Abstract
Background
Nonadherence is a well-known problem among schizophrenia patients, among whom relapse is fivefold more likely, adversely affecting health, employment, and social functioning. The Spanish Adherencia Terapéutica en la Esquizofrenia (ADHES) survey was developed to determine the scope and causes of medication nonadherence in schizophrenia.
Methods
The 20-question ADHES survey was distributed to 19,370 psychiatrists in 13 Asia–Pacific countries in January–April 2012, to ascertain psychiatrists’ perceptions of antipsychotic medication adherence levels among their schizophrenia patients, reasons for partial/nonadherence, their preferred methods of assessing adherence, and strategies to improve adherence. Responses are reported as mean and range across countries.
Results
Four thousand, six hundred sixty one psychiatrists (24% of recipients) completed the survey (highest contributors: People’s Republic of China, 1854; India, 1616). Psychiatrists perceived that 56% (range, 30%–71%) of schizophrenia patients were non- or partially adherent to medication. Patients discontinue medication primarily due to lack of insight into their condition (mean, 37%; 1%–65%) and because patients consider medication unnecessary when feeling better (mean, 27%; 15%–68%). Over half of psychiatrists (mean, 55%; 42%–99%) assess medication adherence at every visit, almost exclusively (81%) by asking their patients, versus quantitative measures. One in three psychiatrists expressed their preference to switch to or add a long-acting antipsychotic to improve adherence (15%–82%).
Conclusions
The substantial prevalence of partial/nonadherence to medication demonstrates that more proactive management of patients with schizophrenia is needed to improve adherence and thereby treatment outcomes.
Registration
Registration of this study was not required.
Background
Nonadherence to antipsychotic medication is one of the major challenges for clinicians treating patients with schizophrenia,Citation1 and on the order of exercise or weight reduction with regard to trouble in achieving adherence adequate enough to advance beneficial effects.Citation2 The prevalence of medication nonadherence in schizophrenia is consistent with that of other chronic illnesses (eg, hypertension, asthma).Citation3
In a review of 39 studies published between 1981 and 2002, Lacro et al noted medication nonadherence rates ranging from 4% to 72% (median, 40%) among patients with schizophrenia, depending on how adherence was defined and measured, the patient population studied (eg, stable vs recently hospitalized outpatients), and the duration and type of evaluation (eg, retrospective, cross-sectional, observational).Citation4 The 3-year prospective, observational Worldwide-Schizophrenia Outpatient Health Outcomes (W-SOHO) trial and the National Institute of Mental Health-sponsored Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) trial provide further evidence of how nonadherence can play out in clinical practice. At the baseline of the W-SOHO study, which recruited 17,384 schizophrenia patients from 37 countries (regions: East Asia, n = 1,223; Europe, n = 12,254; Latin America, n = 2,566; North Africa/Middle East, n = 1,341), 15% of investigators cited incomplete medication adherence as the reason for initiating or changing medication at study entry (range, 10% in East Asia to 21% in Latin America).Citation5 In the sentinel CATIE trial of patients with chronic schizophrenia, the majority discontinued their assigned antipsychotic agent (a surrogate measure of nonadherence): In Phase I of the study, 74% of 1,460 patients discontinued before completing the 18 months of assigned treatment with an antipsychotic agent.Citation6 In Phase II of CATIE, 69% of 90 patients (efficacy pathway) and 74% of 333 patients (tolerability pathway) discontinued treatment before completion of the study; median treatment duration was 4 and 5 months in the respective pathways.Citation7,Citation8 Taken together, these findings underscore how challenging it is for schizophrenia patients to remain on antipsychotic treatment over a sustained period of time.
The implications of nonadherence for schizophrenia management are far-reaching.Citation9 Partial/nonadherence to medication has a major impact on the course of illness and treatment outcomes, resulting in persistence of symptoms, approximately fivefold increased risk of relapse (as compared with patients who continue taking their medication), occupational and social dysfunction, increased rate and duration of hospitalization, and increased risk of attempted suicide.Citation10–Citation13 In addition, relapse begets relapse, with illness becoming resistant to treatment and previous gains increasingly more difficult to achieve.Citation14,Citation15 Nonadherence to medication also impacts cost of care, increasing outpatient service costs for schizophrenia by almost threefold.Citation16
The Spanish Adherencia Terapéutica en la Esquizofrenia (ADHES) program (translated as: therapeutic adherence in schizophrenia) commenced in 2003, aimed at raising awareness of the problem of partial/nonadherence to medication in the treatment of mental illness. As a component of the ADHES program, a survey was developed and first conducted in Spain,Citation17 and then in the whole of Europe, the Middle East, and Africa (EMEA),Citation18 appraising psychiatrists’ opinions about the scope and causes of partial or nonadherence to antipsychotic agents among their schizophrenia patients. Using the ADHES survey, the objectives of the study reported here were to determine perceptions of Asia–Pacific (APAC) psychiatrists regarding antipsychotic medication adherence levels among their schizophrenia patients, reasons for their patients’ partial/nonadherence, and their preferred methods of assessing adherence.
Methods
The ADHES survey has been described in detail elsewhere.Citation17 In brief, the ADHES survey consists of 20 questions relating to the demographic characteristics and practice settings of participating psychiatrists and to their perceptions of different factors that affect schizophrenia patients’ partial/nonadherence to antipsychotic medication. The original survey was translated from Spanish to English and then from English into local languages; the survey was then checked for accuracy by native speakers and by back-translation to English before being administered in APAC.
Surveys were handed out at a national conference in India (January 2012) at which the majority of Indian psychiatrists were in attendance. In all other APAC countries, extensive lists of psychiatrists by country were used to disseminate the survey widely during January–April 2012, either by mail (Australia) or via Janssen-Cilag representatives. Psychiatrists received the ADHES survey in a package that also contained a prepaid envelope and a letter explaining the objectives of the survey.
Data collection and analysis
Respondents completed the survey under anonymity; patient-specific information was not collected. No effort was made to follow-up with nonresponding survey recipients. A research agency (Millward Brown, Warwick, UK) summarized survey response data descriptively. Statistical testing was not performed.
In recording their responses, psychiatrists indicated the adherence status of the schizophrenia patients they had seen in the preceding month, by estimating the percentage of patients in each of the following categories: adherent (took ≥90% of prescribed doses), partially adherent (took ≥30 to <90% of prescribed doses), or nonadherent (took <30% of prescribed doses).Citation18 The arithmetic mean of the values entered for each of the above categories (ie, percentages of patients who were adherent, partially adherent, or nonadherent to treatment) was calculated based on all respondents who answered the question.
Regarding patients’ views and behaviors contributing to partial or nonadherence, psychiatrists were instructed to estimate some responses based on the percentage of patients falling into each of three groupings (ie, <20%, 20%–50%, and >50% of patients). The mean percent of patients was predefined as: <20% of patients, mean score value = 10%; between 20% and 50% of patients, mean score value = 35%; and, >50% of patients, mean score value = 75%.
For all questions except those assessing adherence (as noted above), the raw data were converted to percentages that were based on all respondents who were asked the question. If there was no response to the question then that respondent was included in the base, but defaulted into the ‘not answered’ category. The data were not weighted.
Results
The ADHES survey was distributed to 19,370 psychiatrists across 13 countries in the APAC region. A total of 4,661 (24%) psychiatrists completed the survey. The highest number of respondents practiced in the People’s Republic of China and India. The countries in which respondents were in practice (and number of respondents, in decreasing order) were: People’s Republic of China (1,854), India (1,616), Australia (406), Taiwan (195), Vietnam (107), New Zealand (99), Indonesia (97), Hong Kong (77), Philippines (71), Thailand (68), Singapore (42), Malaysia (17), and Korea (12). The respondents were 60% male; 15% aged ≤30 years, 60% aged 31–50 years, 16% aged 51–60 years, and 7% aged ≥61 years (2% data missing); and, 76% in clinical (vs academic) practice (). Over half (58%) treat their patients, at least in part, in an inpatient setting.
Table 1 Summary of survey respondents (n = 4,661)
APAC psychiatrists estimated that 56% of patients with schizophrenia are partially or nonadherent with their anti-psychotic medication (), with variations seen within APAC (lowest partial/nonadherence in Vietnam [30%], Australia, and Thailand [each 51%], and highest in Singapore and Malaysia [each 71%]).
Figure 1 Proportion of schizophrenia patients perceived to be partially or nonadherent to their antipsychotic medication.*
Abbreviations: AU, Australia; CN, People’s Republic of China; HK, Hong Kong; IN, India; ID, Indonesia; KR, Korea; MY, Malaysia; NZ, New Zealand; PH, Philippines; SG, Singapore; TW, Taiwan; TH, Thailand; VN, Vietnam; APAC, Asia–Pacific.

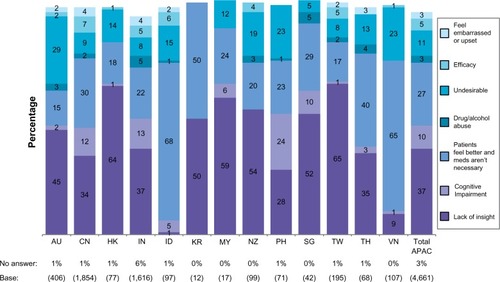
Psychiatrists opined that their schizophrenia patients discontinue antipsychotic medication primarily due to lack of insight into their condition (mean across APAC, 37%; highest in Hong Kong [64%] and Taiwan [65%]) and because patients consider medication unnecessary when feeling better (mean across APAC, 27%; highest in Indonesia [68%] and Vietnam [65%]) (). Other less common reasons for discontinuation, with substantial variability across APAC countries, were cognitive impairment (highest in the Philippines [24%], India [13%], and the People’s Republic of China [12%]) and undesirable side effects (highest in Australia [29%]).
Figure 2 Psychiatrists’ views on the most important reason for their schizophrenia patients discontinuing antipsychotic medication.*
Abbreviations: AU, Australia; CN, People’s Republic of China; HK, Hong Kong; IN, India; ID, Indonesia; KR, Korea; MY, Malaysia; NZ, New Zealand; PH, Philippines; SG, Singapore; TW, Taiwan; TH, Thailand; VN, Vietnam; APAC, Asia–Pacific.
According to the ADHES survey respondents, only a minority (32%) of patients are able to attribute clinical deterioration to medication nonadherence (lowest in Vietnam [14%] and Korea [18%] and highest in Indonesia [41%]). In the caregivers’ view, fewer than 4 in 10 patients (37%) understand there is a risk of relapse if they do not take their medication regularly (lowest in Vietnam [18%] and highest in Australia [42%], Taiwan [48%], and Korea [55%]).
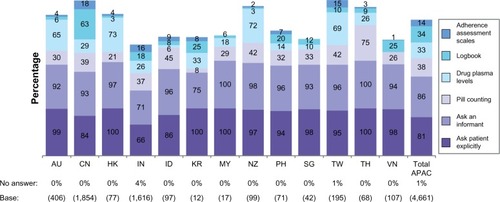
Across APAC, over half of psychiatrists (mean of 55%; lowest in India [42%] and highest [≥87%] in Indonesia, Hong Kong, Malaysia, and Vietnam) reported that they assess medication adherence at every visit (). The majority of psychiatrists assess adherence almost exclusively by asking their patients (81%) or a close informant (86%), versus using objective measures (), which are used most often in Thailand (75% count pills), Hong Kong, Taiwan, Australia (drug plasma levels measured in 73%, 69%, and 65%, respectively), and the People’s Republic of China (63% use logbook and 18% use adherence scale).
Figure 3 Psychiatrists’ views on the frequency with which they assess adherence in their patients.*
Abbreviations: AU, Australia; CN, People’s Republic of China; HK, Hong Kong; IN, India; ID, Indonesia; KR, Korea; MY, Malaysia; NZ, New Zealand; PH, Philippines; SG, Singapore; TW, Taiwan; TH, Thailand; VN, Vietnam; APAC, Asia–Pacific.
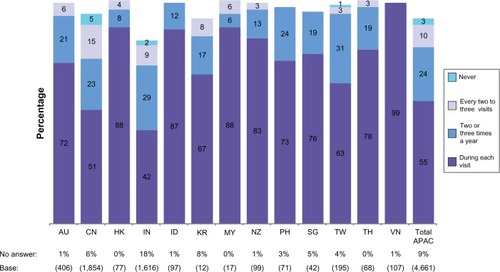
Figure 4 Psychiatrists’ views on the approaches they use to assess adherence.*
Abbreviations: AU, Australia; CN, People’s Republic of China; HK, Hong Kong; IN, India; ID, Indonesia; KR, Korea; MY, Malaysia; NZ, New Zealand; PH, Philippines; SG, Singapore; TW, Taiwan; TH, Thailand; VN, Vietnam; APAC, Asia–Pacific.
Psychiatrists reported that 42% of their patients, on average, need reminding by family members/carers to take their medication as prescribed (range, 36%–37% in Singapore and India to 55%–58% in Taiwan, Indonesia, Thailand, and Hong Kong). Fewer of their patients (36%; range, 30%–31% in Singapore and India, to 48%–59% in Malaysia and Korea) rely on a nurse, psychiatrist, or professional carer to do so.
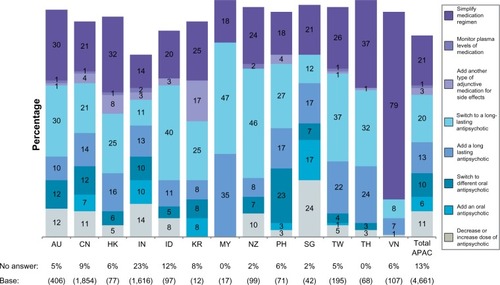
The strategies considered to manage nonadherence reflect a change or simplification in the current treatment regimen. Among all treatment modifications considered, one-third of APAC psychiatrists (lowest in Vietnam [15%] and India [24%] and highest [51%–82%] in Indonesia, New Zealand, Thailand, Taiwan, and Malaysia) favor switching to or adding a long-acting antipsychotic as their preferred treatment option for addressing adherence problems ().
Figure 5 APAC psychiatrists’ views on the preferred pharmacological approach they use to address an adherence problem in their patients.*
Abbreviations: AU, Australia; CN, People’s Republic of China; HK, Hong Kong; IN, India; ID, Indonesia; KR, Korea; MY, Malaysia; NZ, New Zealand; PH, Philippines; SG, Singapore; TW, Taiwan; TH, Thailand; VN, Vietnam; APAC, Asia–Pacific.
Discussion
The ADHES schizophrenia survey was conducted in APAC to gain insights into the perceptions of psychiatrists in the region regarding the scope and causes of antipsychotic medication nonadherence among their schizophrenia patients as well as the methods of assessing adherence, and preferred strategies to improve adherence. By using a survey administered in the EMEA previously, similarities and differences not only among APAC countries, but also between APAC and EMEA can be identified, thereby promoting a cross-cultural understanding of antipsychotic nonadherence in schizophrenia.
We report on a large study sample of 4,661 psychiatrists practicing in 13 countries within the APAC region. The ADHES response rate of 24% in the APAC was twofold higher than that in the EMEA (12%).Citation18 Although eight of the APAC countries had fewer than 100 respondents each, they were generally well represented in the survey, as reflected by the proportion that respondents comprised to the total number of practicing psychiatrists per country (eg, Singapore [31%], Hong Kong [25%], New Zealand [24%], Thailand [23%], and Philippines [20%]).Citation19
APAC psychiatrists considered that over half (56%) of patients with schizophrenia are partially or nonadherent with their antipsychotic medication. Based on prevalence figures from the World Health Organization,Citation20 this represents approximately 7.9 million affected patients. Overall, similar levels of adherence were reported by psychiatrists across APAC and EMEA, where 53% of patients were reported partially or nonadherent.Citation18 Within APAC, the lowest rate of nonadherence was reported in Vietnam (30%), which may not be representative of the other countries. Most Vietnamese survey respondents (88%) reported following and treating schizophrenia patients in a hospital, where they can achieve good adherence. Their view on adherence among other patients is limited by the fact that these patients are managed by local mental health care centers, therefore the original treating physicians are not able to monitor and follow-up on their patient’s treatment.
APAC psychiatrists cited a lack of insight as the main reason for patient partial/nonadherence, a perspective similarly held by EMEA psychiatrists. To the extent that lack of insight is static, trait-like, and unmodifiable by patient education, it follows that cooperation may need to be bypassed, for instance with long-acting injectable antipsychotics. Cognitive impairment was a more common reason for nonadherence in APAC than reported in EMEA. In the opinion of ADHES survey respondents, a minority of schizophrenia patients in APAC (32%) and EMEA (32%Citation21) relate clinical deterioration to antipsychotic nonadherence.
APAC psychiatrists noted that approximately a third of their patients need help from caregivers (family member or professional), placing a burden on them to help patients adhere to their treatment plan. The perceived caregiver burden in APAC was lower than that reported in the EMEACitation18), due in large part to low rates of caregiver burden reported by respondents from India. In APAC countries, more so than in EMEA and other developed regions, schizophrenia patients tend to live with and are supported by an extended family system (rather than in residential facilities), due not only to cultural influences, but also the relative lack of a social welfare system for such patients.Citation22
Our observations confirm those of others who implicate patients’ lack of insight as the most important among factors associated with poor medication adherence in schizophrenia patients.Citation4,Citation13 Forming the basis for 2009 Consensus Practice GuidelinesCitation13 for assessing and improving adherence, 41 leading experts in schizophrenia management completed a survey in which they answered questions about the definition and extent of nonadherence, risk factors and assessment methods for nonadherence, and interventions for specific nonadherence problems. The experts ranked the following factors (in descending order of importance) as potential contributors to adherence problems in schizophrenia: poor insight into having an illness; distress associated with persistent side effects (or fear of potential side effects); lack of/partial efficacy with continued symptoms; belief that medications are no longer needed; ongoing substance use problems; cognitive deficits; lack of social support to help with medication-taking; practical problems (eg, transportation, financial); difficulty building therapeutic alliance (with health care providers, caregivers); lack of daily routines; complexity of treatment regimen; significant others ambivalent/opposed to medication; stigma associated with mental illness and medication; and, negative attitudes towards medications in general.
Compared with their EMEA counterparts (76%), APAC psychiatrists assess adherence levels less frequently, with 55% doing so regularly or during every visit. The lowest adherence assessment frequency was reported in the People’s Republic of China (51%) and India (42%). Furthermore, APAC psychiatrists reported assessing medication adherence with objective measures less often than EMEA psychiatrists who had previously responded to the ADHES survey.Citation18 Basing adherence on patient interview can be especially unreliable in countries where patients have negative beliefs about psychiatric conditions or embarrassment about taking antipsychotic medication ().
One out of every three APAC psychiatrists favor switching to or adding a long-acting antipsychotic as their preferred treatment option for addressing adherence problems, compared to three out of every five (62%) EMEA survey respondents.Citation18 Treatment of schizophrenia patients with a long-acting injectable antipsychotic (vs oral) agent has been shown to decrease relapse and hospitalization rates in many, but not all, studies.Citation23,Citation24 The preference of Australian psychiatrists for a long-acting agent (40%), as well as their responses to other questions (eg, higher perceived adherence level, undesirable side effects as a key driver for nonadherence) indicates that they are more aligned with psychiatrists in the EMEA than other APAC countries. This may be a reflection of similarities in its health care system, earlier introduction of long-acting antipsychotic agents, and community-based treatment programs.
Our findings on the prevalence of antipsychotic nonadherence are limited by the fact that its assessment by physicians’ clinical judgment oftentimes results in underestimated rates, as compared with an objective tool.Citation25 A single method for identifying survey respondents was not utilized: some received the survey by mail and others either during a conference or from a representative of the survey’s sponsor. Thus, a social desirability bias cannot be ruled out. Furthermore, it is unknown whether the survey sample is representative of all psychiatrists in APAC and whether their responses to the ADHES reflect those of the broad population of their colleagues in the region. Nevertheless, comparisons among APAC countries or between APAC and EMEA on the same survey items remain of interest.
In summary, the substantial prevalence of partial/nonadherence to antipsychotic medication in APAC, as reported by psychiatrists practicing in the region, demonstrates that more proactive management of patients with schizophrenia is needed to improve adherence and thereby treatment outcomes. To further our findings, future trials could examine other factors affecting adherence (eg, cognitive impairment, disease severity, motivational deficits, stigma, environmental stressors, lack of social support, substance abuse, cultural and religious beliefs, treatment-related side effects, poor therapeutic alliance, access to treatment, cost of medication) and other measures of adherence (eg, prolactin). We also propose longitudinal, multi-country study of patients’ beliefs, as compared to those of their health care providers.
Contributions
JMO conceived the original ADHES survey. JMO, MT, JK, MYZ, HYZ, and FZ were members of this study’s Steering Committee, which ratified the survey and designed the conduction of the study. All authors had full access to the data, contributed to data interpretation and the development of the manuscript, and read and approved the final manuscript in accordance with ICMJE criteria.
Acknowledgments
Sandra Norris, Pharm.D. provided writing assistance and Wendy P Battisti, Ph.D. (Janssen Research and Development, LLC) provided additional editorial assistance. The authors thank the survey respondents for their contributions to this data.
Disclosure
Funded by Janssen Asia Pacific, a division of Johnson and Johnson Pte. Ltd, Singapore. Registration of this study was not required. Dr Fan Zhang is an employee of Xian Janssen Pharmaceutical, Beijing, People’s Republic of China. Other authors report no conflicts of interest.
References
- KaneJMReview of treatments that can ameliorate nonadherence in patients with schizophreniaJ Clin Psychiatry200667Suppl 591416822091
- KeithSJKaneJMPartial compliance and patient consequences in schizophrenia: our patients can do betterJ Clin Psychiatry200364111308131514658944
- LlorcaPMPartial compliance in schizophrenia and the impact on patient outcomesPsychiatr Res20081612235247
- LacroJPDunnLBDolderCRLeckbandSGJesteDVPrevalence of and risk factors for medication nonadherence in patients with schizophrenia: a comprehensive review of recent literatureJ Clin Psychiatry2002631089290912416599
- KaragianisJNovickDPecenakJWorldwide-Schizophrenia Outpatient Health Outcomes (W-SOHO): baseline characteristics of pan-regional observational data from more than 17,000 patientsInt J Clin Pract200963111578158819780867
- LiebermanJAStroupTSMcEvoyJPClinical Antipsychotic Trials of Intervention Effectiveness (CATIE) InvestigatorsEffectiveness of antipsychotic drugs in patients with chronic schizophreniaN Engl J Med2005353121209122316172203
- StroupTSLiebermanJAMcEvoyJPCATIE InvestigatorsEffectiveness of olanzapine, quetiapine, risperidone, and ziprasidone in patients with chronic schizophrenia following discontinuation of a previous atypical antipsychoticAm J Psychiatry2006163461162216585435
- McEvoyJPLiebermanJAStroupTSCATIE InvestigatorsEffectiveness of clozapine versus olanzapine, quetiapine, and risperidone in patients with chronic schizophrenia who did not respond to prior atypical antipsychotic treatmentAm J Psychiatry2006163460061016585434
- MasandPSRocaMTurnerMSKaneJMPartial adherence to antipsychotic medication impacts the course of illness in patients with schizophrenia: a reviewPrim Care Companion J Clin Psychiatry200911414715419750066
- McEvoyJPHoweACHogartyGEDifferences in the nature of relapse and subsequent inpatient course between medication-compliant and noncompliant schizophrenic patientsJ Nerv Ment Dis198417274124166144721
- NovickDHaroJMSuarezDPerezVDittmannRWHaddadPMPredictors and clinical consequences of non-adherence with anti-psychotic medication in the outpatient treatment of schizophreniaPsychiatry Res20101762–310911320185182
- RobinsonDWoernerMGAlvirJMPredictors of relapse following response from a first episode of schizophrenia or schizoaffective disorderArch Gen Psychiatry199956324124710078501
- VelliganDIWeidenPJSajatovicMExpert Consensus Panel on Adherence Problems in Serious and Persistent Mental Illness CollaboratorsThe expert consensus guideline series: adherence problems in patients with serious and persistent mental illnessJ Clin Psychiatry200970Suppl 414619686636
- KaneJMTreatment adherence and long-term outcomesCNS Spectrums20071210 Suppl 17212617934386
- LiebermanJAKoreenARChakosMFactors influencing treatment response and outcome of first-episode schizophrenia: implications for understanding the pathophysiology of schizophreniaJ Clin Psychiatry199657Suppl 9598823344
- KnappMKingDPugnerKLapuertaPNon-adherence to antipsychotic medication regimens: associations with resource use and costsBr J Psychiatry200418450951615172945
- GinerJCañasFOlivaresJMTreatment adherence in schizophrenia. A comparison between patient’s, relative’s and psychiatrist’s opinions. [Article in Spanish]Actas Esp Psiquiatr200634638639217117335
- OlivaresJMAlptekinKAzorinJMPsychiatrists’ awareness of adherence to antipsychotic medication in patients with schizophrenia: results from a survey conducted across Europe, the Middle East and AfricaPatient Prefer Adherence2013712113223390361
- World Health OrganizationMental Health Atlas-2011 country profiles Available at: http://www.who.int/mental_health/evidence/atlas/profiles/en/index.htmlAccessed June 19, 2013
- World Health OrganizationThe global burden of disease: 2004 updateGeneva, SwitzerlandWorld Health Organization200432
- NaberDAlptekinKAzorinJMThe EMEA ADHES survey in schizophrenia: psychiatrists’ perceptions of the extent of assessment and management of partial and non-adherence to medication [P03-277]Eur Psychiatry201126S11446
- RazaliSMPrevention of relapse and interventions for enhancing medication adherence in schizophrenia: An East Asian perspectiveAsia-Pacific Psychiatry2010226876
- OlivaresJMRodriguez-MoralesADielsJLong-term outcomes in patients with schizophrenia treated with risperidone long-acting injection or oral antipsychotics in Spain: Results from the electronic Schizophrenia Treatment Adherence Registry (e-STAR)Eur Psychiatry200924528729619195847
- ZhornitskySStipEOral versus long-acting injectable antipsychotics in the treatment of schizophrenia and special populations at risk for treatment nonadherence: a systematic reviewSchizophr Res Treatment20122012407171 Epub February 15, 201222966436
- ByerlyMFisherRWhatleyKA comparison of electronic monitoring vs clinician rating of antipsychotic adherence in outpatients with schizophreniaPsychiatry Res20051332–312913315740989