Abstract
Many emotional disturbances such as post-stroke depression (PSD) and emotional incontinence (EI) commonly occur following cerebrovascular events. The efficacy of antidepressants for these conditions has been established but their comorbid treatment has not been well characterized. In the current study, the authors describe two cases of post-stroke emotional dysregulation; one case with EI; and the other with EI complicated by PSD. The authors describe their differential responses to treatment. Case 1 developed EI after an infarct due to occlusion of the penetrating branches of the left middle cerebral artery (MCA). Case 2 developed both PSD and EI after right MCA stem occlusion. Both patients were initially treated with the selective serotonin reuptake inhibitor (SSRI) paroxetine. Case 1 reacted promptly to SSRI treatment. However, Case 2 had only a partial response to paroxetine, even after many months of treatment. Adjunctive therapy with low-dose aripiprazole was eventually added, resulting in complete improvement of both EI and PSD after 2 additional months of treatment. Thus, Case 2 required a different treatment strategy than Case 1. These findings suggest that aripiprazole adjunctive therapy could be effective for some complex post-stroke emotional disorders.
Introduction
Emotional disorders are common in post-stroke patients. Many studies have examined the effects and treatment of post-stroke depression (PSD).Citation1 Patients with left-sided basal ganglia lesions have shown a significantly higher frequency and severity of depression compared with patients with right-sided basal ganglia or thalamic lesions.Citation2 Emotional lability – described as emotionalism, pathological laughing, crying and emotional incontinence (EI) – are common complications in stroke patients. The prevalence of EI has been reported to be 15%–20%.Citation3 A previous study showed that EI was frequent in patients with small lenticulocapsular strokes, and was often associated with lesions affecting the dorsal rather than ventral part of the globus pallidus.Citation4 Infarcts of the corona radiata are common in the regions supplied by the small blood vessels of the middle cerebral artery (MCA). Thus, ischemic injury involving the internal capsule and basal ganglia seems to be associated with emotional disorders as a result of a stroke. The pathogenesis of post-stroke emotional disorders can involve damage to the biogenic amine pathways, such as serotonin projections that play an important role in the modulation of mood.Citation2
Controlled studies of cases with post-stroke emotional disorders (EI and PSD) have examined the effectiveness and tolerability of selective serotonin reuptake inhibitors (SSRIs) such as citalopram, fluoxetine, and paroxetine.Citation5–Citation7 Many patients with EI have shown a rapid response to low-dose SSRI treatment. Based on evidence of intolerance or poor treatment response to SSRIs, it has been reported that a change in lamotrigine dosage has been effective.Citation8 A rapid response to mirtazapine was observed in a study where subjects with both EI and PSD failed to respond to SSRIs.Citation9 Moreover, in a double-blind study using nortriptyline for EI, the non-PSD group showed greater improvements in EI compared with the PSD group.Citation10 As a result, it appears that improvements in PSD are not directly associated with improvements in EI. To the current authors’ knowledge, studies on the treatment of complex emotional disorders such as comorbid EI and PSD following stroke did not include the use of adjunctive therapy. The current study reports two cases of emotional disorders following corona radiata infarct that required differential treatment, thereby suggesting that low-dose aripiprazole adjunctive therapy could be effective in some patients with complex emotional disorders.
Case 1
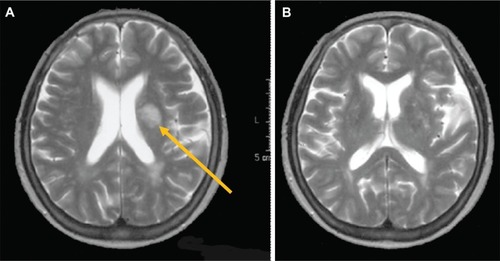
A 60-year-old woman being treated for hypertension developed dysarthria, right hemiplegia, and tingling. As a result, a diagnosis of acute phase ischemic stroke in the perforating arteries of the MCA was made. Evidence of a single infarct of the left corona radiata was observed on magnetic resonance imaging (MRI) taken the next day (). The patient had no history of psychiatric illness such as depression on presentation, and there was no history of psychiatric treatment. Six months after her stroke, the patient displayed daily uncontrollable crying. Although this distressed her caregivers, it was not initially recognized as a psychiatric problem. As a result, the patient only received a psychiatric examination 13 months later. She had been crying for no reason more than ten times a day, but it was also observed that occasionally she could not stop laughing. She described the crying spells as lasting several minutes and stated that she could not resist them. A depressed mood and symptoms consistent with a mood disorder were dismissed following medical examination. The patient had a Hamilton Rating Scale for Depression (HRSD17)Citation11 score of 10 points out of a possible 50 (10/50).
Figure 1 Axial T2-weighted magnetic resonance imaging (MRI) of the body of the lateral ventricle showing a single infarction in the left corona radiata.
To measure the severity of the EI, the current study evaluated the patient using the Pathological Laughter and Crying Scale (PLACS).Citation10 A pretreatment PLACS score of 21/27 points suggested moderate disability. Paroxetine 10 mg daily, an SSRI whose efficacy has been supported by previous treatment case reports of EI, was administered. At 2 week follow-up, the subject reported that her crying spells had significantly decreased after initiation of paroxetine, and her PLACS score had decreased from 21 points to 10 points. After 4 weeks of treatment, her PLACS score had decreased to 4/27. At 8 weeks follow-up, she described that her crying spells had ceased. The patient then stopped her hospital visits and discontinued paroxetine. She subsequently had a relapse of crying spells 2 months later accompanied by a PLACS score of 19/27. Treatment with paroxetine 10 mg was restarted and EI was rapidly alleviated. Within 4 weeks, the patient’s PLACS score decreased to 2/27. Medication with low-dose paroxetine was continued for 3 months and then treatment was stopped with no signs of recurrence of EI.
Case 2
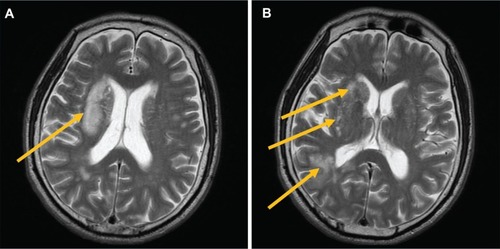
A 67-year-old man with a history of depression since age 50 presenting with symptoms of dysarthria and left hemiplegia was admitted to the stroke care unit. An MRI showed an infarct of the right corona radiata as well as infarcts in the caudate nucleus, lentiform nucleus, and right posterior temporal lobe () due to occlusion of the MCA. An MCA stem (M1) occlusion was observed on brain angiography. He showed improvements in blood flow to the MCA after treatment based on acute stroke treatment guidelines; after 30 days, he was transferred to a rehabilitation hospital. Three months after his stroke, he was crying for no reason several times a day and complained of loss of interest and a tendency to be pessimistic. An HRSD17 score of 18/50 suggested that the patient had developed mild to moderate depression and a PLACS score of 20/27 suggested moderate disability.
Figure 2 Axial T2-weighted magnetic resonance imaging (MRI) of the body of the lateral ventricle showing infarction of the right corona radiata, without major brain infarction in the left hemisphere.
A score of 28 on the Mini Mental State Examination (MMSE)Citation12 did not suggest significant cognitive impairment. As a result, he was diagnosed with comorbid PSD and EI and was started on paroxetine 10 mg. Paroxetine was gradually increased to 40 mg over 12 weeks. The PLACS score decreased to 10/27 during the first 4 weeks and HRSD17 decreased to 13. However, PLACS and HRSD17 scores did not decrease over the next 8 weeks. The left hemiplegia did not improve, even 9 months after his stroke, and he subsequently received superficial temporal artery-to-middle cerebral artery bypass surgery after assessment by cerebral angiography. Administration of paroxetine 40 mg was continued.
He was transferred again to the rehabilitation hospital, where his clinical symptoms improved after surgery. His MMSE score did not decrease but his PLACS and HRSD17 scores did not decrease. In addition, unstable emotional thinking, pessimistic irritability, and aggressive behavior were observed. Therefore, with the informed consent of the patient and family, adjunctive therapy with low-dose aripiprazole 3 mg/day was started. Within 4 weeks, uncontrolled crying spells stopped. Aripiprazole was increased to 6 mg/day over 2 weeks, and after 2 more weeks, his depressive symptoms, irritability, and aggressive behavior were relieved, with a HRDS17 score of 7 and sustained clinical improvement in EI. No adverse effects from the aripiprazole were seen. His lower limb remained hemiplegic but the decreased motivation for rehabilitation was markedly improved. PSD and EI remained in remission (PLACS 0; HRDS17 4) after 2 months of adjunctive therapy with aripiprazole.
Discussion
This study reported two cases of emotional disorder after corona radiata infarct. Case 1 showed post-stroke EI after a single lesion infarct of the left corona radiata who responded rapidly to low-dose SSRI. Case 2 showed both post-stroke PSD and EI after multiple lesions, including a right corona radiata infarct. In Case 2, SSRI treatment showed partial efficacy for the post-stroke EI but was ineffective for the depressive symptoms of PSD. Adjunctive therapy with low-dose aripiprazole was beneficial for the treatment of post-stroke EI and PSD. These results suggest that the course of post-stroke emotional disorders and prognosis for successful treatment after infarction of the MCA can be different in subjects with EI or with a combination of EI and PSD.
In a previous report on the association between PSD and corona radiata infarction, Vataja et alCitation13 reported that in PSD patients, the brain infarct often significantly affected the basal ganglia, mainly the caudate, putamen and pallidum, as well as the posterior corona radiata. They also reported that the frequency of depression was greater in these subjects, with larger infarct size at the sites. However, a clear relationship between specific stroke lesion and development of EI was not established. Previous studies have reported that small lenticulocapsular strokes of the basal ganglia in the right anterior region were closely related to EI.Citation14–Citation16 Patients with lenticulocapsular stroke more often develop EI than depression.Citation4 The risk factors associated with PSD are: history of depression, increased stroke severity, and post-stroke cognitive or physical impairment.Citation17 However, EI does not appear to be related to the presence of motor or general disability.Citation4 Most EI patients also have PSD. EI was found to be significantly correlated with mood score and post-stroke depression, as well as with lesion size, activities of daily living (ADL) scores, and intellectual impairment, but not with lesion location, history of stroke, or depression.Citation18
Another study found that a past history of depression and cortical lesions were independent predictors of EI.Citation19 PSD patients with EI had more severe depressive symptoms compared with patients without comorbid EI.Citation3 Therefore, it is thought that the pathologies of post-stroke EI and PSD are partially linked. These previous reports suggest a possible explanation for the two cases in the current study. Case 1 with no history of depression appeared to have pure EI due to a single small corona radiata infarction that was disrupting serotonergic ascending projections. In Case 2, there was a possibility that the activity of other monoamines and serotonin was reduced by multiple infarctions, including the corona radiata, and that history of depression and physical impairment also played an important role in the appearance of both PSD and EI. Starkstein et alCitation20 reported that PSD following MCA lesions was of significantly longer duration than PSD following brainstem and/or cerebellar infarcts. Moreover, ADL were more significantly impaired in patients without PSD than in patients with PSD in the MCA group.Citation20 Thus, the delays in recovery from PSD and recovery from physical impairment were interrelated in Case 2.
The most interesting finding in these case reports was that low-dose aripiprazole adjunctive therapy could be effective for post-stroke emotional disorders that were not improving with SSRIs alone. The efficacy of antidepressant treatment for PSD and EI is well-established, and SSRIs are the first-line drugs of choice. Many pure EI cases showed a rapid response to low-dose SSRI treatment as in Case 1. Andersen et alCitation21 investigated the correlation between severity of post-stroke pathological crying with lesion size and location in twelve EI patients. Patients with the most severe EI had relatively large bilateral pontine lesions without lesions in the hemispheres, and clinically least-affected patients had mainly unilateral large subcortical lesions. Therefore, the authors concluded that the destruction of serotonergic raphe nuclei or their ascending serotonergic hemispheric projections could be underlying causes of EI.Citation6
This hypothesis is supported by positron emission tomography (PET)-mapping results of high-binding serotonin 5-HT1A receptors in the raphe nuclei of patients with post-stroke EI.Citation22 In addition, polymorphisms in the serotonin transporter 5-HTT gene have been shown to be associated with a prevalence of post-stroke EI, with the 5-HTT gene-linked promoter region 5-HTTLPR genotype conferring increased susceptibility to EI.Citation23 There was rapid improvement in EI symptoms with antidepressant administration but PSD did not improve. The effectiveness of SSRIs for PSD has not been completely established but a more significant effect of nortriptyline compared to fluoxetine has been reported.Citation1
A recent study reported on the efficacy and tolerability of adjunctive aripiprazole in patients with treatment-resistant major depression and partial response to antidepressant treatment.Citation24 The authors stated that aripiprazole is a second generation antipsychotic with pharmacological properties distinct from other antipsychotics. It acts as a partial agonist at dopamine D2 and D3 and serotonin 5-HT1A receptors, and as an antagonist at 5-HT2A receptors. Activity at these receptors is shared by a number of antidepressant agents, giving aripiprazole a pharmacological rationale for use in depression.Citation24
Herrmann et al reported that atypical antipsychotics can be associated with an increased risk of stroke in the elderly.Citation25 US Food and Drug Administration approved revisions to the safety labeling for aripiprazole warn of the risk of cerebrovascular adverse events, including stroke, associated with its use in elderly patients with dementia-related psychosis. In recognition of these findings, the current study added a low dose of aripiprazole to the case with post-stroke emotional disorder without dementia that had not improved with SSRI treatment, expecting that its dopamine and serotonin agonism would target the symptoms of irritability and aggressive behavior. Severity of depression, other psychopathologies, and neurobiological factors appear to contribute to irritability and aggressive behavior in stroke patients. Moreover, post-stroke irritable and aggressive patients with higher HRSD17 scores responded more favorably to antidepressants.
Although depressed mood was more likely to occur in subjects with emotionalism, most of them were not depressed.Citation26 Calvert et alCitation27 reported that post-stroke EI was associated with simple depression, irritability, and ideas of reference among 14 possible psychiatric symptoms derived by aggregating scores from individual items of using a short form of the Present State Examination (PSE) administered during the interview. Post-stroke emotional disorder can have a negative impact on a patient’s participation in the rehabilitation process and associated rehabilitation outcomes and be a cause of caregiver stress.Citation2 Accordingly, early medical assessment for PSD and appropriate treatment can lead to improved physical and cognitive recovery and decreased mortality.
It is well known that serotonergic and noradrenergic fibers that originate from the brainstem nuclei and innervate the limbic system, prefrontal cortex, and associated structures are involved in the regulation of mood. Furthermore, dopaminergic pathways seem to play a crucial role in mood and depression. The effectiveness of a combination of modafinil, a dopamine agonist, and aripiprazole in a young adult PSD case with aggressive behavior and emotional lability has been reported.Citation28 In addition to monoamines, the cholinergic system, through nicotinic acetylcholine receptors, has recently been suggested to be involved in the etiology of major depressive disorders. These pathways can be disrupted by the stroke lesion, which can result in depression and contribute to the complexity of the disorder.Citation29
The first-line treatment for PSD are antidepressants but there are exceptions. Dementia was not a factor in the current study, but the risks of using second generation antipsychotics in elderly patients should have been considered. Adjunctive therapy with aripiprazole to minimize sedation can be effective in antidepressant refractory post-stroke emotional disorders, particularly those associated with irritability and aggression. Further studies are required to clarify the efficacy of antipsychotic drugs in complex post-stroke emotional disorders.
Acknowledgments
We would like to thank Dr Usuda who provided carefully considered feedback and valuable comments.
Disclosure
The authors report no conflicts of interest in this work.
References
- RobinsonRGSchultzSKCastilloCNortriptyline versus fluoxetine in the treatment of depression and in short-term recovery after stroke: a placebo-controlled, double-blind studyAm J Psychiatry2000157335135910698809
- RobinsonRGThe Clinical Neuropsychiatry of Stroke: Cognitive, Behavioral and Emotional Disorders following Vascular Brain Injury2nd edCambridgeCambridge University Press2006
- HouseADennisMMolyneuxAWarlowCHawtonKEmotionalism after strokeBMJ198929866799919942499390
- KimJSPost-stroke emotional incontinence after small lenticulocapsular stroke: correlation with lesion locationJ Neurol2002249780581012140660
- MüllerUMuraiTBauer-WittmundTvon CramonDYParoxetine versus citalopram treatment of pathological crying after brain injuryBrain Inj1999131080581110576464
- AndersenGVestergaardKLauritzenLEffective treatment of poststroke depression with the selective serotonin reuptake inhibitor citalopramStroke1994256109911048202964
- WiartLPetitHJosephPAMazauxJMBaratMFluoxetine in early poststroke depression: a double-blind placebo-controlled studyStroke20003181829183210926942
- RamasubbuRLamotrigine treatment for post-stroke pathological laughing and cryingClin Neuropharmacol200326523323514520162
- KimSWShinISKimJMLimSYYangSJYoonJSMirtazapine treatment for pathological laughing and crying after strokeClin Neuropharmacol200528524925116239769
- RobinsonRGParikhRMLipseyJRStarksteinSEPriceTRPathological laughing and crying following stroke: validation of a measurement scale and a double-blind treatment studyAm J Psychiatry199315022862938422080
- HamiltonMA rating scale for depressionJ Neurol Neurosurg Psychiatry196023566214399272
- FolsteinMFolsteinSEMcHughPR“Mini-Mental State” a Practical Method for Grading the Cognitive State of Patients for the ClinicianJ Psychiatr Res19751231891981202204
- VatajaRPohjasvaaraTLeppävuoriAMagnetic resonance imaging correlates of depression after ischemic strokeArch Gen Psychiatry2001581092593111576030
- MacHaleSMO’RourkeSJWardlawJMDennisMSDepression and its relation to lesion location after strokeJ Neurol Neurosurg Psychiatry19986433713749527152
- KimJSChoiKSPoststroke depression and emotional incontinence: correlation with lesion locationNeurology20005491805181010802788
- ChoiKSHanKChoiSPoststroke depression and emotional incontinence: factors related to acute and subacute stagesNeurology201278151130113722459674
- JohnsonJLMinarikPANyströmKVBautistaCGormanMJPost-stroke depression incidence and risk factors: an integrative literature reviewJ Neurosci Nurs200638431632716989301
- AndersenGVestergaardKIngeman-NielsenMPost-stroke pathological crying: frequency and correlation to depressionEur J Neurol199521455024283580
- TangWKChanSSChiuHFUngvariGSWongKSKwokTCEmotional incontinence in Chinese stroke patients-diagnosis, frequency, and clinical and radiological correlatesJ Neurol2004251786586915258791
- StarksteinSERobinsonRGBerthierMLPriceTRDepressive disorders following posterior circulation as compared with middle cerebral artery infarctsBrain1998111Pt 23753873378141
- AndersenGIngeman-NielsenMVestergaardKRiisJOPathoanatomic correlation between post-stroke pathological crying and damage to brain areas involved in serotonergic neurotransmissionStroke1994255105010527818634
- MøllerMAndersenGGjeddeASerotonin 5HT1A receptor availability and pathological crying after strokeActa Neurol Scand20071162839017661792
- KimJMStewartRKangHJAssociations of serotonergic genes with poststroke emotional incontinenceInt J Geriatr Psychiatry201227879980621915913
- MarcusRNMcQuadeRDCarsonWHThe efficacy and safety of aripiprazole as adjunctive therapy in major depressive disorder: a second multicenter, randomized, double-blind, placebo-controlled studyJ Clin Psychopharmacol200828215616518344725
- HerrmannNMamdaniMLanctôtKLAtypical antipsychotics and risk of cerebrovascular accidentsAm J Psychiatry200416161113111515169702
- ChanKLCampayoAMoserDJArndtSRobinsonRGAggressive behavior in patients with stroke: association with psychopathology and results of antidepressant treatment on aggressionArch Phys Med Rehabil200687679379816731214
- CalvertTKnappPHouseAPsychological associations with emotionalism after strokeJ Neurol Neurosurg Psychiatry19986569289299854975
- CapaldiVFIIWynnGHPost Stroke Depression: Treatments and Complications in a Young AdultPsychiatr Q2010811737920033774
- LoubinouxIKronenbergGEndresMPost-stroke depression: mechanisms, translation and therapyJ Cell Mol Med20121691961196922348642
