Abstract
Background
Repetitive transcranial magnetic stimulation (rTMS) of the dorsolateral prefrontal cortex (DLPFC) appears to have short-term antidepressant properties. The aim of the current study was to update our previous meta-analysis and to investigate factors associated with the antidepressant properties of rTMS.
Method
Following a systematic literature search conducted in Medline and PsycInfo, N=14 sham-controlled, parallel design studies (published after 2008 to August 2013) that had utilized rTMS of the DLPFC in major depression were included in the current meta-analysis. The sensitivity and moderator analyses also included data from N=40 studies (published in 1997–2008) from our previous meta-analysis. The effect size (Cohen’s d) in each study was the standardized difference in mean depression scores (on Hamilton Depression Rating Scale, Beck Depression Inventory, Montgomery Åsberg Depression Rating Scale) from baseline to final (after last session) in rTMS compared to sham groups.
Results
According to a random-effects model with inverse-variance weights, depression scores were significantly reduced after rTMS compared to sham in studies published from 2008–2013 based on N=659 patients (overall mean weighted d=−0.42, 95% confidence interval: −0.66, −0.18, P=0.001). Combining studies from our past and current meta-analyses (published in 1997–2013; N=54) revealed that depression was significantly reduced after left-fast (>1 Hz), right-slow (≤1 Hz), and bilateral (or sequential) rTMS of DLPFC compared to sham. Significant antidepressant properties of rTMS were observed in studies with patients who were treatment resistant, unipolar (or bipolar), non-psychotic, medication-free (or started on antidepressants concurrently with rTMS). According to univariate meta-regressions, depression scores were significantly lower in studies with more female patients and fewer stimuli per session. There was little evidence that publication bias occurred in the analysis.
Conclusion
According to this study, the largest meta-analysis to date, short-term antidepressant properties of rTMS are independent of concurrent antidepressants and might depend on sex and the number of stimuli per session.
Background
A large volume of academic publications has been dedicated to the antidepressant properties of repetitive transcranial magnetic stimulation (rTMS) in the treatment of major depression. Our search of the Medline and PsycInfo databases identified N=963 sources (duplicates excluded) with terms “rTMS” and “depression” in their titles or subject between (any date to September 2013). A vast majority of these sources are narrative literature reviews largely suggesting that approximately ten sessions of daily rTMS appear to be effective in acute cases of major depression (or major depressive episode) in the short-term (by comparing depression scores before the first versus after the last session of rTMS). However, the exact factors mediating the antidepressant properties of rTMS are still not well understood. According to randomized-controlled trials (RCTs) and open-label studies conducted on mostly unipolar patients, rTMS was more effective in patients who were younger,Citation1,Citation2 less treatment-resistant (in the current episode or with less prior treatment failures),Citation1,Citation3–Citation5 with a shorter current episode,Citation3,Citation5 and without a comorbid anxiety disorder.Citation5 Furthermore, extension trials in patients who failed to respond during the short-term, double-blind phases of studies showed that the antidepressant response to rTMS was superior in female patients,Citation5 was observed only after longer stimulation periods (such as 4 weeks or more),Citation5,Citation6 and required an alteration in the stimulation site and frequency (from left-fast to right-slow rTMS of dorsolateral prefrontal cortex [DLPFC]).Citation6
Surprisingly, the antidepressant predictors of rTMS from the primary studies listed above have not been systematically confirmed in the relevant 17 quantitative meta-analyses (published 2001–2013) of the high-quality primary studies (sham-controlled randomized trials).Citation7–Citation23 According to the meta-analyses to date, the short-term antidepressant properties were most consistently observed in studies using the fast (>1 Hz) rTMS of the left DLPFC.Citation22,Citation24 The slow (≤1 Hz) rTMS of the left or right DLPFC and bilateral or sequential designs were also effective at reducing depression severity in the short-term but were utilized in only very few primary studies.Citation14,Citation18,Citation19,Citation21,Citation23
Similarly to the RCTs, the benefit of longer study designs (with ten or 15 rTMS sessions) in treating depression has already been noted in the earlier meta-analyses.Citation9,Citation12,Citation15 However, neither duration of study and other rTMS parameters (frequency of stimulation, motor threshold, stimuli/session, total stimuli) nor mean age of patients were associated with the effect sizes in meta-analyses.Citation8,Citation14,Citation17,Citation19,Citation20,Citation23 Furthermore, rTMS was effective in studies with medicated or medication-free patients,Citation11,Citation14,Citation19,Citation22,Citation23 as well as in studies with medication-resistant patients.Citation14,Citation16,Citation17,Citation20 However, a better outcome was expected with less resistance.Citation8,Citation15 Finally, the antidepressant effect of rTMS was higher in studies with non-psychotic patientsCitation19 but was similar in studies with unipolar versus bipolar patients.Citation20,Citation23
One reason for such inconsistent findings is that most past meta-analyses included too few studies to reliably detect any differences in effect sizes based on study characteristics (clinical and/or rTMS parameters). Furthermore, unlike in meta-analyses, predictors of rTMS response were often identified during different (open-label and/or follow-up) phases of primary studies. Finally, meta-analyses were computed based on group data compared to primary studies that had utilized individual patient data.
In an attempt to improve the statistical power of the past analyses, we have conducted a meta-analysis on N=40 sham-controlled studies selected from the past 13 meta-analysesCitation4,Citation7–Citation14,Citation16–Citation19 published between 2001 and 2010. A short-term antidepressant effect of the left-fast rTMS of DLPFC was univariately observed in studies with higher proportions of female patients not controlling for any other study characteristics (clinical and/or properties of rTMS). The antidepressant effect of the left-fast rTMS was also present in studies with patients who were medication-free, unipolar (or bipolar), treatment-resistant and without psychotic features.
The current study had three main aims. Since our previous meta-analysis included primary studies published up to 2008, the first aim of the current study was to update our results by conducting a new meta-analysis of the short-term effects of rTMS in depression in studies published after 2008 until August 2013. These “new” studies were located using a novel systematic literature search in contrast to the N=40 “old” studies in our previous meta-analysis that were selected from the past 13 meta-analyses published in 2001–2010. Thus, the second aim of the current study was to compare the overall mean weighted effect sizes of the “old” studies with the “new” studies due to the different methods of searching for primary studies utilized in the two meta-analyses. Furthermore, our previous meta-analysis focused on the characteristics of studies that had utilized only the left-fast rTMS of DLPFC. Thus, the third aim of the current analysis was to find out if any patient characteristics or rTMS parameters would be associated with the short-term antidepressant properties of rTMS in all “new” and “old” sham-controlled studies published between September 1997 and August 2013. The reason for combining all studies was to improve the statistical power of all statistical (moderator and subgroup) analyses.
Based on our and other past meta-analyses, it was hypothesized that depression would be reduced following the active rTMS compared to sham in the “new” studies (those after 2008). It was expected that such an antidepressant effect would be higher in the “new” compared to the “old” studies if the quality of the more recent studies has improved due to more advanced stimulators and better established parameters of rTMS. Based on our past meta-analysis of the left-fast rTMS studies, it was expected that, when combining all studies regardless of rTMS parameters, depression scores would be significantly reduced in studies with higher proportions of female patients. We also expected that, based on results from primary studies, the antidepressant properties of rTMS could be related to other patient characteristics and/or rTMS parameters if the statistical power of such comparisons were improved by adding the “new” studies to the “old” ones.
Methods
Systematic literature search and study selection
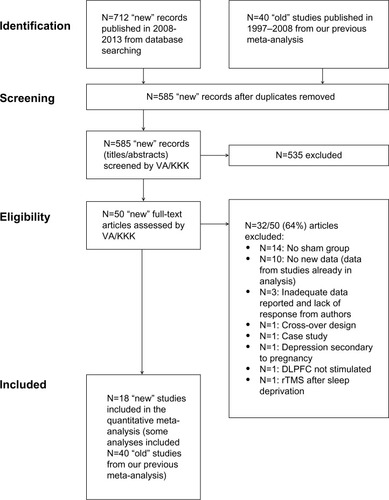
The details of the systematic literature search are shown in . A “control search” was first conducted in the PsycInfo and Medline databases for N=40 studies published between 1995 and 2008 that were included in our previous meta-analysis. These N=40 studies were obtained from the past 13 meta-analyses (published 2001–2010) rather than from a systematic literature search (). Since all N=40 studies were located during the control search, we concluded that these two databases were adequate for performing the current literature search for studies published in (any month of) 2008 until August 2013.
Table 1 Details of the systematic search strategy (all searches were performed in English with no language restrictions)
The results of the systematic literature search and the study selection procedure are summarized in the PRISMA flowchart ().Citation25 Following the exclusion of irrelevant studies (based on titles and abstracts), N=50 primary studies were assessed in full-length ( and ). A total of N=18 out of 50 “new” studies (published 2010–2013) located during our systematic search met the inclusion criteria for the current analysis (none of the studies published in 2009 met the inclusion criteria). Most studies were excluded because they were not sham-controlled or contained data published in other studies already included in the current analysis (other exclusion criteria are listed in ). The inclusion criteria for the current meta-analysis were:
Figure 1 Study assessment and exclusionary criteria.
sham-controlled parallel design;
major depressive disorder or episode diagnosed according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) or International Statistical Classification of Diseases and Related Health Problems (ICD-10) criteria;
depression severity assessed using any version of a standardized scale (Hamilton Depression Rating Scale (HAMD),Citation26 Beck Depression Inventory (BDI),Citation27 and Montgomery Åsberg Depression Rating Scale (MADRSCitation28));
and active rTMS and sham administered at the same location of DLPFC (left, right, or bilateral).
As explained in the Results section, four of the 18 “new” studies were identified as outliers and removed from all analyses. Thus, the current meta-analysis was performed on N=14 “new” studies. To improve the power of comparisons, the sensitivity analyses also included data from N=40 “old” studies (published in 1997–2008) from our previous meta-analysis ().
Data extraction
Data were extracted from all N=18 studies by two authors (VA and KKK) independently and any inconsistencies were resolved (there were no major inconsistencies requiring additional experts’ opinion). The rTMS parameters are shown in , and the clinical and demographic characteristics of patients are shown in .
Table 2 rTMS parameters in the N=18 studies included in the current meta-analysis
Table 3 Patient characteristics and depression scores in the active rTMS and sham groups in N=18 studies
Meta-analysis
The mathematical approach used in the current meta-analysis is based on the method of Hedges et al.Citation29 The mean depression scores at baseline as well as after the last session (final) in the sham and the active rTMS groups in each study are listed in . The mean (M) and standard deviations (SD) of depression scores in the sham and the active rTMS groups were computed for each group separately in SPSS version 21 (IBM Corporation, Armonk, NY, USA) using the difference score (depression score at baseline – final). These difference scores and their SD are shown in the last two columns of . Multiple independent subgroups of patients were combined into one active rTMS and one sham group per scale and per study to comply with the assumption of meta-analysis that each study should contribute only one effect size to the overall analysis. These combined scores appear in rows labelled “all” in .
The meta-analysis was computed using Comprehensive Meta-Analysis 2.0 (CMA; Biostat Inc., Englewood, NJ, USA). If one study utilized multiple depression scales then multiple effect sizes based on each scale were computed; these effect sizes were combined into one effect size per study using an arithmetic mean. The effect size used in the current analysis was the standardized mean difference (Cohen’s d) between depression scores at baseline to final after sham compared to active rTMS. The interpretation criteria for the absolute size of Cohen’s d are: d=0.20–0.49 (small), d=0.50–0.79 (moderate), and d≥0.80 (large).Citation30
The current study utilized the random-effects model of meta-analysisCitation29 with the inverse-variance weights (a sum of the within- and between-study variance).Citation31 The overall mean weighted effect size d of all studies was the sum of the product of all effect sizes and weights divided by the sum of all weights.Citation29 Negative values of d indicated that rTMS had antidepressant properties compared to sham.
The heterogeneity among the effect sizes was investigated using a Q statistic and an I2 index (I2=100%×(Q−df)/Q with df=k−1; k=number of studies).Citation29 The I2 index shows the variability in effect sizes due to real (rather than chance) differences among studies and can be interpreted using the following criteria: 25% (little heterogeneity due to real differences among studies), 50% (moderate heterogeneity), and 75% (high heterogeneity).Citation32
Sensitivity and moderator analyses
The stability of the overall mean weighted d over time was investigated as one study at a time was added to all previous studies (cumulative analysis) and as one study at a time was removed from the overall analysis (one study removed analysis). The moderator analyses (subgroup analyses and univariate meta-regressions) were used to test the influence of systematic differences among studies (clinical characteristics or patients and rTMS parameters) on the overall mean weighted d.
Publication bias analyses
Publication bias was assessed using methods available in CMA (Biostat). The Rosenthal’s Fail-Safe NCitation33 was computed to find out the number of studies (theoretically missing from the current analysis) required to lower the overall mean weighted d to zero in the current analysis. The Duval and Tweedie’s Trim-and-Fill analysisCitation34 was used to test if the so-called funnel plot of d versus standard error of the mean (SEM)/studyCitation35 was symmetrical around the overall mean weighted d of all studies. Finally, the Begg and Mazumdar Rank Order Correlation (Kendall’s tau b) between the standardized d versus SEM in each study,Citation36 and the Egger’s regression of 1/SEM (predictor) on the standardized d, Citation37 were used to test whether smaller studies differ systematically (significantly) from the larger studies. It was assumed that publication bias might be present if the Fail-Safe N is low, the funnel plot is asymmetrical, Begg and Mazumdar Correlation is statistically significant, and/or the intercept of the regression line significantly deviates from zero, causing an asymmetry of the funnel plot.Citation29
Results
An inspection of the weighted effect sizes d for each of the N=58 studies revealed that N=4 studies (all “new” studies)Citation38–Citation41 were outliers in the current analysis. Specifically, weighted ds in these studies were statistically significantly higher than the overall mean weighted d of all other studies ( and ). As a consequence, the overall mean weighted d was inflated when these studies were included in the meta-analysis of the N=18 “new” studies (d=−0.80) compared to when these studies were removed from the analysis (N=14 “new” studies: d=–0.42; ). Thus, these N=4 “new” studies were excluded and all subsequent analyses were computed using N=14 “new” studies.
Table 4 Results of the random-effects meta-analysis of the N=14 “new” studies (2010–2013) and all N=54 studies: N=40 “old” studies (1997–2008) and N=14 “new” studies
One of the four studiesCitation39 might have been an outlier because of the following methodological differences between this and all other studies: the use of a clinical interview for HAMD scale (rather than HAMD scale alone), depression diagnosed using ICD-10 (rather than DSM-IV), inclusion of high proportions of patients with bipolar (30%) and psychotic depression (68%; ). The reasons why the other three studies might have been outliers are addressed in the Discussion section.
The N=14 “new” studies were conducted in nine countries (three each in the US and People’s Republic of China; two in Spain; one each in France, Italy, Turkey, India, Canada, and Australia; ). These studies were conducted on a total of N=659 patients in the active rTMS (N=340) and sham (N=319) groups. All patients had diagnoses of a major depressive episode and/or disorder according to DSM-IV or ICD-10 (). There was little evidence that the publication bias systematically affected the results of the current analysis ().
There was a moderate antidepressant effect of rTMS because the change in mean depression scores from baseline to final was significantly higher after rTMS compared to sham in the N=14 “new” studies (d=−0.42; and ). The “new” studies did not show a superior antidepressant effect of rTMS compared to the “old” studies because the overall mean weighted d did not significantly differ between the two groups of studies (“old” d=−0.54 versus “new” d=−0.42; P=0.151; ).
Figure 2 Random-effects meta-analysis of N=14 “new” studies (2010–2013) comparing the change in mean depression scores on HAMD, BDI, and/or MADRS (baseline – final), after rTMS versus sham.
Abbreviations: BDI, Beck Depression Inventory; CI, confidence interval; HAMD, Hamilton Depression Rating Scale; MADRS, Montgomery Åsberg Depression Rating Scale; rTMS, repetitive transcranial magnetic stimulation; SEM, standard error of mean; Std diff, standardized mean difference d.
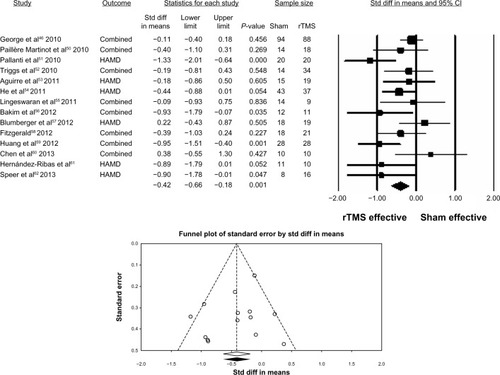
The 50% heterogeneity in the effect sizes among the N=14 “new” studies () was probably due to methodological differences among these studies in terms of depression scales used (HAMD in all N=14 studies, MADRS in N=6 studies, and BDI in N=3 studies), clinical characteristics of patients (), and different parameters of rTMS (). Some of the N=14 “new” studies did not report the above characteristics ( and ) and thus the percentage scores shown below are computed based on studies with valid responses only.
The N=40 “old” studies and the N=14 “new” studies were conducted on mostly middle-aged patients (aged 40 years old and above). Similarly to the “old” studies, 50% of the “new” studies utilized 60% or more female patients per study.
Like the “old” studies, most of the “new” studies were conducted on patients with ():
treatment-resistance, defined as a failure to respond to or tolerate ≥2 antidepressant trials (N=8/9, 89% of studies),
non-psychotic depression (N=8/9, 89% of studies), and
concurrent antidepressant treatment (N=11/14, 79% of studies). Of these N=11 studies, most included patients on stable doses of antidepressants (N=10/11 studies). Antidepressants were started on day 1 of the study in only N=1/11 studies.
In contrast to the majority of “old” studies that had included any proportions of bipolar patients, the “new” studies were mostly conducted on patients with unipolar depression (N=8/12, 67% of studies).
The current results also suggest that similar properties of rTMS have been used over the last 16 years of research on depression (in studies published in 1997–2013). Similarly to the “old” studies, the most commonly utilized rTMS parameters among the “new” studies were: 10 Hz frequency of stimulation (N=5/14, 36% of studies), 110% motor threshold stimulation (N=4/13, 41% of studies), 800 or 1,600 stimuli/session (N=4/10, 40% of studies), 20 trains/session (N=6/13, 46% of studies), a 70 mm stimulating coil diameter (N=4/5, 80% of studies), and a figure-of-eight shape of the stimulating coil (N=13/13 studies). In contrast to the 10 rTMS sessions most commonly used among the “old” studies, the “new” studies most often utilized longer paradigms of 15 sessions (N=6/14, 43% of studies).
Interestingly, even though the new “sham-coils” improve the blinding of studies and prevent stimulation of the brain due to an inbuilt magnetic shield, these coils have not been commonly used in the “new” studies yet (possibly due to a high cost of replacing the older stimulators with the newest ones). In fact, similarly to the “old” studies, the most common sham practice among the “new” studies was to tilt the active coil by a 90° angle from the scalp (N=6/14, 43% of studies).
Finally, just like the “old” studies, the left-fast rTMS (>1 Hz) of the DLPFC was the most common combination of the location-frequency of rTMS among the “new” studies (N=10/14, 71% of studies), followed by the bilateral or sequential rTMS (N=3/14, 21% of studies), and the left-slow (≤1 Hz), right-slow, and right-fast rTMS that were utilized in one study (7%) each.
Since there were too few “new” studies, we have combined all “old” and “new” studies (total N=54) to conduct moderator and subgroup analyses. The results of these analyses are shown in .
Table 5 Random-effects subgroup analyses and meta-regressions of the change in depression scores (baseline – final) after rTMS compared to sham in N=54 sham-controlled studies published in 1997 – August 2013
The overall mean weighted d=−0.51 in all N=54 studies suggests that rTMS was only moderately better than sham at reducing depression scores over the last 16 years in a total of 2,242 patients in 17 countries (; ; ). Even though only moderate, this overall effect size became stable around −0.50 to −0.54 over the last 8 years as studies were removed from the analysis one at a time (), or cumulatively added to the analysis ().
Univariate comparisons of subgroups of studies based on common study properties showed that no one specific characteristic was superior in terms of producing higher antidepressant effects. For example, except for the right-fast rTMS of the DLPFC that was utilized in only one study, all combinations of the location-frequency of rTMS were effective at significantly reducing depression scores compared to sham (). There was a non-significant trend toward higher overall mean weighted effect sizes in studies with non-treatment resistant patients compared to those with treatment-resistant patients (). rTMS was also similarly effective in studies with unipolar depression compared to studies with generally low proportions of bipolar patients (). However, it remains unclear if the antidepressant properties of rTMS extend to psychotic depression because there were too few studies with low proportions of patients with psychotic depression in the current analysis (N=5; ).
According to the current results, the antidepressant effect of rTMS was probably not secondary to concurrent antidepressants. shows that depression was reduced after rTMS compared to sham in studies with patients who were medication-free or started on antidepressants concurrently with rTMS on day 1 of a study. Overall mean weighted effect sizes did not differ statistically between studies with medicated versus medication-free patients ().
The current study also shows that depression was reduced after rTMS compared to sham using both stimulating coil shapes (figure-of-eight or circular) and various sham designs. Although studies using sham coils produced the highest overall mean weighted effect size (d=−0.63; ) compared to all other sham designs, more than N=10 studies using sham coils are needed to statistically confirm the superiority of this blinding method. Compared to sham coils, tilting of active coils at 45° or 90° from the scalp was the most commonly used sham practice in studies published until August 2013 (). The most commonly used stimulators were the MagStim (UK; N=28/54, 52% of studies) and the MagPro (USA; N=10/54, 18% of studies) models.
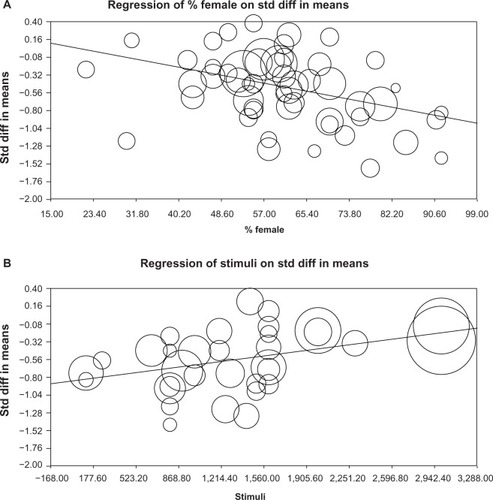
Finally, seven univariate meta-regressions were conducted to find out if any demographic characteristics of patients (mean age/study and proportion of female patients/study) or rTMS parameters (frequency of stimulation, motor threshold, total number of sessions, stimuli/session, trains/session) could predict a change in the effect sizes weighted according to the random-effects model. Two regressions showed that the antidepressant effect of rTMS was superior in studies with more female patients and fewer stimuli per session (; ). However, a change in weighted ds could not be significantly predicted using the mean age of all patients per study, frequency of stimulation, motor threshold, or a total number of sessions as predictors. Predictors “stimuli/session” and “% female patients” explained 91% and 52% of the between-study variability in effect sizes, respectively.
Figure 3 Univariate random-effects meta-regressions of various study characteristics used as predictors (proportion of female patients/study and stimuli/session) on the weighted effect sizes d (the outcome) in studies published in 1997–2013.
Abbreviations: rTMS, repetitive transcranial magnetic stimulation; Std diff, standardized mean difference d.
Discussion
The current meta-analysis conducted on N=54 studies published in 1997–2013 showed that rTMS has a short-term antidepressant effect that is superior in studies with more female patients and fewer stimuli per session ( and ). The most commonly used characteristics of patients and rTMS parameters in the sham-controlled studies over the last 16 years (1997–2013) included in the current analysis were: at least 60% female patients/study in half of all studies (range: 22%–92%); mostly middle-aged or older patients (range of the mean age of all patients per study: 39–62 years); fast (>1 Hz) stimulation of the left DLPFC; frequency of 10 Hz; 110% motor threshold; figure-of-eight coil with 70 mm diameter; 1,600 stimuli/session; 20 trains/session; and 10 sessions/study (although the more recent studies published after 2008 most commonly used longer protocols of 15 sessions/study). The most commonly used sham strategy was tilting of the active coil at the 90° angle from scalp (). Most of the studies to date included proportions of patients with treatment resistance, on concurrent antidepressants (particularly at the stable dose), with bipolar and non-psychotic depression ().
It is likely that sex plays a role in the short-term response to the left-fast rTMS because 80% of all studies in the current meta-analysis utilized this combination of rTMS parameters (). This result confirms another univariate finding that out of patients who failed to respond to a 4-week, double-blind phase of rTMS in a large RCT,Citation42 only females showed a superior response to rTMS during the extension (open-label) phase of the study.Citation5 However, such a response to treatment was probably related to a combination of factors rather than sex alone. This is because the patients in the RCT were unipolar, non-psychotic, medication-free, moderately–severely treatment-resistant, and required more than four weeks of treatment to respond to rTMS.Citation5 Another open-label study also showed that the improved response to rTMS in females depended on younger (premenopausal) age and the ovarian hormonal levels.Citation43 Such a result is not surprising because depression has a strong hormonal component.Citation44,Citation45 Thus, it can be speculated that the superior effect of sex in our meta-analysis was also due to younger age of female patients, and other factors (such as less severe unipolar depression and/or medication-free status). However, such confounding factors can be investigated only to a limited extent in meta-analyses that are computed on data. It should be possible to compute multiple meta-regressions on group data as new studies using rTMS become available in the future, providing that these studies report the characteristics of their patients and/or rTMS properties used.
The second important finding in the current meta-analysis is that the short-term antidepressant properties of rTMS were observed in studies using fewer stimuli per session according to a univariate meta-regression ( and ). Other meta-analyses showed that the efficacy of rTMS was not associated with the number of stimuli/session nor total stimuli.Citation14,Citation19,Citation20,Citation23 The initial negative correlation between the effect sizes and the total number of stimuli in one meta-analysisCitation20 was attributed to one large RCT only.Citation42 Similarly, this and another large RCTCitation42,Citation46 contributed to the additional significant univariate meta-regression of the total number of stimuli (computed as “stimuli per session” × “total sessions” per study based on the data shown in ) on weighted d in the current analysis (). However, the meta-regression of stimuli/session on weighted d remained unchanged after the removal of the same two RCTsCitation42,Citation46 in the current analysis (). In general, the findings from the two largest RCTsCitation42,Citation46 suggest that the initially non-responsive patients appear to indeed require more than 15 rTMS sessions with a high number (3,000) of stimuli/session to show a response to rTMS. However, the results of the current meta-analysis suggest that the short-term response to rTMS (during the double-blind phase of the study) might require fewer stimuli per session. Again, based on the current results, it can only be speculated that particularly the less treatment-resistant female patients require fewer stimuli per session in the short (up to 10 sessions), left-fast rTMS paradigms to demonstrate the antidepressant response to rTMS.
Interestingly, some evidence in support of the speculation above can be found in three of the four studies classified as outliers in the current analysis. Specifically, a large antidepressant effect of rTMS was observed in the total of N=86 patients (63%–65% males) on concurrent antidepressants, with unipolar, non-psychotic depression, and with moderate–severe treatment-resistance using long (20 sessions), left-fast paradigms with a high number (3,000) of stimuli/session.Citation38,Citation40,Citation41 Therefore, in contrast to female patients, male patients with more severe major depression might require longer, left-fast paradigms with more stimuli per session to show an antidepressant response to rTMS during the double-blind phases of studies. Furthermore, such a sex-dependent effect could also explain why the two largest RCTs to date, with similar study characteristics to those in the three outlier studies, have demonstrated only small antidepressant effects of rTMS in mostly female (medication-free) patients: d=−0.30 in N=301 patientsCitation42 () and d=−0.11 in N=190 patientsCitation46 (). Such small effect sizes might have resulted from a high quality of blinding (with sham coils) in the RCTs compared to the large effect sizes using tilted active coils in the outlier studies. Thus, future primary studies should investigate the effects of rTMS separately in both sexes controlling for severity of treatment resistance and the number of stimuli/session in the left-fast rTMS paradigms.
The significant reduction in depression scores after rTMS associated with fewer stimuli per session raises the question of whether or not the brain can be “overstimulated” during rTMS leading to a reduction in the antidepressant properties of this method. One mechanism of such an “overstimulation” could be related to the firing properties of neurons. In general, voltage-gated sodium channels are key players in membrane excitation and the production of action potentials. The classical model of sodium channel gating described by Hodgkin and Huxley suggests that a voltage-gated mechanism mediates the activation (opening of sodium channels) as well as inactivation following a refractory period during which no excitation can occur.Citation47 A strong depolarization involving a large number of neurons can inactivate sodium channels and thereby prevent further excitation for a prolonged period of time. Since neurons need to recover from firing before being able to produce new action potentials, stimulating the brain with too many stimuli might lead to a neural saturation (inability of most neurons to produce new action potentials) and consequently a reduction in antidepressant properties of rTMS. In practical terms, using shorter sessions with fewer stimuli could be less costly as well as time consuming for patients and administrators.
Univariately, the mean age of all patients (rather than age of individual patients) was not related to a better antidepressant outcome of rTMS in the current and past meta-analysesCitation14,Citation20 possibly due to the use of group data. Similarly, effect sizes were unrelated to severity of treatment-resistance or presence versus absence of treatment-resistant patients in other meta-analyses.Citation14,Citation16,Citation17,Citation20 In our analysis there was only a trend toward higher antidepressant effect of rTMS in (very few) studies with non-treatment-resistant patients compared to studies with treatment-resistant patients (). The reason for this result could be that we have not controlled for severity of illness in our meta-analysis. Furthermore, our classification of studies into subgroups was also not optimal for unipolar versus bipolar and psychotic versus non-psychotic depression. In general, very few patients had such diagnoses per study (). Thus, there was no difference in effect sizes between groups of studies with all unipolar and all non-psychotic patients compared to studies with mostly unipolar and mostly non-psychotic patients, respectively (). Other meta-analyses have also found no differences in effect sizes or response and remission rates between studies with unipolar compared to bipolar patients.Citation14,Citation23 While effect sizes were higher in studies with non-psychotic versus psychotic patients in one meta-analysis,Citation19 such result was not confirmed by another meta-analysis,Citation14 possibly due to including studies with unknown psychosis status in the non-psychotic group.
The short-term antidepressant effect of rTMS was not secondary to concurrent antidepressants in the current analysis. Specifically, it was observed in studies with patients who were all medication-free or who started on antidepressants concurrently with rTMS (). However, the current analysis did not confirm the finding from other meta-analyses that the short-term response to rTMS was higherCitation23 or tended to be higherCitation19 in studies using rTMS as monotherapy versus an add-on therapy. The reason for this result might be that we have not controlled for proportions of patients on concurrent antidepressants in the add-on studies.
According to our results depression severity was reduced after rTMS compared to sham in studies using different rTMS properties, such as different stimulating coils (figure-of-eight or circular), different sham paradigms, and different combinations of the location (right or left) and frequency (slow or fast) of DLPFC stimulation (). Although blinding is facilitated by the use of shielded sham coils that resemble active coils visually and produce similar auditory effects while not stimulating the brain,Citation48 these coils were still not commonly used compared to tilting of active coils (possibly due to high costs of replacing the older with newer equipment). Furthermore, except for five studies, all other studies used the “5 cm rule” to define the position of the DLPFC () in the current analysis. Even though it is so frequently used, the “5 cm rule” is less accurate than the 10–20 EEG (electroencephalogram) system and the magnetic resonance image (MRI)-guided neuronavigation.Citation49 Therefore, the antidepressant properties of rTMS could be further strengthened by the use of either MRI or the F5 location of the EEG system.Citation49
The moderate effect sizes in the current and most other meta-analyses on this topic could be related to statistical methods of computing the effect sizes and performing a meta-analysis. The magnitude of effect sizes in individual studies might largely depend on the blinding quality of studies and the computation of effect sizes. Therefore, assuming that baseline depression scores are similar, the well-blinded studies could have smaller standardized differences in mean depression scores between rTMS and sham groups. This is because patients could respond to rTMS (due to its antidepressant properties) and to sham (due to placebo effect) in well-blinded studies. In contrast, the poorly-controlled studies in which patients and/or administrators guess the treatment allocation could show larger effect sizes. This time patients could respond to rTMS (guessing that they receive the real treatment) but not to sham (guessing that they receive the inactive treatment). This scenario is possible because patients can easily inform themselves about the method from the social media, for instance by watching industry-sponsored videos on YouTube directed toward the general population.
Furthermore, the past meta-analyses in this field used two general approaches to computing the effect sizes: the mean depression scores were compared before versus after rTMS or sham (in some studies controlling for baseline depression scores) using standardized mean differences (Cohen’s d or Hedges’ g), or proportions of patients who remitted after rTMS or sham versus baseline were compared using the odds ratios. None of these approaches of computing effect sizes is ideal from the statistical point of view. Mean scores could be skewed in studies with small sample sizes (<30 patients). Thus, the “true average” depression score would be shown more accurately using the mode (most commonly occurring depression score in the rTMS versus sham groups) or the median rather than the skewed mean. On the other hand, the odds ratios are also problematic because they rely on classifying patients into two groups (non-depressed versus depressed) based on a subjective cut-off on a depression scale. As a result, a patient with a score of 17 on a specific scale might be classified as “non-depressed” while another one with a score of 18 might already fall into the “depressed group” regardless of such a low difference between their scores. Furthermore, the odds ratios computed from each primary study would need to be based on the same cut-off for presence/absence of depression to reliably combine the results of these studies in meta-analysis. Therefore, the “all or nothing” classification of patients according to the odds ratio might be reliable and valid when large differences among patients’ scores occur and thus the group membership can be reliably justified. Despite the limitations above, the advantage of mean scores is that they show the severity of depression without needing a specific cut-off to classify patients into groups.
Furthermore, different methods of weighing of studies and meta-analysis were utilized in the meta-analyses to date. The weights in the current meta-analysis were computed based on variance. Therefore, studies with higher variability of scores (due to rTMS being effective at reducing depression in only some, but not all, patients) had lower weights and thus lower influence on the overall mean weighted effect size. However, other methods of meta-analysis advocate the use of other weighing methods, such as the sample size, and correcting the effect sizes in individual studies for study-related artifacts before conducing any meta-analysis.Citation29 Despite all the statistical differences, most of the past 17 meta-analyses (published 2001–2013) and the current meta-analysis report similar (moderate) weighted effect sizes (standardized mean differences or odds ratios). Therefore, it is likely that the true effect of rTMS is either only moderate or indeed even higher in clinical practice considering the statistical limitations described above.
Although no strong evidence for publication bias was detected in the current study (), the sources included in our analysis were biased toward studies published in peer-reviewed journals and written in the English language. Such an apparent bias in selection of sources was not related to the systematic search strategy (). Our search was conducted for any type of resource (published or not published) in any language (because the authors of this study are multilingual speakers of six different languages). Instead, it appears that the majority of sources on this topic on PsycInfo and Medline were indeed published in peer-reviewed journals and written in English (or at least included a title and an abstract written in English). Therefore, such a linguistic bias is probably related to the fact that PsycInfo and Medline mostly store published sources and these sources are most often written in English. However, the results of our analysis are generalizable beyond the English-speaking world because the N=54 studies were conducted in a total of 17 countries around the world (for the list see ). According to the File Drawer ProblemCitation33 studies with statistically significant results are more likely to be published while those with non-significant results remain in “file drawers” and are never published. Even though such so-called “gray (unpublished) literature” was not included, only 50% of all studies in the current meta-analysis reached the traditional significance level (). Furthermore, no checklist for the quality of studies was used in the current analysis. Instead, the quality of studies was assessed indirectly by weighing the effect sizes based on variability of scores within and between studies. It was assumed that studies with low variability of scores were of higher quality and thus contributed more weight to the overall mean weighted effect sizes and vice-versa.
Conclusion
In conclusion, the results of the current study suggest that the short-term antidepressant properties of rTMS are not secondary to concurrent antidepressants and might depend on sex and the number of stimuli per session. Depending on degree of treatment-resistance and age, male and female patients with unipolar depression might require paradigms with different properties (number of stimuli per session, total number of sessions, left-fast or other combinations of location-frequency of stimulation) to show comparable antidepressant effects. While the clinical efficacy of the fast rTMS of the left DLPFC seems to be widely accepted, the right-slow and bilateral or sequential paradigms appear to be promising alternatives in the short-term treatment of acute major depression.
Author contributions
VA conducted the systematic search and assessed all studies for inclusion with KKK. The data were independently extracted by KKK and SKR (studies up to 2008), and KKK and VA (2009–2013). VA performed the pilot analyses in SPSS/CMA, while KKK performed the final analyses in SPSS/CMA and wrote the manuscript. All authors critically revised the manuscript.
Acknowledgments
We would like to thank the authors of four studies for additional data and Ms Anja Kakau (Systems Librarian at Jacobs University) for her assistance with the literature search.
Supplementary materials
Figure S1 Random-effects meta-analysis of N=58 studies with standardized residuals and their P-values.
Notes: “All” indicates that rTMS was administered using different properties into different subgroups of patients in a study and the depression scores for such subgroups were combined. “Combined” indicates that more than one depression scale was used in a study and the effect sizes according to the multiple scales were combined). According to the P-values, 4/18 “new” studies were classified as outliers: Zheng et al 2010,Citation90 Ray et al 2011,Citation75 Peng et al 2012,Citation74 and Spampinato et al 2013.Citation81 These studies were excluded from all subsequent analyses.
Abbreviations: CI, confidence interval; HAMD, Hamilton Depression Rating Scale; MADRS, Montgomery Åsberg Depression Rating Scale; rTMS, repetitive transcranial magnetic stimulation; Std diff, standardized mean difference d; Std, standardized.
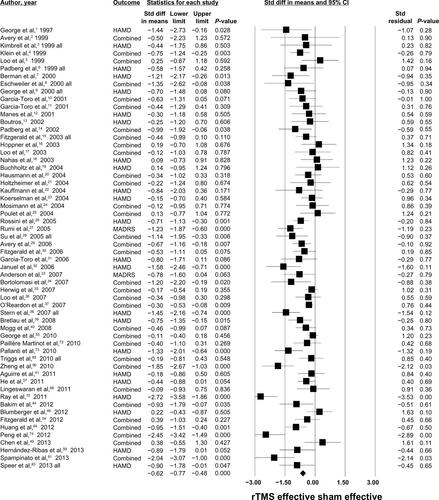
Figure S2 Forest plot showing the comparison of the N=4 outliers with N=54 studies.
Notes: Subgroup analysis using the mixed-effects model revealed that the overall mean weighted effect size d was significantly higher in the N=4 outlier studies (d=−2.26) compared to the N=54 studies (d=−0.51): Q(df 1)=58.3, P<0.001. The variability of the weighted effect sizes was high among the N=4 outlier studies (SEM =0.23) compared to the N=54 studies (SEM =0.06).
Abbreviations: CI, confidence interval; rTMS, repetitive transcranial magnetic stimulation; SEM, standard error of mean; Std diff, standardized mean difference d.
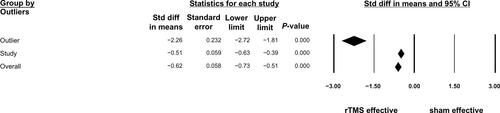
Figure S3 Random-effects meta-analysis of N=54 studies.
Notes: “All” indicates that rTMS was administered using different properties into different subgroups of patients in a study and the depression scores for such subgroups were combined. “Combined” indicates that more than one depression scale was used in a study and the effect sizes according to the multiple scales were combined). The mean number of patients per group was used in the final calculations if patients dropped out throughout the study between baseline and final sessions.
Abbreviations: CI, confidence interval; HAMD, Hamilton Depression Rating Scale; MADRS, Montgomery Åsberg Depression Rating Scale; rTMS, repetitive transcranial magnetic stimulation; Std diff, standardized mean difference d.
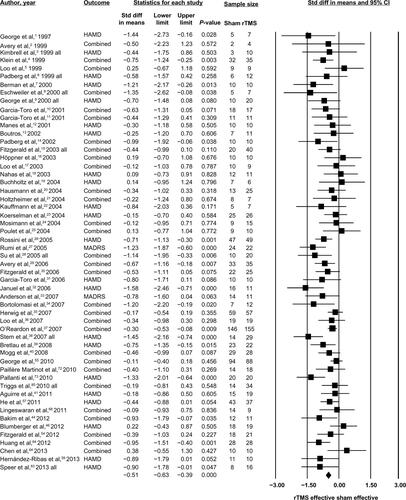
Figure S4 One study removed analysis (N=54 studies).
Notes: “All” indicates that rTMS was administered using different properties into different subgroups of patients in a study and the depression scores for such subgroups were combined. “Combined” indicates that more than one depression scale was used in a study and the effect sizes according to the multiple scales were combined). “Point” refers to the overall mean weighted d of all studies except for the study listed in each row.
Abbreviations: CI, confidence interval; HAMD, Hamilton Depression Rating Scale; MADRS, Montgomery Åsberg Depression Rating Scale; rTMS, repetitive transcranial magnetic stimulation; Std diff, standardized mean difference d.
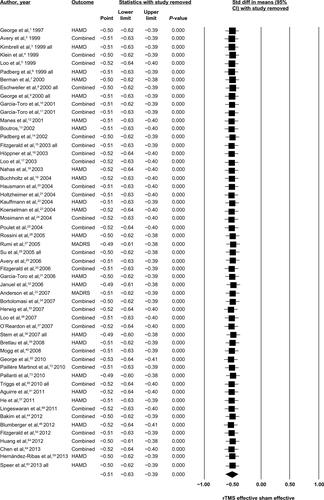
Figure S5 Cumulative meta-analysis (N=54 studies).
Notes: “All” indicates that rTMS was administered using different properties into different subgroups of patients in a study and the depression scores for such subgroups were combined. “Combined” indicates that more than one depression scale was used in a study and the effect sizes according to the multiple scales were combined). “Point” refers to the overall mean weighted d of all studies before and including the study listed in each row.
Abbreviations: CI, confidence interval; HAMD, Hamilton Depression Rating Scale; MADRS, Montgomery Åsberg Depression Rating Scale; rTMS, repetitive transcranial magnetic stimulation; Std diff, standardized mean difference d.
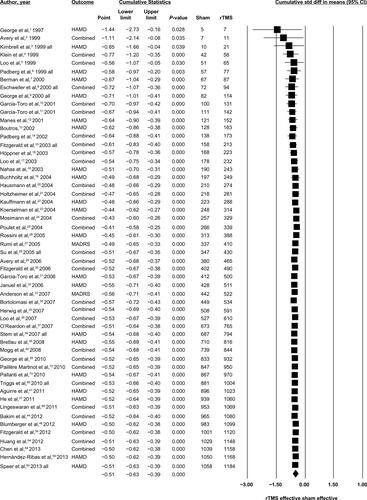
Figure S6 Univariate meta-regression of the total stimuli/study on the effect size d weighted according to the random-effects model.
Notes: Total stimuli = stimuli/session × total number of sessions. (A) The top figure shows the results of a significant meta-regression (slope P=0.015) in N=33 studies. However, the significance of this regression was due to two largest RCTs by O’Reardon et alCitation37 and George et alCitation55 (depicted as two largest circles on the right-hand side of (A). (B) These two RCTs are removed from the analysis in the bottom figure (slope, P=0.208).
Abbreviations: RCT, randomized controlled trial; std diff, standardized mean difference d.
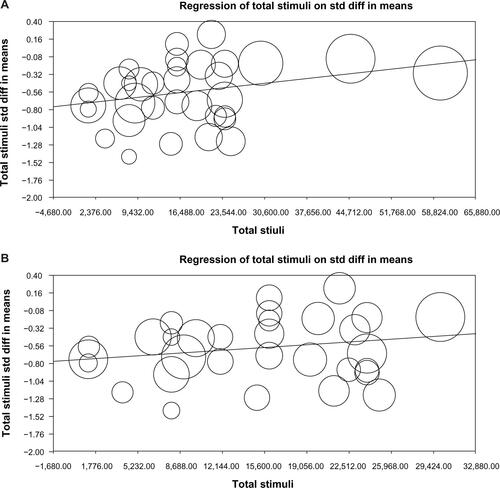
Figure S7 Univariate meta-regression of the stimuli/session on the effect size d weighted according to the random-effects model (two largest RCTs removed).
Notes: The slope of meta-regression conducted on N=31 studies remained positive and statistically significant (P=0.018) following the removal of O’Reardon et alCitation37 and George et alCitation55 studies.
Abbreviations: RCT, randomized controlled trial; std diff, standardized mean difference d.
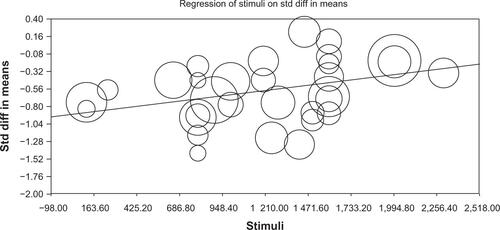
Table S1 A list of N=40 “old” studies on the association between rTMS from our previous meta-analysis (unpublished). These studies were included in sensitivity and moderator analyses in the current study
Table S2 A list of N=50 studies on the association between rTMS and depression assessed in full-length and reasons for exclusion from the current meta-analysis
Table S3 Location (country) where the N=54 studies published from 1997 to August 2013 were conducted
References
- GeorgeMWassermannEMWilliamsWEMood improvement following daily left prefrontal repetitive transcranial magnetic stimulation in patients with depression: A placebo-controlled crossover trialAmerican Journal of Psychiatry1997154175217569396958
- AveryDClaypooleKRobinsonLRepetitive transcranial magnetic stimulation in the treatment of medication-resistant depression: preliminary dataJournal of Nervous and Mental Disease1999187211411710067953
- KimbrellTLittleJDunnRFrequency dependence of antidepressant response to left prefrontal repetitive transcranial magnetic stimulation (rTMS) as a function of baseline cerebral glucose metabolismBiological Psychiatry1999461603161310624541
- KleinEKreininIChistyakovATherapeutic efficacy of right prefrontal slow repetitive transcranial magnetic stimulation in major depression: A double blind controlled studyArchives of General Psychiatry19995631532010197825
- LooCMitchellPSachdevPMcDarmontBParkerGGandeviaSDouble-blind controlled investigation of transcranial magnetic stimulation for the treatment of resistant major depressionAmerican Journal of Psychiatry199915694694810360138
- PadbergFZwanzgerPThomaHRepetitive transcranial magnetic stimulation (rTMS) in pharmacotherapy-refractory major depression: comparative study of fast, slow and sham rTMSPsychiatry Research19998816317110622338
- BermanRHoffmanRNarashimaMA randomized clinical trial of repetitive transcranial magnetic stimulation in the treatment of major depressionBiological Psychiatry20004733233710686268
- EschweilerGWegererCSchlotterWLeft prefrontal activation predicts therapeutic effects of repetitive transcranial magnetic stimulation (rTMS) in major depressionPsychiatry Research: Neuroimaging Section200099161172
- GeorgeMNahasZMolloyMA controlled trial of daily left prefrontal cortex TMS for treating depressionBiological Psychiatry20004896297011082469
- Garcia-ToroMMayolAArnillasHModest adjunctive benefit with transcranial magnetic stimulation in medication-resistant depressionJournal of Affective Disorders2001642–327127511313095
- García-ToroMPascual-LeoneARomeraMPrefrontal repetitive transcranial magnetic stimulation as add on treatment in depressionJournal of Neurology, Neurosurgery and Psychiatry200171546548
- ManesFJorgeRMorcuendeMYamadaTParadisoSRobinsonRA controlled study of repetitive transcranial magnetic stimulation as a treatment of depression in the elderlyInternational Psychogeriatrics200113222523111495396
- BoutrosNLack of a therapeutic effect of a 2-week sub-threshold transcranial magnetic stimulation course for treatment-resistant depressionPsychiatry Research2002113324525412559481
- PadbergFZwanzgerPKeckMRepetitive transcranial magnetic stimulation (rTMS) in major depression: relation between efficacy and stimulation intensityNeuropsychopharmacology200227463864512377400
- FitzgeraldPBrownTMarstonNDaskalakisZde CastellaAKulkarniJTranscranial magnetic stimulation in the treatment of depression: a double-blind, placebo-controlled trialArchives of General Psychiatry2003601002100814557145
- HöppnerJSchulzMIrmischGMauRSchläfkeDRichterJAntidepressant efficacy of two different rTMS procedures: High frequency over left versus low frequency over right prefrontal cortex compared with sham stimulationEuropean Archives of Psychiatry and Clinical Neuroscience200325310310912799750
- LooCMitchellPCrokerVDouble-blind controlled investigation of bilateral prefrontal transcranial magnetic stimulation for the treatment of resistant major depressionPsychological Medicine200333334012537034
- NahasZKozelFLiXAndersonBGeorgeMLeft prefrontal transcranial magnetic stimulation (rTMS) treatment of depression in bipolar affective disorder: a pilot study of acute safety and efficacyBipolar Disorder2003514047
- BuchholtzHVidebechPClemmensenKSturlasonRJensenHVestergaardPRepetitive transcranial magnetic stimulation as add-on antidepressant treatment. The applicability of the method in a clinical settingNordic Journal of Psychiatry200458645545716195088
- HausmannAKemmlerGWalpothMNo benefit derived from repetitive transcranial magnetic stimulation in depression: a prospective, single-centre, randomised, double blind, sham-controlled “add on” trialJournal of Neurology, Neurosurgery and Psychiatry2004752320322
- HoltzheimerPIIIRussoJClaypooleKRoy-ByrnePAveryDShorter duration of depressive episode may predict response to repetitive transcranial magnetic stimulationDepression and Anxiety200419243014978782
- KauffmannCCheemaMMillerBSlow right prefrontal transcranial magnetic stimulation as a treatment for medication-resistant depression: A double-blind, placebo-controlled studyDepression and Anxiety200419596214978787
- KoerselmanFLamanDvan DuijnHvan DuijnMWillemsMA 3-month, follow-up, randomized, placebo-controlled study of repetitive transcranial magnetic stimulation in depressionJournal of Clinical Psychiatry2004651323132815491234
- MosimannUSchmittWGreenbergBRepetitive transcranial magnetic stimulation: a putative add-on treatment for major depression in elderly patientsPsychiatry Research200412612313315123391
- PouletEBrunelinJBoeuveCRepetitive transcranial magnetic stimulation does not potentiate antidepressant treatmentEuropean Psychiatry20041938238315363481
- RossiniDMagriLLuccaAGiordaniSSmeraldiEZanardiRDoes rTMS hasten the response to escitalopram, sertraline, or venlafaxine in patients with major depressive disorder? A double-blind, randomized, sham-controlled trialJournal of Clinical Psychiatry200566121569157516401159
- RumiDGattazWRigonattiSTranscranial magnetic stimulation accelerates the antidepressant effect of amitriptyline in severe depression: a double-blind placebo-controlled studyBiological Psychiatry20055716216615652875
- SuTHuangCWeiIAdd-on rTMS for medication-resistant depression:a randomized, double-blind, sham-controlled trial in Chinese patientsJournal of Clinical Psychiatry200566793093716013911
- AveryDHoltzheimerPIIIFawazWA controlled study of repetitive transcranial magnetic stimulation in medication-resistant major depressionBiological Psychiatry20065918719416139808
- FitzgeraldPBenitezJde CastellaADaskalakisZBrownTKulkarniJA randomized, controlled trial of sequestial bilateral repetitive transcranial magnetic stimulation for treatment-resistant depressionAmerican Journal of Psychiatry2006163889416390894
- Garcia-ToroMSalvaJDaumalJHigh (20-Hz) and low (1-Hz) frequency transcranial magnetic stimulation as adjuvant treatment in medication-resistant depressionPsychiatry Research: Neuroimaging20061465357
- JanuelDDumortierGVerdonCA double-blind sham controlled study of right prefrontal repetitive transcranial magnetic stimulation (rTMS): Therapeutic and cognitive effect in medication free unipolar depression during 4 weeksProgress In Neuro-Psychopharmacology and Biological Psychiatry20063012613016242826
- AndersonIDelvaiNAshimBAdjunctive fast repetitive transcranial magnetic stimulation in depressionBritish Journal of Psychiatry200719053353417541116
- BortolomasiMMinelliAFuggettaGLong-lasting effects of high frequency repetitive transcranial magnetic stimulation in major depressed patientsPsychiatry Research2007150218118617303249
- HerwigUFallgatterAHoppnerJAntidepressant effects of augmentative transcranial magnetic stimulation. Randomised multicentre trialBritish Journal of Psychiatry200719144144817978325
- LooCMitchellPMcFarquharTMalhiGSachdevPA sham-controlled trial of the efficacy and safety of twice-daily rTMS in major depressionPsychological Medicine20073734134917176505
- O’ReardonJSolvasonHJanicakPEfficacy and safety of transcranial magnetic stimulation in the acute treatment of major depression: A multisite randomized controlled trialBiological Psychiatry2007621208121617573044
- SternWTormosJPressDPearlmanCPascual-LeoneAAntidepressant effects of high and low frequency repetitive transcranial magnetic stimulation to the dorsolateral prefrontal cortex:a double-blind, randomized, placebo-controlled trialJournal of Neuropsychiatry and Clinical Neurosciences200719217918617431065
- BretlauLLindbergLUndenMDissingSBechPRepetitive transcranial magnetic stimulation (rTMS) in combination with escitalopram in patients with treatment-resistant major depression. A double-blind, randomised, sham-controlled trialPharmacopsychiatry2008412414718311683
- MoggAPluckGErantiSA randomized controlled trial with 4-month follow-up of adjunctive repetitive transcranial magnetic stimulation of the left prefrontal cortex for depressionPsychological Medicine20083832333317935639
- AguirreICarreteroBIbarraOAge predicts low-frequency transcranial magnetic stimulation efficacy in major depressionJournal of Affective Disorders2011130346646921093060
- AveryDHHoltzheimerPE3rdFawazWTranscranial magnetic stimulation reduces pain in patients with major depression: a sham-controlled studyThe Journal of Nervous And Mental Disease2007195537838117502802
- BaekenCDe RaedtRVanderhasseltM-AA “hypersensitive” hypothalamic-pituitary-adrenal system could be indicative for a negative clinical high-frequency repetitive transcranial magnetic stimulation outcome in melancholic depressed patientsBrain Stimulation201031545720633431
- BakimBUzunUEKaramustafaliogluOThe combination of antidepressant drug therapy and high-frequency repetitive transcranial magnetic stimulation in medication-resistant depressionBulletin of Clinical Psychopharmacology2012223244253
- BaresMKopecekMNovakTLow frequency (1-Hz), right pre-frontal repetitive transcranial magnetic stimulation (rTMS) compared with venlafaxine ER in the treatment of resistant depression: A double-blind, single-centre, randomized studyJournal of Affective Disorders20091181–39410019249105
- BlumbergerDMMulsantBHFitzgeraldPBA randomized double-blind sham-controlled comparison of unilateral and bilateral repetitive transcranial magnetic stimulation for treatment-resistant major depressionThe World Journal of Biological Psychiatry201213642343521736507
- BrakemeierE-LLuborzewskiADanker-HopfeHKathmannNBajboujMPositive predictors for antidepressive response to prefrontal repetitive transcranial magnetic stimulation (rTMS)Journal of Psychiatric Research200741539540316554071
- BrakemeierE-LWilbertzGRodaxSPatterns of response to repetitive transcranial magnetic stimulation (rTMS) in major depression: Replication study in drug-free patientsJournal of Affective Disorders20081081–2597017963846
- ChenS-JChangC-HTsaiH-CChenS-TLinCCHSuperior antidepressant effect occurring 1 month after rTMS: Add-on rTMS for subjects with medication-resistant depressionNeuropsychiatric Disease and Treatment20139
- CohenRBBoggioPSFregniFRisk factors for relapse after remission with repetitive transcranial magnetic stimulation for the treatment of depressionDepression and Anxiety200926768268819170101
- Dell’ossoBAltamuraACAugmentative transcranial magnetic stimulation (TMS) combined with brain navigation in drug-resistant rapid cycling bipolar depression: a case report of acute and maintenance efficacyThe World Journal of Biological Psychiatry: The Official Journal of The World Federation of Societies of Biological Psychiatry2009104 Pt 2673676
- FitzgeraldPBHoyKEHerringSEA double blind randomized trial of unilateral left and bilateral prefrontal cortex transcranial magnetic stimulation in treatment resistant major depressionJournal of Affective Disorders2012139219319822397890
- FurtadoCPHoyKEMallerJJSavageGDaskalakisZJFitzgeraldPBCognitive and volumetric predictors of response to repetitive transcranial magnetic stimulation (rTMS)—a prospective follow-up studyPsychiatry Research20122021121922608156
- GalletlyCGillSClarkePBurtonCFitzgeraldPBA randomized trial comparing repetitive transcranial magnetic stimulation given 3 days/week and 5 days/week for the treatment of major depression: Is efficacy related to the duration of treatment or the number of treatments?Psychological Medicine201242598198821910937
- GeorgeMSLisanbySHAveryDDaily left prefrontal transcranial magnetic stimulation therapy for major depressive disorder: a sham-controlled randomized trialArchives of General Psychiatry201067550751620439832
- HadleyDAndersonBSBorckardtJJSafety, tolerability, and effectiveness of high doses of adjunctive daily left prefrontal repetitive transcranial magnetic stimulation for treatment-resistant depression in a clinical settingThe Journal of ECT2011271182521343710
- HeMLGuZTWangXYShiHPTreatment of depression using sleep electroencephalogram modulated repetitive transcranial magnetic stimulationChinese Medical Journal2011124121779178321740832
- HerbsmanTAveryDRamseyDMore lateral and anterior prefrontal coil location is associated with better repetitive transcranial magnetic stimulation antidepressant responseBiological Psychiatry200966550951519545855
- Hernández-RibasRDeusJPujolJIdentifying brain imaging correlates of clinical response to repetitive transcranial magnetic stimulation (rTMS) in major depressionBrain Stimulation201361546122417767
- HerwigUCardenas-MoralesLConnemannBJKammerTSchönfeldt-LecuonaCSham or real–post hoc estimation of stimulation condition in a randomized transcranial magnetic stimulation trialNeuroscience Letters20104711303320064587
- HoeppnerJPadbergFDomesGInfluence of repetitive transcranial magnetic stimulation on psychomotor symptoms in major depressionEuropean Archives of Psychiatry and Clinical Neuroscience2010260319720219680706
- HoyKESegraveRADaskalakisZJFitzgeraldPBInvestigating the relationship between cognitive change and antidepressant response following rTMS: A large scale retrospective studyBrain Stimulation20125453954622305343
- HuangC-CWeiIHChouY-HSuT-PEffect of age, gender, menopausal status, and ovarian hormonal level on rTMS in treatment-resistant depressionPsychoneuroendocrinology200833682183118468810
- HuangMlLuoByHuJbRepetitive transcranial magnetic stimulation in combination with citalopram in young patients with first-episode major depressive disorder: A double-blind, randomized, sham-controlled trialAustralian and New Zealand Journal of Psychiatry201246325726422391283
- JakobFBrakemeierE-LSchommerNCUltrahigh frequency repetitive transcranial magnetic stimulation in unipolar depressionJournal of Clinical Psychopharmacology200828447447618626288
- KozelFAJohnsonKANahasZFractional anisotropy changes after several weeks of daily left high-frequency repetitive transcranial magnetic stimulation of the prefrontal cortex to treat major depressionThe Journal of ECT201127151020559144
- KreuzerPMLangguthBSchecklmannMEichhammerPHajakGLandgrebeMCan repetitive transcranial magnetic stimulation prolong the antidepressant effects of sleep deprivation?Brain Stimulation20125214114722037130
- LingeswaranARepetitive Transcranial Magnetic Stimulation in the Treatment of depression: A Randomized, Double-blind, Placebo-controlled TrialIndian Journal of Psychological Medicine2011331354422021951
- LisanbySHHusainMMRosenquistPBDaily left prefrontal repetitive transcranial magnetic stimulation in the acute treatment of major depression: clinical predictors of outcome in a multisite, randomized controlled clinical trialNeuropsychopharmacology200934252253418704101
- MyczkowskiMLDiasAMLuvisottoTEffects of repetitive transcranial magnetic stimulation on clinical, social, and cognitive performance in postpartum depressionNeuropsychiatric Disease and Treatment2012849150023118543
- NongpiurASinhaVKPraharajSKGoyalNTheta-patterned, frequency-modulated priming stimulation enhances low-frequency, right prefrontal cortex repetitive transcranial magnetic stimulation (rTMS) in depression: A randomized, sham-controlled studyThe Journal of Neuropsychiatry and Clinical Neurosciences201123334835721948897
- Paillère MartinotM-LGalinowskiARinguenetDInfluence of prefrontal target region on the efficacy of repetitive transcranial magnetic stimulation in patients with medication-resistant depression: A [18F]-fluorodeoxyglucose PET and MRI studyInternational Journal of Neuropsychopharmacology2010131455919267956
- PallantiSBernardiSDi RolloAAntoniniSQuercioliLUnilateral low frequency versus sequential bilateral repetitive transcranial magnetic stimulation: is simpler better for treatment of resistant depression?Neuroscience2010167232332820144692
- PengHZhengHLiLHigh-frequency rTMS treatment increases white matter FA in the left middle frontal gyrus in young patients with treatment-resistant depressionJournal of Affective Disorders201213624925722217432
- RaySNizamieSHAkhtarSPraharajSKMishraBRZia-ul-HaqMEfficacy of adjunctive high frequency repetitive transcranial magnetic stimulation of left prefrontal cortex in depression: A randomized sham controlled studyJournal of Affective Disorders20111281–215315920621361
- RosenquistPBKrystalAHeartKLDemitrackMAVaughn McCallWLeft dorsolateral prefrontal transcranial magnetic stimulation (TMS): sleep factor changes during treatment in patients with pharmacoresistant major depressive disorderPsychiatry Research20132051–2677323021320
- SchrijversDLBaekenCDe RaedtRSabbeBGCThe impact of high-frequency repetitive transcranial magnetic stimulation on fine motor functions in medication-resistant major depressionNeuropsychobiology201266425225823095489
- SchutterDJLGLamanDMvan HonkJVergouwenACKoerselmanGFPartial clinical response to 2 weeks of 2 Hz repetitive transcranial magnetic stimulation to the right parietal cortex in depressionInternational Journal of Neuropsychopharmacology200912564365018925985
- SchutterDJLGvan HonkJLamanMVergouwenACKoerselmanFIncreased sensitivity for angry faces in depressive disorder following 2 weeks of 2-Hz repetitive transcranial magnetic stimulation to the right parietal cortexInternational Journal of Neuropsychopharmacology20101391155116120587129
- SimpsonKNWelchMJKozelFADemitrackMANahasZCost-effectiveness of transcranial magnetic stimulation in the treatment of major depression: a health economics analysisAdvances In Therapy200926334636819330495
- SpampinatoCAgugliaEConcertoCTranscranial magnetic stimulation in the assessment of motor cortex excitability and treatment of drug-resistant major depressionIEEE Transactions on Neural Systems and Rehabilitation Engineering201321339140323559064
- SpeerAMBensonBEKimbrellTKOpposite effects of high and low frequency rTMS on mood in depressed patients: Relationship to baseline cerebral activity on PETJournal of Affective Disorders2009115338639419027962
- SpeerAMWassermannEMBensonBEHerscovitchPPostRMAntidepressant Efficacy of High and Low Frequency rTMS at 110% of Motor Threshold versus Sham Stimulation over Left Prefrontal CortexBrain Stimulation2013
- TamasRLMenkesDEl-MallakhRSStimulating research: a prospective, randomized, double-blind, sham-controlled study of slow transcranial magnetic stimulation in depressed bipolar patientsThe Journal of Neuropsychiatry and Clinical Neurosciences200719219819917431073
- TriggsWJRicciutiNWardHERight and left dorsolateral pre-frontal rTMS treatment of refractory depression: A randomized, sham-controlled trialPsychiatry Research2010178346747420643486
- TrojakBChauvet-GelinierJ-CVergèsBBoninBSignificant increase in plasma thyroid-stimulating hormone during low-frequency repetitive transcranial magnetic stimulationThe Journal of Neuropsychiatry and Clinical Neurosciences2011231E12E1221304111
- UllrichHKranasterLSiggesEAndrichJSartoriusAUltra-high-frequency left prefrontal transcranial magnetic stimulation as augmentation in severely ill patients with depression: a naturalistic sham-controlled, double-blind, randomized trialNeuropsychobiology201266314114822948250
- ZarkowskiPNavarroRPavlicovaMGeorgeMSAveryDThe effect of daily prefrontal repetitive transcranial magnetic stimulation over several weeks on resting motor thresholdBrain Stimulation20092316316720161065
- ZhengH-rLiL-jZhangLTreatment of rTMS on young patients with intractable depressionChinese Journal of Clinical Psychology20101814446
- ZhengHZhangLLiLHigh-frequency rTMS treatment increases left prefrontal myo-inositol in young patients with treatment-resistant depressionProgress in Neuro-Psychopharmacology and Biological Psychiatry20103471189119520600472
Disclosure
The authors report no conflicts of interest in this work. No external funding was received for this study.
References
- FregniFMarcolinMAMyczkowskiMPredictors of antidepressant response in clinical trials of transcranial magnetic stimulationInt J Neuropsychopharmacol20069664165416939662
- KozelFANahasZdeBruxCHow coil-cortex distance relates to age, motor threshold, and antidepressant response to repetitive transcranial magnetic stimulationJ Neuropsychiatry Clin Neurosci200012337638410956572
- BrakemeierELLuborzewskiADanker-HopfeHKathmannNBajboujMPositive predictors for antidepressive response to prefrontal repetitive transcranial magnetic stimulation (rTMS)J Psychiatr Res200741539540316554071
- BrakemeierELWilbertzGRodaxSPatterns of response to repetitive transcranial magnetic stimulation (rTMS) in major depression: replication study in drug-free patientsJ Affect Disord20081081–2597017963846
- LisanbySHHusainMMRosenquistPBDaily left prefrontal repetitive transcranial magnetic stimulation in the acute treatment of major depression: clinical predictors of outcome in a multisite, randomized controlled clinical trialNeuropsychopharmacology200934252253418704101
- McDonaldWMDurkalskiVBallERImproving the antidepressant efficacy of transcranial magnetic stimulation: maximizing the number of stimulations and treatment location in treatment-resistant depressionDepression Anxiety2011281197398021898711
- McNamaraBRayJLArthursOJBonifaceSTranscranial magnetic stimulation for depression and other psychiatric disordersPsychol Med20013171141114611681540
- HoltzheimerPERussoJAveryDHA meta-analysis of repetitive transcranial magnetic stimulation in the treatment of depressionPsychopharmacol Bull200135414916912397863
- MartinJLBarbanojMJSchlaepferTETranscranial magnetic stimulation for treating depressionCochrane Database Syst Rev20022CD00349312076483
- KozelFAGeorgeMSMeta-analysis of left prefrontal repetitive transcranial magnetic stimulation (rTMS) to treat depressionJ Psychiatr Pract20028527027515985889
- BurtTLisanbySHSackeimHANeuropsychiatric applications of transcranial magnetic stimulation: a meta analysisInt J Neuropsychopharmacol2002517310312057034
- MartinJLBarbanojMJSchlaepferTEThompsonEPérezVKulisevskyJRepetitive transcranial magnetic stimulation for the treatment of depression. Systematic review and meta-analysisBr J Psychiatry200318248049112777338
- CouturierJLEfficacy of rapid-rate repetitive transcranial magnetic stimulation in the treatment of depression: a systematic review and meta-analysisJ Psychiatry Neurosci2005302839015798783
- HerrmannLLEbmeierKPFactors modifying the efficacy of transcranial magnetic stimulation in the treatment of depression: a reviewJ Clin Psychiatry200667121870187617194264
- GrossMNakamuraLPascual-LeoneAFregniFHas repetitive transcranial magnetic stimulation (rTMS) treatment for depression improved? A systematic review and meta-analysis comparing the recent vs the earlier rTMS studiesActa Psychiatr Scand2007116316517317655557
- LamRWChanPWilkins-HoMYathamLNRepetitive transcranial magnetic stimulation for treatment-resistant depression: a systematic review and metaanalysisCan J Psychiatry200853962163118801225
- SchutterDJAntidepressant efficacy of high-frequency transcranial magnetic stimulation over the left dorsolateral prefrontal cortex in double-blind sham-controlled designs: a meta-analysisPsychol Med2009391657518447962
- SchutterDJQuantitative review of the efficacy of slow-frequency magnetic brain stimulation in major depressive disorderPsychol Med201040111789179520102670
- SlotemaCWBlomJDHoekHWSommerIEShould we expand the toolbox of psychiatric treatment methods to include Repetitive Transcranial Magnetic Stimulation (rTMS)? A meta-analysis of the efficacy of rTMS in psychiatric disordersJ Clin Psychiatry201071787388420361902
- AllanCLHerrmannLLEbmeierKPTranscranial magnetic stimulation in the management of mood disordersNeuropsychobiology201164316316921811086
- BerlimMTVan den EyndeFDaskalakisZJA systematic review and meta-analysis on the efficacy and acceptability of bilateral repetitive transcranial magnetic stimulation (rTMS) for treating major depressionPsychol Med201343112245225423200131
- BerlimMTVan den EyndeFDaskalakisZJHigh-frequency repetitive transcranial magnetic stimulation accelerates and enhances the clinical response to antidepressants in major depression: a meta-analysis of randomized, double-blind, and sham-controlled trialsJ Clin Psychiatry2013742e122e12923473357
- BerlimMTVan den EyndeFJeff DaskalakisZClinically meaningful efficacy and acceptability of low-frequency repetitive transcranial magnetic stimulation (rTMS) for treating primary major depression: a meta-analysis of randomized, double-blind and sham-controlled trialsNeuropsychopharmacology201338454355123249815
- Dell’OssoBCamuriGCastellanoFMeta-Review of Metanalytic Studies with Repetitive Transcranial Magnetic Stimulation (rTMS) for the Treatment of Major DepressionClin Pract Epidemiol Ment Health2011716717722135698
- MoherDLiberatiATetzlaffJAltmanDGPRISMA groupPreferred reporting items for systematic reviews and meta-analyses: the PRISMA statementAnn Intern Med2009151426426919622511
- HamiltonMA rating scale for depressionJ Neurol Neurosurg Psychiatry196023566214399272
- BeckATWardCHMendelsonMMockJErbaughJAn inventory for measuring depressionArch Gen Psychiatry1961456157113688369
- MontgomerySAAsbergMA new depression rating scale designed to be sensitive to changeBr J Psychiatry1979134382389444788
- BorensteinMHedgesLVHigginsJPTRothsteinHRIntroduction to Meta-AnalysisHoboken, NJJohn Wiley and Sons, Ltd2009
- CohenJStatistical Power Analysis for the Behavioural SciencesHillsdale, NJLawrence Erlbaum Associates1988
- DerSimonianRLairdNMeta-analysis in clinical trialsControl Clin Trials1986731771883802833
- HigginsJPThompsonSGDeeksJJAltmanDGMeasuring inconsistency in a meta-analysesBMJ2003327741455756012958120
- RosenthalRThe ‘file drawer’ problem and tolerance for null resultsPsychological Bulletin1979863638641
- DuvalSTweedieRA nonparametric ‘trim and fill’ method of accounting for publication bias in meta-analysisJ Am Stat Assoc2000954498998
- SterneJAEggerMFunnel plots for detecting bias in meta-analysis: guidelines on choice of axisJ Clin Epidemiol200154101046105511576817
- BeggCBMazumdarMOperating characterstics of a rank correlation test for publication biasBiometrics1994504108811017786990
- EggerMSmithGDSchneiderMMinderCBias in meta-analysis detected by a simple graphical testBMJ199731571096296349310563
- PengHZhengHLiLHigh-frequency rTMS treatment increases white matter FA in the left middle frontal gyrus in young patients with treatment-resistant depressionJ Affect Disord2012136324925722217432
- RaySNizamieSHAkhtarSPraharajSKMishraBRZia-ul-HaqMEfficacy of adjunctive high frequency repetitive transcranial magnetic stimulation of left prefrontal cortex in depression: A randomized sham controlled studyJ Affect Disord20111281–215315920621361
- SpampinatoCAgugliaEConcertoCTranscranial magnetic stimulation in the assessment of motor cortex excitability and treatment of drug-resistant major depressionIEEE Trans Neural Syst Rehabil Eng201321339140323559064
- ZhengHZhangLLiLHigh-frequency rTMS treatment increases left prefrontal myo-inositol in young patients with treatment-resistant depressionProg Neuropsychopharmacol Biol Psychiatry20103471189119520600472
- O’ReardonJPSolvasonHBJanicakPGEfficacy and safety of transcranial magnetic stimulation in the acute treatment of major depression: a multisite randomized controlled trialBiol Psychiatry2010672e15e1719914602
- HuangCCWeiIHChouYHSuTPEffect of age, gender, menopausal status, and ovarian hormonal level on rTMS in treatment-resistant depressionPsychoneuroendocrinology200833682183118468810
- Fernández-GuastiAFiedlerJLHerreraLHandaRJSex, stress, and mood disorders: at the intersection of adrenal and gonadal hormonesHorm Metab Res201244860761822581646
- Quera SalvaMAHartleySMood disorders, circadian rhythms, melatonin and melatonin agonistsJ Cent Nerv Syst Dis20124152623650464
- GeorgeMSLisanbySHAveryDDaily left prefrontal transcranial magnetic stimulation therapy for major depressive disorder: a sham-controlled randomized trialArch Gen Psychiatry201067550751620439832
- KandelERSchwartzJHJessellTMSiegelbaumSAHudspethAJPrinciples of Neural Science5th edNew YorkMcGraw-Hill Professional2013
- BerlimMTBroadbentHJVan den EyndeFBlinding integrity in randomized sham-controlled trials of repetitive transcranial magnetic stimulation for major depression: a systematic review and meta-analysisJ Neuropsychopharmacol201316511731181
- RusjanPMBarrMSFarzanFOptimal transcranial magnetic stimulation coil placement for targeting the dorsolateral prefrontal cortex using novel magnetic resonance image-guided neuronavigationHum Brain Mapp201031111643165220162598
- Paillère MartinotMLGalinowskiARinguenetDInfluence of prefrontal target region on the efficacy of repetitive transcranial magnetic stimulation in patients with medication-resistant depression: a [(18)F]-fluorodeoxyglucose PET and MRI studyInt J Neuropsychopharmacol2010131455919267956
- PallantiSBernardiSDi RolloAAntoniniSQuercioliLUnilateral low frequency versus sequential bilateral repetitive transcranial magnetic stimulation: is simpler better for treatment of resistant depression?Neuroscience2010167232332820144692
- TriggsWJRicciutiNWardHERight and left dorsolateral pre-frontal rTMS treatment of refractory depression: A randomized, sham-controlled trialPsychiatry Res2010178346747420643486
- AguirreICarreteroBIbarraOAge predicts low-frequency transcranial magnetic stimulation efficacy in major depressionJ Affect Disord2011130346646921093060
- HeMLGuZTWangXYShiHPTreatment of depression using sleep electroencephalogram modulated repetitive transcranial magnetic stimulationChin Med J (Engl)2011124121779178321740832
- LingeswaranARepetitive Transcranial Magnetic Stimulation in the Treatment of depression: A Randomized, Double-blind, Placebo-controlled TrialIndian J Psychol Med2011331354422021951
- BakimBUzunUEKaramustafaliogluOThe combination of antidepressant drug therapy and high-frequency repetitive transcranial magnetic stimulation in medication-resistant depressionBCP2012223244253
- BlumbergerDMMulsantBHFitzgeraldPBA randomized double-blind sham-controlled comparison of unilateral and bilateral repetitive transcranial magnetic stimulation for treatment-resistant major depressionWorld J Biol Psychiatry201213642343521736507
- FitzgeraldPBHoyKEHerringSEA double blind randomized trial of unilateral left and bilateral prefrontal cortex transcranial magnetic stimulation in treatment resistant major depressionJ Affect Disord2012139219319822397890
- HuangMLLuoBYHuJBRepetitive transcranial magnetic stimulation in combination with citalopram in young patients with first-episode major depressive disorder: a double-blind, randomized, sham-controlled trialAust N Z J Psychiatry201246325726422391283
- ChenSJChangCHTsaiHCChenSTLinCChSuperior antidepressant effect occurring 1 month after rTMS: add-on rTMS for subjects with medication-resistant depressionNeuropsychiatr Dis Treat2013939740123576870
- Hernández-RibasRDeusJPujolJIdentifying brain imaging correlates of clinical response to repetitive transcranial magnetic stimulation (rTMS) in major depressionBrain Stimul201361546122417767
- SpeerAMWassermannEMBensonBEHerscovitchPPostRMAntidepressant efficacy of high and low frequency rTMS at 110% of motor threshold versus sham stimulation over left prefrontal cortexBrain Stimul201371364123928104
