Abstract
Neuroleptic malignant syndrome is an uncommon but dangerous complication of antipsychotic drugs, characterized by clinical symptoms that include hyperthermia, severe muscle rigidity, autonomic dysfunction, and altered mental state. Serum creatine kinase (CK) elevation occurs in over 90% of cases. Many diagnostic criteria sets for neuroleptic malignant syndrome have been proposed, all of which include hyperthermia and muscle rigidity as major symptoms, and serum CK elevation as either a major or minor symptom. In general, elevated CK occurs in the initial stage of neuroleptic malignant syndrome and corresponds temporally with the onset of muscle rigidity. However, in some exceptional cases, CK elevation and emergence of muscle rigidity do not appear in the same stage, making early diagnosis of neuroleptic malignant syndrome more difficult. Two rare cases of neuroleptic malignant syndrome are presented in which elevated serum CK and emergence of muscle rigidity did not occur in the same stage of neuroleptic malignant syndrome. An elevated CK level is common in the early stage of neuroleptic malignant syndrome, suggesting that serum CK elevation is a useful indicator for early detection of neuroleptic malignant syndrome. However, a definitive diagnosis of neuroleptic malignant syndrome must be determined from the presence of specific clinical symptoms.
Introduction
Neuroleptic malignant syndrome (NMS) is a serious adverse reaction to antipsychotic drugs. The syndrome is characterized by four main symptoms, ie, hyperthermia, extreme muscle rigidity, autonomic instability, and mental status changes. The first diagnostic criteria proposed for NMS by Levenson in 1985Citation1 included major criteria (fever, rigidity, and elevated creatine kinase [CK] level) and minor criteria (tachycardia, abnormal blood pressure, tachypnea, altered level of consciousness, diaphoresis, and leukocytosis). Diagnosis using this criteria set rests on the presence of all three major criteria or two major criteria and four minor criteria.
Other diagnostic standards for NMS have since been proposed,Citation2–Citation4 and all include hyperthermia and muscle rigidity as major symptoms and elevated serum CK as a minor symptom. Serum CK elevation is not specific to NMS,Citation5 but is reported to be found in over 90% of patients with NMS.Citation3,Citation6 Therefore, an elevated CK level is suggestive of NMS. In addition, follow-up of the CK level has been reported to be helpful in establishing the rate of amelioration of NMS.Citation7
Although the literature contains numerous case reports on NMS, there have been no detailed studies of the relationship between level of serum CK and degree of muscle rigidity following onset of NMS. Rosebush and StewartCitation8 reported that the CK level peaked on days 2 and 3 after onset in 64% of 24 consecutive cases, and Velamoor et alCitation9 pointed out muscle rigidity and mental status changes as the initial manifestations in 82.3% of 222 previously reported cases. The findings of these two studies suggest that an increased serum CK level and muscle rigidity both occur in the early stage of NMS.
We report here two cases in which muscle rigidity did not emerge with elevated CK in the early stage of NMS, but rather emerged after the serum CK level had been normalized mid stage. These cases suggest that serum CK elevation does not necessarily parallel the degree of muscle rigidity in patients with NMS. In such cases, diagnosis of NMS may be delayed or the severity of NMS may be incorrectly evaluated.
Case report 1
A 32-year-old man who had been suffering from schizophrenia for 2 years was admitted to the hospital for worsening of his mental condition, including psychomotor agitation, auditory hallucinations, and sleeplessness. On admission, he was prescribed chlorpromazine 100 mg/day. On hospital day 10, the dose of chlorpromazine was increased to 150 mg and haloperidol 9 mg/day was added because the excitation had not improved. On hospital day 13, chlorpromazine 50 mg was given intramuscularly to alleviate the excitation. The patient was drowsy throughout hospital day 14, and his body temperature increased to 39.7°C and heart rate to 120 beats per minute on hospital day 15 (day 1 of NMS). The results of blood tests on hospital day 16 revealed an elevated serum CK of 540 (normal range 46–210) IU/L and a high white blood count of 11,500/mm3. Brain computed tomography, a cerebrospinal fluid study, and a thyroid function test revealed no abnormalities. No obvious infection was detected. Therefore, NMS was suspected. However, because muscle rigidity was not found, neuroleptics were continued. On hospital day 17, serum CK was increased to 722 IU/L. The patient continued to be restless and began to cry in a loud voice. Administration of an intravenous bolus of haloperidol 10 mg was started on hospital day 21. On hospital day 23, the patient was unresponsive, but intravenous administration of haloperidol was continued because serum CK had normalized to 143 IU/L. Generalized muscular rigidity was noted on hospital day 24 (day 10 of NMS).
Symptoms of autonomic disturbance started to appear (mydriasis, generalized perspiration, and diarrhea), and NMS was finally diagnosed on hospital day 26. Intravenous injections of haloperidol were stopped, and fluid replacement and dantrolene 100 mg/day were started. Serum CK remained in the normal range (79 IU/L). On hospital day 27, serum CK was measured again and was still in the normal range (83 IU/L). On hospital day 29, the akinetic mutism was improved, and on hospital day 32, fever, muscular rigidity, diaphoresis, and diarrhea were no longer present, and it was judged that the patient no longer had NMS (day 20 from onset of symptoms).
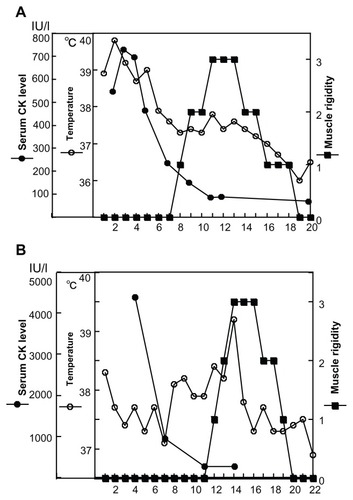
To monitor changes in muscle rigidity and serum CK values more accurately, the NMS evaluation scale proposed by SachdevCitation10 was used. Muscle rigidity was rated as follows: 0, nil (no rigidity); 1, mild (slight rigidity present, particularly obvious on recruitment of muscles with jaw clenching); 2, moderate (definitely present to a significant degree but produces no limitation of passive movement); or 3, severe (rigidity that produces some limitation of passive movement). The changes in these values during the course of NMS were monitored, and changes in serum CK levels and body temperature were also assessed. These data are shown in .
Case report 2
A 29-year-old woman with mild mental retardation and bipolar disorder was admitted to the hospital for emotional instability and dysthymia. She engaged in acts of self-mutilation, such as attempting to cut her hand with a knife. Her mood was unstable for the 6 months following admission. Paliperidone 6 mg/day, chlorpromazine 150 mg/day, and carbamazepine 300 mg/day were prescribed. Eight months later, the dysthymia had stabilized and the patient was scheduled for discharge. However, around hospital day 240, the patient lost vigor and lay in bed most of the time. On hospital 247, fever (body temperature, 38.3°C) was noted (day 1 of NMS) and this fever of unknown origin (body temperature approximately 37.5°C) persisted. On hospital day 250, serum CK was 4273 (normal range 46–210) IU/L and white cell count was 6400/mm3. Results of other laboratory tests and brain imaging were normal. There was no sign of muscular rigidity or dysphagia, but extreme diaphoresis appeared. Based on the CK level, NMS was suspected. All antipsychotics were stopped, and fluid replacement and dantrolene 75 mg/day were started.
On hospital day 253, the serum CK value was 841 IU/L. In the evening of the same day, the patient became nauseous and vomited. Because the physician in charge was not present, a resident administered metoclopramide 10 mg intravenously (day 7 of NMS). On hospital day 254, her body temperature was 38.1°C and tremor was noted in both upper limbs. In addition, the patient was almost mute. However, muscle rigidity was not observed. Serum CK normalized to 154 IU/L on hospital day 257, and dantrolene was stopped on hospital days 258 and 259 when it was judged that the NMS had improved. On hospital day 260, although her serum CK value was 160 IU/L, her white cell count was high at 13,100/mm3 and body temperature was 39.2°C. In addition, tremor and muscle rigidity was noted in all four limbs. Although serum CK was normal, it was judged that the NMS had not yet improved because full-blown NMS symptoms were evident. Dantrolene was restarted and from hospital day 264 onwards, the patient showed signs of responsiveness, such as opening her eyes when called. On hospital day 268 (day 22 of NMS), the muscle rigidity, dysphagia, tremor, and diaphoresis disappeared, and her body temperature decreased to 36°C. Changes in muscle rigidity, serum CK level, and body temperature are shown in .
Discussion
Typical neuroleptics, ie, chlorpromazine and haloperidol, were administered in case 1, and the patient presented with fever (body temperature > 38°C) and elevated serum CK levels. A typical neuroleptic and an atypical neuroleptic, ie, chlorpromazine and paliperidone, respectively, were administered in case 2 and the patient presented with fever (body temperature > 38°C) and elevated serum CK. These two drugs appear to have been the cause of NMS in case 2. However, the patient was also treated with metoclopramide (on day 7 of NMS) for nausea and vomiting. Although metoclopramide is an antiemetic, it also has anti-dopamine D2 receptor effects and reports of metoclopramide-induced NMS have appeared in the literature.Citation11 Therefore, metoclopramide may have caused the NMS in case 2.
In both cases, the four major clinical symptoms of NMS and elevated serum CK were present in the initial or middle stage of the illness and therefore diagnosis of NMS was not so difficult. However, the unusual timing of the characteristic symptoms did present some difficulties. The most characteristic feature of NMS was the increase in serum CK in the initial stage. However, muscle rigidity was not seen at that time, and appeared only after CK levels had decreased to the normal range. Serum CK values usually peak on day 2 to 3 of NMS as they did in both cases, but the muscle rigidity and mental status changes that are often found in the initial stage of NMS were not apparent. Védie et alCitation12 pointed out that CK elevation occurs very early and corresponds temporally with the onset of rigidity, and while HarschCitation13 reported that CK elevation and fever did not necessarily parallel the duration or degree of muscle rigidity in nine cases of NMS, he did not observe an inverse relationship between elevated CK level and the appearance of rigidity.
Given these findings, the nonsimultaneous occurrence of muscle rigidity and elevated serum CK levels observed in the present cases appears to be a rare finding. In case 1, fever and elevated serum CK were evident in the initial stage of NMS, but there was no muscle rigidity, which delayed the diagnosis of NMS. In case 2, NMS was suspected in the early stage when fever and elevated CK were found, but serum CK normalized as expected over the course of the illness, leading to the conclusion that the NMS had improved when it had not, and dantrolene administration was stopped for 2 days.
Serum CK elevation is not specific to NMS. However, it occurs in up to 90% of NMS casesCitation6 and is found at a high rate in the initial stage of NMS.Citation8 Therefore, if an increase in serum CK is found along with fever of unknown origin during the administration of neuroleptics, physicians should suspect NMS. In this respect, serum CK elevation may be a useful indicator for early detection of NMS. However, this elevation of accompanying fever is not sufficient for a definite diagnosis of NMS, which should be determined from the presence of other clinical symptoms, such as muscle rigidity, autonomic disturbance, and mental status changes. Physicians should be cognizant that muscle rigidity may appear after the serum CK level normalizes, as occurred in the present cases.
It is unclear why muscle rigidity appeared after the serum CK levels normalized in the present cases. This phenomenon indicates that the elevated CK levels are not due to muscle rigidity. It is also unclear how many patients with NMS show nonsimultaneous occurrence of CK elevation and muscle rigidity. Further studies are needed on the relationship between CK and degree of muscle rigidity during the course of NMS.
Conclusion
In general, it appears that both serum CK levels and muscle rigidity increase in the early stage of NMS, but there are exceptional cases, like those described here, where the elevated serum CK level and emergence of muscle rigidity do not appear in the same stage. In such cases, the diagnosis of NMS may be difficult and consequently the treatment may be delayed. While these NMS cases may be rare, physicians should keep in mind the possibility of exceptional NMS cases.
Disclosure
The author reports no conflicts of interest in this work.
References
- LevensonJLNeuroleptic malignant syndromeAm J Psychiatry1985142113711452863986
- PopeHGKeckPEMcElroySIFrequency and presentation of neuroleptic malignant syndrome in a large psychiatric hospitalAm J Psychiatry1986143122712332876647
- CaroffSNMannSCNeuroleptic malignant syndromeMed Clin North Am1993771852028093494
- American Psychiatric AssociationMedication-induced movement disorders: neuroleptic malignant syndromeDiagnostic and Statistical Manual of Mental Disorders: DSM-IV-TRWashington, DCAmerican Psychiatric Association2000
- O’DwyerAMSheppardNPThe role of creatine kinase in the diagnosis of neuroleptic malignant syndromePsychol Med1993233233268101383
- AddonizioGSusmanVLRothDSNeuroleptic malignant syndrome: review and analysis of 115 casesBiol Psychiatry198722100410202886157
- PeloneroAILevensonJLPandurangiAKNeuroleptic malignant syndrome: a reviewPsychiatr Serv199849116311729735957
- RosebushPStewartTA prospective analysis of 24 episodes of neuroleptic malignant syndromeAm J Psychiatry19891467177252567121
- VelamoorVRNormanRMGCaroffSNMannSCSullivanKAAnteloREProgression of symptoms in neuroleptic malignant syndromeJ Nerv Ment Dis19941821681737906709
- SachdevPSA rating scale for neuroleptic malignant syndromePsychiatry Res200513524925615996751
- SuparivalaAKantGJeanRENeuroleptic malignant syndrome with metoclopramide overdose coexisting with Clostridium difficile diarrheaIntensive Care Med2011371706170821688103
- VédieCPoinsoFHemmiFRivetBMajor symptoms and differential diagnosis of neuroleptic malignant syndrome: three case reportsEur Psychiatry20001533433710954878
- HarschHHNeuroleptic malignant syndrome: physiological and laboratory findings in a series of nine casesJ Clin Psychiatry1987483283332886491