Abstract
Skull metastasis from hepatocellular carcinoma (HCC) is reported rarely. In addition, solitary skull metastasis as the first symptom of HCC is reported even less. Here, we reported a case of solitary skull metastasis as the first symptom of HCC and reviewed the literature on skull metastasis. A 49-year-old male patient was admitted to Jinjiang Hospital of Quanzhou Medical College with a painless parietal-occipital scalp mass, and he denied any history of hepatic disease. A cranial computed tomography demonstrated a hypervascular enhancement with osteolytic change in the right parietal-occipital region, cranial magnetic resonance imaging indicated a highly enhanced and osteolytic skull tumor, and abdominal computed tomography showed a huge tumor in the liver. The other examinations showed no other metastases. Laboratory data showed no liver dysfunction while hepatitis B surface antigen was positive, and alpha fetal protein level was high. A craniectomy was performed and the mass was totally removed. The histological diagnosis was skull metastasis from HCC. The patient was subsequently treated by transcatheter arterial chemoembolization. In a review of published literature, the incidence of skull metastasis from HCC in the period between 1990 and 2011 has significantly increased. The misdiagnosis rate of skull metastases as the first symptom from HCC was high. Therefore, it is necessary to give each patient with a scalp mass that has invaded the skull a liver ultrasound or computed tomography scan. On the other hand, we found that metastases that occurred in the calvaria site were more frequent than those that occurred in the skull base and facial skeleton. This may be worthy of further investigation in the future.
Case report
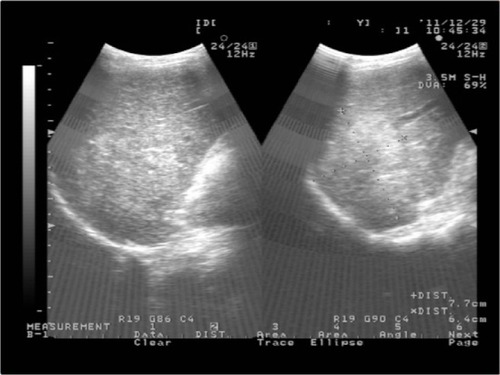
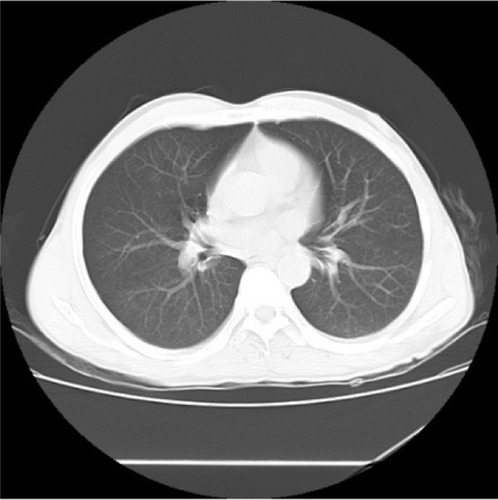
A 49-year-old male visited Jinjiang Hospital of Quanzhou Medical College with the complaint of a painless mass in the right parietal-occipital region of the skull. The mass was found incidentally 1 month earlier by the patient himself and it had grown rapidly. He denied any head traumas or any significant medical problems, including prior history of hepatic disease or chronic alcoholism. Bony window of cranial nonenhanced computed tomography (CT) scan showed a 5 × 5 cm2 soft tissue mass with irregular destruction (), and contrast-enhanced CT scan showed a hypervascular enhancement with osteolytic pathological change in the parietal-occipital region of the skull (). On admission, neurological and physical examinations revealed no neurological deficits, hepatomegaly, or obvious abnormalities except a painless non-movable mass about 5 × 5 cm2 in size over the right parietal-occipital region. Laboratory data showed no liver dysfunction while HBsAg (hepatitis B surface antigen) was positive, and AFP (alpha fetal protein) level was high (). On cranial magnetic resonance imaging, the tumor was a homogeneous well-defined mass with involvement of the inner and outer skull table. It revealed isosignal intensity on T2-weighted () and T1-weighted imaging (), with significant enhancement by gadolinium (). Abdominal B ultrasound showed a large mass in the right lobe of the liver (); therefore, a contrast-enhanced CT of the abdomen and a nonenhanced CT of the breast were taken. Contrast-enhanced CT of the abdomen showed a huge enhanced carcinoma in the right lobe of the liver (–). Nonenhanced CT of the breast showed no lung metastases (). A single-photon emission computed tomography of total skeletal bones showed no metastases (). Our diagnosis was hepatocellular carcinoma (HCC) with skull metastasis and chronic hepatitis B.
Figure 1 CT of cranial bones.
Abbreviation: CT, computed tomography.
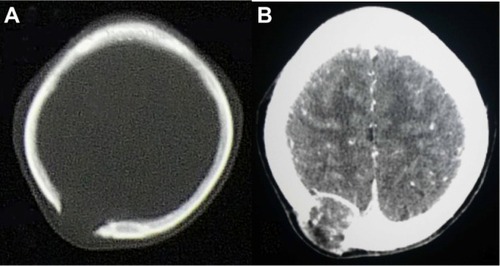
Figure 2 MRI of cranial bones.
Abbreviation: MRI, magnetic resonance imaging.
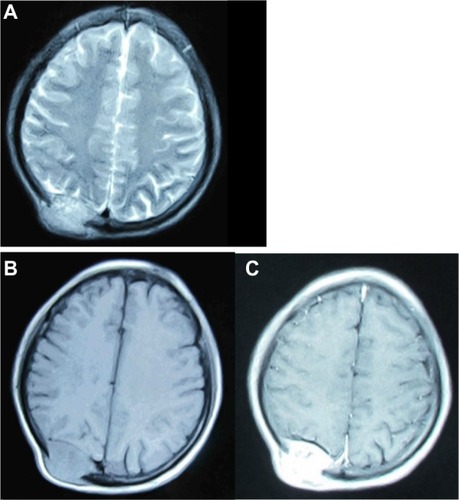
Figure 4 Contrast-enhanced computed tomography of abdomen showed a huge enhanced carcinoma in the liver.

Figure 6 Single-photon emission computed tomography of total skeletal bones showed no other metastases.
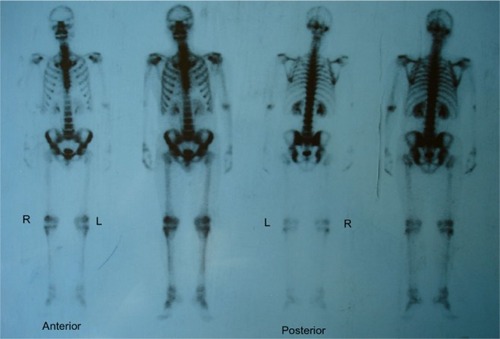
Table 1 Laboratory data on admission
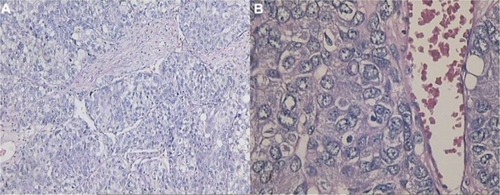
The carcinoma was radically resected with surrounding normal bone via right parietal-occipital craniectomy under general anesthesia. During the operation, a large and well-demarcated reddish-brown mass was found to have penetrated both tables of the skull through the diploic space. The carcinoma looked like cauliflower, and the underlying dura was intact and did not show any evidence of gross carcinoma invasion. The dural surface attached to the carcinoma was curetted and the rough surface of the dura was cauterized by bipolar forceps. The carcinoma was totally removed. Histopathological examination of the carcinoma revealed pleomorphic tumor cells with eosinophilic cytoplasm, and prominent nucleoli and mitosis arranged in trabecular and solid pattern. The pathological findings confirmed the diagnosis of metastasic HCC ( and ). Postoperative recovery was satisfactory. To treat the primary carcinoma, transcatheter arterial chemoembolization with pirarubicin (40 mg), carboplatin (200 mg), floxuridine (250 mg), Lipiodol, and Gelatin sponge particles was performed after selecting a feeding artery of the tumor on aortography. The patient was discharged 1 month later. The patient survived after half a year of follow up and did not show any evidence of recurrence in the skull. However, because of the recurrence of hepatocellular carcinomas, the patient died from liver failure in the 18 months since he received transcatheter arterial chemoembolization.
Figure 7 The histopathological characteristics of carcinoma and the immunohistochemical finding.
Abbreviations: HE, hematoxylin-eosin staining; AFP, alpha fetal protein; CK, creatine kinase; CD, cluster of differentiation or leukocyte differentiation antigen; Ki67, nuclear-associated antigen Ki67.
Discussion
Hepatocellular carcinoma is the fifth most common cancer in the world and is especially prevalent in Africa and East Asia.Citation1 The incidence of HCC in developing countries is third most common of the various types of cancer.Citation2 Intrahepatic metastasis is the most common metastasis of HCC. Extrahepatic metastases of HCC usually occurs in the regional lymph nodes (16%–40%) and lungs (34%–70%), but less commonly in the skeleton (1.6%–16%).Citation3–Citation6 In skeleton metastasis, HCC usually metastasizes preferentially to the vertebral column, pelvis, femora, and ribs, but rarely to the skull. The incidence of skull metastases from HCC is 0.4%–1.6%,Citation3–Citation5,Citation7,Citation8 and 9% of patients with calvarial metastases have other skeletal deposits.Citation9
After a thorough search of the literature, we found 48 articles in total describing patients who were identified with calvaria, skull base, or facial skeleton metastasis from HCC, which formed the basis of this review. In our review of published literature, a total of 59 patients with skull metastasis from HCC were found.Citation1,Citation3,Citation7,Citation8,Citation10–Citation53 The incidence of skull metastasis from HCC in the period between 1990 and 2011 was significantly increased compared to incidence in the period between 1966 and 1989 (45:14, respectively) because of the prolonged survival rate of HCC patients due to the recent progress in both the diagnosis and treatment of the primary lesion after 1990. Metastases occurring in the calvarial site were more frequent than those occurring in the skull base and facial skeleton (31:16:12, respectively) (). This may be because of the fact that calvarial metastasis are more easily found and HCC cells have more affinity to calvaria. In our review, 24 cases with the skull metastases as the first symptom from HCC (24/59, 41%) and 14 cases with the solitary skull metastases from HCC (14/59, 24%) were identified (). In all 24 cases of the skull metastasis as the first symptom from HCC, almost 71% of these cases were misdiagnosed (17/24). The reason for the high rate of misdiagnosis is that the incidence of skull metastasis of HCC is low and doctors lack a full understanding of this disease. We must pay more attention to such cases in order to reduce the misdiagnosis rate, diagnose as early as possible, and give the patients best treatment to improve their prognosis and quality of life. Molecular imaging by positron emission tomography is, therefore, set to probe the molecular abnormalities that are the basis of disease and provide different additional biochemical or molecular information about primary brain tumors.Citation54,Citation55 In all, it is necessary to give each patient with a scalp mass that has invaded the skull molecular neuroimaging, such as positron emission tomography, to reduce the misdiagnosis rate and to rule out the possibility of skull metastasis from HCC.
Table 2 Summary of reported cases in the literature with skull metastases from HCC (n=59)Table Footnote*
Table 3 Summary of reported cases in the literature with skull metastases as the first symptom from HCC (n=33)
Disclosure
The authors report no conflicts of interest in this work.
References
- HsiehCTSunJMTsaiWCTsaiTHChiangYHLiuMYSkull metastasis from hepatocellular carcinomaActa Neurochir (Wien)200714918519017180305
- TangZYHepatocellular carcinomaShanghaiShanghai Scientific and Technological Education Publishing House2001
- ChanCHTrostNMcKelviePRophaelJAMurphyMAUnusual case of skull metastasis from hepatocellular carcinomaANZ J Surg20047471071315315584
- FukutomiMYokotaMChumanHIncreased incidence of bone metastases in hepatocellular carcinomaEur J Gastroenterol Hepatol2001131083108811564960
- McIverJIScheithauerBWRydbergCHAtkinsonJLMetastatic hepatocellular carcinoma presenting as epidural hematoma: case reportNeurosurgery20014944744911504122
- YenFSWuJCLaiCRClinical and radiological pictures of hepatocellular carcinoma with intracranial metastasisJ Gastroenterol Hepatol1995104134188527707
- ChangJWHowngSLSkull metastasis of primary hepatoma: case reportGaoxiong Yi Xue Ke Xue Za Zhi199176576621724474
- MurakamiRKorogiYSakamotoYSkull metastasis from hepatocellular carcinoma. CT, MR and angiographic findingsActa Radiol1995365976028519569
- KidoDKGouldRTaatiFDuncanASchnurJComparative sensitivity of CT scans, radiographs and radionuclide bone scans in detecting metastatic calvarial lesionsRadiology1978128371375663247
- SaneluxsanaSUrathamakulSRecurrent skull metastasis of hepatocellular carcinoma at 2 month post operationJ Med Assoc Thai201093Suppl 6S212S21421280537
- FukushimaMKatagiriAMoriTWatanabeTKatayamaYCase of skull metastasis from hepatocellular carcinoma at the site of skull fractureNo Shinkei Geka201038371377 [Japanese]20387580
- WooKMKimBCChoKTKimEJSpontaneous epidural hematoma from skull base metastasis of hepatocellular carcinomaJ Korean Neurosurg Soc20104746146320617094
- BairMJLeiWYChenCLElectronic images of the month. An unusual presentation of hematemesis: a presentation of maxillary metastasis from hepatocellular carcinomaClin Gastroenterol Hepatol20108e61e6220060067
- GotoTDohmenTMiuraKSkull metastasis from hepatocellular carcinoma with chronic hepatitis BWorld J Gastrointest Oncol2010216516821160825
- TrivediPGuptaAPasrichaSAgrawalGShahMIsolated skull base metastasis as the first manifestation of hepatocellular carcinoma: a rare case report with review of literatureJ Gastrointest Cancer200940101419705301
- KanaiRKubotaHTeradaTHataTTawarayaEFujiiKSpontaneous epidural hematoma due to skull metastasis of hepatocellular carcinomaJ Clin Neurosci20091613714019013817
- KimSJKimHJLeeHWHepatocellular carcinoma with metastasis to the cavernous sinus of skull base causing ptosisKorean J Gastroenterol200852389393 [Korean]19096257
- KamataniTTatemotoYTateishiYYamamotoTIsolated metastasis from hepatocellular carcinoma to the mandibular condyle with no evidence of any other metastases: a case reportBr J Oral Maxillofac Surg20084649950118272270
- ShimYSAhnJYChoJHLeeKSSolitary skull metastasis as initial manifestation of hepatocellular carcinomaWorld J Surg Oncol200866618570669
- HsuSYChangFLSheuMMTsaiRKHomonymous hemianopia caused by solitary skull metastasis of hepatocellular carcinomaJ Neuroophthalmol200828515418347460
- HirunwiwatkulPTirakunwichchaSMeesuaypongPShuangshotiSOrbital metastasis of hepatocellular carcinomaJ Neuroophthalmol200828475018347459
- MorofujiYMatsuoTToyodaKSkull metastasis of hepatocellular carcinoma successfully treated by intraoperative photodynamic diagnosis using 5-aminolevulinic acid: case reportNo Shinkei Geka200735913918 [Japanese]17867312
- HuangSFWuRCChangJTIntractable bleeding from solitary mandibular metastasis of hepatocellular carcinomaWorld J Gastroenterol2007134526452817724815
- KimSRKandaFKobesshoHHepatocellular carcinoma metastasizing to the skull base involving multiple cranial nervesWorld J Gastroenterol2006126727672917075993
- EscardaAVaquerPBonetLMiralbésSGómezCObradorAClivus metastasis from hepatocarcinoma associated with transarterial hepatic chemoembolizationGastroenterol Hepatol200629401404 [Spanish]16938255
- De SimonePCarraiPMorelliLPosttransplant hepatocellular carcinoma metastasis at a skull trauma siteTransplantation2005801358135916314812
- KawaharaITsutsumiKHiroseMMatsuoYYokoyamaHSkull metastasis of hepatocellular carcinoma: case reportNo Shinkei Geka200533903909 [Japanese]16164187
- NamSWHanJYKimJISpontaneous regression of a large hepatocellular carcinoma with skull metastasisJ Gastroenterol Hepatol20052048849215740500
- JegouJPerruziPAravEPluotMJaussaudRRemyGCutaneous and bone metastases revealing hepatocarcinomaGastroenterol Clin Biol200428804806 [French]15646542
- TorresMAlvarezRLópezDTitóLHepatocellular carcinoma skull metastasis with both extradural and subcutaneous extensionJ Hepatol20023656911943432
- AungTHPoYCWongWKHepatocellular carcinoma with metastasis to the skull base, pituitary gland, sphenoid sinus, and cavernous sinusHong Kong Med J20028485111861994
- NeffBAPribitkinEAWillcoxTOJrHepatocellular cancer metastatic to the zygoma: primary resection and immediate reconstructionEar Nose Throat J200281575811816393
- KleinjungTHeldPMetastasis in the frontal skull base from hepatocellular carcinomaHNO200149126129 [German]11270194
- HayashiKMatsuoTKuriharaMDaikokuMKitangeGShibataSSkull metastasis of hepatocellular carcinoma associated with acute epidural hematoma: a case reportSurg Neurol20005337938210825524
- IsakaTNakagawaHSuzukiTYamadaJWadaKKadotaTSuccessful removal of a giant skull base metastasis from hepatocellular carcinoma after direct ethanol injection: case reportSkull Base Surg200010818617171106
- ShibukawaMInagawaTKatohYTokudaYOhbayashiNYoshiokaYA case of cranial metastasis of hepatocellular carcinomaNo To Shinkei19954710871091 [Japanese]7495615
- MomojiJShimabukuroHHigaTTodaTA rare case of cranial metastasis from hepatocellular carcinomaNo Shinkei Geka1995239971002 [Japanese]7477723
- RaoulJLLe SimpleTLe PriséEMeunierBBen HasselMBretagneJFBone metastasis revealing hepatocellular carcinoma: a report of three cases with a long clinical courseAm J Gastroenterol199590116211647611219
- TranfaFCennamoGRosaNDe RosaGBoscainoABonavolontàGAn unusual orbital lesion: hepatoma metastatic to the orbitOphthalmologica19942083293327845650
- YoshidaDChenMNAwayaSNakazawaSCranial metastasis of hepatocellular carcinoma in a female: case reportNeurol Med Chir (Tokyo)1993338398447512232
- KatoHHashimotoMKobayashiTOhmoriKFukuiTSunagaTA case of hepatocellular carcinoma with the skull metastasisNihon Shokakibyo Gakkai Zasshi19928913191322 [Japanese]1320145
- NakagawaYYoshinoESuzukiKTatebeAAndachiHSpontaneous epidural hematoma from a hepatocellular carcinoma metastasis to the skull: case reportNeurol Med Chir (Tokyo)1992323003021378949
- NakaoNKuboKMoriwakiHCranial metastasis of hepatocellular carcinoma associated with chronic epidural hematoma: case reportNeurol Med Chir (Tokyo)1992321001031376859
- KnöbberDJahnkeVMetastasis to the ENT areaHNO199139263265 [German]1657838
- KuratsuJMurakamiMUemuraSUshioYBrain and skull metastases of hepatic or pancreatic cancer: report of six casesNeurol Med Chir (Tokyo)1990304764821701858
- KanazawaHSatoKGingival metastasis from primary hepatocellular carcinoma: report of a case and review of literatureJ Oral Maxillofac Surg1989479879902668472
- OgasawaraHInagawaTYamamotoMKamiyaKMondenSCranial metastasis of hepatocellular carcinoma: case reportNo Shinkei Geka19881614791482 [Japanese]2852309
- NakaoSSatoSFukumitsuTOgataMShiraneHCranial metastasis of hepatocellular carcinoma. Report of three casesNeurol Med Chir (Tokyo)198525229234 [Japanese]2409470
- ReixachRGalvánPLamarcaJCranial metastasis and hepatic tumor. Report of an anatomo: clinical caseRev Clin Esp1983171211213 [Spanish]6322247
- YasunagaATsujimuraMShibataSSimple metastasis of hepatocellular carcinoma to the skull: a case reportNo Shinkei Geka1982106556586289152
- ChangYCChenRCCraniospinal and cerebral metastasis of primary hepatomas: a report of 7 casesTaiwan Yi Xue Hui Za Zhi197978594604226652
- SarrazinABousquetOVaillantJMBrocheriouCTrinh-Dinh-HyMandibular metastasis revealing a hepatomaAnn Med Interne (Paris)19741256164 [French]4135831
- MényéPAOdoulamiHAtanganeSBile-secreting cranial metastasis revealing an undiscovered primary liver cancerBull Soc Med Afr Noire Lang Fr197015235240 [French]4339399
- SchallerBJCorneliusJFSanduNBuchfelderMMolecular imaging of brain tumors personal experience and review of the literatureCurr Mol Med2008871172619075670
- SchallerBJModoMBuchfelderMMolecular imaging of brain tumors: a bridge between clinical and molecular medicine?Mol Imaging Biol20079607117203238