Abstract
Background
Mirtazapine, a noradrenergic and specific serotonergic antidepressant, which blocks the α2-adrenergic autoreceptors and heteroreceptors, has shown anxiolytic properties in clinical trials and preclinical animal experiments. The addition of mirtazapine to selective serotonin reuptake inhibitors (SSRIs) is clinically suggested to be more effective for anxiety disorders. In this study, we examined the combined effects of mirtazapine and citalopram, an SSRI, on the freezing behavior of rats, which was induced by contextual conditioned fear as an index of anxiety or fear.
Methods
Male Sprague Dawley rats individually received footshocks in a shock chamber, and 24 hours later, they were given citalopram and/or mirtazapine injections. One hour after citalopram and 30 minutes after mirtazapine administration, freezing behavior was analyzed in the same shock chamber without shocks.
Results
Mirtazapine decreased freezing in a dose-dependent manner, which is consistent with a previous report; it also enhanced an anxiolytic-like effect at a high dose (30 mg/kg) of citalopram. Because mirtazapine blocks α2-adrenoreceptors, the combined effect of atipamezole, a selective α2 receptor antagonist, with citalopram was also examined. Similar to mirtazapine, atipamezole reduced freezing dose-dependently, but the enhancement of citalopram’s effects by atipamezole was not clear when compared with mirtazapine.
Conclusion
The present findings suggest that mirtazapine has an anxiolytic-like effect and may enhance the anxiolytic-like effect of SSRIs, but this enhancement may not be explained by its anti-α2 property alone.
Introduction
Selective serotonin reuptake inhibitors (SSRIs) are recommended as a first-line treatment by the recent treatment guidelines for anxiety disorders; benzodiazepines are the second-line treatment due to the patients’ risks of developing drug dependency.Citation1,Citation2 However, not all patients with anxiety disorders remit even after adequate treatment; for instance, the remission rate was 45% in a clinical trial of one treatment in panic disorders.Citation3 Such treatment-resistant anxiety disorders have not been studied enough.Citation2 The “switching to” or “augmenting by” drugs with different pharmacological profiles are recommended as the third or fourth treatment by the treatment guideline. Among them, mirtazapine, a noradrenergic and specific serotonergic antidepressant that blocks the α2 -adrenergic autoreceptors, heteroreceptors, and serotonin (5-HT)2C/2A/3 receptors,Citation4 is a third or fourth line of treatment option for panic disorder, obsessive–compulsive disorder, and posttraumatic stress disorder, as indicated by the recent treatment guidelines.Citation2
Because mirtazapine is often chosen as an augmentation therapy of SSRIs for major depression,Citation5–Citation7 mirtazapine augmentation of SSRIs also seems promising for treatment-resistant anxiety disorders, but only one single-blind study reported that adding mirtazapine to citalopram resulted in a faster onset of efficacy for obsessive-compulsive disorder.Citation8 As mentioned above, because the pharmacological profile of mirtazapine is quite different from those of SSRIs,Citation4 the addition of mirtazapine may augment the anxiolytic effect of SSRIs. A recent preclinical study using in vivo microdialysis supported this idea; this study showed that mirtazapine itself increased 5-HT neurotransmission in the hippocampus and enhances 5-HT neurotransmission increased by the serotonin noradrenaline reuptake inhibitor (SNRI) milnacipran in the hippocampus and prefrontal cortex.Citation9 Increased 5-HT neurotransmission is related to the anxiolytic effect of antidepressants, including SSRIsCitation10,Citation11 and possibly mirtazapine.Citation9
Preclinical studies using animal models of anxiety are necessary before the clinical introduction of new pharmacological treatments or their combinations are used to see whether their putative efficacy in animals can be confirmed, and to determine whether the mechanism of action can be clarified. However, efficacy studies of the putative anxiolytic effect of mirtazapine in animal anxiety models have rarely been performed in contrast to preclinical studies of SSRIs.Citation11 Only one study by Kakui et alCitation12 reported that mirtazapine has an anxiolytic-like effect in the rat contextual conditioned fear model, and this effect is mediated by activation of the 5-HT1A receptor and the α1-adrenoreceptor. Hence, a behavioral study to examine the anxiolytic-like effect of adding mirtazapine to SSRIs in animals has never been performed.
The aim of this study was to examine whether the combination of mirtazapine and the very specific SSRI, citalopram,Citation4 increases the anxiolytic-like effect of citalopram on the expression of rat contextual conditioned fear. Specifically, drugs were administered to rats 24 hours after conditioning by footshock and shortly before the observation of freezing behavior. Furthermore, to clarify the role of the α2-adrenoreceptor in this effect, the effect of the highly selective α2-adrenoreceptor antagonist, atipamezole,Citation13 was tested alone or in combination with citalopram.
Methods
Animals
Male Sprague Dawley rats (230–300 g) were obtained from Japan SLC, Inc. (Shizuoka, Japan). A total of 292 rats were used. The number of rats per group for each experiment is described in –. The rats were housed in polypropylene cages with wood shavings on the floor; there were four animals per cage, with free access to food and water. The subjects were maintained under a 12-hour light–dark cycle (light phase: 6.30 am to 6.30 pm) in a temperature-controlled environment (22°C±1°C). The rats were tested during the light phase. Experiments began after a 2-week period of acclimatization. All experiments were performed between 8.00 am and 1.00 pm. All experiments were approved by the Hokkaido University School of Medicine Animal Care and Use Committee, and they were conducted in compliance with the Guide for the Care and Use of Laboratory Animals, Hokkaido University School of Medicine.
Figure 1 Effect of acute mirtazapine or atipamezole treatment on conditioned freezing in rats.
Abbreviations: Veh, vehicle; N, number.
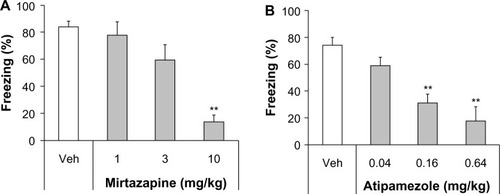
Figure 2 Effect of the coadministration of low-dose citalopram with subeffective doses of mirtazapine or atipamezole on conditioned freezing.
Abbreviations: Veh, vehicle; Cit, citalopram; N, number.
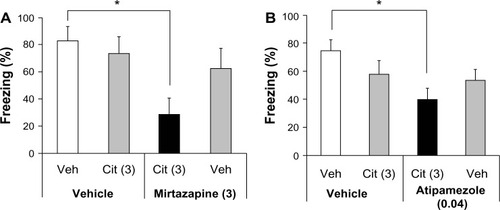
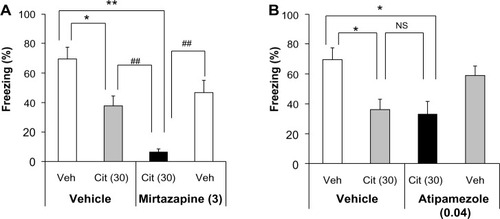
Figure 3 Effect of the coadministration of high-dose citalopram with subeffective mirtazapine or atipamezole on conditioned freezing.
Abbreviations: Veh, vehicle; Cit, citalopram; N, number; NS, not significant.
Drugs
Citalopram hydrobromide (a gift from Dainippon Sumitomo Pharma Co, Ltd, Osaka, Japan) was dissolved in 0.9% sterile saline. Atipamezole (Antisedan® 5 mg/mL; Orion Pharma, Espoo, Finland) was diluted with distilled water. Mirtazapine (obtained from Merck and Co, Inc, Whitehouse Station, NJ, USA) was dissolved in 0.15% tartaric acid. The vehicle alone was administered as a control. Citalopram was administered 60 minutes before testing, and mirtazapine or atipamezole was administered 30 minutes before testing. Citalopram and atipamezole were injected subcutaneously at a volume of 1 mL/kg. Mirtazapine was injected intraperitoneally in a volume of 2 mL/kg. The doses and routes of administration of citalopram, mirtazapine, and atipamezole used in this study were determined based on our previous experimentsCitation11,Citation12 and on earlier reports by other investigators.Citation14,Citation15
Procedures of conditioned fear stress-induced freezing
The total duration of the conditioning session was 5 minutes. The rats were individually subjected to inescapable electric footshocks for a total of 2.5 minutes in a shock chamber with a grid floor (19 × 22 × 20 cm; Medical Agent Co, Ltd, Tokyo, Japan). Five electric footshocks (2.5 mA unpredictable shock, each of a 30-second duration) were delivered at intershock intervals of 35–85 seconds (mean: 60 seconds) using a Model SGS-02D Shock Generator (Medical Agent Co, Ltd). One day after the footshocks, the rats were again placed in the shock chamber without footshocks and observed for 5 minutes. During the observation period, the duration of their freezing behavior was recorded using a modified time-sampling procedure, as previously described.Citation16 Every 10 seconds, the animal was classified as either freezing or active according to its behavior throughout the entire 10-second period. Freezing was defined as the absence of all observable movement of the skeleton and the vibrissae, except those related to respiration. All other behaviors were scored as activity. The percentage scores for the duration of freezing behavior (% freezing) were calculated for the 5-minute observation period.
In this study, six experiments, as shown in –, were performed independently. Each experiment was done once or twice, in which 28–32 rats, which included all groups, were tested on the same day to avoid the effect of variation between experiments. The rats were only used once for the experiments.
Data analysis
All the data are presented as the means ± standard error of the mean of the individual values for each rat in all groups. The statistical analysis of the data was performed using the nonparametric Kruskal–Wallis test followed by the Steel test to compare each of the treatments with a single vehicle control in dose–response experiments, or with the Steel–Dwass test to compare all possible pairs of means in combined treatment experiments for multiple comparisons as a post hoc test.
Results
Effect of acute mirtazapine or atipamezole treatment on the expression of conditioned freezing
Both mirtazapine and atipamezole affected the expression of conditioned freezing significantly (Kruskal–Wallis test, mirtazapine, H=16.625, P<0.001; atipamezole, H=23.448, P<0.0001). A Steel post hoc test to compare each of the treatments with the vehicle control group revealed that mirtazapine showed significant inhibitory effects at 10 mg/kg (P<0.01 versus the vehicle control group), but not at 1 mg/kg and 3 mg/kg (), and that atipamezole showed inhibitory effects at 0.16 mg/kg and at 0.64 mg/kg (P<0.01 versus the vehicle control group), but not at 0.04 mg/kg ().
Effect of coadministration of low-dose citalopram with mirtazapine or atipamezole on the expression of conditioned freezing
We previously reported that acute treatment with the SSRI citalopram dose-dependently reduced the expression of conditioned freezing.Citation17 At a low dose (3 mg/kg), citalopram did not change the expression of conditioned freezing significantly.Citation17 On the other hand, at a high dose (30 mg/kg), citalopram showed the maximal inhibitory effect.Citation17 In other words, even at a very high dose (100 mg/kg), the inhibitory effect of citalopram was equivalent to that of 30 mg/kg.Citation17 To investigate the combined effect of citalopram with mirtazapine or atipamezole, we used a subeffective low dose (3 mg/kg) of citalopram and subeffective doses of the other drugs (ie, 3 mg/kg of mirtazapine and 0.04 mg/kg of atipamezole). At each dose, any drug alone did not reduce freezing significantly. The coadministration of low-dose citalopram with subeffective doses of mirtazapine or atipamezole reduced the expression of conditioned freezing significantly (Kruskal–Wallis test, citalopram with mirtazapine, H=8.808, P<0.05; citalopram with atipamezole, H=8.588, P<0.05) (). A Steel–Dwass post hoc test showed that coadministration of low-dose citalopram with subeffective doses of mirtazapine or atipamezole significantly reduced freezing compared with the controls (vehicle + vehicle versus citalopram + mirtazapine, P<0.05; vehicle + vehicle versus citalopram+ atipamezole, P<0.05).
Effect of the coadministration of high-dose citalopram with mirtazapine or atipamezole on the expression of conditioned freezing
To investigate whether the maximal inhibitory effect of citalopram is augmented by mirtazapine or atipamezole, we used a high dose (30 mg/kg) of citalopram with subeffective doses of mirtazapine (3 mg/kg) or atipamezole (0.04 mg/kg). Coadministration of high-dose citalopram with subeffective mirtazapine or atipamezole doses significantly reduced the expression of conditioned freezing (Kruskal–Wallis test, citalopram with mirtazapine, H=27.223, P<0.0001; citalopram with atipamezole, H=13.971, P<0.005) (). A Steel–Dwass post hoc test showed that both high-dose citalopram alone and the coadministration of high-dose citalopram with subeffective mirtazapine significantly reduced freezing compared with the controls (vehicle + vehicle versus citalopram + vehicle, P<0.05; vehicle + vehicle versus citalopram + mirtazapine, P<0.01). Moreover, the coadministration of high-dose citalopram with subeffective mirtazapine significantly reduced freezing compared with high-dose citalopram alone and mirtazapine alone (citalopram + vehicle versus citalopram+ mirtazapine, P<0.01; citalopram + mirtazapine versus vehicle + mirtazapine, P<0.01; Steel–Dwass post hoc test) (). Similarly, both high-dose citalopram alone and the coadministration of high-dose citalopram with subeffective doses of atipamezole also significantly reduced freezing compared with controls (vehicle + vehicle versus citalopram + vehicle, P<0.05; vehicle + vehicle versus citalopram + atipamezole, P<0.05). However, there was no significant difference in freezing between high-dose citalopram alone and the coadministration of high-dose citalopram with subeffective atipamezole (citalopram + vehicle versus citalopram + atipamezole, P>0.05, Steel–Dwass post hoc test) ().
Discussion
Consistent with our previous studies,Citation12,Citation18 mirtazapine reduced the expression of conditioned freezing dose-dependently, and the SSRI citalopram inhibited conditioned freezing. In this study, the combination of subeffective doses of mirtazapine (3 mg/kg) and citalopram (3 mg/kg) enhanced the inhibitory effect of both drugs on conditioned freezing. Our previous study showed that high-dose citalopram (30 mg/kg) produces the maximal effect on conditioned freezing.Citation17 In this study, adjunctive subeffective mirtazapine enhanced the maximal inhibitory effect of high-dose citalopram (30 mg/kg) on conditioned freezing. These results suggest that mirtaza-pine itself has an anxiolytic-like effect, and that mirtazapine enhances the anxiolytic-like effect of SSRIs. This study is the first study to show that the combination of mirtazapine and an SSRI augments the anxiolytic-like effects of each drug. Based on these experimental findings, the putative efficacy of the combination therapy with mirtazapine and SSRI for treatment-resistant anxiety disorders may be promising, as this combination therapy is adapted to treatment-resistant forms of major depression.Citation6
In contextual conditioned fear in rats, drugs that facilitate 5-HT neurotransmission (ie, that increase extracellular 5-HT levels in the brain) generally reduce conditioned freezing.Citation11 Based on this principle, the previous findings of in vivo microdialysis studies may account for the augmentation effect of the combined mirtazapine and an SSRI.Citation9,Citation19 There are conflicting results as to whether mirtazapine alone increases extracellular 5-HT levels in the brain; some studies reported that mirtazapine increased extracellular 5-HT levels in the hippocampus,Citation9,Citation19 but others reported negative results in the hippocampus and other forebrain regions.Citation20,Citation21 Interestingly, mirtazapine enhances the increasing effect of the SNRI, milnacipran, on extracellular 5-HT levels in the hippocampus and prefrontal cortex.Citation9 Hence, these previous findings suggest that the augmentation effect of the combined mirtazapine and SSRI in contextual conditioned freezing is mediated by more increases in extracellular 5-HT. Moreover, 5-HT1A receptors are a potentially strong candidate for the target receptors, in which the anxiolytic-like activities of mirtazapine alone and its combination with an SSRI is mediated by an increase in 5-HT activity. It should be noted that 5-HT1A agonists reportedly reduced the expression of contextual conditioned freezing.Citation11 Furthermore, approximately one-half of the anxiolytic-like effect of mirtazapine in the expression of contextual conditioned freezing was antagonized by the selective 5-HT1A receptor antagonist, WAY-100635.Citation12
As indicated in the introduction, mirtazapine blocks not only α2-adrenergic autoreceptors and heteroreceptors, but also 5-HT2C/2A/3 receptors.Citation4 This study showed that the very selective α2 receptor antagonist, atipamezole, dose-dependently reduced conditioned freezing at low doses, as did mirtazapine. An earlier study reported that another α2 receptor antagonist, yohimbine, also reduced the expression of conditioned freezing.Citation22 The addition of subeffective doses of atipamezole to citalopram increased the inhibitory effect of low-dose citalopram, which was similar to what was shown with mirtazapine. A pharmacodynamic mechanism may be involved in this enhancement because atipamezole reportedly enhanced the effect of an SSRI and SNRI on 5-HT.Citation15 Furthermore, the α2 receptor antagonist idazoxan, like mirtazapine, reportedly enhances the increases in extracellular 5-HT levels by the SNRI milnacipran in the prefrontal cortex.Citation9 However, the enhancement of citalopram’s effects by atipamezole was not clear when compared with mirtazapine. Interestingly, atipamezole did not enhance the effect of high-dose citalopram, which induces the maximal effect, on conditioned freezing in contrast to mirtazapine. Therefore, although the effect of mirtazapine on conditioned freezing may be mediated by its α2 receptor antagonism, we cannot account for the enhancing effect of mirtazapine on citalopram only by the mechanism of α2 receptor antagonism.
Clinically, SSRIs and mirtazapine exert anxiolytic effects after chronic treatment;Citation2 however, in the animal model, acute SSRI and mirtazapine exerted an anxiolytic-like effect in contextual conditioned fear. As we previously discussed in our review,Citation11 this model is an animal model of fear or anxiety, but not of anxiety disorders. We found that prolonging the period between conditioning and exposure to conditioned fear stress for up to 7–14 days diminished the acute effects of SSRIs and mirtazapine, and the anxiolytic-like effects required chronic treatment (our publishedCitation11 and unpublished data). Thus, the long interval between conditioning by footshock and exposure to conditioned fear stress might improve the predictive and face validities of contextual conditioned freezing as an animal model of anxiety disorders. In future studies, we plan to study the combined effect of mirtazapine and SSRIs on the expression of contextual conditioned freezing while using a longer interval between conditioning by footshock and exposure to conditioned fear stress.
Conclusion
This study shows that the anxiolytic-like effect of the SSRI citalopram in contextual conditioned fear is enhanced by the adjunctive subeffective dose of mirtazapine and, to a lesser extent, by the α2-adrenoceptor antagonist atipamezole. The combination of an SSRI and mirtazapine may be a promising strategy for treating anxiety disorders. In contextual conditioned fear, mirtazapine has an anxiolytic-like effect and may enhance the anxiolytic-like effect of SSRIs, but this enhancement may not be explained by its anti-α2 property alone.
Acknowledgments
This work was supported in part by a Grant-in-Aid for Scientific Research No 24591673 (Takeshi Inoue) from the Japanese Ministry of Education, Culture, Sports, Science and Technology (Tokyo, Japan).
Disclosure
Dr Takeshi Inoue has received honoraria from Glaxo-SmithKline, Pfizer, Astellas, Eli Lilly, Mitsubishi Tanabe Pharma, Mochida Pharmaceutical, Otsuka Pharmaceutical, Meiji Seika Pharma, Asahi Kasei Pharma, Shionogi, Janssen Pharmaceutical, Takeda Pharmaceutical, and Yoshitomi Pharmaceutical; has received research/grant support from Otsuka Pharmaceutical; and is a member of the advisory boards of GlaxoSmithKline, Eli Lilly, Mochida Pharmaceutical, and Mitsubishi Tanabe Pharma. Dr Shin Nakagawa has received honoraria from GlaxoSmithKline, Eisai, Pfizer, Daiichi-Sankyo, Meiji Seika Pharma, Ono Pharmaceutical, and Eli Lilly, and has received research/grant support from Pfizer, Eli Lilly, Eisai, and Ono Pharmaceutical. Dr Ichiro Kusumi has received honoraria from Eli Lilly; has received research/grant support from Takeda Pharmaceutical, Astellas, and Dainippon Sumitomo Pharma; and is a member of the advisory board of Dainippon Sumitomo Pharma and Tanabe Mitsubishi Pharma. Dr Tsukasa Koyama has received honoraria from GlaxoSmithKline, Astellas, and Eli Lilly; has received research/grant support from Astellas and GlaxoSmithKline; and is a member of the advisory boards of GlaxoSmithKline and Mitsubishi Tanabe Pharma. Dr Yuji Kitaichi has received honoraria from Otsuka Pharmaceutical and Meiji Seika Pharma. Dr Takahiro Masuda and Dr Naoki Takamura are employed by Dainippon Sumitomo Pharma. Dr Yan An reports no conflicts of interest in this work.
References
- IronsJFluvoxamine in the treatment of anxiety disordersNeuropsychiatr Dis Treat20051428929918568110
- BandelowBZoharJHollanderEWFSBP Task Force on Treatment Guidelines for Anxiety, Obsessive-Compulsive and Post-Traumatic Stress DisordersWorld Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the pharmacological treatment of anxiety, obsessive-compulsive and post-traumatic stress disorders – first revisionWorld J Biol Psychiatry20089424831218949648
- PollackMHLepolaUKoponenHA double-blind study of the efficacy of venlafaxine extended-release, paroxetine, and placebo in the treatment of panic disorderDepress Anxiety200724111416894619
- MillanMJMulti-target strategies for the improved treatment of depressive states: Conceptual foundations and neuronal substrates, drug discovery and therapeutic applicationPharmacol Ther2006110213517016522330
- FurukawaTAAkechiTShimoderaSStrategic use of new generation antidepressants for depression: SUN(^_^)D study protocolTrials20111211621569309
- PapakostasGIManaging partial response or nonresponse: switching, augmentation, and combination strategies for major depressive disorderJ Clin Psychiatry200970Suppl 6162519922740
- MoretCCombination/augmentation strategies for improving the treatment of depressionNeuropsychiatr Dis Treat20051430130918568111
- PallantiSQuercioliLBruscoliMResponse acceleration with mirtazapine augmentation of citalopram in obsessive-compulsive disorder patients without comorbid depression: a pilot studyJ Clin Psychiatry200465101394139915491244
- YamauchiMImanishiTKoyamaTA combination of mirtazapine and milnacipran augments the extracellular levels of monoamines in the rat brainNeuropharmacology20126272278228722342987
- ErikksonEHumbleMSerotonin in psychiatric pathophysiology. A review of data from experimental and clinical researchPohlRGershonSProgress in Basic Clinical PharmacologyBaselKarger1990366119
- InoueTKitaichiYKoyamaTSSRIs and conditioned fearProg Neuropsychopharmacol Biol Psychiatry20113581810181921925230
- KakuiNYokoyamaFYamauchiMAnxiolytic-like profile of mirtazapine in rat conditioned fear stress model: Functional significance of 5-hydroxytryptamine 1A receptor and alpha1-adrenergic receptorPharmacol Biochem Behav200992339339819167420
- PertovaaraAHaapalinnaASirviöJVirtanenRPharmacological properties, central nervous system effects, and potential therapeutic applications of atipamezole, a selective alpha2-adrenoceptor antagonistCNS Drug Rev200511327328816389294
- HaapalinnaAViitamaaTMacDonaldEEvaluation of the effects of a specific alpha 2-adrenoceptor antagonist, atipamezole, on alpha 1-and alpha 2-adrenoceptor subtype binding, brain neurochemistry and behaviour in comparison with yohimbineNaunyn Schmiedebergs Arch Pharmacol199735655705829402036
- GobertARivetJMCistarelliLMelonCMillanMJAlpha2-adrenergic receptor blockade markedly potentiates duloxetine- and fluoxetine-induced increases in noradrenaline, dopamine, and serotonin levels in the frontal cortex of freely moving ratsJ Neurochem1997696261626199375697
- InoueTLiXBAbekawaTSelective serotonin reuptake inhibitor reduces conditioned fear through its effect in the amygdalaEur J Pharmacol2004497331131615336949
- MurakiIInoueTKoyamaTEffect of co-administration of the selective 5-HT1A receptor antagonist WAY 100,635 and selective 5-HT1B/1D receptor antagonist GR 127,935 on anxiolytic effect of citalopram in conditioned fear stress in the ratEur J Pharmacol20085861–317117818423441
- HashimotoSInoueTKoyamaTSerotonin reuptake inhibitors reduce conditioned fear stress-induced freezing behavior in ratsPsychopharmacology (Berl)199612321821868741941
- de BoerTHNefkensFvan HelvoirtAvan DelftAMDifferences in modulation of noradrenergic and serotonergic transmission by the alpha-2 adrenoceptor antagonists, mirtazapine, mianserin and idazoxanJ Pharmacol Exp Ther199627728528608627567
- BengtssonHJKeleJJohanssonJHjorthSInteraction of the antidepressant mirtazapine with alpha2-adrenoceptors modulating the release of 5-HT in different rat brain regions in vivoNaunyn Schmiedebergs Arch Pharmacol20003624–540641211111835
- MillanMJGobertARivetJMMirtazapine enhances frontocortical dopaminergic and corticolimbic adrenergic, but not serotonergic, transmission by blockade of alpha2-adrenergic and serotonin2C receptors: a comparison with citalopramEur J Neurosci20001231079109510762339
- MuellerDOlivera-FigueroaLAPineDSQuirkGJThe effects of yohimbine and amphetamine on fear expression and extinction in ratsPsychopharmacology (Berl)2009204459960619242678
