Abstract
Background
A growing, but conflicting body of literature suggests altered empathic abilities in subjects with anorexia nervosa-restricting type (AN-R). This study aims to characterize the cognitive and affective empathic profiles of adolescents with purely AN-R.
Methods
As part of a standardized clinical and research protocol, the Interpersonal Reactivity Index (IRI), a valid and reliable self-reported instrument to measure empathy, was administered to 32 female adolescents with AN-R and in 41 healthy controls (HC) comparisons, matched for age and gender. Correlational analyses were performed to evaluate the links between empathy scores and psychopathological measures.
Results
Patients scored significantly lower than HC on cognitive empathy (CE), while they did not differ from controls on affective empathy (AE). The deficit in CE was not related to either disease severity nor was it related to associated psychopathology.
Conclusion
These results, albeit preliminary, suggest that a dysfunctional pattern of CE capacity may be a stable trait of AN-R that should be taken into account not only for the clinical management, but also in preventive and therapeutic intervention.
Introduction
Anorexia nervosa (AN) is a serious psychiatric disorder affecting mainly young females and it is associated with poor long-term outcome.Citation1 According to the current version of the Diagnostic and Statistical Manual of Mental Disorders, the essential features of AN are a significantly low body weight for the developmental stage of the subject, an intense fear of gaining weight or persistent behavior that interferes with weight gain, and disturbance in experiencing body weight and shape.Citation2 Two different subtypes of the disorders are specified, the restricting type (AN-R), in which weight loss is accomplished exclusively through a massive reduction in food intake and excessive exercise over the previous 3 months, and the binge-eating/purging type (AN-BE), in which binge eating is usually associated with purging through self-induced vomiting or misuse of laxatives and diuretics or enemas during the previous 3 months.Citation2 Despite neither diagnostic criteria nor reports on common associated psychopathology describe empathic alterations in AN, clinical observation as well as some research data suggests that empathic difficulty could be part of the AN phenotype.Citation3 Empathy is a complex multidimensional construct and a core component of social cognition. A schematic distinction of empathy includes: a) sharing the emotional states of others (affective empathy [AE]), and b) understanding the perspective of another person (cognitive empathy [CE]).Citation4 A phenomenon partially overlapping with empathy is theory of mind (ToM). ToM consists of the ability to make inferences regarding others’ emotions (affective or emotional ToM) or beliefs and motivations (cognitive ToM); while the latter is strongly similar to CE, the former may be related to both affective and cognitive empathy.Citation5
A considerable subgroup of AN subjects with associated empathy disorders was revealed in a Gillberg et al study:Citation6 the authors described these patients as impaired in understanding the cognitive and emotional perspectives of other people and with a clinical picture suggestive of an autism spectrum disorder (ASD). Subsequent reports confirmed autistic traits as predictiveCitation1 or comorbid factors in AN patients:Citation7 this has led some authors to consider AN as a version of ASD.Citation8 However, an impaired empathic profile in AN is not a consistent finding; for example, a self-report evaluation of empathic abilities failed to detect statistically significant differences between AN patients and healthy controls.Citation9 On the other hand, Tchan-turia et alCitation10 first explored cognitive ToM in women with AN, revealing a clear impairment in a subgroup of these patients of which the study lacked the power to demonstrate statistically. Later reports showed abnormalities in both affective and cognitive ToM,Citation11 in emotional ToM only,Citation12 or no relevant differences between adult patients with AN and controls in emotional ToM.Citation13 Finally, a recent investigation that evaluated, among other things, the social perception domain through a multidomain neuropsychological battery designed specifically for children and adolescents, reported an absence of deficit in this area in AN-R patients.Citation14
The assessment of empathic response can be performed through physiological measurements (eg, heart rate or skin conductance registration), indirect indices (facial, gestural, bodily, and vocal expression recognition), and psychological evaluation (test administration, reports from significant others, and self-reported questionnaires). Among self-reported psychological tests aimed at evaluating empathic functioning, the Interpersonal Reactivity Index (IRI) represents one of the most widely used and comprehensive instruments.Citation4 In fact, different abnormalities in CE and AE levels, assessed through the IRI, have been reported in a variety of psychiatric conditions, including psychopathy,Citation15 borderline personality disorder,Citation16 Asperger syndrome,Citation17 schizophrenia,Citation18 major depressive disorder,Citation19 bipolar disorder,Citation20 and patients with alcohol dependence.Citation21 To our knowledge, no study has evaluated empathy abnormalities in adolescents with AN-R.
In this study, we analyzed the empathic abilities of a homogeneous group of adolescents with AN-R. As AN-R subjects are characterized by starvation and associated internalizing psychopathology that can impact cognitive abilities,Citation22 we specifically investigated the empathic profile controlling for disease severity and associated psychopathology.
Materials and methods
Participants
Thirty-two adolescent females (mean age ± standard deviation [SD] =14.78 ± 1.75 years; range =11.00–17.33 years) with AN-R were consecutively recruited from the inpatient eating disorders unit at the IRCCS Stella Maris Foundation. These adolescents (all between 11 and 18 years) were characterized by restrictive behaviors and weight loss purely by dieting without binge eating or purging behaviors. They fulfilled the criteria for the diagnosis of AN-R according to the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV).Citation23 Patients with psychotic symptoms, intelligence quotient [IQ] below 80, medical pathology not correlated with the eating disorder, current or history of substance abuse, and significant intrinsic instability requiring constant medical care supervision (such as severe bradycardia, dehydration, or electrolyte imbalance) were excluded. The mean body mass index was 15.07 ± 1.54 kg/m2 and the mean duration of illness was 19.56 ± 18.38 months. Twenty-seven patients (84.38%) fulfilled the criteria for an Axis I anxiety and/or mood disorder (assessed through the Italian version of the Kiddie-Sads-Present and Lifetime Version [K-SADS-PL])Citation24 and 3 of these 27 patients also met the criteria for an Axis II Obsessive-Compulsive Personality Disorder (evaluated by the Structured Clinical Interview for DSM-IV Axis II Personality Disorders).Citation25 Twelve patients (37.5%) received psychopharmacological treatment with selective serotonin reuptake inhibitors and/or atypical antipsychotics and/or mood modulators, while the remaining 20 subjects were medication-naïve.
The AN-R clinical sample was compared to a healthy control group (HC) composed of 41 healthy female adolescents recruited from students (mean age =14.02 ± 1.69 years; range =11.08–17.16 years) of a middle and a high school in the metropolitan area of Pisa. All control subjects attended regular classes and schools without a support teacher.
Measures
The following established measures, which were part of a larger suite of tests, were administered for this study.
Assessment of empathic abilities
The Italian versionCitation26 of the IRICitation4 was used to evaluate empathic abilities. The IRI is a 28-item self-reported questionnaire that allows a multi-dimensional assessment of empathy, which can be measured by two cognitive subscales (perspective taking [PT]; fantasy [FS]) and two affective subscales (empathic concern [EC]; personal distress [PD]). Participants respond to each item using a 5-point Likert scale ranging from −2 “does not describe me well” to +2 “does describe me well”. Therefore the scores of each subscale range between −14 and +14 points where higher scores indicate more empathic abilities.
Assessment of eating disorder severity
To address eating disorder severity, the following measures were considered: 1) the Body Mass Index (BMI) calculated by dividing body weight in kilograms by height in meters squared (kg/m2); 2) the Eating Attitudes Test (EAT-26),Citation27 a 26-item self-reported questionnaire of disordered eating patterns. The total score ranges from 0 to 78; a higher score reflects a greater degree of eating pathology, with a score over 20 indicating a possible eating problem; 3) disease duration, defined as the time interval between the onset of the first eating disorder symptoms and the administration of the tests.
Assessment of possible psychopathological traits associated to the eating disorder
To address psychopathological traits associated with the eating disorder, two questionnaires were used: 1) the Child Behavior Checklist (CBCL 6–18),Citation28 a 118 item parent-reported measure designed to record the problem behaviors as well as the competencies of children or adolescents. Each item describes a specific behavior and the parent is asked to rate its frequency on a 3-point Likert scale. The scoring gives a summary profile including internalizing (INT), external-izing (EXT), and total problems (TP), and a syndrome profile (withdrawn, anxious/depressed, somatic complaints, social problems, thought problems, attention problems, delinquent behavior, and aggressive behavior); 2) the Youth Self Report (YSR 11–18), an118 items self-reported questionnaire for adolescents from 11 to 18 years old.Citation28 The YSR provides a summary profile and a syndrome profile paralleling those of the CBCL 6–18.
Procedure
The study was carried out according to the standards for good ethical practice of the IRCCS Stella Maris Foundation, and was approved by the educational board of each school of the HC group. Written informed consent from a parent or guardian of each patient was obtained. Patients and their parents completed all the tests (IRI, EAT-26, CBCL 6–18, and YSR 11–18) during the first days of the clinical assessment. HC, in addition to the IRI, completed the EAT-26 and the YSR 11–18, in order to rule out subjects with eating problems and/or Axis I psychopathology, respectively. In fact, the YSR has been found to show a significant correlation with clinical DSM-IV diagnoses.Citation28–Citation30 Thus, subjects with an EAT-26 score >20, and/or a score >60 on INT and/or EXT and/or TP at the YSR, were excluded from the study. HC data were collected by a physician resident in Child and Adolescent Psychiatry (PF) during school hours and informed consent was obtained from participants and their parents through the head teacher’s office at each school.
Data analysis
A Student’s t-test was used to compare differences in EAT-26, YSR, and IRI mean scores between AN-R and HC groups; multivariate analysis of variance (ANOVA) with EAT-26 and with INT, EXT, and TP mean scores of the YSR as a covariate was used to identify IRI scales discriminating between AN-R and HC groups; Spearman correlations were adopted to assess the relationship between IRI scales and 1) associated psychopathology (CBCL), and 2) eating disorder severity (BMI and disease duration), respectively.
P<0.05 was considered statistically significant. All statistical analyses were performed using SPSS 18.0 for Windows (IBM Corporation, Armonk, NY, USA).
Results
Independent t-test analysis indicated no significant differences between the AN-R and the HC groups in age (t[71]=1.88; P=0.065). The two groups showed significant differences between EAT-26 (t[70]=8.47; P<0.001) and YSR (INT: t[71]=4.96; P<0.001; EXT: t[71]=2.68; P=0.009; TP: t[71]=3.78; P<0.001) scores.
Cognitive and affective empathy
To examine the cognitive versus affective aspects of empathy, the total scores for the cognitive (PT + FS) scales and the affective (EC + PD) scales were calculated. As observed in , AN-R had a significantly lower CE mean score than HC (AN-R mean score: 0.44 ± 6.87; HC mean score: 5.24 ± 6.45; t[71] =3.0; P=0.003). The AN-R group scored significantly lower on both PT (t[71] =2.36; P=0.021) and FS (t[71] =2.18; P=0.032) scales. The two groups didn’t show significant differences on AE mean score (AN-R mean score: 4.69 ± 7.08; HC mean score: 4.20 ± 4.75; t[71] =0.35; P=0.725) and the two related subscales (see ).
Figure 1 Mean score of cognitive empathy and affective empathy reported by healthy controls and patients with AN-R.
Abbreviations: AE, affective empathy; CE, cognitive empathy; AN-R, anorexia nervosa-restricting type.
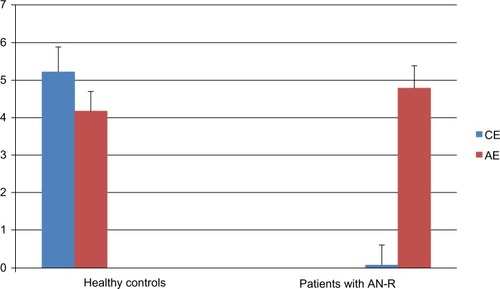
Table 1 Mean score (and standard deviation) of the IRI scales and group comparison
Cognitive empathy, disease severity, and associated psychopathology
Significant differences between groups with respect to CE (F[69]=5.19; P=0.008) and the PT subscale (F[69]=3.70; P=0.03) when EAT-26 mean scores were used as a covariate; no significant differences on the FS subscale (F[69]=2.61; P=0.081) were obtained.
Significant differences between groups in IRI when YSR mean scores were used as a covariate were noted. Specifically, when INT was used as a covariate: CE (F[70]=5.15; P=0.008), PT (F[70]=2.41; P=0.098), FS (F[70]=3.52; P=0.035); when EXT was used as a covariate: CE (F[70]=5.08; P=0.009), PT (F[70]=5.24; P=0.008), FS (F[70]=2.29; P=0.109); when TP was used as a covariate: CE (F[70]=4.46; P=0.015), PT (F[70]=2.92; P=0.061), FS (F[70]=3.25; P=0.045). No statistically significant associations between cognitive empathy and: 1) BMI (rho=−0.32; P=0.069); 2) disease duration (rho=−0.07; P=0.69); or 3) CBCL 6–18 (INT: rho=0.23; P=0.213; EXT =−0.05; P=0.806; TP =0.16; P=0.401) were detected.
Discussion
This study adds to the limited literature regarding empathy in AN-R and the results show statistically significant differences between patients with AN-R and the HC with respect to empathic profile assessed using the IRI.Citation4 The main finding arising from the current investigation, performed on a carefully selected population of adolescent females with AN-R, is the impairment in empathic abilities limited to the cognitive domain, while sparing the affective component. Cognitive capacity is the ability to take the perspective of the other person in real (perspective taking scale) and in fictional (fantasy scale) situations. In particular, a low score on the PT scale is indicative of an impairment in interpersonal functioning,Citation4 and converges with the repeated findings of altered social skills in anorectic patients.Citation6 Moreover, since executive functions contribute to the effective development of CECitation31 and, at the same time, are consistently reported as impaired in AN subjects,Citation32 further research is warranted to clarify the possibility that executive functions deficits interfere with the reduced CE abilities of AN patients.
Only two other studies assessed empathic abilities in AN-R through the IRI.Citation33,Citation34 In contrast with our results, these investigations reported no significant differences between patients and controlsCitation33 and higher ratings for emotional empathy in AN subjects than HC participants.Citation34 Moreover, a mixed sample of both AN-R and AN-BE patients were enrolled in this latter study, whereas in the current investigation subjects who engaged in binging/purging behaviors were excluded. Hence, it is difficult to compare our work with the other two, as they do present substantial differences not only with respect to sample age (adolescents in our report versus adults in Guttman and Laporte, and Beadle et al)Citation33,Citation34 and clinical severity (inpatients versus outpatients), but also as to the methods of score attribution. A lower CE and similar AE scores, compared to controls, is instead a finding that our AN patients have commonalities with Asperger subjects,Citation17 providing further support for the similarities between the two disorders.Citation7,Citation8
Results point out specific CE impairment in adolescents with AN-R. In particular, this finding suggests three key issues: first, on the basis of its independence from associated psychopathology assessed through the YSR, a CE deficit could be considered a specific marker of the adolescent AN-R, not mediated by comorbid symptoms; second, the independence of a CE deficit from the severity of illness suggests that it is not directly attributable to the profound effects of starvation on neuropsychological functioning.Citation35 In the future, longitudinal studies comparing ill and recovered AN-R patients may clarify whether the reduction in CE is a state-correlated characteristic or if it also persists after recovery. Third, the absence of correlation between CE scores and disease duration indicates the possible presence of a deficit in CE from the beginning of the disorder or even before AN-R onset. The hypothesis of CE impairment as a precursor of AN-R is consistent with other studies on the personality traits involved in creating a predisposition to developing this disorder.Citation1,Citation36 In this view, low CE could become one of the risk factors that precede the onset of a restrictive eating disorder. However, a prospective exploration of empathic skills in a non-clinical population is required to sustain the hypothesis of an association with the subsequent development of AN.
Finally, empathic impairment limited to the cognitive domain supports its functional independence from the affective one; neuroimaging (for a review, see Decety and Meyer)Citation37 as well as lesion studiesCitation5 sustain this hypothesis. In particular, two distinct brain systems for cognitive and AE have been described: the ventromedial prefrontal cortex is involved in CE, whereas the inferior frontal gyrus is a part of the AE network. Interestingly, ventromedial prefrontal cortex anomalies have been frequently reported in neuroimaging studies conducted in AN patients (eg, Uher et al);Citation38,Citation39 future functional MRI research is needed to investigate the response to empathy-eliciting stimuli in AN-R.
Conclusion
The main result of this study is that adolescents with AN-R type do not show global empathy abilities deficit, but rather a specific CE impairment. The current findings need to be qualified by a number of limitations. Specifically, self-reported measurements’ lack of objectivity, can be biased by denial or exaggeration of symptoms, as well as social desirability, and only reflect the self-perception of empathic characteristics. Moreover, a subject may not understand a question and give a misleading answer. However, this issue was mitigated in the present study by having a clinical psychologist remain with the subject in order to clarify possible misunderstandings during the administration of the IRI scale.
Secondly, the control subjects were screened for possible Axis I psychopathology through the YSR. However, besides the possible false positive and false negative results, the YSR does not evaluate personality disorders that could be present in the subjects enrolled in the study as controls.
The vast majority (84.4%) of AN-R patients involved in this study also meet diagnostic criteria for an additional internalizing diagnosis assessed through the K-SADS-PL.Citation24
Since internalizing disorders could impact empathic abilities,Citation19 we cannot rule out that the low levels of CE may be due to the influence of comorbid psychiatric symptoms rather than to AN-R itself. Also, while subjects with major depressive disorders assessed through the IRI reported significantly lower levels of both cognitive and affective empathy,Citation19 our AN-R patients showed a selective impairment of CE. However, in order to investigate the specific role of internalizing symptoms on empathic abilities, future studies should include an additional control sample composed of depressed/anxious subjects matched for demographic characteristics.
Further, the selective inclusion criteria of the patient group imply a relatively small sample size that limits the statistical power of results. Notwithstanding the problematic issues raised above, these data, if supported by a larger replication study, could have a 3-fold implications for AN-R: a) clinical, since the overall management of these patients should take into account the compromised empathic skills; b) therapeutic, with the development of specific intervention goals focused on CE enhancement; and c) preventive, with the aim of early individuation of subjects with CE deficits, a marker that, in addition to other susceptibility factors, may play an important role in the development and maintenance of the anorexic disorder.
Acknowledgments
The authors thank the adolescents and parents who participated in the study.
Disclosure
The authors report no conflicts of interest in this work.
References
- WentzEGillbergICAnckarsäterHGillbergCRåstamMAdolescent-onset anorexia nervosa: 18-year outcomeBr J Psychiatry2009194216817419182181
- Diagnostic and Statistical Manual of Mental Disorders5th edWashington, DCAmerican Psychiatric Association2013
- GodartNTPerdereauFCurtFPredictive factors of social disability in anorexic and bulimic patientsEat Weight Disord20049424925715844396
- DavisMHMeasuring individual differences in empathy: Evidence for a multidimensional approachJ Pers Soc Psychol1983441113126
- Shamay-TsoorySGAharon-PeretzJPerryDTwo systems for empathy: a double dissociation between emotional and cognitive empathy in inferior frontal gyrus versus ventromedial prefrontal lesionsBrain2009132Pt 361762718971202
- GillbergICRåstamMGillbergCAnorexia nervosa 6 years after onset: Part I. Personality disordersCompr Psychiatry199536161697705090
- AnckarsäterHHofvanderBBillstedtEThe sociocommunica-tive deficit subgroup in anorexia nervosa: autism spectrum disorders and neurocognition in a community-based, longitudinal studyPsychol Med20124291957196722186945
- OldershawATreasureJHambrookDTchanturiaKSchmidtUIs anorexia nervosa a version of autism spectrum disorders?Eur Eat Disord Rev201119646247421280165
- HambrookDTchanturiaKSchmidtURussellTTreasureJEmpathy, systemizing, and autistic traits in anorexia nervosa: a pilot studyBr J Clin Psychol200847Pt 333533918208640
- TchanturiaKHappéFGodleyJ“Theory of Mind” in anorexia nervosaEur Eat Disord Rev200412361366
- RussellTASchmidtUDohertyLYoungVTchanturiaKAspects of social cognition in anorexia nervosa: affective and cognitive theory of mindPsychiatry Res2009168318118519467562
- OldershawAHambrookDTchanturiaKTreasureJSchmidtUEmotional theory of mind and emotional awareness in recovered anorexia nervosa patientsPsychosom Med2010721737919995886
- Medina-PradasCBlas NavarroJÁlvarez-MoyaEMEmotional theory of mind in eating disordersInt J Clin Health Psychol2012122189202
- CalderoniSMuratoriFLeggeroCNeuropsychological functioning in children and adolescents with restrictive-type anorexia nervosa: an in-depth investigation with NEPSY-IIJ Clin Exp Neuropsychol201335216717923351019
- Shamay-TsoorySGHarariHAharon-PeretzJLevkovitzYThe role of the orbitofrontal cortex in affective theory of mind deficits in criminal offenders with psychopathic tendenciesCortex201046566867719501818
- HarariHShamay-TsoorySGRavidMLevkovitzYDouble dissociation between cognitive and affective empathy in borderline personality disorderPsychiatry Res2010175327727920045198
- RogersKDziobekIHassenstabJWolfOTConvitAWho cares? Revisiting empathy in Asperger syndromeJ Autism Dev Disord200737470971516906462
- Shamay-TsoorySGShurSBarcai-GoodmanLMedlovichSHarariHLevkovitzYDissociation of cognitive from affective components of theory of mind in schizophreniaPsychiatry Res20071491–3112317107716
- CusiAMMacqueenGMSprengRNMcKinnonMCAltered empathic responding in major depressive disorder: relation to symptom severity, illness burden, and psychosocial outcomePsychiatry Res2011188223123621592584
- Shamay-TsoorySHarariHSzepsenwolOLevkovitzYNeuropsychological evidence of impaired cognitive empathy in euthy-mic bipolar disorderJ Neuropsychiatry Clin Neurosci2009211596719359453
- MauragePGrynbergDNoëlXDissociation between affective and cognitive empathy in alcoholism: a specific deficit for the emotional dimensionAlcohol Clin Exp Res20113591662166821599717
- GodartNTPerdereauFReinZComorbidity studies of eating disorders and mood disorders. Critical review of the literatureJ Affect Disord2007971–3374916926052
- Diagnostic and Statistical Manual of Mental Disorders4th ed text revisionWashingtonAmerican Psychiatric Association2000
- KaufmanJBirmaherBBrentDSchedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity dataJ Am Acad Child Adolesc Psychiatry19973679809889204677
- FirstMBGibbonMSpitzerRLStructured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II)WashingtonAmerican Psychiatric Press1997
- AlbieroPIngogliaSLo CocoAContributo all’adattamento italiano dell’Interpersonal Reactivity Index. [Contribution to the Italian adaptation of the Interpersonal Reactivity Index]Testing Psicometria Metodologia2006132107125 Italian
- GarnerDMOlmstedMPBohrYGarfinkelPEThe eating attitudes test: psychometric features and clinical correlatesPsychol Med19821248718786961471
- AchenbachTMRescorlaLAManual for the ASEBA School-Age forms and ProfilesBurlingtonUniversity of Vermont, Research Center for Children, Youth, and Families2001
- AebiMMetzkeCWSteinhausenHCPrediction of major affective disorders in adolescents by self-report measuresJ Affect Disord20091151–214014918947881
- FerdinandRFValidity of the CBCL/YSR DSM-IV scales Anxiety Problems and Affective ProblemsJ Anxiety Disord200822112613417321103
- DecetyJJacksonPLThe functional architecture of human empathyBehav Cogn Neurosci Rev2004327110015537986
- Jáuregui-LoberaINeuropsychology of eating disorders: 1995–2012Neuropsychiatr Dis Treat2013941543023580091
- GuttmanHALaporteLEmpathy in families of women with borderline personality disorder, anorexia nervosa, and a control groupFam Process200039334535811008652
- BeadleJNParadisoSSalernoAMcCormickLMAlexithymia, emotional empathy, and self-regulation in anorexia nervosaAnn Clin Psychiatry201325210712023638441
- KeysABrozekJHenschelAThe biology of human starvationMinneapolisMinnesota University Press1950
- Rothschild-YakarLLevy-ShiffRFridman-BalabanRGurESteinDMentalization and relationships with parents as predictors of eating disordered behaviorJ Nerv Ment Dis2010198750150720611053
- DecetyJMeyerMFrom emotion resonance to empathic understanding: a social developmental neuroscience accountDev Psychopathol20082041053108018838031
- UherRBrammerMJMurphyTRecovery and chronicity in anorexia nervosa: brain activity associated with differential outcomesBiol Psychiatry200354993494214573322
- UherRMurphyTBrammerMJMedial prefrontal cortex activity associated with symptom provocation in eating disordersAm J Psychiatry200416171238124615229057