Abstract
Background
Post-stroke depression (PSD) can aggravate the mortality and recurrence rate in stroke patients. The relationship between family functioning and PSD at different phases after a first-ever stroke is unclear. The purpose of this longitudinal study was to investigate the patterns and relationship of family functioning and PSD at acute hospitalization and 6 months post-discharge in first-ever stroke survivors.
Methods
This is a longitudinal study conducted in Guangzhou, China. Family functioning and depression were measured by the Short Form Family Assessment Device (SF-FAD) and Self-Rating Depression Scale (SDS) at baseline and 6 months post-discharge. Multiple linear regression analysis was used to explore the relationship between family functioning and PSD.
Results
The prevalence of PSD at acute hospitalization and 6 months post-discharge was 32.9% and 20.0%, respectively. SDS scores decreased significantly from baseline to 6 months post-discharge, while SF-FAD scores did not change significantly during this period. The Pearson correlation coefficient showed that SF-FAD scores were positively associated with SDS scores at the two time points (r1 = 0.341, r2 = 0.510, P < 0.05). Multiple linear regression analyses indicated that SF-FAD scores could predict PSD at baseline (unstandardized coefficient: 7.010, P < 0.05) and 6 months post-discharge (unstandardized coefficient: 9.672, P < 0.001).
Conclusion
This study found that first-ever stroke survivors had good family functioning at baseline and 6 months post-discharge. The findings in this study verified that poor family functioning is positively associated with PSD at different phases post-stroke. Good family functioning is an important protective factor against PSD.
Keywords:
Introduction
The socio-economic burden of stroke in China is sharply increasing, and the number of stroke patients in China ranks first worldwide, with approximately 17.04 million people over the age 40 have experienced strokes.Citation1 Additionally, Chinese residents over the age of 25 have the highest lifetime risk of stroke in the world, which means about two-fifths of Chinese people have a stroke risk in their lifetime.Citation2 Stroke is the leading cause of death and disability in China, which is characterized by high prevalence, mortality, and disability rates, posing a serious threat to the health of the Chinese population.Citation1 The weighted prevalence of stroke in Chinese people over age 40 years is increasing with time, reaching 2.58% in 2019.Citation3 In 2019, there were 3.94 million new cases of stroke, and stroke caused 2.19 million deaths and 45.9 million disability-adjusted life years (DALYs) in China.Citation4
Stroke severely impairs the physical condition of patients, with studies showing that 10.4% of stroke patients experienced severe disability within 1 month after a stroke.Citation5 Stroke survivors can also develop psychological disorders. Post-stroke depression (PSD) was the most common neuropsychiatric complication after a stroke, and about one-third of stroke patients experience post-stroke depression.Citation6 The most common risk factors for PSD were stroke severity, cognitive deficits and physical impairment.Citation7 Current studies found that 35.2% to 87% stroke patients had cognitive deficits, and there is a strong correlation between cognitive deficits and PSD.Citation8 The Edelkraut study found that there is a higher incidence of depression in stroke patients with aphasia.Citation9 The Williams and Demeyere study found that cognitive deficits in spatial attention, executive function, memory, number and language processing, and praxis could exacerbate depressive symptoms at 6 months post-stroke.Citation10 Depression seriously threatens the recovery and health outcomes for stroke patients. Stroke survivors with depression are more likely to have less effective rehabilitation post-stroke, higher all-cause mortality, suicidal ideation and stroke recurrence.Citation11–14 The stroke recurrence of patients with PSD was 1.48 times higher than that in those without PSD.Citation14
Psychotherapy plays a significant role in the treatment of PSD, and social support is considered the most meaningful factor against PSD.Citation15 In China, the family is the most basic social unit for individuals, and family relationships are an integral part of social support, especially for elder adults.Citation16 Family functioning refers to the family’s ability to meet the basic needs of family members and personal growth needs, as well as the ability to cope with difficult circumstances.Citation17 Family plays an important role in regulating an individual’s mental health, and one Chilean study conducted with 6206 families found that good family functioning is associated with fewer health problems in the family, especially a reduction of psychological and mental disorders.Citation18 A Chinese study of different family structures found that it is family functioning rather than family structure that can significantly affect an individual’s psychological well-being.Citation19 Family care is directly related to the quality of life of stroke patients at home.Citation20
Current study suggest an association between family functioning and depression in patients with major depressive disorder, and patients with healthy family functioning have shorter duration of depression.Citation21 Nan found that family care is beneficial in preventing depression in patients with chronic diseases, and patients with higher satisfaction with home support have lower depression levels.Citation22 One cross-sectional study of stroke patients in the acute phase found that family functioning is negatively associated with PSD.Citation23 Stroke patients remain at high risk of depression within 6 months post-stroke,Citation24 but there is a lack of longitudinal studies exploring the relationship between family functioning and PSD in different phases after stroke.
Therefore, the purposes of this study were to explore the development of family functioning and PSD from acute hospitalization to 6 months post-discharge, as well as the association between family functioning and PSD at the two time points in this population.
Methods
Study Design and Participants
This was a longitudinal study conducted over a period of 6 months. Convenience sampling was used in this study. Stroke survivors were recruited from the inpatient department of neurology of a hospital in Guangzhou, China. The inclusion criteria included the following: (1) hospitalized within one month after first-ever ischemic stroke, and (2) having clear consciousness to be able to read the questionnaires. The exclusion criteria were as follows: (1) history of depression; (2) Wernicke aphasia, or (3) accompanying diseases such as heart or liver disease, renal insufficiency, or malignant tumors.
Questionnaire Instruments and Variables
Sociodemographic and Disease-Related Characteristics
Sociodemographic and disease-related information consisted of gender, age, education, marriage, job, family history of stroke, smoking, the diagnosis of diabetes, hyperlipidemia, and disability post-stroke. Disability post-stroke was assessed by the Modified Rankin Scale (mRS) with good validity and reliability.Citation25 The total scores ranged from 0 (no disability) to 5 (severe disability requiring ongoing care). A score of ≥3 represents post-stroke disability.
Short Form Family Assessment Device
Family functioning was assessed by the Short Form Family Assessment Device (SF-FAD). The SF-FAD was simplified by Wang based on the Family Assessment Device.Citation26,Citation27 The SF-FAD contains six sub-scales, including problem solving, communication, affective responsiveness, affective involvement, behavior control and general functioning. SF-FAD contains 24 items, and each item has four responses “much like my home”, “like my home”, “not like my home”, or “not like my home at all” corresponding to a score of 1 to 4. The total SF-FAD score is equal to the total score of all entries/number of entries, and the total SF-FAD score ranges from 1 to 4. A higher SF-FAD and sub-scales score represents poorer family functioning, and a score lower than 2 indicates good family functioning. Cronbach’s alpha for the SF-FAD is 0.899.Citation26
Self-Rating Depression Scale
Depression was measured using the Self-Rating Depression Scale (SDS). This scale was developed by Zung to assess depression in terms of psychotic emotional symptoms, corporality disorders, psychomotor disorders and depressed psychological disorders.Citation28 The SDS consists of 20 items and the total score ranges from 20 to 80. Higher SDS scores indicate more severe depressive symptoms. The depression severity index is calculated from the cumulative score of 20 items out of 80 (maximum total score). The index ranges from 0.25 to 1.00. The higher the index, the more severe the depression, with an index ≥0.5 indicating depression.
Data Collection
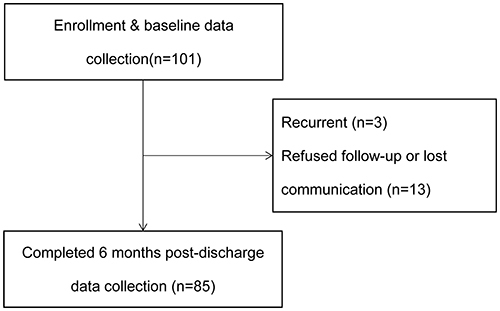
For patients who met the study inclusion criteria, the investigator explained the purpose, significance, requirements of the study, and the principles of privacy protection. Patients were informed that they had the right to decide to participate in or refuse this study, and they could withdraw from the study at any time for any reason, which would not negatively affect their treatment. Data collection began after patients voluntarily participated and signed an informed consent form. Sociodemographic and disease-related characteristics were collected during acute hospitalization (T1), and family functioning and PSD were assessed using the SF-FAD and SDS at the two time points (T1, at acute hospitalization and T2, 6 months post-discharge). Baseline data were collected at T1, including sociodemographic and disease-related characteristics, SF-FAD and SDS. The investigators collected baseline data with participants face-to-face in the ward. Prior to the time point of 6 months post-discharge, the investigators contacted participants in advance by telephone to determine the follow-up time. Participants needed to complete the SF-FAD and SDS at T2. Follow-up data were collected during participants’ outpatient review. If the patient could not return to the hospital, telephone interviews or electronic questionnaires were used to collect information. One hundred and one participants were recruited at baseline and completed the baseline measurement (). Eighty-five participants completed follow-up measurement at T2. Sixteen participants were excluded in this study because they did not complete follow-up assessment at T2 (three of whom had a recurrence of stroke and 13 refused follow-up or lost communication).
Statistical Analysis
Descriptive statistical analyses were performed to describe sociodemographic and disease-related characteristics, family functioning and PSD. Paired t-tests were used to explore the changes in SF-FAD and SDS scores at the two time points. The relationship between participants’ sociodemographic and disease-related characteristics and PSD was measured by the independent sample t-test and one-way analysis of variance. The Pearson correlation coefficient was used to examine the relationship between SF-FAD and SDS scores at the two time points. Multiple linear regression analysis (stepwise method) was used to verify the association between family functioning and PSD at baseline and 6 months post-discharge. All variables with P < 0.3 in the univariate analysis, as well as some common influencing factors (age, gender),Citation29,Citation30 were included as independent variables in the multivariate analyses at the two time points. All statistical analyses were performed by SPSS 25.0 (IBM Corp, Armonk, NY, USA), and P values less than 0.05 were considered statistically significant.
Results
Sociodemographic and Disease-Related Characteristics
The sociodemographic and disease-related characteristics are shown in . Eighty-five participants completed the 6 months follow-up. Among them, 62.4% participants were male, 51.8% were over 60 years old, 50.6% had a high school/technical secondary school education or higher, 91.8% had a spouse and 31.8% were in service. Of the participants, 35.3% had a family history of stroke, 31.8% were smokers, 30.6% also had diabetes, 44.7% also had hyperlipidemia, and 18.8% had post-stroke disability.
Table 1 Associations Between Sociodemographic and Disease-Related Characteristics of Participants and PSD at the Two Time Points (Univariate Analysis)
The Levels and Changes in Family Functioning and PSD at T1 (at Baseline) and T2 (6 Months Post-Discharge)
The SDS scores were 35.31±7.52 at T1 and 32.73±8.06 at T2, reducing significantly (P=0.013). indicates that 28 (32.9%) participants developed PSD during acute hospitalization, and 17 (20.0%) participants developed PSD at 6 months post-discharge, respectively.
Table 2 Changes in Family Functioning and PSD at the Two Time Points
The SF-FAD scores were 1.79±0.37 and 1.78±0.42 at the two time points, with no statistical difference in the SF-FAD scores during this period (P>0.05, ). All sub-scale scores of the SF-FAD were not statistically changed between T1 and T2 (P>0.05).
Relationship Between Family Functioning and PSD at T1 (Baseline)
At T1, there was a positive correlation between SF-FAD and SDS score (r1=0.341, P=0.001, ). Since higher SF-FAD and SDS score represent poorer family functioning and higher levels of depression severity, respectively, poor family functioning is positively associated with PSD at baseline. Scores on the sub-scales of “problem solving”, “communication”, “affective responsiveness”, “affective involvement”, and “general functioning” were positively correlated with SDS score (r1=0.297, 0.219, 0.288,0.296, 0.257, all P < 0.05).
Table 3 The Association Between Family Functioning and PSD by Pearson Correlation Coefficients at the Two Time Points
At baseline, the results of univariate analysis showed that sociodemographic and disease-related characteristics of participants were not associated with PSD (). The results of multiple linear regression analysis with the stepwise method at T1 showed that family functioning was the only factor for PSD (), and patients with higher SF-FAD score (poorer family functioning) had more severe depressive symptoms (unstandardized coefficient: 7.010, P=0.001, for model 1). This model explained approximately 10.5% of the variance in PSD at baseline (Rad2=0.105).
Table 4 The Association Between Family Functioning and PSD at the Two Time Points by Multiple Linear Regression (Stepwise Method)
Relationship Between Family Functioning and PSD at T2 (at 6 Months Post-Discharge)
At T2, scores on SF-FAD and its six sub-scales (including problem solving, communication, affective responsiveness, affective involvement, behavior control and general functioning) were positively correlated with SDS score (r2=0.510, 0.419, 0.399, 0.435, 0.341, 0.336, 0.440, respectively, all P<0.05, ).
Univariate analysis showed that there were no significant relationships between sociodemographic and disease-related characteristics and PSD at T2 (). The multiple linear regression results showed that family functioning remained associated with PSD at T2 (unstandardized coefficient: 9.672, P<0.001, ). Family functioning explained approximately 25.1% of the variance in PSD at 6 months post-discharge in stroke patients (Rad2=0.251).
Discussion
This study shows that first-ever stroke survivors had a high risk of PSD. The prevalence of PSD at acute hospitalization and 6 months post-discharge was 32.9% and 20.0%, respectively. Poor family functioning is positively associated with PSD at the two time points, and good family functioning is an important factor in preventing PSD.
A previous study has found that depressive symptoms show a non-statistically significant downward trend from 1 month to 3 months post-stroke.Citation31 This study further found that depressive symptoms significantly decreased from baseline to 6 months post-discharge. This study also found a high prevalence of PSD in the acute phase, which is similar to that in other studies.Citation32,Citation33 Of first-ever stroke survivors, 32.9% developed depression at acute hospitalization that needed attention. This study indicated that the risk of PSD is gradually reduced from acute hospitalization to 6 months post-discharge. It is noteworthy that one-fifth of participants suffered from PSD at 6 months post-discharge. PSD could contribute to a decline in the stroke patient’s physical function.Citation34 Therefore, early identification and treatment of PSD are necessary. However, the screening and diagnosis of depression in stroke patients is seriously insufficient.Citation35 One study found that only approximately 5% of stroke patients were diagnosed with depression in clinical practice.Citation36 Considering stroke patients have a high risk of PSD, attention should be paid to depression screening of hospitalized stroke patients and continuous follow-up post-discharge.
The results showed that participants in this study had good family functioning at baseline and 6 months post-discharge, which is better than that one Chinese study of outpatient stroke patients.Citation37 There were no significant differences in family functioning between the two time points. This suggests that the family system of the participants was robust enough to withstand the challenges of stroke post-discharge. This may have something to do with the family’s active coping with stroke. After a stroke, Chinese families make full use of family resources to meet the patient’s care and emotional needs,Citation38 which contributes to the stability of the family system. Gawulayo’s study suggests that when families provide a support system for stroke patients, stroke may improve family relationships and strengthen emotional ties.Citation39
This is the first longitudinal study to explore the association between family functioning and depression in stroke survivors. The results demonstrated the positive correlation between poor family functioning and PSD at baseline and 6 months post-discharge, and good family functioning is an important factor in preventing PSD. In addition, the sub-scale of general functioning represents overall functioning of family, and the “general functioning” sub-scale score is also positively related to PSD at the two time points. This further confirms the important role of family functioning in overcoming post-stroke depression. The observed preventive effect of good family functioning on PSD can be attributed to the stroke patients’ seeking support from their families. Family support and health status were found to be the most important protective factors against depression in Chinese older adults in one study.Citation40 Elderly people with good family functioning had a comfortable home environment and better care, thereby reducing depressive symptoms.Citation41 Stroke patients are dependent on family support, especially those with disabilities. One study showed that harmonious relationships between stroke patients and family members (including spouses and children) could enhance their life satisfaction.Citation42 Therefore, when a stroke patient has a good and stable family support system, family members provide adequate life and emotional support to the patient, which helps to reduce the psychological stress in stroke patients.
An interesting finding was that “problem solving” sub-scale score was positively associated with PSD over time. Problem solving refers to the family’s ability to cope with challenges and resolve instrumental or emotional problems and conflicts to maintain the effective functioning of the family system.Citation43 When a problem persists and cannot be solved, it will threaten the family system. For stroke patients and families, the onset of a stroke is a huge challenge, and it leads to a range of problems over time, including physical disability, psychological problems, and caregiving issues.
Caring for stroke patients is regarded as long-term, painful, and hard work for family caregivers that might impair their own physical and mental health.Citation44,Citation45 Family caregivers required a broad range of caregiving skills (such as medication administration, physical care, and nutrient), and they rely on clinical workers to obtain these relevant education.Citation44 However, the truth is that it is difficult for caregivers to get the information they need from clinical workers.Citation44 An intervention study found that problem-solving therapy was effective in reducing anxiety and depression levels and improving quality of life in stroke patients.Citation46 Therefore, clinical workers should educate stroke patients’ families on skills for daily living and caregiving to improve their problem-solving abilities and thus improve the mental health of stroke patients.
This study found that a positive association between “communication” sub-scale score and PSD over time. A previous study in patients with major depression has found poor communication ability of families was associated with longer depression duration.Citation21 This suggests that there should be a focus on the importance of family communication in alleviating the patient’s depressive symptoms.
There has been interest in studying the role of emotional support of family in preventing depression. The “affective involvement” sub-scale refers to family members taking an interest in each other’s affairs, and the “affective responsiveness” sub-scale indicates that family remember could provide appropriate affective reactions.Citation17 The findings in this study showed the scores of “affective involvement” and “affective responsiveness” were positively correlated to PSD at the two time points, which means poor affective involvement and affective responsiveness ability was associated with more severe depressive symptoms. Fang’s study found that the positive attitude of family member would improve patients’ cognitive recovery.Citation47
While the scores on “affective responsiveness” and “communication” sub-scales at the two time points indicate that stroke patients were performed poorly in these areas, which is consistent with the results of Jiang’s study.Citation37 This may be related to the introverted character of the Chinese people, especially the elderly, who are not good at expressing their thoughts and emotions directly. Therefore, family members should be encouraged to pay attention to the patient’s psychological condition and actively communicate and respond to the patient’s emotional needs to help alleviate depressive symptoms.
It is noteworthy that first-ever stroke patients had a high incidence of PSD. This study demonstrated that good family functioning is an important factor in preventing PSD. This study makes important contributions for management of PSD in stroke patients: (1) Clinical staff should recognize the importance of involving family systems in caring for patients’ mental health; (2) Current interventions for PSD in stroke patients typically target the individual and ignore the impact of the family system on the individual’s mental health. Studies in patients with major depression have found positive outcomes of family interventions in alleviating depressive symptoms.Citation48 This suggests that clinical workers should conduct family-based psychosocial interventions to prevent and treat PSD. (3) Family members should improve family functioning, including improving problem-solving skills, providing good care, offering adequate emotional support and communicating effectively to decrease stroke patients’ depressive symptoms.
Study Limitations
There are some limitations in this study. For instance, the participants enrolled in this study are from a single region in China, which may limit the generalization of the results. Patients’ family functioning and PSD were self-reported and therefore prone to bias. The sample size of this study was limited and future studies could expand the sample size to further investigate the relationship between family functioning and sociodemographic and disease-related factors and PSD.
Conclusion
First-ever stroke survivors are at high risk of depression at acute hospitalization and 6 months post-discharge. Medical workers need to monitor depressive symptoms in hospitalized stroke patients and continue to track their mental health post-discharge. This study demonstrates that family functioning is associated with PSD at acute hospitalization and 6 months post-discharge, and good family functioning is an important factor in preventing depression. Future interventions based on family systems should be considered to alleviate depression in post-stroke patients.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Informed Consent
This study was approved by the ethics committee of The Third Affiliated Hospital of Sun Yat-sen University (Approval no. [2018]02-421-01) in Guangzhou, China. This study was carried out in accordance with the Declaration of Helsinki. All participants signed the informed consent prior to their participation.
Disclosure
All authors report no conflicts of interest in this work.
Acknowledgment
We thank all the participants in this study.
Additional information
Funding
References
- Wang L, Peng B, Zhang H, et al. Brief report on stroke prevention and treatment in China, 2020. Chin J Cerebrovasc Dis. 2022;19(2):136–144.
- Feigin VL, Nguyen G, Cercy K, et al. Global, regional, and country-specific lifetime risks of stroke, 1990 and 2016. N Engl J Med. 2018;379(25):2429–2437. doi:10.1056/NEJMoa1804492
- Tu W, Hua Y, Yan F, et al. Prevalence of stroke in China, 2013–2019: a population-based study. Lancet Reg Health West Pac. 2022:100550. doi:10.1016/j.lanwpc.2022.100550
- Ma Q, Li R, Wang L, et al. Temporal trend and attributable risk factors of stroke burden in China, 1990–2019: an analysis for the Global Burden of Disease Study 2019. Lancet Public Health. 2021;6(12):e897–e906. doi:10.1016/S2468-2667(21)00228-0
- O’Donnell MJ, Chin SL, Rangarajan S, et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. Lancet. 2016;388(10046):761–775. doi:10.1016/S0140-6736(16)30506-2
- Mitchell AJ, Sheth B, Gill J, et al. Prevalence and predictors of post-stroke mood disorders: a meta-analysis and meta-regression of depression, anxiety and adjustment disorder. Gen Hosp Psychiatry. 2017;47:48–60. doi:10.1016/j.genhosppsych.2017.04.001
- Babkair LA. Risk factors for poststroke depression: an integrative review. J Neurosci Nurs. 2017;49(2):73–84. doi:10.1097/JNN.0000000000000271
- Terroni L, Sobreiro MFM, Conforto AB, et al. Association among depression, cognitive impairment and executive dysfunction after stroke. Dement Neuropsychol. 2012;6(3):152–157. doi:10.1590/S1980-57642012DN06030007
- Edelkraut L, López-Barroso D, Torres-Prioris MJ, et al. Spectrum of neuropsychiatric symptoms in chronic post-stroke aphasia. World J Psychiatry. 2022;12(3):450–469. doi:10.5498/wjp.v12.i3.450
- Williams OA, Demeyere N. Association of depression and anxiety with cognitive impairment 6 months after stroke. Neurology. 2021;96(15):e1966–e1974. doi:10.1212/WNL.0000000000011748
- Kobylańska M, Kowalska J, Neustein J, et al. The role of biopsychosocial factors in the rehabilitation process of individuals with a stroke. Work. 2018;61(4):523–535. doi:10.3233/WOR-162823
- Cai W, Mueller C, Li Y, Shen W, Stewart R. Post stroke depression and risk of stroke recurrence and mortality: a systematic review and meta-analysis. Ageing Res Rev. 2019;50:102–109. doi:10.1016/j.arr.2019.01.013
- Bartoli F, Pompili M, Lillia N, et al. Rates and correlates of suicidal ideation among stroke survivors: a meta-analysis. J Neurol Neurosurg Psychiatry. 2017;88(6):498–504. doi:10.1136/jnnp-2017-315660
- Wu QE, Zhou AM, Han YP, et al. Poststroke depression and risk of recurrent stroke: a meta-analysis of prospective studies. Medicine. 2019;98(42):e17235. doi:10.1097/MD.0000000000017235
- Das J, R GK. Post stroke depression: the sequelae of cerebral stroke. Neurosci Biobehav Rev. 2018;90:104–114. doi:10.1016/j.neubiorev.2018.04.005
- Chi I, Chou K. Social support and depression among elderly Chinese people in Hong Kong. Int J Aging Hum Dev. 2001;52(3):231–252. doi:10.2190/V5K8-CNMG-G2UP-37QV
- Epstein NB, Bishop DS, Levin S. The McMaster model of family functioning. J Marital Fam Ther. 1978;4:19–31. doi:10.1111/j.1752-0606.1978.tb00537.x
- García-Huidobro D, Puschel K, Soto G. Family functioning style and health: opportunities for health prevention in primary care. Br J Gen Pract. 2012;62(596):e198–e203. doi:10.3399/bjgp12X630098
- Cheng Y, Zhang L, Wang F, Zhang P, Ye B, Liang Y. The effects of family structure and function on mental health during China’s transition: a cross-sectional analysis. BMC Fam Pract. 2017;18(1):59. doi:10.1186/s12875-017-0630-4
- Baumann M, Le Bihan E, Chau K, Chau N. Associations between quality of life and socioeconomic factors, functional impairments and dissatisfaction with received information and home-care services among survivors living at home two years after stroke onset. BMC Neurol. 2014;14:92. doi:10.1186/1471-2377-14-92
- Song J, Chen H, Liang T. Family functioning and 1-year prognosis of first-episode major depressive disorder. Psychiatry Res. 2019;273:192–196. doi:10.1016/j.psychres.2019.01.021
- Nan H, Lee PH, McDowell I, Ni MY, Stewart SM, Lam TH. Depressive symptoms in people with chronic physical conditions: prevalence and risk factors in a Hong Kong community sample. BMC Psychiatry. 2012;12:198. doi:10.1186/1471-244X-12-198
- Yang L, Zhao Q, Liu H, Zhu X, Wang K, Man J. Family functioning mediates the relationship between activities of daily living and poststroke depression. Nurs Res. 2021;70(1):51–57. doi:10.1097/NNR.0000000000000472
- Towfighi A, Ovbiagele B, El Husseini N, et al. Poststroke depression: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2017;48(2):e30–e43. doi:10.1161/STR.0000000000000113
- Banks JL, Marotta CA. Outcomes validity and reliability of the modified Rankin Scale: implications for stroke clinical trials. Stroke. 2007;38(3):1091–1096. doi:10.1161/01.STR.0000258355.23810.c6
- Wang M. The Construction of the Ecological Model of Healthy Behavior of Hypertension Patients with Stroke at the End of Recovery Period. Sun Yat-sen University; 2020.
- Miller IW, Epstein NB, Bishop DS, Keitner GI. The McMaster family assessment device: reliability and validity. J Marital Fam Ther. 1985;11:345–356. doi:10.1111/j.1752-0606.1985.tb00028.x
- Zung W, Gianturco J. Personality dimension and the self-rating depression scale. J Clin Psychol. 1971;27(2):247–248. doi:10.1002/1097-4679(197104)27:2<247::aid-jclp2270270230>3.0.co;2-6
- Almhdawi KA, Alazrai A, Kanaan S, et al. Post-stroke depression, anxiety, and stress symptoms and their associated factors: a cross-sectional study. Neuropsychol Rehabil. 2021;31(7):1091–1104. doi:10.1080/09602011.2020.1760893
- Lyu Y, Li W, Tang T. Prevalence trends and influencing factors of post-stroke depression: a study based on the National Health and Nutrition Examination Survey. Med Sci Monit. 2022;28:e933367. doi:10.12659/MSM.933367
- Hu R, Wang X, Liu Z, et al. Stigma, depression, and post-traumatic growth among Chinese stroke survivors: a longitudinal study examining patterns and correlations. Top Stroke Rehabil. 2022;29(1):16–29. doi:10.1080/10749357.2020.1864965
- Zhou X, Liu Z, Zhang W, Zhou L. Resilience is associated with post-stoke depression in Chinese stroke survivors: a longitudinal study. J Affect Disord. 2020;273:402–409. doi:10.1016/j.jad.2020.04.042
- Isuru A, Hapangama A, Ediriweera D, Samarasinghe L, Fonseka M, Ranawaka U. Prevalence and predictors of new onset depression in the acute phase of stroke. Asian J Psychiatr. 2021;59:102636. doi:10.1016/j.ajp.2021.102636
- El Husseini N, Goldstein LB, Peterson ED, et al. Depression status is associated with functional decline over 1-year following acute stroke. J Stroke Cerebrovasc Dis. 2017;26(7):1393–1399. doi:10.1016/j.jstrokecerebrovasdis.2017.03.026
- Bhattacharjee S, Axon DR, Goldstone L, Lee JK. Patterns and predictors of depression treatment among stroke survivors with depression in ambulatory settings in the United States. J Stroke Cerebrovasc Dis. 2018;27(3):563–567. doi:10.1016/j.jstrokecerebrovasdis.2017.09.047
- Swartz RH, Bayley M, Lanctôt KL, et al. Post-stroke depression, obstructive sleep apnea, and cognitive impairment: rationale for, and barriers to, routine screening. Int J Stroke. 2016;11(5):509–518. doi:10.1177/1747493016641968
- Jiang S, Shen L, Ruan H, Li L, Gao L, Wan L. Family function and health behaviours of stroke survivors. Int J Nurs Sci. 2014;1:272–276. doi:10.1016/j.ijnss.2014.05.024
- Qiu X, Sit J, Koo FK. The influence of Chinese culture on family caregivers of stroke survivors: a qualitative study. J Clin Nurs. 2018;27(1–2):e309–e319. doi:10.1111/jocn.13947
- Gawulayo S, Erasmus CJ, Rhoda AJ. Family functioning and stroke: family members’ perspectives. Afr J Disabil. 2021;10:801. doi:10.4102/ajod.v10i0.801
- Yu J, Li J, Cuijpers P, Wu S, Wu Z. Prevalence and correlates of depressive symptoms in Chinese older adults: a population‐based study. Int J Geriatr Psychiatry. 2012;27(3):305–312. doi:10.1002/gps.2721
- Souza RA, Costa GDD, Yamashita CH, et al. Family functioning of elderly with depressive symptoms. Rev Esc Enferm USP. 2014;48(3):469–476. doi:10.1590/s0080-623420140000300012
- Liu Y, Liu J, Zhou S, et al. Life satisfaction and its influencing factors of middle-aged and elderly stroke patients in China: a national cross-sectional survey. BMJ Open. 2022;12(8):e059663. doi:10.1136/bmjopen-2021-059663
- Zhang Y. Family functioning in the context of an adult family member with illness: a concept analysis. J Clin Nurs. 2018;27(15–16):3205–3224. doi:10.1111/jocn.14500
- Camak DJ. Addressing the burden of stroke caregivers: a literature review. J Clin Nurs. 2015;24(17–18):2376–2382. doi:10.1111/jocn.12884
- Zhang J, Lee DTF. Meaning in stroke family caregiving: a literature review. Geriatr Nurs. 2017;38(1):48–56. doi:10.1016/j.gerinurse.2016.07.005
- Chalmers C, Leathem J, Bennett S, Mcnaughton H, Mahawish K. The efficacy of problem solving therapy to reduce post stroke emotional distress in younger (18–65) stroke survivors. Disabil Rehabil. 2019;41(7):753–762. doi:10.1080/09638288.2017.1408707
- Fang Y, Tao Q, Zhou X, et al. Patient and family member factors influencing outcomes of poststroke inpatient rehabilitation. Arch Phys Med Rehabil. 2017;98(2):249–55.e2. doi:10.1016/j.apmr.2016.07.005
- Katsuki F, Watanabe N, Yamada A, Hasegawa T. Effectiveness of family psychoeducation for major depressive disorder: systematic review and meta-analysis. BJPsych Open. 2022;8(5):e148. doi:10.1192/bjo.2022.543