Abstract
Purpose
The study aims to clarify the negative psychological state and resilience impairments of schizophrenia (SCZ) with metabolic syndrome (MetS) while evaluating their potential as risk factors.
Patients and Methods
We recruited 143 individuals and divided them into three groups. Participants were evaluated using the Positive and Negative Syndrome Scale (PANSS), Hamilton Depression Rating Scale (HAMD)-24, Hamilton Anxiety Rating Scale (HAMA)-14, Automatic Thoughts Questionnaire (ATQ), Stigma of Mental Illness scale and Connor–Davidson Resilience Scale (CD-RISC). Serum biochemical parameters were measured by automatic biochemistry analyzer.
Results
The score of ATQ was highest in the MetS group (F = 14.5, p < 0.001), and the total score of CD-RISC, subscale tenacity score and subscale strength score of CD-RISC were lowest in the MetS group (F = 8.54, p < 0.001; F = 5.79, p = 0.004; F = 10.9, p < 0.001). A stepwise regression analysis demonstrated that a negative correlation was observed among the ATQ with employment status, high-density lipoprotein (HDL-C), and CD-RISC (β=−0.190, t=−2.297, p = 0.023; β=−0.278, t=−3.437, p = 0.001; β=−0.238, t=−2.904, p = 0.004). A positive correlation was observed among the ATQ with waist, TG, WBC, and stigma (β=0.271, t = 3.340, p = 0.001; β=0.283, t = 3.509, p = 0.001; β=0.231, t = 2.815, p = 0.006; β=0.251, t=−2.504, p = 0.014). The area under the receiver-operating characteristic curve analysis showed that among all independent predictors of ATQ, the TG, waist, HDL-C, CD-RISC, and stigma presented excellent specificity at 0.918, 0.852, 0.759, 0.633, and 0.605, respectively.
Conclusion
Results suggested that the non-MetS and MetS groups had grievous sense of stigma, particularly, high degree of ATQ and resilience impairment was shown by the MetS group. The TG, waist, HDL-C of metabolic parameters, CD-RISC, and stigma presented excellent specificity to predict ATQ, and the waist showed excellent specificity to predict low resilience level.
Introduction
Schizophrenia (SCZ) is a debilitating psychiatric disorder with unknown etiology affecting ~1% of the population worldwide; it is also considered one of the most incapacitating diseases.Citation1 Previous observational studies have reported that the prevalence of metabolic syndrome (MetS) is high in patients with SCZ, from the increased coronary risk two-fold to four-fold of the remaining population,Citation2 even to the extent of obtaining higher standardized mortality rate in SCZ patients.Citation3,Citation4 MetS refers to the co-occurrence of several known cardiovascular risk factors, including insulin resistance, obesity, atherogenic dyslipidemia and hypertension,Citation5 studies also indicated that the MetS in persons with SCZ would increase their risk of developing cardiovascular disease, consequently reducing their life expectancy by approximately 10 to 25 years.Citation3,Citation6 Generally, antipsychotics are considered to be one of the main causes of MetS.Citation4,Citation7 Furthermore, researchers showed clear evidence of an increased risk of all cardiovascular and metabolic diseases, including untreated and antipsychotic-naive individuals.Citation8,Citation9 The evidence indicated that the risk factors for cardiovascular diseases, diabetes mellitus, and MetS of SCZ may have other influences dependent on common unhealthy lifestyle, smoking, weight, adipokines dysregulation, and inflammation pathophysiologic mechanisms or psychosocial mechanisms.Citation10,Citation11 Hence, a comprehensive study between psychosocial mechanisms and MetS component in the SCZ is necessary.
Reports show that in patients with SCZ, 54.6–61.0% is comorbid with depression.Citation12 Previous studies have investigated the MetS component in specific SCZ, and results displayed that psychosocial risk may be closely related to severity of MetS in SCZ.Citation13,Citation14 Thus, the management of psychosocial factors could address an important predisposing factor for MetS in SCZ. Psychosocial risk factors related to MetS in SCZ have been reported to include negative automatic thoughts and stigma.Citation15 These psychosocial risk factors play a pivotal role to initiate and facilitate unhealthy habits, such as poor treatment compliance, unhealthy dietary pattern, lack of physical activity,Citation16 excessive drinking, smoking, and sleeping problems,Citation17 which contribute to the generation and development of cardiovascular diseases, diabetes mellitus, and MetS.Citation18 Prior investigations have indicated that negative affect and internalized stigma are not only less valuable because they have a mental illness,Citation19 but can also be obstacles to treatment adherence and negatively influence long-term recovery.Citation20 However, studies on the psychosocial risk mechanisms of MetS in SCZ are limited; thus, further research would provide useful insights into this issue.
Recently, cognitive variables, such as resilience variables, have attracted remarkable attention on account of their association with clinical symptom, psychosocial outcomes and quality of life in patients with SCZ.Citation21 Furthermore, investigators detected that negative beliefs and positive beliefs about oneself are necessary for recovery in the MetS in SCZ.Citation20,Citation22 Resilience ability would be a shift in focus from risk to protective factors and from psychopathological remission to personal recovery.Citation23,Citation24 In this regard, they suggested that a lower ability of resilience could contribute to failure experiences, avoidance of activities of daily living, and difficulties in daily life.Citation16,Citation25 Resilience has become one of the key concepts in understanding the possibility of subjective wellness in SCZ. Previous studies have shown the associations of resilience in SCZ with self-esteem and hopelessness,Citation26 but lack of knowledge about stigma and negative automatic thoughts about MetS of SCZ, as well as deficiency of these information appear to be shortcomings to the active monitoring of physical health in patients with SCZ.
To the best of our knowledge, studies investigating the psychiatric parameters of negative automatic thinking, stigma, and resilience in the SCZ with MetS are rare. We hypothesize that these negative psychological mechanism and resilience play a diverse role in SCZ patients with MetS, contributing to the understanding of the effective treatment goal for SCZ. This study aims to test that negative automatic thinking, stigma, and resilience are related to SCZ with MetS and to determine clinical factors that predict these negative psychological parameters and resilience in SCZ patients with MetS. Thus, this study was considered to make a distinct contribution to the literature by evaluating negative automatic thinking, stigma, and resilience as a multidimensional concept for focusing on clinical psychotic symptoms and metabolic parameters expected to predict factors in SCZ with MetS.
Materials and Methods
Participants
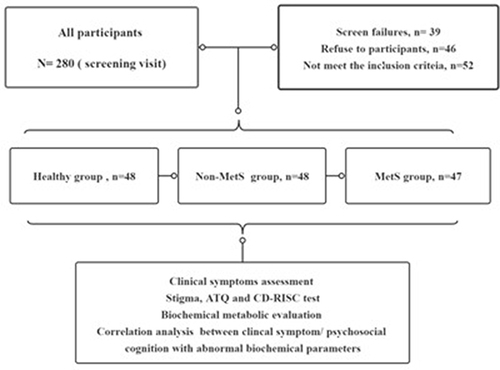
This cross-sectional cohort research was conducted at the Anhui Mental Health Center (AMHC). All participants signed a written consent prior to research participation in conformity to the principles of the Declaration of Helsinki. The present research was approved by the Medical Ethics Committee of AMHC, and the trial clinical registration number was ChiCTR2100045240. Initially, 280 participants were selected from February 2019 and September 2021, among which 39 individuals failed to complete the questionnaires, 46 individuals refused to participate in the study, and 52 individuals did not meet the criteria. Ultimately, the remaining 143 participants were included and divided into three groups according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5),Citation27 and the guideline standards for the prevention and treatment of dyslipidemia in Chinese adults in 2007 for MetS;Citation28 namely, the healthy control group (n = 48), nonmetabolic syndrome (non-MetS) group (n = 48), and MetS group (n = 47). The healthy controls were recruited from the community of healthy people, and the patients of non-MetS and MetS were hospitalized in AMHC ().
All individuals were evaluated using Chinese version of the Mini-International Neuropsychiatric Interview 5.0.0. (C-MINI5.0.0).Citation29 At the time of study admission, the inclusion criteria for the patients in the MetS group were as follows: (1) age = 18–65 years; (2) satisfied the DSM-5 criteria for SCZ; (3) patients treated with second-generation anti SCZ drugs (SGAs) for more than three months, and satisfied the guideline standards for the prevention and treatment of dyslipidemia in Chinese adults in 2007 for MetS. (4) non acute exacerbation patients. The inclusion criteria for the patients in the non-MetS group were as follows: (1) satisfied the first and second criteria for the inclusion in the MetS group; (2) after taking the SGAs for three months, non-fulfillment of the guideline standards for the prevention and treatment of dyslipidemia in Chinese adults in 2007. (3) non acute exacerbation patients. Healthy controls were recruited from the local community through advertising. The exclusion criteria were as follows: (1) except SCZ, patients suffering from other mental diseases and substance abuse; (2) people with cardiovascular diseases, diabetes mellitus, MetS, and endocrine and other serious physical diseases prior to participating in the study; (3) patients with epilepsy and dementia; (4) had received electroconvulsive therapy for six months; (5) pregnant or lactating women. All subjects received basic sociodemographic assessments, clinical scale evaluation, and metabolic testing from trained professional psychiatrists.
Clinical Assessments
Sociodemographic Information
Including age, gender, ethnicity, marital status, educational attainment, and employment status were collected. Participants provided information on whether they knew a close friend or family member with a mental illness. Their occupation and length of service also were recorded.
Assessments C-MINI 5.0.0
Chinese version of the Mini-International Neuropsychiatric Interview (C-MINI) 5.0.0 demonstrated excellent validity and reliability. The reliability inter-rater and test–retest of C-MINI 5.0.0 were excellent, and the kappa values were above 0.80 and 0.90, respectively. The C-MINI is the gold standard to diagnose SCZ.Citation30
Positive and Negative Syndrome Scale
We used the Positive and Negative Syndrome Scale (PANSS) to assess positive and negative symptoms in SCZ patients, the Mandarin version model of the PANSS has a Cronbach’s alpha coefficient of 0.928 and an intra-class coefficient of 0.878. Higher scores indicate a greater level of symptom severity.Citation31
Hamilton Depression Rating Scale-24
Hamilton Depression Rating Scale-24 (HAMD-24) was the most commonly evaluated depressive symptom scale. It has a high specificity to assess the severity of depression symptoms. The Cronbach’s α score of HAMD-24 is 0.88, and the κ-score is 0.92.Citation32
Hamilton Anxiety Rating Scale-14
Hamilton Anxiety Rating Scale-14 (HAMA-14) is one of the most widely used rating scales to evaluate the severity of perceived anxiety; a higher score represented greater anxiety. HAMA-14 score is from 0 to 4; it provides a general guideline to distinguish the severity of staged anxiety.Citation32
Automatic Thoughts Questionnaire
Automatic Thoughts Questionnaire (ATQ) is widely used to assess the frequent occurring negative thoughts. ATQ shows good internal consistency among Chinese with mental disorders (Cronbach’s α= 0.96). Higher scores indicate heavier negative thinking and depression.Citation33
Internalized Stigma of Mental Illness Scale
Internalized Stigma of Mental Illness Scale is a scale for assessing sense of self-stigma of patient and has a long history to assess a differential effect of mental health attitudes. Research participants were instructed to rate patients using a 4-point Likert scale ranging from 1. “I do not think so” to 4. “I very much think so”. Higher scores indicate greater stigma (α = 0.82).Citation34,Citation35
Connor–Davidson Resilience Scale
Connor–Davidson Resilience Scale (CD-RISC) may be viewed as a measure of stress-coping ability. CD-RISC comprises 25 items, each rated on a 5-point scale (0–4), with higher scores reflecting greater resilience. The CD-RISC has sound higher distinguish reliability and validity, CD-RISC shows good internal consistency, and Cronbach’s α for the full scale is 0.89.Citation36
Laboratory Biochemical Evaluation
After an overnight fasting period, peripheral venous blood samples (5 mL) were collected from all individuals between 6:30 and 7:00 in the morning. Samples were sent to the Department of Clinical Laboratory for blood biochemistry analysis within 2 h. Blood routine analysis was performed using an automatic hematology analyzer (Mindray BC-2800, Shenzhen, China). Serum biochemical parameters were measured by an automatic biochemistry analyzer (AU480, Beckman Coulter, USA) using commercial kits (Roche, Switzerland). An automatic sphygmomanometer was used to measure systolic pressure (DBP) and diastolic pressure (SBP) prior to blood collection. Waist circumference was tested by horizontal girth across the center of the umbilicus. MetS is diagnosed when three or more of the following items are satisfied: (1) abdominal obesity according to waist circumference (CM): male >90, female >85; (2) blood triglyceride (TG) >1.7 mmol/l; (3) blood high-density lipoprotein (HDL-C) <1.04 mmol/L; (4) blood pressure ≥130/85 mmHg; (5) fasting blood glucose (FPG) >6.1 mmol/l and/or postprandial 2-hour blood glucose kk (2H PG) is more than 7.8 mmol/l or with diabetes history.
Statistical Analysis
Demographic characteristics and clinic symptoms were determined using Chi-square test and one-way ANOVA to compare differences among the three groups. Fisher’s least significant difference (LSD) was used for multiple comparisons. Spearman correlation analysis was used to test the possible correlation among clinical symptoms, MetS factors with ATQ, resilience, and stigma scale scores. Stepwise linear regression analysis was conducted to explore the relationship between ATQ, resilience, and stigma and metabolic factors in patients with MetS. The area under the receiver-operating characteristic curve (ROC) was used to assess the metabolic indicators to evaluate the impairments of ATQ, resilience, and stigma function. The sensitivity and specificity were also obtained at the optimal cutoff value of 0.5 as defined by ROC. All statistical tests were two-tailed tests, and the statistical significance was set to α < 0.05. All analyses were conducted using the SPSS version 22.0 (IBM Corp).
Results
Demographic and Clinical Characteristics of the Participants
Demographic and clinical features of participants classified into categories are shown in and . The final sample included 52.1% (n = 25) males and 47.9% (n = 23) females in the healthy control, 43.8% (n = 21) males and 56.2% (n = 27) females in the no-MetS group, and 55.3% (n = 26) males and 44.7% (n = 21) females in the MetS group (F = 1.358, p = 0.507). Overall, apart from the employment status that exhibited a significant difference (F = 6.157, P = 0.046), no significant difference was found in the demographic background, such as age, years of education, course of disease, and marital status among the three groups (p≥ 0.05). No diversity was found in the white blood cell, neutrophile granulocyte, and red blood cell of blood routine parameters among the three groups (F = 2.270, p = 0.107; F = 0.446, p = 0.641; F = 1.824, p = 0.165). Furthermore, we investigated the biochemical parameters, and the results showed that the MetS group had the highest levels of systolic pressure, waist, fasting blood glucose, and triglyceride (TG) (F = 10.191, p < 0.001; F = 39.818, p < 0.001, F = 15.892, p < 0.001; F = 25.895, p < 0.001). On the contrary, the levels of HDL-C and apolipoprotein-A (Apo-A) were the lowest in the MetS group (F = 53.553, p < 0.001; F = 39.818, p < 0.001). Conclusively, the results of the clinical symptom evaluation showed no significant difference in psychotic symptoms, depressive symptoms, and stigma between the metabolic group and the non-metabolic group (p≥ 0.05). Fascinatingly, the ATQ total score was the highest (F=14.5, <0.001), and the CD-RISC total score, tenacity, and strength of the CD-RISC subscales were the lowest in the MetS group (F = 8.54, p < 0.001; F = 5.79, p = 0.004; F = 10.9, p < 0.001).
Table 1 General Demographic Background, Blood Routine, and Biochemical Indicators Among the Three Groups
Table 2 Comparison of Resilience, Automatic Thoughts and Stigma Among Three Groups
Factors Correlated Between Clinical Symptoms and Resilience, Stigma, and Negative Automatic Thoughts
The potential risk factors correlated between clinical symptoms and resilience, stigma, and negative automatic thoughts are evaluated, and the results are shown in . First, we found that ATQ had negative correlation with strength of CD-RISC (r = −0.218, p = 0.034) and positive correlation with stigma (r = 0.244, p = 0.017). Second, we figured out that the negative symptoms and depression symptoms of PANSS were positively correlated to the ATQ (r = 0.253, p = 0.013; r = 0.242, p = 0.018). Finally, the results of the present study indicated that total scores of HAMD and of HAMA were positively related to ATQ (r = 0.301, p = 0.003; r = 0.202, p = 0.049).
Table 3 Correlation Analysis Among Clinical Symptoms and Resilience, Stigma and Automatic Thinking
In the same way, we used Spearman correlation analysis to assess the correlation between the blood routine and biochemical parameters and resilience, stigma, and negative automatic thoughts. The results are shown in . The indices indicated that waist, FGB and TG have a negative correlation with tenacity (r=−0.215, p = 0.036; r=−0.225, p = 0.028; r=−0.21, p = 0.041); meanwhile, waist and FGB also have a negative correlation with strength (r=−0.174, p = 0.092; r=−0.275, p = 0.007); moreover, waist and Apo-B have a negative correlation with optimism (r=−0.206, p = 0.045; r=−0.245, p = 0.017). Furthermore, waist and FGB revealed negative correlation with resilience (r=−0.226, p = 0.007; r=−0.220, p = 0.008), whereas Cr and RED showed positive correlation with resilience (r = 0.221, p = 0.008; r = 0.166, p = 0.047). HDL-C and Apo-A showed a negative correlation with ATQ (r=−0.291, p < 0.001; r=−0.338, p < 0.001). On the contrary, the parameters of waist, FGB, TG, WBC, and NEU were positively correlated with ATQ (r = 0.270, p = 0.001; r = 0.198, p = 0.018; r = 0.265; p = 0.001; r = 0.247, p = 0.003; r = 0.242, p = 0.004).
Table 4 Correlation Analysis Among Biochemical Parameters with Stigma, Resilience and Automatic Thoughts
Independent Predictors of Resilience, Stigma, and Negative Automatic Thoughts
Stepwise regression analyses of demographic features and biochemical parameters were conducted to predict risk factors for resilience, stigma, and negative automatic thoughts. The final model from forward regression indicated that the ATQ, years of education, and course of disease accounted for the remarkable variance in the stigma. The stigma showed a significant positive relationship with ATQ and course of disease (β=0.251, t = 2.504, p = 0.014; β=0.228, t = 2.255, p = 0.026), but negative correlation with years of education (β=−0.216, t=−2.130, p = 0.036). Moreover, the final model from forward regression indicated that the employment status, waist, TG, HDL-C, WBC, CD-RISC, and stigma accounted for the remarkable variance in the ATQ. Among these factors, a negative correlation was observed between the ATQ and employment status, HDL-C, and CD-RISC (β=−0.190, t=−2.297, p = 0.023; β=−0.278, t=−3.437, p = 0.001; β=−0.238, t=−2.904, p = 0.004). Meanwhile, a positive correlation was observed between the ATQ and waist, TG, WBC, and stigma (β=0.271, t = 3.340, p = 0.001; β=0.283, t = 3.509, p = 0.001; β=0.231, t = 2.815, p = 0.006; β=0.251, t=−2.504, p = 0.014). Ultimately, the final model from forward regression indicated that the waist and Cr accounted for the remarkable variance in the CD-RISC. A negative correlation was observed between the CD-RISC and waist (β=−0.229, t=−2.787, p = 0.006); conversely, the index of Cr showed a positive relationship with CD-RISC (β=0.215, t = 2.612, p = 0.010). The results are shown in .
Table 5 Stepwise Linear Regression Analysis of Stigma, CD-RISC and Automatic Thinking
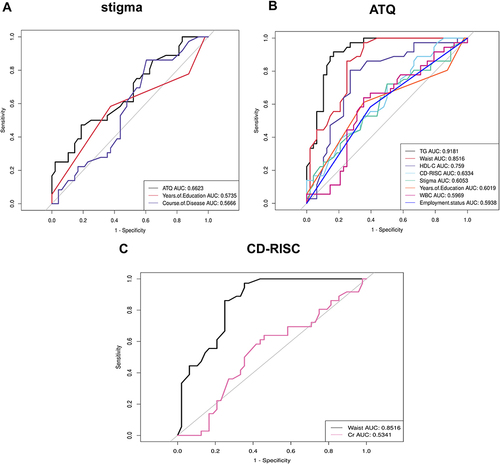
The ROC curve analysis was conducted to predict the stigma, negative automatic thoughts, and resilience function impairments of MetS groups by using dysbiosis of MetS indexes and clinical symptoms. The results showed that among all independent predictors of stigma, ATQ was 0.662 () and had excellent specificity. Furthermore, among all independent predictors of ATQ, the TG, waist, HDL-C, CD-RISC, and stigma presented excellent specificity at 0.918, 0.852, 0.759, 0.633, and 0.605, respectively (). Eventually, among all independent predictors of CD-RISC, waist was 0.852 () and showed excellent specificity.
Figure 2 ROC curve analysis was used to predict the psychological structure impairment of MetS groups by using dysbiosis of MetS parameters and demographic and clinical characteristics. (A) Independent risk factors used to predict stigma; (B) Independent risk factors used to predict ATQ; (C) lndependent risk factors used to predict CD-RISC.
Discussion
The present study has explored the relationship between metabolic parameters and self-stigma, ATQ, as well as resilience in SCZ with MetS. First, an important outcome of our study explored the increased impaired resilience and intensity of ATQ in SCZ with MetS group compared with that in the SCZ with non-MetS group. Second, the results of this study have shown that ATQ was not only positively related to the negative symptoms of PANSS, HAMA, and HAMD, but also positively correlated with metabolic parameters such as waist, FGB, and TG. Moreover, the ATQ was proven to exhibit excellent specificity in predicting higher levels of self-stigma. Especially, the high level of TG, waist, HDL-C and self-stigma also presented excellent specificity in predicting ATQ. Most importantly, the waist showed excellent specificity in predicting low resilience level. Therefore, ATQ emerged closely correlated with self-stigma, severity of clinical symptoms and metabolic indicators. These findings indicated that psychological factors may be meaningful targets for psychosocial interventions aimed at improving metabolic dysfunctional outcome in SCZ.
Similar results of the metabolic parameters as specific risk predictors have been found previously in SCZ,Citation37 indicating relevant influence on multifaceted disorders of sugar, lipid, and protein metabolism.Citation38,Citation39 Especially, the high levels of waist circumference, body mass index (BMI),Citation2,Citation40,Citation41 blood sugar, hypertriglyceridemia, LDL-C, hypertension, and low level of HDL-C were most correlated with MetS in SCZ.Citation38,Citation42 Consistent with these homologous results, the SBP, waist, FGB, CHOL, and TG of the metabolic parameters showed the highest level in the MetS group among three groups. In addition, the MetS group obtained the lowest levels of HDL-C and Apo-A. Moreover, a considerable number of studies demonstrated that the metabolic disturbances in SCZ increase with illness durationCitation43 and age.Citation44 Some controversial studies could not detect metabolic indexes alterations in first-episode, drug-naive SCZ patients, but these findings could also be due to small sample sizes, low severity, and short disease duration.Citation3 Unfortunately, in our study, we did not find that illness duration and age had correlation with the metabolic disturbances in SCZ.
Generally, antipsychotic treatments have been dedicated to clinical MetS dysregulations.Citation45 In particular, second-generation antipsychotics have been reported to induce weight gain, abdominal obesity, lipid, and fasting plasma glucose level alterations.Citation46 However, some studies have proven metabolic alterations to occur even without weight gain.Citation43 Controversial results have triggered speculation on whether SCZ confers an inherent risk for metabolic alterations or whether the impact is not solely due to antipsychotic use.Citation3 Prior investigations have indicated that stigmatization to patients with SCZ is a global problem, and they even experience stigma as a “second illness”.Citation47 The negative consequences of stigma have been reported to impact the recovery of symptoms and life quality, adhering to mental health care, employment, income, and suicidality.Citation17,Citation34,Citation48 In the present study, the discrepancy of perceived stigma severity was not found between the MetS group and non-MetS group. Nevertheless, the proportion of stigma showed that more than 40% patients in the MetS and non-MetS groups feel highly stigmatized. Intriguingly, we found that stigma had a positive correlation with ATQ, and ATQ, high educational level, and longer course of disease can sensitively predict the stigma in the SCZ with MetS. These results may provide purposeful insight into the psychological structure of recovery and could achieve effective interventions for patients with SCZ.
The psychotic structure of SCZ impairs memory, attention, testing reality, and perceptual ability, leading to dysfunctional thoughts.Citation49 Previous studies demonstrated that these dysfunctional thoughts, including negative ATQ and resilience impairment seriously affect the emotions and behavior of patients with SCZ and are responsible for the daily life function, social adaptation, or rehabilitation of clinical symptoms.Citation50 The results of our previous research showed that the aberrant parameters of high waist circumference, triglyceride, and negative ATQ had effective predictive roles for cognitive impairments in the SCZ with MetS.Citation18 We found that the total score of ATQ was the highest in the MetS group, and that of CD-RISC was the lowest in the MetS group. The tenacity subscale score of CD-RISC and strength subscale score of CD-RISC presented the lowest in the MetS group. Moreover, ATQ had a negative correlation with the strength subscale score of CD-RISC. On the contrary, it was positively related to the negative symptom of PANSS, depression symptom of PANSS, HAMD, HAMA, and stigma. Evidence showed that waist, FGB, and TG of biochemical indexes were positively correlated with the ATQ. Conversely, HDL-C and Apo-A were negatively related to the ATQ. Specifically, the TG, waist, and HDL-C of metabolic parameters can sensitively predict the ATQ in the SCZ with MetS.Citation51 Therefore, whether patients of SCZ with MetS have dysfunctional thoughts and the severity of MetS should be identified to provide a proactive approach in managing MetS in SCZ patients.
This study has several limitations. First, due to the small sample subjects of this research, discrepancies in MetS by different drugs were difficult to compare. Therefore, in future studies, narrower inclusion criteria should be applied, focusing on specific antipsychotic drugs developed for MetS. Second, this study was a short-term cross-sectional design, limiting the extent of causal relationships between MetS and dysfunctional thoughts. In the future, longitudinal research would be sufficient for accurately assessing other potential metabolic risk factors. The causal relationship between MetS and impaired psychological function in SCZ patients with MetS should be confirmed.
In addition, smoking, life styles, and inflammation factors are all recognized pathophysiologic mechanisms for Mets with SCZ should take into account the future related research.
Conclusion
In summary, the ATQ of SCZ patients with MetS was the highest, and its resilience levels were the lowest among the three groups. In addition, the waist, FGB, and TG of the metabolic parameters were positively correlated with the ATQ in the patients of MetS group. On the contrary, HDL-C and Apo-A showed negative correlation with ATQ. Importantly, the TG, waist, HDL-C, CD-RISC, and stigma presented excellent specificity to predict ATQ; the waist showed excellent specificity to predict low resilience level. These predictors are meaningful adjustment and interventable factors for SCZ patients with MetS.
Data Sharing Statement
All data of this study can be obtained by contacting the email address of the corresponding author. The email address of the corresponding author is [email protected].
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgments
This study was supported by funding of central public welfare research institutes (grant number: GY2020G-3), Applied medicine research project of Hefei Health Committee (grant number: Hwk2020zd0016) and Applied medicine research project of Anhui Health Committee (grant number: AHWJ2021a036) and Key research and development plan projects in Anhui Province (grant number: 2022e07020002). The funding sources had no involvement in study design, collection, analysis, writing of this paper and publication.
References
- North HF, Weissleder C, Fullerton JM, Sager R, Webster MJ, Weickert CS. A schizophrenia subgroup with elevated inflammation displays reduced microglia, increased peripheral immune cell and altered neurogenesis marker gene expression in the subependymal zone. Transl Psychiatry. 2021;11(1):635. doi:10.1038/s41398-021-01742-8
- Sahpolat M, Ari M. Higher prevalence of metabolic syndrome and related factors in patients with first-episode psychosis and schizophrenia: a cross-sectional study in Turkey. Nord J Psychiatry. 2021;75(1):73–78. doi:10.1080/08039488.2020.1815080
- Penninx B, Lange SMM. Metabolic syndrome in psychiatric patients: overview, mechanisms, and implications. Dialogues Clin Neurosci. 2018;20(1):63–73. doi:10.31887/DCNS.2018.20.1/bpenninx
- Ringen PA, Engh JA, Birkenaes AB, Dieset I, Andreassen OA. Increased mortality in schizophrenia due to cardiovascular disease - a non-systematic review of epidemiology, possible causes, and interventions. Front Psychiatry. 2014;5:137. doi:10.3389/fpsyt.2014.00137
- Huang PL. A comprehensive definition for metabolic syndrome. Dis Model Mech. 2009;2(5–6):231–237. doi:10.1242/dmm.001180
- Laursen TM, Munk-Olsen T, Vestergaard M. Life expectancy and cardiovascular mortality in persons with schizophrenia. Curr Opin Psychiatry. 2012;25(2):83–88. doi:10.1097/YCO.0b013e32835035ca
- Ijaz S, Blanca B, Davies S, et al. Antipsychotic polypharmacy and metabolic syndrome in schizophrenia: a review of systematic reviews. Focus. 2020;18(4):482–492. doi:10.1176/appi.focus.18307
- Thakore JH, Mann JN, Vlahos I, Martin A, Reznek R. Increased visceral fat distribution in drug-naive and drug-free patients with schizophrenia. Int J Obes Related Metabol Disord. 2002;26(1):137–141. doi:10.1038/sj.ijo.0801840
- Lin P, Sun J, Lou X, et al. Consensus on potential biomarkers developed for use in clinical tests for schizophrenia. General Psychiatry. 2022;35(1):e100685. doi:10.1136/gpsych-2021-100685
- Sun MJ, Jang MH. Risk factors of metabolic syndrome in community-dwelling people with schizophrenia. Int J Environ Res Public Health. 2020;17(18):6700. doi:10.3390/ijerph17186700
- Sugawara N, Yasui-Furukori N, Yamazaki M, et al. Attitudes toward metabolic adverse events among patients with schizophrenia in Japan. Neuropsychiatr Dis Treat. 2016;12:427–436. doi:10.2147/NDT.S98711
- Dai J, Du X, Yin G, et al. Prevalence, demographic and clinical features of comorbid depressive symptoms in drug naive patients with schizophrenia presenting with first episode psychosis. Schizophr Res. 2018;193:182–187. doi:10.1016/j.schres.2017.06.029
- Gross J, Vancampfort D, Stubbs B, Gorczynski P, Soundy A. A narrative synthesis investigating the use and value of social support to promote physical activity among individuals with schizophrenia. Disabil Rehabil. 2016;38(2):123–150. doi:10.3109/09638288.2015.1024343
- Sun L, Xu M, Shi Y, Xu Y, Chen J, He L. Decoding psychosis: from national genome project to national brain project. General Psychiatry. 2022;35(4):e100889. doi:10.1136/gpsych-2022-100889
- Komatsu H, Ono T, Onoguchi G, Tomita H, Kakuto Y. Mediating effects of self-stigma and depression on the association between autistic symptoms and recovery in patients with schizophrenia-spectrum disorders: a cross-sectional study. BMC Psychiatry. 2021;21(1):464. doi:10.1186/s12888-021-03472-z
- Küçükkubaş N, Korkusuz F. What happens to bone mineral density, strength and body composition of ex-elite female volleyball players: a cross sectional study. Sci Sports. 2019;34(4):e259–e269. (). doi:10.1016/j.scispo.2018.11.006
- Ivezić S, Sesar MA, Mužinić L. Effects of a group psychoeducation program on self-stigma, empowerment and perceived discrimination of persons with schizophrenia. Psychiatr Danub. 2017;29(1):66–73. doi:10.24869/psyd.2017.66
- Zhang X, He C, Ju P, et al. The predictive role of aberrant metabolic parameters and negative automatic thinking on the cognitive impairments among schizophrenia patients with metabolic syndrome. Neuropsychiatr Dis Treat. 2022;18:1087–1097. doi:10.2147/NDT.S367392
- Popa CO, Rus AV, Lee WC, et al. The relation between negative automatic thoughts and psychological inflexibility in schizophrenia. J Clin Med. 2022;11(3):871. doi:10.3390/jcm11030871
- Valery KM, Prouteau A. Schizophrenia stigma in mental health professionals and associated factors: a systematic review. Psychiatry Res. 2020;290:113068. doi:10.1016/j.psychres.2020.113068
- Mizuno Y, Hofer A, Frajo-Apor B, et al. Religiosity and psychological resilience in patients with schizophrenia and bipolar disorder: an international cross-sectional study. Acta Psychiatr Scand. 2018;137(4):316–327. doi:10.1111/acps.12838
- Takeda T, Nakataki M, Ohta M, et al. Negative and positive self-thoughts predict subjective quality of life in people with schizophrenia. Neuropsychiatr Dis Treat. 2019;15:293–301. doi:10.2147/NDT.S190381
- Bozikas VP, Parlapani E, Holeva V, et al. Resilience in patients with recent diagnosis of a schizophrenia spectrum disorder. J Nerv Ment Dis. 2016;204(8):578–584. doi:10.1097/NMD.0000000000000541
- Senormanci G, Guclu O, Senormanci O. Resilience and associated factors in schizophrenia. Turk Psikiyatri Derg. 2022;33(1):1–10. doi:10.5080/u25738
- Demir A, Manolya A, Küçükkubaş N. Comparison of dynamic balance properties of hypermobility in boys. Int J Sport Exer Train Sci. 2019;5(1):15–22. doi:10.18826/useeabd.510426
- Hofer A, Mizuno Y, Frajo-Apor B, et al. Resilience, internalized stigma, self-esteem, and hopelessness among people with schizophrenia: cultural comparison in Austria and Japan. Schizophr Res. 2016;171(1–3):86–91. doi:10.1016/j.schres.2016.01.027
- First MB. Diagnostic and statistical manual of mental disorders, 5th edition, and clinical utility. J Nerv Ment Dis. 2013;201(9):727–729. doi:10.1097/NMD.0b013e3182a2168a
- Joint Committee for Developing Chinese guidelines on Prevention and Treatment of Dyslipidemia in Adults. [Chinese guidelines on prevention and treatment of dyslipidemia in adults]. Zhonghua xin xue guan bing za zhi. 2007;35(5):390–419. Chinese.
- Haig GM, Wang D, Zhao J, Othman AA, Bain EE. Efficacy and safety of the α7-nicotinic acetylcholine receptor agonist ABT-126 in the treatment of cognitive impairment associated with schizophrenia: results from a Phase 2b randomized controlled study in smokers. J Clin Psychiatry. 2018;79(3). doi:10.4088/JCP.16m11162
- Si T-M, Shu L, Dang W-M, et al. Evaluation of the reliability and validity of Chinese version of the Mini-International Neuropsychiatric Interview in patients with mental disorders. Chin Mental Health J. 2009;23:493–503.
- Wu BJ, Lan TH, Hu TM, Lee SM, Liou JY. Validation of a five-factor model of a Chinese Mandarin version of the Positive and Negative Syndrome Scale (CMV-PANSS) in a sample of 813 schizophrenia patients. Schizophr Res. 2015;169(1–3):489–490. doi:10.1016/j.schres.2015.09.011
- Li J, Oakley LD, Brown RL, Li Y, Luo Y. Properties of the early symptom measurement of post-stroke depression: concurrent criterion validity and cutoff scores. J Nurs Res. 2020;28(4):e107. doi:10.1097/jnr.0000000000000380
- Wong DF, Chau P, Kwok A, Kwan J. Cognitive-behavioral treatment groups for people with chronic physical illness in Hong Kong: reflections on a culturally attuned model. Int J Group Psychother. 2007;57(3):367–385. doi:10.1111/ppc.12994
- Corrigan PW, Mittal D, Reaves CM, et al. Mental health stigma and primary health care decisions. Psychiatry Res. 2014;218(1–2):35–38. doi:10.1016/j.psychres.2014.04.028
- Boyd JE, Adler EP, Otilingam PG, Peters T. Internalized Stigma of Mental Illness (ISMI) scale: a multinational review. Compr Psychiatry. 2014;55(1):221–231. doi:10.1016/j.comppsych.2013.06.005
- Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety. 2003;18(2):76–82. doi:10.1002/da.10113
- Mitchell AJ, Vancampfort D, Sweers K, van Winkel R, Yu W, De Hert M. Prevalence of metabolic syndrome and metabolic abnormalities in schizophrenia and related disorders--a systematic review and meta-analysis. Schizophr Bull. 2013;39(2):306–318. doi:10.1093/schbul/sbr148
- Malhotra N, Grover S, Chakrabarti S, Kulhara P. Metabolic syndrome in schizophrenia. Indian J Psychol Med. 2013;35(3):227–240. doi:10.4103/0253-7176.119471
- Sahpolat M, Ari M, Kokacya MH. Plasma apelin, visfatin and resistin levels in patients with first episode psychosis and chronic schizophrenia. Clin Psychopharmacol Neurosci. 2020;18(1):109. doi:10.9758/cpn.2020.18.1.109
- Yaprak Y, Küçükkubaş N. Gender-related differences on physical fitness parameters after core training exercises: a comparative study. Progress Nutr. 2020;22(3):e2020028.
- Küçükkubaş N, Günay A, Löklüoğlu B, Kakil B. Relationship between body composition, vertical jump, 30 M sprint, static strength and anaerobic power for athletes. Int J Sport Exer Train Sci. 2019;5(2):68–78. doi:10.18826/useeabd.517037
- Malan-Muller S, Kilian S, van den Heuvel LL, et al. A systematic review of genetic variants associated with metabolic syndrome in patients with schizophrenia. Schizophr Res. 2016;170(1):1–17. doi:10.1016/j.schres.2015.11.011
- Carney R, Cotter J, Bradshaw T, Firth J, Yung AR. Cardiometabolic risk factors in young people at ultra-high risk for psychosis: a systematic review and meta-analysis. Schizophr Res. 2016;170(2–3):290–300. doi:10.1016/j.schres.2016.01.010
- Emul M, Kalelioglu T. Etiology of cardiovascular disease in patients with schizophrenia: current perspectives. Neuropsychiatr Dis Treat. 2015;11:2493–2503. doi:10.2147/NDT.S50006
- Liu J, Fu L. Metabolic syndrome in patients with schizophrenia: why should we care. Medicine. 2022;101(32):e29775. doi:10.1097/MD.0000000000029775
- Hasnain M, Fredrickson SK, Vieweg WV, Pandurangi AK. Metabolic syndrome associated with schizophrenia and atypical antipsychotics. Curr Diab Rep. 2010;10(3):209–216. doi:10.1007/s11892-010-0112-8
- Brohan E, Slade M, Clement S, Thornicroft G. Experiences of mental illness stigma, prejudice and discrimination: a review of measures. BMC Health Serv Res. 2010;10:80. doi:10.1186/1472-6963-10-80
- Mosanya TJ, Adelufosi AO, Adebowale OT, Ogunwale A, Adebayo OK. Self-stigma, quality of life and schizophrenia: an outpatient clinic survey in Nigeria. Int J Soc Psychiatry. 2014;60(4):377–386. doi:10.1177/0020764013491738
- Sevi O, Eylen Özyurt B. OTOMATİK DÜŞÜNCELER ÖLÇEĞİ’NİN ŞİZOFRENİ HASTALARININ OLUMSUZ OTOMATİK DÜŞÜNCELERİNİ DEĞERLENDİRMEDE GEÇERLİK VE GÜVENİRLİĞİNE DAİR BİR ÖN ÇALIŞMA [A pilot study of the reliability and validity of automatic thoughts questionnaire in assesment of schizophphrenic patient’s automatic thoughts]. Anatol J Clin Invest. 2013;7:1–9.
- Sahin AO, Ozer D, Bulut R, Sahin F. Investigation of the relationship between the negative automatic thoughts of patients with schizophrenia and their levels of social functionality. Perspect Psychiatr Care. 2022;58(4):1819–1825.
- Sahpolat M, Ayar D, Ari M, Karaman MA. Elevated monocyte to high-density lipoprotein ratios as an inflammation markers for schizophrenia patients. Clin Psychopharmacol Neurosci. 2021;19(1):112. doi:10.9758/cpn.2021.19.1.112