and Informed Consent
The study was approved by the SingHealth Centralized Institutional Review Board, Singapore (SingHealth CIRB Ref: 2014/670/D and 2018/3128) and registered on Clinicaltrials.gov (NCT02278601) on 26 Oct 2014. The authors declare that all the recruited patients provided informed consent, and that this work was conducted in accordance with the Declaration of Helsinki.
Consent for Publication
All patients provided informed consent on the use of their de-identified data for publication purpose.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval for the version to be published; and agreed to be accountable for all aspects of the work.
Acknowledgments
We would like to thank Ms. Agnes Teo (Senior Clinical Research Coordinator), Yvonne Yong (Senior Clinical Research Coordinator), Denise Anne (Clinical Research Coordinator) and Beverly Chia (Research Coordinator) for their administrative support in this work.
Disclosure
All authors report no conflicts of interest in this work.
Additional information
Funding
References
- GiriRK, KhatriRB, MishraSR, KhanalV, SharmaVD, GartoulaRP. Prevalence and factors associated with depressive symptoms among post-partum mothers in Nepal. BMC Res Notes. 2015;8(1):1–7. doi:10.1186/s13104-015-1074-325645429
- DengAW, XiongRB, JiangTT, LuoYP, ChenWZ. Prevalence and risk factors of postpartum depression in a population-based sample of women in Tangxia Community, Guangzhou. Asian Pac J Trop Med. 2014;7(3):244–249. doi:10.1016/S1995-7645(14)60030-424507649
- LauY, WongDF, ChanKS. The utility of screening for perinatal depression in the second trimester among Chinese: a Three-Wave Prospective Longitudinal Study. Arch Womens Ment Health. 2010;13(2):153–164. doi:10.1007/s00737-009-0134-x20058040
- Alfayumi-ZeadnaS, Kaufman-ShriquiV, ZeadnaA, LaudenA, Shoham-VardiI. The association between sociodemographic characteristics and postpartum depression symptoms among Arab-Bedouin women in Southern Israel. Depress Anxiety. 2015;32(2):120–128. doi:10.1002/da.2229025044129
- HalbreichU. Postpartum Disorders: Multiple Interacting Underlying Mechanisms and Risk Factors. 2005.
- TanCW, SultanaR, KeeMZ, MeaneyMJ, SngBL. Investigating the association between labour epidural analgesia and postpartum depression: a Prospective Cohort Study. Eur J Anaesthesiol. 2020;37(9):796–802. doi:10.1097/EJA.000000000000123632453169
- ZengY, TanCW, SultanaR, et al. Association of pain catastrophizing with postnatal depressive states in nulliparous parturients: a Prospective Study. Neuropsychiatr Dis Treat. 2020;16:1853–1862. doi:10.2147/NDT.S25646532982241
- VahabzadehA, GillespieCF, ResslerKJ. Fear-related anxiety disorders and post-traumatic stress disorder. Neurobiol Brain Disord. 2015;612–620.
- Falah-HassaniK, ShiriR, DennisCL. Prevalence and risk factors for comorbid postpartum depressive symptomatology and anxiety. J Affect Disord. 2016;198:142–147. doi:10.1016/j.jad.2016.03.01027016657
- DennisCL, Falah-HassaniK, ShiriR. Prevalence of antenatal and postnatal anxiety: systematic review and meta-analysis. Br J Psychiatr. 2017;210(5):315–323. doi:10.1192/bjp.bp.116.187179
- JensenTS, BaronR, HaanpääM, et al. A new definition of neuropathic pain. Pain. 2011;152(10):2204–2205. doi:10.1016/j.pain.2011.06.01721764514
- EserF, NebioğluS, AliyevaA, et al. Neuropathic pain in pregnant Turkish women with lumbopelvic pain and its impact on health-related quality of life. Eur J Rheumatol. 2018;5(1):37. doi:10.5152/eurjrheum.2017.1608829657873
- DescalziG, MitsiV, PurushothamanI, et al. Neuropathic pain promotes adaptive changes in gene expression in brain networks involved in stress and depression. Sci Signal. 2017;10(471):eaaj1549. doi:10.1126/scisignal.aaj154928325815
- EisenachJC, PanPH, SmileyR, Lavand’hommeP, LandauR, HouleTT. Severity of acute pain after childbirth, but not type of delivery, predicts persistent pain and postpartum depression. Pain. 2008;140(1):87–94. doi:10.1016/j.pain.2008.07.01118818022
- DworkinRH, TurkDC, RevickiDA, et al. Development and initial validation of an expanded and revised version of the short-form McGill Pain Questionnaire (SF-MPQ-2). Pain. 2009;144(1–2):35–42. doi:10.1016/j.pain.2009.02.00719356853
- ChenH, WangJ, Ch’ngYC, MingooR, LeeT, OngJ. Identifying mothers with postpartum depression early: integrating perinatal mental health care into the obstetric setting. ISRN Obstet Gynecol. 2011;2011:1–7. doi:10.5402/2011/309189
- CoxJL, HoldenJM, SagovskyR. Detection of postnatal depression: development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatr. 1987;150(6):782–786. doi:10.1192/bjp.150.6.782
- BrooksR, GroupE. EuroQol: the current state of play. Health Policy (New York). 1996;37(1):53–72. doi:10.1016/0168-8510(96)00822-6
- FerberSG, GranotM, ZimmerEZ. Catastrophizing labor pain compromises later maternity adjustments. Am J Obstet Gynecol. 2005;192(3):826–831. doi:10.1016/j.ajog.2004.10.58915746678
- CohenS, Janicki‐DevertsDE. Who’s stressed? Distributions of psychological stress in the United States in probability samples from 1983, 2006, and 2009. J Appl Soc Psychol. 2012;42(6):1320–1334. doi:10.1111/j.1559-1816.2012.00900.x
- GhoshJK, WilhelmMH, Dunkel-SchetterC, LombardiCA, RitzBR. Paternal support and preterm birth, and the moderation of effects of chronic stress: a study in Los Angeles County mothers. Arch Womens Ment Health. 2010;13(4):327–338. doi:10.1007/s00737-009-0135-920066551
- GunningM, DenisonFC, StockleyCJ, HoSP, SandhuHK, ReynoldsRM. Assessing maternal anxiety in pregnancy with the State‐Trait Anxiety Inventory (STAI): issues of validity, location and participation. J Reprod Infant Psychol. 2010;28(3):266–273. doi:10.1080/02646830903487300
- MeadesR, AyersS. Anxiety measures validated in perinatal populations: a systematic review. J Affect Disord. 2011;133(1–2):1–5. doi:10.1016/j.jad.2010.10.00921078523
- SheehanDV, LecrubierY, SheehanKH, et al. The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatr. 1998;59(20):22–33.
- RosierC, CamdessanchéJP. Neuropathy and pregnancy: an overview. Rev Neurol (Paris). 2020;177(3):220–4.32653214
- LimG, FarrellLM, FaccoFL, GoldMS, WasanAD. Labor analgesia as a predictor for reduced postpartum depression scores: a Retrospective Observational Study. Anesth Analg. 2018;126(5):1598. doi:10.1213/ANE.000000000000272029239949
- LimG, LaSordaKR, FarrellLM, McCarthyAM, FaccoF, WasanAD. Obstetric pain correlates with postpartum depression symptoms: a Pilot Prospective Observational Study. BMC Pregnancy Childbirth. 2020;20(1):1–4. doi:10.1186/s12884-020-02943-7
- OrtnerCM, TurkDC, TheodoreBR, SiaulysMM, BollagLA, LandauR. The short-form-McGill pain questionnaire-revised to evaluate persistent pain and surgery-related symptoms in healthy women undergoing a planned cesarean delivery. Reg Anesth Pain Med. 2014;39(6):478–486. doi:10.1097/AAP.000000000000015825304476
- ThiagaysonP, KrishnaswamyG, LimML, et al. Depression and anxiety in Singaporean high-risk pregnancies—prevalence and screening. Gen Hosp Psychiatry. 2013;35(2):112–116. doi:10.1016/j.genhosppsych.2012.11.00623265951
- RosselandLA, RemeSE, SimonsenTB, ThoresenM, NielsenCS, GranME. Are labor pain and birth experience associated with persistent pain and postpartum depression? A Prospective Cohort Study. Scand J Pain. 2020;20(3):591–602. doi:10.1515/sjpain-2020-002532469334
- Orbach-ZingerS, LandauR, HarouschAB, et al. The relationship between women’s intention to request a labor epidural analgesia, actually delivering with labor epidural analgesia, and postpartum depression at 6 weeks: a Prospective Observational Study. Anesth Analg. 2018;126(5):1590–1597. doi:10.1213/ANE.000000000000250128930940
- AlehaganS, WijmaB, LundberU, MelinB, WijmaB. Caecholamine and cortisol reaction to childbirth. Int J Behav Med. 2001;8(1):50–65. doi:10.1207/S15327558IJBM0801_04
- RazurelC, KaiserB, AntoniettiJP, EpineyM, SellenetC. Relationship between perceived perinatal stress and depressive symptoms, anxiety, and parental self-efficacy in primiparous mothers and the role of social support. Women Health. 2017;57(2):154–172. doi:10.1080/03630242.2016.115712526909523
- GrantKA, McMahonC, AustinMP. Maternal anxiety during the transition to parenthood: a Prospective Study. J Affect Disord. 2008;108(1–2):101–111. doi:10.1016/j.jad.2007.10.00218001841
- BruntonRJ, DryerR, SalibaA, KohlhoffJ. The initial development of the pregnancy-related anxiety scale. Women Birth. 2019;32(1):e118–30. doi:10.1016/j.wombi.2018.05.00429859678
- SomervilleS, DedmanK, HaganR, et al. The perinatal anxiety screening scale: development and preliminary validation. Arch Womens Ment Health. 2014;17(5):443–454. doi:10.1007/s00737-014-0425-824699796
- SilverioSA, DaviesSM, ChristiansenP, et al. A validation of the postpartum specific anxiety scale 12-item research short-form for use during global crises with five translations. BMC Pregnancy Childbirth. 2021;21(1):1–2. doi:10.1186/s12884-021-03597-933388035
- FieldT. Postnatal anxiety prevalence, predictors and effects on development: a narrative review. Infant Behav Dev. 2018;51:24–32. doi:10.1016/j.infbeh.2018.02.00529544195
- GhaedrahmatiM, KazemiA, KheirabadiG, EbrahimiA, BahramiM. Postpartum depression risk factors: a narrative review. J Educ Health Promot. 2017;6:60.28852652