Abstract
Background
Recently, a relationship between obesity and schizophrenia has been reported. The prediction of resting energy expenditure (REE) is important to determine the energy expenditure of patients with schizophrenia. However, there is a lack of research concerning the most accurate REE predictive equations among Asian patients with schizophrenia. The purpose of the study reported here was to compare the validity of four REE equations for patients with schizophrenia taking antipsychotics.
Methods
For this cross-sectional study, we recruited patients (n=110) who had a Diagnostic and Statistical Manual of Mental Disorders, fourth edition, diagnosis of schizophrenia and were admitted to four psychiatric hospitals. The mean (± standard deviation) age of these patients was 45.9±13.2 years. Anthropometric measurements (of height, weight, body mass index) were taken at the beginning of the study. REE was measured using indirect calorimetry. Comparisons between the measured and estimated REEs from the four equations (Harris–Benedict, Mifflin–St Jeor, Food and Agriculture Organization/World Health Organization/United Nations University, and Schofield) were performed using simple linear regression analysis and Bland–Altman analysis.
Results
Significant trends were found between the measured and predicted REEs for all four equations (P<0.001), with the Harris–Benedict equation demonstrating the strongest correlation in both men and women (r=0.617, P<0.001). In all participants, Bland–Altman analysis revealed that the Harris–Benedict and Mifflin–St Jeor equations did not show a significant bias in the prediction of REE, however, a significant overestimation error was shown for the Food and Agriculture Organization/World Health Organization/United Nations University and Schofield equations.
Conclusion
When estimating REE in patients with schizophrenia taking antipsychotics, the Harris–Benedict equation appears to be the most appropriate for clinical use.
Introduction
Weight gain among patients with schizophrenia is a growing concern because the prevalence of obesity among patients with schizophrenia is higher than the prevalence in the general population.Citation1–Citation3 Patients with schizophrenia are at risk for becoming obese due to antipsychotic drug use,Citation4 poor dietary habits,Citation5 and lack of exercise or limited activity due to the negative symptoms of the disease.Citation6
Several studies have shown that being overweight is a major risk factor for metabolic syndrome, cardiovascular diseases, and premature death.Citation7–Citation9 Further, obesity is associated with increased medication costs,Citation10 noncompliance with antipsychotic medication regimens,Citation11 poorer psychosocial adaptation,Citation12 and reduced quality of lifeCitation13 among patients with schizophrenia.
There are three principal components of energy expenditure (EE) in humans: 1) the resting energy expenditure (REE), 2) the thermic effects of food, and 3) the EE of physical activity. REE is the largest component of EE, ranging from 68% to 80% of non-activity total EE,Citation14 and it is determined by several factors, including age,Citation15 sex,Citation16 body weight, and fat-free mass.Citation17 The maintenance of weight is the result of a balance between energy intake and expenditure.Citation18
Previous studies among patients with severe mental illnesses (SMIs) have assessed the predictive equations for REE only in Western populations.Citation19–Citation21 The differences in lifestyle and physique make it difficult to extrapolate the predictive REE equations used in populations of European descent for use in Asian populations. Therefore, the purpose of the study reported here was to measure REE in a group of male and female patients with schizophrenia who were taking antipsychotic medication and to determine whether REE can be reliably estimated using previously published predictive equations.
Methods
Participants
This study was conducted between January and September 2012. The subjects included 110 outpatients (69 males and 41 females) at four psychiatric hospitals in Japan who were diagnosed with either schizophrenia or schizoaffective disorder based on Diagnostic and Statistical Manual of Mental Disorders, fourth edition, diagnostic criteria.Citation22 The diagnoses of the patients were recorded from their medical charts. The data collection for this study was approved by the Ethics Committee of Hirosaki University School of Medicine, and all subjects provided written informed consent before participating in the study.
Procedure
Demographic (age and sex) and medication data were obtained from the participants’ medical records. Of the 110 subjects in the study, 73 were receiving antipsychotic combination therapy and 37 were receiving antipsychotic monotherapy. Of the 37 patients receiving antipsychotic monotherapy, ten were taking high metabolic risk antipsychotics (olanzapine =6, quetiapine =4), 13 patients were taking risperidone, eleven patients were taking aripiprazole, two patients were taking blonanserin, and one patient was taking perospirone. Patient height was determined without shoes on a portable stadiometer with the mandible plane parallel to the floor.
The REE measurements were performed using a MedGem™ portable indirect calorimeter (HealtheTech, Inc., Golden, CO, USA) following an overnight fast and 30 minutes of rest at a constant temperature in a relaxing environment. Subjects were instructed to position the nose clips and try to breathe nasally to test that nasal respiration was blocked. The calorimeter used for this study was auto-calibrated for 5 minutes before testing. After the calibration was complete, the patients were instructed to place the single-use mouthpiece into their mouths and breathe normally. A typical reading took approximately 10 minutes to obtain.
Predictive REE equations
The predictive regression equations of Harris and Benedict,Citation23 Mifflin et al (the Mifflin–St Jeor equation),Citation24 the Food and Agriculture Organization/World Health Organization/United Nations University (FAO/WHO/UNU),Citation25 and SchofieldCitation26 were used to calculate REE ().
Table 1 Equations used for the estimation of resting energy expenditure in kcal/day
Statistical analysis
Descriptive statistical analyses were performed to describe the demographic and clinical variables. To compare the main demographic and clinical characteristics between sexes, an unpaired Student’s t-test was performed to analyze continuous variables. The data are presented as the means ± standard deviation. The relationship between measured and predicted REEs was tested using simple linear regression analysis. The root mean square error (RMSE) was used to evaluate the model fit. Pearson’s correlation coefficient (r) was calculated to observe the association between the measured and predicted REEs for each of the predictive regression equations used. Bland–Altman analysisCitation27 was used to calculate agreement between the measured and predicted REEs. A value of P<0.05 was considered significant. Data were analyzed using the PASW Statistics 18 software for Windows (IBM Corporation, Armonk, NY, USA).
Results
Participant characteristics
The characteristics of the participants are listed in . Significant differences were found between sexes in the anthropometric measurements, such as body weight and height. Moreover, males had significantly higher measured and predicted REEs than females. No differences were observed for any of the other characteristics.
Table 2 Anthropometric characteristics and resting energy expenditures (REEs) of subjects
Linear regression
In all participants, linear regression analysis revealed that the Harris–Benedict equation had the lowest RMSE and thus the best predictive accuracy of all tested equations (RMSE =283.41, r=0.617, P<0.001), followed by the Mifflin–St Jeor equation (RMSE =291.31, r=0.588, P<0.001), the Schofield equation (RMSE =301.70, r=0.546, P<0.001), and the FAO/WHO/UNU equation (RMSE =303.93, r=0.536, P<0.001). All four predictive equations were found to reliably predict the measured REE (P<0.001).
In males, linear regression analysis revealed that the Harris–Benedict equation had the lowest RMSE and thus the best predictive accuracy of all tested equations (RMSE =319.04, r=0.613, P<0.001), followed by the Mifflin–St Jeor equation (RMSE =322.38, r=0.602, P<0.001), the Schofield equation (RMSE =339.86, r=0.540, P<0.001), and the FAO/WHO/UNU equation (RMSE =345.77, r=0.516, P<0.001). All four predictive equations were found to reliably predict the measured REE in males (P<0.001).
In females, linear regression analysis revealed that the Mifflin–St Jeor equation had the lowest RMSE and thus the best predictive accuracy of all tested equations (RMSE =229.66, r=0.593, P<0.001), followed by the FAO/WHO/UNU equation (RMSE =231.52, r=0.584, P<0.001), the Harris–Benedict equation (RMSE =232.56, r=0.579, P<0.001), and the Schofield equation (RMSE =238.41, r=0.549, P<0.001). All four predictive equations were found to reliably predict the measured REE in females (P<0.001).
Bland–Altman analysis
For all participants, Bland–Altman analysis revealed that the Harris–Benedict (−1.7±282.3 kcal/day; ) and Mifflin–St Jeor (−46.7±290.3 kcal/day; ) equations did not show a significant bias in the prediction of REE. For the other two equations, Bland–Altman analysis showed significant mean biases of 88.7±305.5 kcal/day for the FAO/WHO/UNU equation () and 64.7±301.8 kcal/day for the Schofield equation ().
Figure 1 Bland–Altman plot of measured resting energy expenditure (REE) and predicted REE using the Harris–Benedict (HB) equationCitation23 in males (black squares) and females (gray circles).
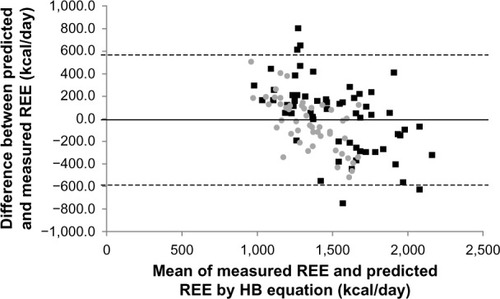
Figure 2 Bland–Altman plot of measured resting energy expenditure (REE) and predicted REE using the Mifflin–St Jeor (M) equationCitation24 in males (black squares) and females (gray circles).
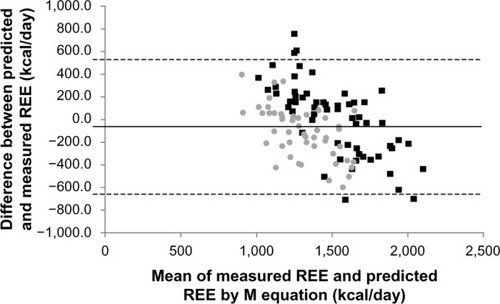
Figure 3 Bland–Altman plot of measured resting energy expenditure (REE) and predicted REE using the Food and Agriculture Organization/World Health Organization/United Nations University (F) equationCitation25 in males (black squares) and females (gray circles).
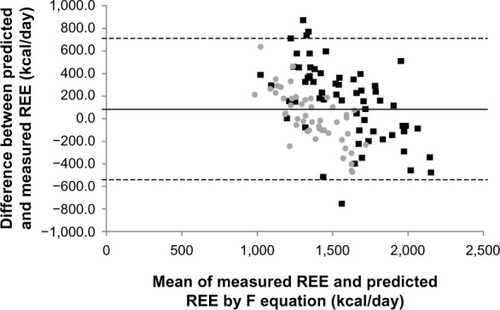
Figure 4 Bland–Altman plot of measured resting energy expenditure (REE) and predicted REE using the Schofield (S) equationCitation26 in males (black squares) and females (gray circles).
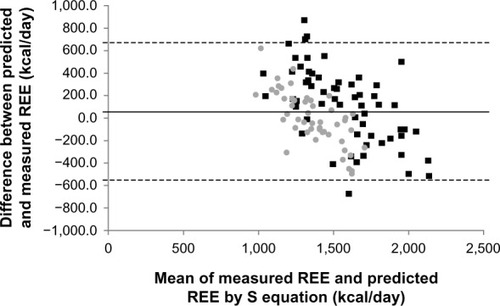
In males, Bland–Altman analysis revealed that the Harris–Benedict (27.6±316.4 kcal/day) and Mifflin–St Jeor (9.4±323.3 kcal/day) equations did not show a significant bias in the prediction of REE. For the other two equations, the analysis showed significant mean biases of 149.5±343.5 kcal/day for the FAO/WHO/UNU equation and 119.0±337.0 kcal/day for the Schofield equation.
In females, Bland–Altman analysis revealed that the Harris–Benedict (−38.1±231.1 kcal/day), FAO/WHO/UNU (13.1±232.2 kcal/day), and Schofield (−2.9±237.6 kcal/day) equations did not show a significant bias in the prediction of REE. In contrast, the analysis showed a significant mean bias of −116.5±227.3 kcal/day for the Mifflin–St Jeor equation.
Discussion
To the best of our knowledge, this study is the first to compare actual REE measurements with predicted REEs determined by the Harris–Benedict, Mifflin–St Jeor, FAO/WHO/UNU, and Schofield equations in Asian patients diagnosed with schizophrenia. REE corresponds to the calories the body uses to maintain vital body functions (eg, heart rate, brain function, and breathing) and represents the number of calories an individual would burn daily if awake at rest. An FAO/WHO/UNU expert panel adopted the principle of expressing the energy requirements of adults in terms of multiples of REE.Citation25 Therefore, REE is used to estimate the 24-hour EE and physical activity level (24-hour EE divided by REE). In this study, we found that in Japanese patients with schizophrenia, the Harris–Benedict equation reliably predicted the energy needs of male and female patients with an insignificant estimation bias.
Individuals with a lower REE tend to gain more weight than those with a normal REE.Citation28,Citation29 To develop an appropriate intervention program for weight reduction in patients with schizophrenia, an accurate assessment of REE for each patient is needed.Citation28
Recently, direct or indirect calorimeters and respiratory chambers have been developed to measure REE. However, these devices are expensive, and their operation requires trained personnel and long testing times for patients with schizophrenia. Therefore, the calculation of REE by mathematical equation has been adopted as the major method to assess the energy needs of individuals.Citation28
In the study reported here, we employed four predictive equations for REE. These equations were developed to predict the REE in healthy populations. The Harris–Benedict equation was derived from predominantly normal-weight Caucasian males (n=136) aged 16 to 63 (27±9) years and females (n=103) aged 15 to 74 (31±14) years in studies conducted from approximately 1907 to 1917.Citation23 The Mifflin–St Jeor equation was developed from a sample of 498 normal-weight, overweight, obese, and severely obese individuals aged 19 to 78 (44.5±14.1) years.Citation24 The racial composition of the sample was not specified, and the representation of older adults (75 to 84 years) was limited. Finally, the FAO/WHO/UNU and Schofield equations were developed from a database of the scientific literature published from 1914 to 1980.Citation25,Citation26 This database consisted of 7,173 subjects, mostly derived from European military and police recruits. The age of the study participants ranged from 19 to 82 years.
A few studies have compared the measured and predicted REEs of SMI patients in Western populations. A previous study of eight Australian male patients with schizophrenia demonstrated that the Harris–Benedict equation overestimated the REE by 284 kcal/day.Citation19 These researchers also found that the Schofield equation overestimated the REE by 287 kcal/day. In another study in Greece,Citation21 the Mifflin–St Jeor equation was determined to be the most appropriate equation for 128 male and female patients with mood or psychotic disorders. Moreover, in our study, this equation was found to be the most accurate because it produced estimation errors of only −1.7 kcal/day in all participants. In Skouroliakou et al’s study,Citation21 the predictive Harris–Benedict and Schofield equations were found to greatly overestimate the real energy needs of male and female patients with SMIs. For example, in males, the Harris–Benedict equation overestimated the measured REE by 175 kcal/day. In a study of 15 patients with bipolar disorder in Italy,Citation20 researchers found that the Harris–Benedict equation overestimated REE by 483 kcal/day and that the Schofield equation overestimated REE by 397 kcal/day.
Our results show sex differences in agreement between the measured and predicted REEs for predictive equations. Because the predictive equations were developed mainly from measurements made on Caucasian subjects, ethnicity could explain the observed differences. In addition, sex hormones such as estrogens and progesterone can affect REE,Citation29 and menstrual condition or menopause may have affected our results.
In contrast to previous studies, our results show that the Harris–Benedict equation was not biased in the prediction of REE. One possible explanation for this is that the mean body mass index of the participants in this study was lower than that of the studies from Western countries. Obesity might be related to a hypometabolic state that is reflected as a decreased REE/kg body mass.Citation30 Another explanation is that differences in physical exercise, sleep pattern, illness duration, severity of negative symptoms, body composition, ethnicity, and socio-environmental factors might have affected our findings.Citation31–Citation34 In particular, antipsychotic medications may be an important factor. Although some studies have found unaltered REEs between patients who were taking antipsychotics and those who were not,Citation5,Citation35 the use of first- or second-generation antipsychotics might have confounded the results. However, a lack of research concerning these mentioned factors in this population limits our ability to determine those factors that might have contributed to the differences among studies. Additional studies are necessary to further establish the predictive value of these equations in a larger population taking different antipsychotic drugs.
Conclusion
The findings of this study suggest the use of the Harris–Benedict equation as the most appropriate means of estimating the REE of male and female patients with schizophrenia taking antipsychotics. An equation that can predict the energy needs of patients with schizophrenia that has a low estimation error and low cost might be useful for a weight reduction program for these patients.
Acknowledgments
The authors would like to thank all coworkers for their skillful contributions to the data collection and management. Funding for this study was provided by a Grant-in-Aid for Young Scientists (B); The Ministry of Education, Culture, Sports, Science and Technology, Japan; the Karoji Memorial Fund for Medical Research (Grant B); and SENSHIN Medical Research Foundation.
Disclosure
The authors declare that they have no competing interests in this work.
References
- SusceMTVillanuevaNDiazFJde LeonJObesity and associated complications in patients with severe mental illnesses: a cross-sectional surveyJ Clin Psychiatry200566216717315705001
- DickersonFBBrownCHKreyenbuhlJAObesity among individuals with serious mental illnessActa Psychiatr Scand2006113430631316638075
- SugawaraNYasui-FurukoriNSatoYPrevalence of metabolic syndrome among patients with schizophrenia in JapanSchizophr Res20101232–324425020850274
- BobesJRejasJGarcia-GarciaMEIRE Study GroupWeight gain in patients with schizophrenia treated with risperidone, olanzapine, quetiapine or haloperidol: results of the EIRE studySchizophr Res20036212778812765737
- GothelfDFalkBSingerPWeight gain associated with increased food intake and low habitual activity levels in male adolescent schizophrenic inpatients treated with olanzapineAm J Psychiatry200215961055105712042200
- VancampfortDKnapenJProbstMScheeweTRemansSDe HertMA systematic review of correlates of physical activity in patients with schizophreniaActa Psychiatr Scand2012125535236222176559
- MartinRLCloningerCRGuzeSBClaytonPJMortality in a follow-up of 500 psychiatric outpatients. I. Total mortalityArch Gen Psychiatry198542147543966852
- AllebeckPSchizophrenia: a life-shortening diseaseSchizophr Bull198915181892717890
- LeuchtSBurkardTHendersonJMajMSartoriusNPhysical illness and schizophrenia: a review of the literatureActa Psychiatr Scand2007116531733317919153
- ChwastiakLARosenheckRAMcEvoyJPThe impact of obesity on health care costs among persons with schizophreniaGen Hosp Psychiatry20093111719134502
- WeidenPJMackellJAMcDonnellDDObesity as a risk factor for antipsychotic noncomplianceSchizophr Res2004661515714693352
- De HertMPeuskensBvan WinkelRBody weight and self- esteem in patients with schizophrenia evaluated with B-WISESchizophr Res2006881–322222616996250
- SugawaraNYasui-FurukoriNSatoYBody mass index and quality of life among outpatients with schizophrenia in JapanBMC Psychiatry20131310823570345
- GoranMIEnergy metabolism and obesityMed Clin North Am200084234736210793646
- VaughanLZurloFRavussinEAging and energy expenditureAm J Clin Nutr19915348218252008859
- FerraroRLilliojaSFontvieilleAMRisingRBogardusCRavussinELower sedentary metabolic rate in women compared with menJ Clin Invest19929037807841522233
- IllnerKBrinkmannGHellerMBosy-WestphalAMüllerMJMetabolically active components of fat free mass and resting energy expenditure in nonobese adultsAm J Physiol Endocrinol Metab20002782E308E31510662716
- RosenbaumMLeibelRLHirschJObesityN Engl J Med199733763964079241130
- SharpeJKByrneNMStedmanTJHillsAPResting energy expenditure is lower than predicted in people taking atypical antipsychotic medicationJ Am Diet Assoc2005105461261515800566
- SorecaIMauriMCastrogiovanniSSimonciniMCassanoGBMeasured and expected resting energy expenditure in patients with bipolar disorder on maintenance treatmentBipolar Disord20079778478817988371
- SkouroliakouMGiannopoulouIKostaraCVasilopoulouMComparison of predictive equations for resting metabolic rate in obese psychiatric patients taking olanzapineNutrition20092518819318947974
- American Psychiatric Association (APA)Diagnostic and Statistical Manual of Mental Disorders4th edWashington DCAPA1994
- HarrisJABenedictFGA Biometric Study of Human Basal MetabolismProc Natl Acad Sci U S A191841237037316576330
- MifflinMDSt JeorSTHillLAScottBJDaughertySAKohYOA new predictive equation for resting energy expenditure in healthy individualsAm J Clin Nutr19905122412472305711
- Energy and protein requirements. Report of a joint FAO/WHO/UNU Expert ConsultationWorld Health Organ Tech Rep Ser198572412063937340
- SchofieldWNPredicting basal metabolic rate, new standards and review of previous workHum Nutr Clin Nutr198539Suppl 15414044297
- BlandJMAltmanDGStatistical methods for assessing agreement between two methods of clinical measurementLancet198632784763073102868172
- FrankenfieldDRoth-YouseyLCompherCComparison of predictive equations for resting metabolic rate in healthy nonobese and obese adults: a systematic reviewJ Am Diet Assoc2005105577578915883556
- DayDSGozanskyWSVan PeltRESchwartzRSKohrtWMSex hormone suppression reduces resting energy expenditure and {beta}-adrenergic support of resting energy expenditureJ Clin Endocrinol Metab20059063312331715741268
- CuerdaCMerchan-NaranjoJVelascoCInfluence of resting energy expenditure on weight gain in adolescents taking second-generation antipsychoticsClin Nutr201130561662321492975
- CarotenutoMBruniOSantoroNDel GiudiceEMPerroneLPascottoAWaist circumference predicts the occurrence of sleep-disordered breathing in obese children and adolescents: a questionnaire-based studySleep Med20067435736116713341
- EspositoMAntinolfiLGallaiBExecutive dysfunction in children affected by obstructive sleep apnea syndrome: an observational studyNeuropsychiatr Dis Treat201391087109423976855
- CarotenutoMEspositoMParisiLDepressive symptoms and childhood sleep apnea syndromeNeuropsychiatr Dis Treat2012836937322977304
- BattagliaGAlesiMIngugliaMSoccer practice as an add-on treatment in the management of individuals with a diagnosis of schizophreniaNeuropsychiatr Dis Treat2013959560323662058
- NilssonBMForslundAHOlssonRMHambraeusLWieselFADifferences in resting energy expenditure and body composition between patients with schizophrenia and healthy controlsActa Psychiatr Scand20061141273516774658
