Abstract
Cognitive impairment and memory dysfunction following stroke diagnosis are common symptoms that significantly affect the survivors’ quality of life. Stroke patients have a high potential to develop dementia within the first year of stroke onset. Currently, efforts are being exerted to assess stroke effects on the brain, particularly in the early stages. Numerous neuropsychological assessments are being used to evaluate and differentiate cognitive impairment and dementia following stroke. This article focuses on the role of available neuropsychological assessments in detection of dementia and memory loss after stroke. This review starts with stroke types and risk factors associated with dementia development, followed by a brief description of stroke diagnosis criteria and the effects of stroke on the brain that lead to cognitive impairment and end with memory loss. This review aims to combine available neuropsychological assessments to develop a post-stroke memory assessment (PSMA) scheme based on the most recognized and available studies. The proposed PSMA is expected to assess different types of memory functionalities that are related to different parts of the brain according to stroke location. An optimal therapeutic program that would help stroke patients enjoy additional years with higher quality of life is presented.
Introduction
Cognitive impairment and memory loss are common after a stroke. Approximately 30% of stroke patients develop dementia within 1 year of stroke onset.Citation1 Stroke affects the cognitive domain, which includes attention, memory, language, and orientation. The most affected domains are attention and executive functions; at the time of stroke diagnosis, memory problems are often prominent. Post-stroke dementia (PSD), particularly vascular dementia (VaD), reflects the vascular risk factors that are mostly correlated with cerebral vascular disease (CVD). Post-stroke cognitive impairment is the evolution of CVD that predisposes individuals to the vascular cognitive impairment (VCI) spectrum. Thus, understanding the VCI spectrum stages is necessary to evaluate the mental state of post-stroke patients, particularly the cognitive dysfunction and memory decline during the period following a stroke diagnosis. Until recently, no specific neuropsychological assessment to evaluate PSD including memory loss existed. Current efforts are focused on combining more than one of the available neuropsychological assessments to obtain a significant diagnosis of cognitive decline severity following a stroke. The aim of this study was to develop a post-stroke memory assessment (PSMA) based on the most popular and available neuropsychological assessments. The proposed PSMA is expected to assess different types of memory functionalities that are related to different parts of the brain according to the affected memory. Results are then correlated and related to the stroke location and severity. PSMA may provide a promising tool for evaluating post-stroke VaD and assisting medical doctors and clinicians in the assessment as well as evaluation of post-stroke memory impairment severity.
Stroke types
Stroke is considered a major cause of long-term physical disabilities in adults; it is the second most common cause of cognitive impairment and dementia and the third leading cause of death after coronary artery diseases and cancer.Citation2,Citation3
A stroke is a “brain attack” that is caused either by reducing blood and oxygen flow to the brain or by bleeding. Stroke can be classified into two main types: ischemic and hemorrhagic. Transient ischemic attack (TIA) is sometimes considered as the third type of stroke and can be referred to as a “mini-stroke.”Citation4 Stroke characteristics are listed in .
Table 1 Classification of stroke
Vascular risk factors and stroke diagnosis criteria
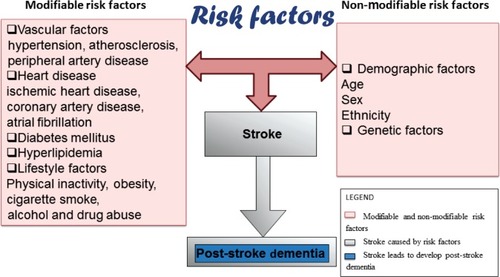
Numerous risk factors band to cause a stroke: modifiable risk factors, including age, sex, ethnicity, genetics; and non-modifiable risk factors, including CVD, heart disease, diabetes mellitus, hyperlipidemia, cigarette smoking, and alcohol abuse, as shown in .Citation5,Citation6 Stroke, which is considered a CVD, is an influential risk factor for cognitive impairment that eventually leads to the development of PSD.Citation7 Thus, stroke survivors require immediate medical control of these risk factors, which are modifiable, to reduce stroke prevalence.
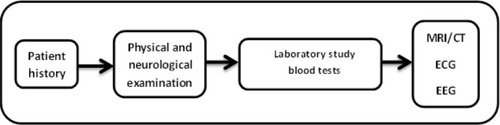
Clinically, stroke can usually be diagnosed through typical symptoms and signs. Medical history is an early step of diagnosis and includes stroke onset, course, and patient information taken from patients’ careers or relatives, followed by physical and neurological examinations of the patients. The neurological examination can be performed using the formal stroke scale developed by the National Institution of Health Stroke ScaleCitation8 to classify early stroke severity. Laboratory testing is the next step; at this stage, blood tests are used to determine the blood sugar level and cholesterol level. This step is followed by an examination of the computer tomography/magnetic resonance imaging scan and electrocardiography recording to indicate stroke location and pulse irregularity, such as cardiovascular status, carotid bruits, fundus examination, peripheral vascular disease, and hypertension.Citation9 Electroencephalography is used to help differentiate between seizure and TIA or between lacunar and cortical infarction in occasional patients, as illustrated in .Citation10
Stroke effects on brain cerebrovascular function
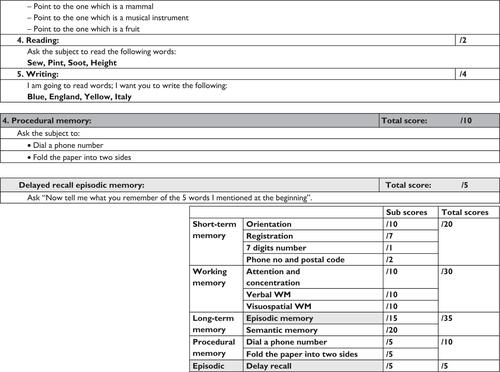
The brain requires a constant supply of blood to carry oxygen and nutrients to the cortical neurons in order for it to function in a normal manner. Numerous arteries cooperate to achieve this demand. In the case where an ischemic or hemorrhagic stroke occurs in one or more of these arteries and/or their branches, it causes damage to a specific neuroanatomic location (ie, right hemisphere cortex, left hemisphere cortex, or subcortex, which can then be localized further to the frontal lobe, temporal lobe, parietal lobe, thalamus, for example). Thus, the part of the brain that does not get the blood it needs starts to die. Brain cellular damage and death within minutes of stroke onset is called the core, whereas the zone in which the blood decreases or marginal perfusion occurs is called the ischemic penumbra, as shown in .Citation4,Citation11
Figure 3 Core and penumbra after stroke.
Owing to the complexity of the neuronal networks concerned in cortical processes, the ischemic or hemorrhagic stroke that occurs in a specific vascular distribution and the damage to a neuroanatomic site typically impairs more than one cognitive function. Moreover, some stroke events may involve multiple neurologic systems that cause cognitive decline based on vascular distribution (ie, perceptual and sensory or motor and sensory), as tabularized in .Citation12
Table 2 Stroke outcome due to vessel infarction
Cognitive disorder following a stroke
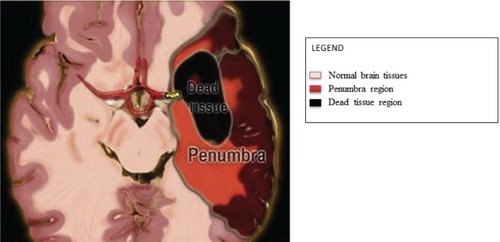
Dementia is associated with neurodegenerative disorder diversity, neuronal dysfunction, and neuronal death. Dementia occurs when the brain is affected by a specific disease or condition that causes cognitive impairment.Citation13 In the case of a stroke, one or more cognitive domains may be affected, including attention, memory, language, and orientation. The highest impact of stroke at the time of diagnosis is on the attention and executive functions rather than on memory, which may be impaired at various post-stroke intervals. Previous studies show that post-stroke memory prevalence varies from 23% to 55% 3 months after stroke, ending with a decline from 11% to 31% 1 year after stroke onset.Citation3,Citation14 Cognitive impairment after a stroke is common and leads to PSD. PSD includes all dementia types that occur after a stroke, including VaD; degenerative dementia, particularly Alzheimer’s disease (AD); or mixed dementia (VaD plus AD).Citation2 VaD, the second leading cause of dementia in the world after AD, occurs as a result of stroke. Between 1% and 4% of elderly people aged 65 years and older suffer from VaD, and its prevalence will double every 5–10 years after this age.Citation15,Citation16 VaD is characterized by impairment in the cognitive function due to vascular lesion and infarction resulting from the stroke. The clinical manifestation of VaD varies based on the size, location, and type of cerebral damage.Citation15 illustrates the cognitive impairment sequences which predispose individuals to the VCI spectrum.
Figure 4 Block diagram of vascular cognitive impairment spectrum.
The VCI spectrum can be viewed as a cognitive consequence in the cognitive domain, starting from mild cognitive impairment (MCI) and ending with severe dementia. The period beyond dementia in which the brain is at risk is called “cognitive impairment no dementia.”Citation17
MCI causes a more considerable decline in cognitive function with respect to individual age and education level, but not notably with the activities of daily life.Citation18,Citation19 Clinically, MCI is the transitional stage between early normal cognition and late severe dementia, and it is considered heterogeneous because some MCI patients develop dementia while others stay and continue as MCI patients for many years. However, by default, patients diagnosed with MCI have a high potential to develop dementia within the third month from the time dementia symptoms begin to arise.Citation2,Citation20 The most observed symptoms of MCI are limited to memory, but the patient’s daily living activities are preserved.Citation21 This article is focused on VaD as a common cause of cognitive impairment following a stroke and the effect of VaD on memory loss. It likewise discusses the available neuropsychological assessments that assess and predict the effect of dementia based on the dementia spectrum as well as aids in detecting signs of dementia, particularly memory disturbance. A number of diagnosis criteria and clinical neuropsychological assessments are combined. The most common diagnosis criteria are developed and characterized by the National Institute of Neurological Disorders and Stroke and Association Internationale pour la Recherché et l’Enseignement en Neurosciences for VaDCitation22–Citation26 and Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition criteria.Citation27 The severity of cognitive symptoms could be assessed using the Clinical Dementia Rating Scale.Citation28 The most usable test to evaluate the early dementia stages, even severity of dementia in clinical practice, is the Mini-Mental State Examination (MMSE).Citation29
Brain memory and causes of memory loss
The brain memory system refers to the process of how our brain transmits and stores available information for future use, with or without conscious awareness. The human brain memory system is a complex structure, with different functionalities, as shown in . Based on stroke location and severity, memory disorder may occur for one or more memory types, eventually ending in memory decline and loss.Citation30
Table 3 Types of memory
Memory loss can be caused by several factors, such as lifestyle, brain injury, infection, thyroid dysfunction, aging, MCI, and dementia ().Citation31
Table 4 Brain memory loss causes
This article focuses on stroke as the major cause of cognitive impairment resulting in memory decline. The effect of stroke varies based on its type, location, and severity.Citation2 After a stroke, the most prominent impairment can be recognized in the patient’s processing speed, attention, and executive function. Note that 20%–50% of stroke patients suffer from memory intricacy that manifests during the period following a stroke diagnosis. PSD, particularly VaD, causes slowing in cognitive flexibility, perceptual disorder, and impairment information retrieval at the time of stroke diagnosis. This period corresponds to MCI in the VCI spectrum, followed by a decline in episodic memory function in case of dementia, and ending in severe dementia and impairment of all cognitive properties.Citation32–Citation35
Cognitive domain and memory assessment after a stroke
Cognitive impairment, particularly memory problems following a stroke, can be evaluated and assessed through neuropsychological assessments. Clinically, different neuropsychological assessments are used to assess cognitive dysfunction in terms of cognitive domain.Citation36 A set of standardized neuropsychological assessments have been selected due to their sensitivity for MCI and to cover different cognitive domains including memory; for example, MMSE,Citation29 Montreal Cognitive Assessment (MoCA),Citation37 and Addenbrooke’s Cognitive Examination Revised (ACE-R)Citation38 are widely used to assess the cognitive dysfunction of patients. Several validated clinical neuropsychological assessments are used to assess cognitive domain, including (but not limited to) Trail Making Test (TMT)Citation39 and Clock Drawing Test (CDT)Citation40 for attention and executive function (both are short tests that evaluate executive function),Citation18 Rey Osterrieth Figure CopyCitation41 for construction praxis test, and Phonological and Semantic Fluency Token test for language test.Citation42 Other tests (eg, Frontal Assessment Battery [FAB]Citation43) can be used as a quick and easy battery test. The Cambridge Examination for Mental Disorders of the Elderly,Citation44 is a standardized instrument that is used to investigate the cognitive domains required to diagnose dementia in multiple domains, including memory. The most common tests to assess memory evaluate memory in terms of retention, retrieval, and encoding (eg, the Wechsler Memory Scale (WMS)-RevisedCitation45 may be employed to distinguish amnesia from dementia in patients). For verbal memory, numerous assessments are used, including the WMS,Citation46 Rey Auditory Verbal Learning Test,Citation47 Rivermead Behavioral Memory Test (RBMT),Citation48 and California Verbal Learning Test.Citation48 Memory disorder in elderly dementia patients can be assessed using the Free and Cued Selective Reminding Test. This test aids in distinguishing dementia from normal aging with acceptable accuracy.Citation36
Until recently, no specific assessment was developed specifically to assess short-term memory, working memory, and long-term memory impairment following stroke VaD. Thus, evaluating memory in terms of its types to predict stroke effect on memory retrieval is important.
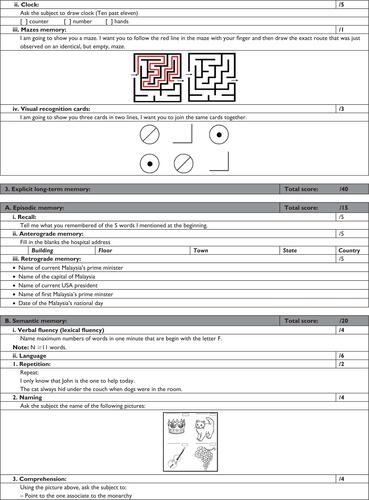
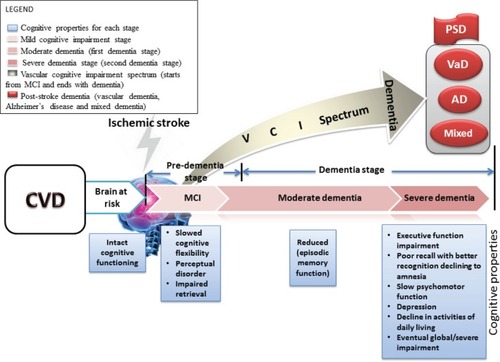
PSMA
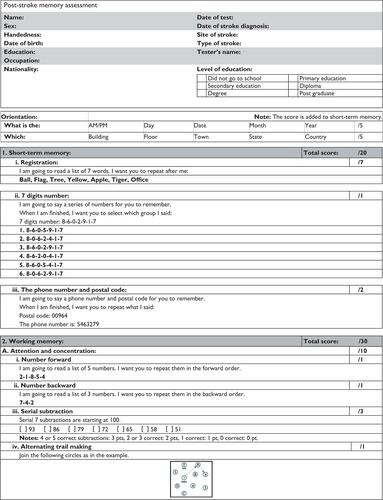
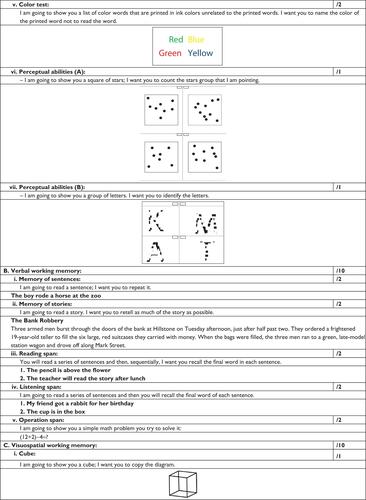
The decline in memory as a result of stroke VaD and the characterization of memory complaint based on VaD development can be assessed through a PSMA. This assessment is based on the most popular studies and is a combination of available neuropsychological assessment tests.Citation49,Citation50 Memory evaluation is proposed to be associated with memory types. Thus, short-term memory and working memory refer to the perceptual and learning areas of the cognitive domain, which are processed by the frontal lobe. Episodic and semantic long-term memory refers to memory, language, and visuospatial domains, which are processed by the parietal, medial temporal lobe, and hippocampus. Procedural memory refers to the procedural domain and is processed by the cerebellum and basil ganglia. describes the proposed PSMA, which achieves this demand. The concept integrated the most usable neuropsychological assessments (MMSE, ACE-R, MoCA, WMS-IV, RBMT, TMT A and B, CDT, FAB, Wechsler Adult Intelligence Scale – Fourth Edition, and others) and reconstructed them to evaluate memory types.Citation50
Table 5 Memory classification
PSMA was designed with inspected administration time of 30 minutes, as illustrated in the Supplementary materials. The test examines the following:
Orientation: in time and place
Short-term memory: a seven-digit number, phone number, and postal code
Working memory: attention and concentration, verbal working memory, and visuospatial working memory
Explicit long-term memory: episodic memory and semantic memory
Procedural memory.
Discussion
Neuropsychological assessments are used in evaluating and assessing cognitive impairment and dementia. Specific assessment is urgently needed to evaluate different types of memory functionalities after stroke. The present study focused on using available neuropsychological assessments to develop a PSMA scheme based on scientific knowledge, which is available through neuropsychological testing. PSMA may help provide impetus to detect the earliest stages of dementia before significant mental decline. Therefore, efforts are being exerted to use more than one assessment to evaluate cognitive impairment and memory dysfunction. For instance, the MMSE is a brief test with extensive international usage; however, several studies have mentioned that the MMSE alone can be used in a sensitive test to detect cognitive impairment, except if cutoff is increased or combined with other neuropsychological tests.Citation51,Citation52 Therefore, the MMSE was used with MoCA and ACE-R to detect MCI because the last two assessments are used to assess early stages of dementia and executive function, as well as identify frontal subcortical infarction.Citation50,Citation53,Citation54 In addition, ACE-R has good sensitivity for dementia, whereas MoCA is specifically used in MCI screening. Moreover, TMT, Stroop, and CDT tests can be used with the MMSE to evaluate frontal lesion verbal fluency, and visuospatial skills can be evaluated through Rey Osterrieth figure recall. FAB has been reported to identify frontal temporal lobe dysfunction.Citation55 MMSE, ACE-R, MoCA, and FAB characteristics are shown in . It can be noticed from the table that the administration time ranged from 35–45 minutes for four assessments. The PSMA administration time was reduced approximately to 30 minutes. PSMA has been designed to incorporate more than one neuropsychological assessment to evaluate short-term, working, and long-term memory with less time consumed compared with multiple test usage. Using more than one assessment to evaluate patient mentality takes a longer time, resulting in patient difficulty in concentrating on the assessment items. PSMA evaluates the cognitive domain and focuses on memory types that are affected by VaD.
Table 6 Neuropsychological assessment characteristics
Conclusion
Currently, no specific neuropsychological assessment to assess memory in terms of its types exists. This article provides an overview of the effects of stroke on the brain and on cognitive impairment, including memory evaluation with the most commonly used neuropsychological tests. The article proposes a PSMA to assess different types of memory based on the available assessments. It likewise uses the widely available neuropsychological assessments to study the association between memory as a part of cognitive domain and cognitive impairment, which lead to memory decline in the period following stroke onset.
Disclosure
The authors declare that there are no conflicts of interest in this work.
References
- CullenBO’NeillBEvansJJCoenRFLawlorBAA review of screening tests for cognitive impairmentJ Neurol Neurosurg Psychiatry200778879079917178826
- LeysDHénonHMackowiak-CordolianiM-APasquierFPoststroke dementiaLancet Neurol200541175275916239182
- CummingTBMarshallRSLazarRMStroke, cognitive deficits, and rehabilitation: still an incomplete pictureInt J Stroke201381384523280268
- MohrJPStroke: Pathophysiology, Diagnosis, and ManagementElsevier Health Sciences2004
- SahathevanRBrodtmannADonnanGADementia, stroke, and vascular risk factors: a reviewInt J Stroke201271617322188853
- IemoloFDuroGRizzoCCastigliaLHachinskiVCarusoCPathophysiology of vascular dementiaImmun Ageing2009611319895675
- SiboltGCurtzeSMelkasSPoststroke dementia is associated with recurrent ischaemic strokeJ Neurol Neurosurg Psychiatry201384772272623418214
- BrottTAdamsHOlingerCPMeasurements of acute cerebral infarction: a clinical examination scaleStroke19892078648702749846
- DemarinVZavoreoIKesVBCarotid artery disease and cognitive impairmentJ Neurol Sci20123221–210711122925533
- SaccoRLAdamsRAlbersGAmerican Heart Association/American Stroke Association Council on StrokeCouncil on Cardiovascular Radiology and InterventionAmerican Academy of NeurologyGuidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack: a statement for healthcare professionals from the American Heart Association/American Stroke Association Council on Stroke: co-sponsored by the Council on Cardiovascular Radiology and Intervention: the American Academy of Neurology affirms the value of this guidelineCirculation200611310e409e44916534023
- ForemanBClaassenJQuantitative EEG for the detection of brain ischemiaCrit Care201216221622429809
- DonovanNJKendallDLHeatonSCKwonSVelozoCADuncanPWConceptualizing functional cognition in strokeNeurorehabil Neural Repair200822212213517761809
- BorsonSFrankLBayleyPJImproving dementia care: the role of screening and detection of cognitive impairmentAlzheimers Dement20139215115923375564
- SnaphaanLde LeeuwF-EPoststroke memory function in nondemented patients: a systematic review on frequency and neuroimaging correlatesStroke200738119820317158333
- McVeighCPassmorePVascular dementia: prevention and treatmentClin Interv Aging20061322918046875
- RuitenbergAOttAvan SwietenJCHofmanABretelerMMIncidence of dementia: does gender make a difference?Neurobiol Aging20012257558011445258
- JacovaCKerteszABlairMFiskJDFeldmanHHNeuropsychological testing and assessment for dementiaAlzheimer Dement200734299317
- KorczynADVakhapovaVGrinbergLTVascular dementiaJ Neurol Sci20123221–221022575403
- AnkolekarSGeeganageCAndertonPHoggCBathPMClinical trials for preventing post stroke cognitive impairmentJ Neurol Sci20102991–216817420855090
- WinbladBPalmerKKivipeltoMMild cognitive impairment – beyond controversies, towards a consensus: report of the International Working Group on Mild Cognitive ImpairmentJ Intern Med2004256324024615324367
- AndradeCRadhakrishnanRThe prevention and treatment of cognitive decline and dementia: an overview of recent research on experimental treatmentsIndian J Psychiatry2009511122519742190
- ShengBChengLFLawCBLiHLYeungKMLauKKCoexisting cerebral infarction in Alzheimer’s disease is associated with fast dementia progression: applying the National Institute for Neurological Disorders and Stroke/Association Internationale pour la Recherche et l’Enseignement en Neurosciences Neuroimaging Criteria in Alzheimer’s Disease with Concomitant Cerebral InfarctionJ Am Geriatr Soc200755691892217537094
- JackCRJrAlbertMKnopmanDSIntroduction to revised criteria for the diagnosis of Alzheimer’s disease: National Institute on Aging and the Alzheimer Association workgroupsAlzheimers Dement20117325726221514247
- AlbertMSDeKoskySTDicksonDThe diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s diseaseAlzheimers Dement20117327027921514249
- McKhannGMKnopmanDSChertkowHThe diagnosis of dementia due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s diseaseAlzheimers Dement20117326326921514250
- SperlingRAAisenPSBeckettLAToward defining the preclinical stages of Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s diseaseAlzheimers Dement20117328029221514248
- AssociationAPDiagnostic and statistical manual of mental disordersfourth editionWashington, DCAmerican Psychiatric Association1994
- HughesCPBergLDanzigerWLCobenLAMartinRLA new clinical scale for the staging of dementiaBr J Psychiatry198214065665727104545
- FolsteinMFFolsteinSEMcHughPRMini-mental stateA prac-321998
- D’EspositoMChapter 11 Working memoryGoldenbergGMillerBLHandbook of Clinical Neurology88Elsevier2008237247
- BucknerRLMemory and executive function in aging and AD: multiple factors that cause decline and reserve factors that compensateNeuron200444119520815450170
- LimCAlexanderMPStroke and episodic memory disordersNeuropsychologia200947143045305819666037
- SnaphaanLRijpkemaMvan UdenIFernandezGde LeeuwFEReduced medial temporal lobe functionality in stroke patients: a functional magnetic resonance imaging studyBrain2009132Pt 71882188819482967
- PlantonMPeifferSAlbucherJFNeuropsychological outcome after a first symptomatic ischaemic stroke with “good recovery”Eur J Neurol201219221221921631652
- CooperSGreeneJDThe clinical assessment of the patient with early dementiaJ Neurol Neurosurg Psychiatry200576Suppl 5v15v2416291917
- PasquierFEarly diagnosis of dementia: neuropsychologyJ Neurol199924616159987708
- SmithTGildehNHolmesCThe Montreal Cognitive Assessment: validity and utility in a memory clinic settingCan J Psychiatry200752532933217542384
- MathuranathPNestorPBerriosGRakowiczWHodgesJA brief cognitive test battery to differentiate Alzheimer’s disease and frontotemporal dementiaNeurology200055111613162011113213
- AmodioPWeninHDel PiccoloFVariability of trail making test, symbol digit test and line trait test in normal people. A normative study taking into account age-dependent decline and sociobiological variablesAging Clin Exp Res200214211713112092785
- ShulmanKIClock-drawing: is it the ideal cognitive screening test?Int J Geriatr Psychiatry200015654856110861923
- CaffarraPVezzadiniGDieciFZonatoFVenneriARey-Osterrieth complex figure: normative values in an Italian population sampleNeurol Sci200222644344711976975
- CarlesimoGCaltagironeCGainottiGThe Mental Deterioration Battery: normative data, diagnostic reliability and qualitative analyses of cognitive impairmentEur Neurol19963663783848954307
- DuboisBSlachevskyALitvanIPillonBThe FAB: a frontal assessment battery at bedsideNeurology200055111621162611113214
- RothMCAMDEX-R: the Cambridge examination for mental disorders of the elderlyCambridge University Press1998
- WechslerDWechsler Memory Scale – RevisedSan Antonio, TXPsychological Corporation1987
- WechslerDWechsler memory scaleNew YorkPsychological Corporation1945
- OsterriethPALe test de copie d’une figure complexeArch Psychol194430206356
- WilsonBACockburnJBaddeleyADThe Rivermead Behavioural Memory TestSuffolk, UKThames Valley Test Company1991
- PendleburySTMarizJBullLMehtaZRothwellPMMoCA, ACE-R, and MMSE Versus the National Institute of Neurological Disorders and Stroke – Canadian Stroke Network Vascular Cognitive Impairment Harmonization Standards Neuropsychological Battery After TIA and StrokeStroke201243246446922156700
- BagnoliSFailliYPiaceriISuitability of neuropsychological tests in patients with vascular dementia (VaD)J Neurol Sci20123221–2414522694976
- MoulaertVRVerbuntJAvan HeugtenCMWadeDTCognitive impairments in survivors of out-of-hospital cardiac arrest: a systematic reviewResuscitation200980329730519117659
- CaoMFerrariMPatellaRMarraCRasuraMNeuropsychological findings in young-adult stroke patientsArch Clin Neuropsychol200722213314217169527
- SikaroodiHYadegariSMiriSRCognitive impairments in patients with cerebrovascular risk factors: a comparison of Mini Mental Status Exam and Montreal Cognitive AssessmentClin Neurol Neurosurg201311581276128023290422
- KandiahNWiryasaputraLNarasimhaluKFrontal subcortical ischemia is crucial for post stroke cognitive impairmentJ Neurol Sci20113091–2929521807379
- BagnoliSFailliYPiaceriISuitability of neuropsychological tests in patients with vascular dementia (VaD)J Neurol Sci20123221414522694976
- SummersDMalloyRCT and MR imaging in the acute ischemic stroke patient: a nursing perspectiveJ Radiol Nurs2011303104115