Abstract
Dementia-related behavioral disturbances are mostly treated with antipsychotics; however, the observed beneficial effects are modest and the risk of serious adverse effects high. We report the case of a 57-year-old woman with severe early-onset Alzheimer’s disease and severe agitation, whom we treated with electroconvulsive therapy (ECT). A significant clinical improvement was achieved over eight ECT sessions, which were tolerated well without cognitive worsening, and lasted approximately 3 months. Our case demonstrates the safe and effective use of ECT in pharmacotherapy-resistant severe agitation in Alzheimer’s disease. The risk–benefit profile of ECT for dementia-related agitation should be further investigated in clinical trials.
Introduction
Agitation, referring to a syndrome involving emotional distress, excessive psychomotor activity, aggression, irritability, disinhibition, and/or vocal disruptive behaviors unexplained by apparent needs, or confusion,Citation1,Citation2 is a very common phenomenon in the course of dementia.Citation3–Citation5 It can afflict patients at any level of dementia severity, but it occurs particularly in middle to later stages.Citation3,Citation6 Agitation and resulting behavioral disturbances are closely associated with impairment in quality of life and more rapid cognitive decline on the part of the patient, caregiver distress, an increased likelihood of institutionalization, and increased health care costs.Citation7
Trials of clinical management often combine nonpharmacological behavioral interventions and pharmacotherapy. Nonpharmacological strategies, especially multisensory stimulation therapy, seem to be promising,Citation8 yet evidence in support of their efficacy is still limited,Citation9 and there is insufficient research for severely impaired patients. Pharmacotherapy usually involves psychotropic medication – mostly antipsychotics; however these show only modest benefits compared with placebo.Citation10,Citation11 Moreover, adverse effects of antipsychotics, such as extrapyramidal symptoms and excessive sedation, can be particularly dangerous in demented patients and can outweigh the moderate improvement of agitation symptoms,Citation8 emphasizing the need for other treatment options for dementia-related behavioral disturbances. It is also noteworthy that there is a definite need for medications with regulatory approval for the indication of management of agitation in patients with dementia, in most countries.
Electroconvulsive therapy (ECT) is regarded as a highly efficient and safe treatment option in severe psychiatric disorders, with only few adverse effects. Despite very rare serious adverse events, cognitive adverse effects in the elderly, including retrograde and anterograde amnesia, are common. Especially in patients with preexisting cognitive impairments, an acute cognitive deterioration occurs more often, but these impairments are reversible within weeks.Citation12 In numerous studies, the effectiveness and safety of ECT was confirmed for demented patients who also suffered from depression.Citation12–Citation18 The evidence supporting the use of ECT for the treatment of agitation and aggression in dementia is limited to several case reports,Citation19–Citation22 two case series,Citation23,Citation24 and one recent studyCitation25 but is clearly suggestive of benefit for this indication.Citation26
Case
Here, we report a case of successful use of ECT in a patient with severe early-onset Alzheimer’s disease and severe agitation, after other nonpharmacological and pharmacological interventions were exhausted.
The patient was a 57-year-old, right-handed woman with a 4-year history of rapid progressive dementia of Alzheimer type, which was previously diagnosed outwards by neuropsychological examination. The diagnosis was confirmed by magnetic resonance imaging, fluorodeoxyglucose positron emission tomography, and examination of cerebrospinal liquid with measurement of dementia parameters. Her psychiatric history included two depressive episodes 26 and 18 years previous, following critical life events, which remitted in the course of months without specific therapy. She was admitted to our clinic for evaluation and treatment of severe behavior disturbances, including severe restlessness, yelling, crying, refusal to eat and drink, physical aggression, and resisting care, which made further caretaking of the patient at home by family members impossible. On hospital admission, she exhibited highly agitated behavior with anxiety, near-continuous pacing, crying, and repetitive local outbursts, and could not be redirected. She attempted hitting unit staff during washing and feeding. Whether psychotic symptoms were partly responsible for the observed behavioral disturbances remained unclear. On the Pittsburgh Agitation Scale (PAS), which rates the severity of four behavior groups (aberrant vocalizations, motor agitation, aggressiveness, and resisting care) on a scale of 0–4Citation27 with higher scores indicating more severe agitation, she scored 11 (out of 16) points.
Verbal communication with the patient and neurocognitive evaluation was substantially hindered by impairment of language comprehension. The patient was not able to perform specific neuropsychometrics, like the Mini–Mental State examination. She had difficulties falling and staying asleep and failed to assist in performing activities of daily living.
Her medication on admission included the acetylcholinesterase inhibitor rivastigmine patch (9.5 mg/d) and antipsychotic agent quetiapine (50 mg/d). Complete blood count, electrolytes, thyroid, liver, and kidney function tests, urinalysis, electrocardiogram, and physical exam were all normal.
Her agitation symptoms proved unresponsive to combined behavioral therapy. Multiple trials of various psychopharmacologic agents were also ineffective: no improvement could be observed with quetiapine at increased doses (up to 175 mg/d), risperidone (up to 2.5 mg/d), melperone (up to 100 mg/d), and pipamperone (up to 80 mg/d). In due consideration of depressive episodes in her medical history, we started an antidepressive combination therapy with sertraline (200 mg/d) and mirtazapine (30 mg/d), which induced an improvement of sleep but no decrease in agitated behavior. Treatment with lorazepam (up to 4 mg/d) brought about a temporary affective loosening, which lasted only 4 days.
After 9 weeks in our hospital, ECT was initiated. At this time, the patient was receiving rivastigmine (9.5 mg/d), sertraline (200 mg/d), and mirtazapine (30 mg/d). Due to her inability to give informed consent, her daughters – who were also her legal guardians – agreed to the treatment, after detailed information and discussion.
To potentially minimize reversible cognitive adverse effects of ECT we decided to use right unilateral electrode placement, dose titration (ie, evaluation of the patient’s individual seizure threshold), a treatment frequency of two sessions per week, a pulse width of 0.25 ms, and S-ketamine for anesthesia.Citation28,Citation29 ECT was administered with a Thymatron® IV device (Somatics, LLC, Lake Bluff, IL, USA). Weight-adjusted S-ketamine (~1.2 mg/kg) was used for anesthesia induction, followed by succinylcholine for muscle relaxation. The seizure threshold was determined at the first treatment (<50 mC). Following sessions were conducted at 150 mC (second – fifth session) and 200 mC (sixth – eighth session). Sufficient seizures, with respect to quantified ictal parameters, were achieved.Citation30 PAS scores were determined weekly to assess the clinical severity of agitation symptoms.
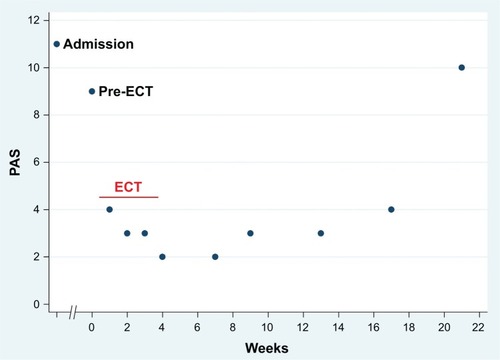
A marked difference in the clinical presentation of the patient was noted after just two ECT treatments: the patient was noticeably less agitated, and crying occurred only for short episodes. Her improvement continued throughout the entire course of eight treatments given over 26 days. She stopped yelling and crying, showed no aggression, smiled spontaneously, and was more redirectable. The patient continued to pace, but she was able to sit and lay down for longer periods. She showed significant reduction in her total PAS score from baseline (11 points) during and after ECT (2 points) (). A worsening of cognitive functions under ECT was not observed. On the contrary, the patient started to eat and drink by herself and was more cooperative in other daily care activities, like washing and dressing. Family members claimed to be able to verbally and nonverbally communicate better with the patient (eg, she followed lowest level instructions).
Figure 1 PAS scores before and during ECT course and in the follow-up period.
Abbreviations: ECT, electroconvulsive therapy; PAS, Pittsburgh Agitation Scale.
The ECT treatment was tolerated well, with signs of headache after the first three sessions. In the third week of treatment, a single self-limiting, spontaneous generalized seizure was observed.
The patient was discharged 5 days after the last ECT treatment. The improvement in agitation symptoms was present on hospital discharge. The guardians refused maintenance ECT since the patient moved away from our clinic to be taken care of by other family members. Katamnestic data on clinical presentation and behavioral symptoms of the patient were collected, by caregiver interviews, every 2 weeks over a period of 4 months after hospital discharge. Based on this information, PAS scores were determined. The improvement of agitation symptoms initiated by ECT lasted for approximately 12 weeks without any additional therapy other than rivastigmine, sertraline, and mirtazapine (). In the follow-up period, two further self-limiting, spontaneous generalized seizures were reported.
Discussion
The etiology of behavioral disturbances in dementia is poorly understood. Abnormalities of neurotransmission (eg, gamma aminobutyric acid [GABA]ergic and dopaminergic dysfunction, cholinergic and serotonergic deficiency, and noradrenergic hyperactivity) have been implicated to play a role in behavior modulation, promoting agitation and aggression.Citation31 It has been previously postulated that ECT may mediate its beneficial effects through its known enhancement of GABAergic transmission and inhibition.Citation24 It is also presumable that the efficacy of ECT relies upon its antidepressant and antipsychotic features since agitation and aggression are frequently associated with psychotic symptoms, and the underlying cause of behavioral disturbances in demented patients might be an agitated mood disorder. Clinically, it is very challenging to establish the presence or absence of a mood disorder in a highly agitated patient with severe Alzheimer’s disease who cannot be interviewed due to impairment of language comprehension. In our case, the patient had a history of two depressive episodes in her past, and the clinical improvement initiated by ECT now persisted for approximately 3 months. The overall time course of the treatment effect was thus comparable with ECT applied in major depression.Citation32 In previous case reports on ECT use for dementia-related agitation in patients without a history of affective disorders, the time to relapse varied over a wide range, from 2 weeksCitation21 to 1 year.Citation20 Successful application of maintenance ECT as well as successful reapplication of ECT in relapsed patients has been reported repeatedly.Citation19–Citation23
The patient described here tolerated the ECT treatment well without any adverse effects going beyond headache. The occurrence of spontaneous seizures was considered to be a result of extensive neurodegeneration in the course of Alzheimer’s disease and not an adverse effect of the treatment since ECT is known to have considerable anticonvulsant effectsCitation33–Citation36 and not to cause epilepsy.Citation37 Our observation of rapid effectiveness and good overall tolerance of the procedure corroborates previous reports. The concern of greater long-term cognitive adverse effects of ECT in patients with severe dementiaCitation17 is not supported by any evidence so far, considering that in most of the reported cases, patients suffering from behavioral disturbances were in the last stage of dementia. Furthermore, at least some evidence exists that in mild Alzheimer’s disease, most patients do not suffer from long-term cognitive adverse effects and some even improve, which has been attributed to an amelioration of pseudodementia.Citation12
Our case demonstrates that ECT can be safely and effectively used in treating pharmacotherapy-resistant severe agitation in early-onset Alzheimer’s disease in its last stage, without any recognizable worsening of cognitive functions. Implementation of randomized and controlled trials with ECT seems justified, to outline potential beneficial effects of this treatment compared with other clinical management strategies of dementia-associated agitation and aggression.
Disclosure
The authors report no conflicts of interest in this work.
References
- ColendaCCIIIAgitation: A conceptual overviewLawlorBABehavioral complications in Alzheimer’s diseaseWashington, DCAmerican Psychiatric Press, Inc1995317
- KongEHAgitation in dementia: concept clarificationJ Adv Nurs200552552653616268859
- LyketsosCGSteinbergMTschanzJTNortonMCSteffensDCBreitnerJCMental and behavioral disturbances in dementia: findings from the Cache County Study on Memory in AgingAm J Psychiatry2000157570871410784462
- BallardCGMargallo-LanaMFosseyJA 1-year follow-up study of behavioral and psychological symptoms in dementia among people in care environmentsJ Clin Psychiatry200162863163611561936
- Cohen-MansfieldJNonpharmacologic treatment of behavioral disorders in dementiaCurr Treat Options Neurol201315676578524136714
- SpallettaGMusiccoMPadovaniANeuropsychiatric symptoms and syndromes in a large cohort of newly diagnosed, untreated patients with Alzheimer diseaseAm J Geriatr Psychiatry201018111026103520808086
- ScarmeasNBrandtJBlackerDDisruptive behavior as a predictor in Alzheimer diseaseArch Neurol200764121755176118071039
- GitlinLNKalesHCLyketsosCGNonpharmacologic management of behavioral symptoms in dementiaJAMA2012308192020202923168825
- KongEHEvansLKGuevaraJPNonpharmacological intervention for agitation in dementia: a systematic review and meta-analysisAging Ment Health200913451252019629775
- SchneiderLSDagermanKInselPSEfficacy and adverse effects of atypical antipsychotics for dementia: meta-analysis of randomized, placebo-controlled trialsAm J Geriatr Psychiatry200614319121016505124
- BallardCHanneyMLTheodoulouMDART-AD InvestigatorsThe dementia antipsychotic withdrawal trial (DART-AD): long-term follow-up of a randomised placebo-controlled trialLancet Neurol20098215115719138567
- HausnerLDamianMSartoriusAFrölichLEfficacy and cognitive side effects of electroconvulsive therapy (ECT) in depressed elderly inpatients with coexisting mild cognitive impairment or dementiaJ Clin Psychiatry2011721919721208587
- NelsonJPRosenbergDRECT Treatment of Demented Elderly Patients with Major Depression: A Retrospective Study of Efficacy and SafetyConvuls Ther19917315716511941118
- PriceTRMcAllisterTWSafety and efficacy of ECT in depressed patients with dementia: a review of clinical experienceConvuls Ther198951617411940996
- RaoVLyketsosCGThe benefits and risks of ECT for patients with primary dementia who also suffer from depressionInt J Geriatr Psychiatry200015872973510960885
- van der WurffFBStekMLHoogendijkWJBeekmanATThe efficacy and safety of ECT in depressed older adults: a literature reviewInt J Geriatr Psychiatry2003181089490414533122
- OudmanEIs electroconvulsive therapy (ECT) effective and safe for treatment of depression in dementia? A short reviewJ ECT2012281343822330702
- HausnerLSartoriusAKranasterLFrölichLShould electroconvulsive therapy be more routinely be used in the treatment of depression in elderly patients with cognitive disturbances?Neuropsychiatry201115403407
- WuQPrenticeGCampbellJJECT treatment for two cases of dementia-related aggressive behaviorJ Neuropsychiatry Clin Neurosci2010222E10E1120463126
- GrantJEMohanSNTreatment of agitation and aggression in four demented patients using ECTJ ECT200117320520911528314
- HolmbergSKTariotPNChallapalliREfficacy of ECT for agitation in dementia: a case reportAm J Geriatr Psychiatry199644330334
- BangJPriceDPrenticeGCampbellJECT treatment for two cases of dementia-related pathological yellingJ Neuropsychiatry Clin Neurosci200820337938018806251
- SutorBRasmussenKGElectroconvulsive therapy for agitation in Alzheimer disease: a case seriesJ ECT200824323924118562945
- UjkajMDavidoffDASeinerSJEllisonJMHarperDGForesterBPSafety and efficacy of electroconvulsive therapy for the treatment of agitation and aggression in patients with dementiaAm J Geriatr Psychiatry2012201617222143072
- AcharyaDHarperDGAchtyesEDSafety and utility of acute electroconvulsive therapy for agitation and aggression in dementiaInt J Geriatr Psychiatry Epub 2014 May 16
- BurgutFTPopeoDKellnerCHECT for agitation in dementia: is it appropriate?Med Hypotheses20107515620434848
- BurnsALawlorBCraigSAssessment Scales in Old Age PsychiatryLondonMartin Dunitz Ltd1999
- KranasterLKammerer-CierniochJHoyerCSartoriusAClinically favourable effects of ketamine as an anaesthetic for electroconvulsive therapy: a retrospective studyEur Arch Psychiatry Clin Neurosci2011261857558221400226
- HoyerCKranasterLJankeCSartoriusAImpact of the anesthetic agents ketamine, etomidate, thiopental, and propofol on seizure parameters and seizure quality in electroconvulsive therapy: a retrospective studyEur Arch Psychiatry Clin Neurosci2014264325526123835527
- KranasterLHoyerCJankeCSartoriusABispectral index monitoring and seizure quality optimization in electroconvulsive therapyPharmacopsychiatry201346414715023359338
- BurkeAPathophysiology of behavioral and psychological disturbances in dementiaMcNamaraPDementia. Vol 3Santa Barbara, CAPraeger2011135158
- SackeimHAHaskettRFMulsantBHContinuation pharmacotherapy in the prevention of relapse following electroconvulsive therapy: a randomized controlled trialJAMA2001285101299130711255384
- BajboujMLangUENiehausLHellenFEHeuserINeuPEffects of right unilateral electroconvulsive therapy on motor cortical excitability in depressive patientsJ Psychiatr Res200640432232716137698
- ScottAIBoddyHThe effect of repeated bilateral electroconvulsive therapy on seizure thresholdJ ECT200016324425111005045
- KrystalADCoffeyCENeuropsychiatric considerations in the use of electroconvulsive therapyJ Neuropsychiatry Clin Neurosci1997922832929144111
- GriesemerDAKellnerCHBealeMDSmithGMElectroconvulsive therapy for treatment of intractable seizures. Initial findings in two childrenNeurology1997495138913929371927
- RayAKDoes electroconvulsive therapy cause epilepsy?J ECT201329320120523291703
