Abstract
Purpose
Vitiligo is an acquired pigmentary skin disease that can cause serious cosmetic problems. There have been numerous and well established studies that have demonstrated the comorbidity of various psychiatric disorders in patients with vitiligo. However, to our knowledge, there have been no studies investigating whether a psychiatric biomarker, such as brain-derived neurotrophic factor (BDNF), is associated with vitiligo.
Patients and methods
This study was conducted in Namık Kemal University Medical Faculty, Departments of Dermatology and Psychiatry between January 2013 and September 2014. After meeting inclusion and exclusion criteria, serum BDNF levels were assayed in 57 patients with first onset vitiligo and no known current or past psychiatric disorder and compared with BDNF levels in 58 age and sex matched healthy subjects.
Results
The age and female/male ratios were similar between groups. The mean values of serum BDNF were 1.57±0.97 ng/dL and 2.37±1.73 ng/dL in the vitiligo group and in the healthy control group, respectively. The mean BDNF level was significantly higher in the healthy control group compared with the vitiligo group (t=2.76, P=0.007).
Conclusion
This is the first study to compare serum BDNF levels between patients with vitiligo and healthy subjects. The reduced level of serum BDNF in patients with vitiligo may be directly related to the etiology of vitiligo or associated with the high percentage of psychiatric disorders in that patient population. Further studies are needed to support our preliminary results.
Keywords:
Introduction
Vitiligo is an acquired pigmentary skin disease that is characterized by the development of white macules resulting from the loss of pigment producing cells.Citation1 The disorder can develop at any age and has a prevalence of approximately 1%.Citation2 The etiology of vitiligo is unclear though factors such as autoimmunity, oxidative imbalance, and sympathetic neurogenic disturbance are thought to contribute to the pathophysiology of this skin disorder.Citation3 Vitiligo is commonly asymptomatic. However, patients with vitiligo can experience a high degree of social functional impairment.Citation4 There have been numerous studies exploring the relationship between psychiatric disorders or symptoms and vitiligo. Vitiligo patients are reported to have high scores of anxiety, depressive disorder, generalized anxiety disorder, social phobia, obsessive symptoms and hypochondria, high rates of alexithymia and avoidance behavior, and high rates of sleep disturbances.Citation5–Citation8 Stigmatization can be strongly associated with the negative psychosocial impact in patients who suffer from vitiligo.Citation9 Furthermore, we have previously reported that patients with vitiligo have a distinct temperament and character profile compared with healthy controls and patients with alopecia areata.Citation10 Vitiligo is of great interest in the field of psychosomatic disorders because of the associated psychiatric comorbidities.
Brain-derived neurotrophic factor (BDNF) is one of the most important and most researched neurotrophins that regulates synaptic plasticity. BDNF is also crucial for learning and memory processes.Citation11 It has been established that BDNF signaling in the mature human brain modulates behavior. Furthermore, in addition to its important role in learning and memory, BDNF has been associated with mood related behaviors as well as cognition. Thus, BDNF is widely studied in neuropsychiatric disorders such as schizophrenia, major depressive disorder, bipolar disorder, addiction, and eating disorders.Citation12
Previous data investigating the association between vitiligo and psychiatric disorders commonly noted that the latter emerged as a consequence of vitiligo. To our knowledge, no study has investigated serum BDNF levels in vitiligo patients without evidence of psychiatric comorbidities. Thus, we aimed to investigate whether patients with vitiligo have a biological predisposition to developing psychiatric disorders by assessing serum BDNF levels.
Material and methods
The present study was conducted in Namık Kemal University Medical Faculty, Departments of Dermatology and Psychiatry between January 2013 and September 2014. We enrolled consecutive patients admitted to the dermatology outpatient service with a diagnosis of first onset vitiligo. The definition of first onset vitiligo was clinically determined and included patients who were admitted to the dermatology outpatient service with a first time diagnosis of vitiligo and who had no previous diagnosis of any skin disease before admission to the service. All patients were referred to a senior psychiatrist for psychiatric assessment. Exclusion criteria included: subjects who were younger than 18 years old and older than 60 years old, who had a history of any psychiatric disorder or were diagnosed with a psychiatric disorder after the psychiatric examination, who had another dermatologic disease, who were following a food restriction diet for medical reasons or who were voluntarily dieting, and who did not want to participate in the study. After exclusions, 57 patients with first onset vitiligo were included in the present study. Fifty-eight age and sex matched healthy subjects consisting of hospital staff were recruited as controls. The severity of vitiligo was assessed using the “rule of nine”. The severity of anxiety and depression was assessed by the Beck Depression Inventory (BDI) and Beck Anxiety Inventory (BAI) in both the vitiligo and healthy control groups. The patients with vitiligo were also evaluated using the dermatology life quality index (DLQI).
Both patients and healthy subjects were given informed consent forms and agreed to participate in the study. The study protocol was approved by the institutional ethical committee.
Biochemical procedure
Blood samples were collected between 8 am and 10 am, after an overnight fast of at least 12 hours. The serum was extracted from the whole blood sample by centrifugation at 2,000 rpm for 15 minutes and frozen immediately. All serum samples were preserved at −80°C until analysis. Using a double-antibody sandwich enzyme-linked immunosorbent assay (ELISA) technique, BDNF serum levels were determined using a commercial kit (Sunred Biological Technology, Shanghai, People’s Republic of China). The samples were processed according to the manufacturer’s instructions. The standard curve ranged from 0.1 ng/mL to 10 ng/mL of BDNF and showed a direct relationship between the optical density and the concentration of BDNF. Two determinations of BDNF levels were made for each sample, and the result was taken as the mean of both determinations. Analytic sensitivity of BDNF ELISA is 0.05 ng/mL.
Rule of nine
The “rule of nine” assessment involves the evaluation of the head and neck, each arm, leg, and the four trunk quadrants for vitiligo patches, each comprising 9% of the total body surface area with the genitalia comprising 1%. Using the Wood’s lamp examination of depigmentation of vitiligo patients, the severity of disease is assessed with the rule of nine, which has been described as subjective and based on visual assessments.Citation13
BAI
The BAI is a self-report scale designed to evaluate the severity of physical symptoms of anxiety. Participants rate the 21 items on a 4-point Likert type severity scale from 0= “not at all” to 3= “severely, I could barely stand it”. Total response scores range from 0 to 63, with higher scores indicating more severe anxiety.Citation14
BDI
The BDI is a self-report scale designed to evaluate the severity of depressive symptoms as well as the tendency toward depression in patients. Participants rate 21 items on a 4-point Likert type severity scale from 0= “not at all” to 3. Total response scores range from 0 to 63, with higher scores indicating more severe depression.Citation15
DLQI
DLQI is an easy, self-administered survey that is the most commonly used 10-item questionnaire. It consists of questions that evaluate patients’ perceptions of the impact of the skin disease on such parameters as feelings, daily activities, leisure, work and school, personal relationships, and side effects of the treatment over the last week. The total score is 30 and higher scores define greater impairment of quality of life.Citation16,Citation17
Statistical methods
Data were analyzed using the Statistical Package for the Social Sciences-PC version 18.0 (SPSS Inc., Chicago, IL, USA). A confidence interval of 95% and a two tailed P-value less than 0.05 were considered statistically significant for all analyses. All numerical variables were tested by the Kolmogorov–Smirnov test for normality of distribution. Differences between groups in terms of age, level of serum BDNF, scores of BAI, and BDI were tested with independent sample t-tests. Differences between sexes were compared with χ2 test. Pearson’s correlation test was performed for analyzing the correlation coefficients between BDNF levels, age, scores of BAI, BDI and DLQI, and “rule of nine” in both groups separately.
Results
The mean ages were 43.63±13.48 years and 40.45±13.23 years in the vitiligo and healthy control group, respectively. The mean age was found to be similar between groups (t=0.91, P=0.61). The male/female ratio was found to be similar between groups (χ2=0.87, P=0.85). The mean values of serum BDNF were 1.57±0.97 ng/dL and 2.37±1.73 ng/dL in the vitiligo and healthy control group, respectively. The mean BDNF level was significantly higher in the healthy control group compared with the vitiligo group (t=2.76, P=0.007) (, ). The mean scores of BAI were 10.24±9.04 and 10.17±7.87 in the vitiligo and healthy control group, respectively. The mean scores of BDI were 11.21±7.32 and 10.62±7.47 in the vitiligo and healthy control group, respectively. The mean scores of BAI and BDI were similar between groups (P>0.05) (). The mean value of DLQI was 7.57±4.451 in the vitiligo group. The mean value of “rule of nine” was 5.13%±3.42% in the vitiligo patients.
Figure 1 The dot plot figure of BDNF in patients with vitiligo and healthy controls.
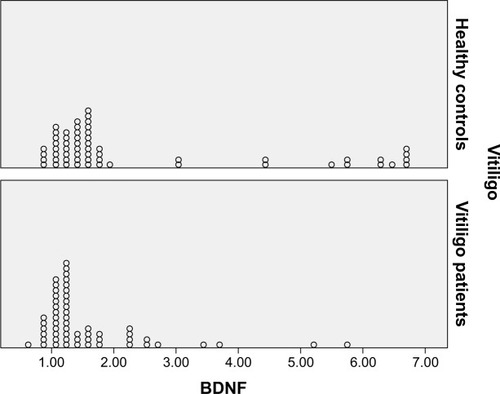
Table 1 Comparison of age, sex, BAI, BDI, and serum BDNF level in subjects with vitiligo and healthy control groups
There was no significant correlation between mean serum BDNF level, mean age, mean scores of BAI, BDI, DLQI, and mean value of “rule of nine” in the vitiligo group. There was also no significant correlation between mean serum BDNF levels and the mean age, mean scores of BAI and BDI in the healthy control group ().
Table 2 Correlation coefficients BDNF, age, BAI, BDI, DLQI, and the value of “rule of nine” in vitiligo and healthy control groups
Discussion
Psychiatric morbidity in vitiligo patients has been broadly studied. Porter et al reported a high rate of depression and low self-esteem in patients with vitiligo.Citation18 In another study, the prevalence of psychiatric disorders was approximately 35%.Citation19 The Indian studies reported a high percentage of adjustment disorders (56%–75%), depression (10%), dysthymia (7%–9%), sleep disturbance (20%), suicidal ideation (10%), and anxiety (3%).Citation8,Citation20,Citation21 A study comparing patients with vitiligo and chronic urticaria with respect to the presence of psychiatric comorbidities, revealed that patients with vitiligo had a higher rate of social phobia, dysthymia, obsessive compulsive disorder, and specific phobias.Citation22 Recently, Noh et al evaluated the degree of psychological stress and impairment of quality of life in a total of 60 patients from each group with vitiligo, atopic dermatitis patients, and healthy controls. They showed that vitiligo involves less psychological impact than atopic dermatitis.Citation23 In a recent study, Krüger and Schallreuter compared stigmatization, avoidance behavior, and difficulties in coping in 96 patients with vitiligo and 23 control subjects. They reported that stigmatization was common in 90% of patients with vitiligo.Citation24 In line with our findings, the two studies previously mentioned, found that the depression scale was similar for both patients with vitiligo and healthy controls. Though vitiligo is known to be a more emotionally disabling disease, there are frequent reports of low DLQI scores in these patients. This finding is thought to be due to the low incidence of depression.Citation25,Citation26 These previous findings suggest that there has not been any established consensus about the presence of psychiatric comorbidities in patients with vitiligo.
Neurotrophins are one of the most important signaling factors that play a leading role in axon targeting, neuronal growth, and synaptic plasticity. Of these neurotrophins, BDNF, is the best known. BDNF’s role in synaptic plasticity has been well established. It is also thought to have a number of potential roles in both the etiology and treatment of many psychiatric disorders.Citation27,Citation28 During development, BDNF is important for proper axonal growth.Citation29 BDNF is also considered to be essential for the development and survival of dopaminergic, serotonergic, GABAergic, and cholinergic neurons.Citation30 The cellular reactions following BDNF signaling develop within seconds and can support long-term potentiation that enhances synaptic strengths between neurons.Citation31
BDNF is one of the most well studied and established neurotrophins in the field of neuropsychiatry. There have been numerous preclinical and clinical studies that have investigated the association between BDNF levels and major depressive disorders, anxiety related disorders, response to stressful events, schizophrenia, bipolar disorders, eating disorders, addiction disorders, and neurodevelopmental disorders. Most of them found that decreased BDNF levels were potentially associated with the development of the aforementioned psychiatric disorders. Furthermore, numerous studies have reported improvement in BDNF levels after appropriate treatment.Citation12 While many studies have investigated psychiatric comorbidities in patients with vitiligo, there have been more reports about depressive disorders, anxiety disorders, and increased stress in these patients than psychotic disorders such as schizophrenia, bipolar disorder, etc. In particular, several studies have reported decreased serum BDNF levels in patients with depressive disorders. Further, serum BDNF was considered to be a good candidate biomarker for major depressive disorders.Citation32–Citation37 In a systematic review and meta-regression analysis, BDNF levels were found to vary in individuals with and without anxiety disorders, though levels were lower in those with an anxiety disorder.Citation38 BDNF levels are also reduced during stressful events in both animal and human studies.Citation39–Citation43
The role of neurotrophins and their receptors has been recently defined in the control of skin hemostasis and hairgrowth.Citation44–Citation48 Botchkarev et al reviewed the molecular mechanisms of normal skin and stress induced hair loss, psoriasis, and atopic dermatitis.Citation49 BDNF is a member of a family of neurotrophins. In skin, BDNF is produced by fibroblasts in vivo, while it is expressed in cutaneous nerve fibers and myocytes of arrector pili and panniculus carnosus muscles in situ.Citation48 Neurotrophins mediate proliferative and survival signals in epidermal keratinocytesCitation46,Citation48,Citation50 and, similarly, influence the proliferation and survival of melanocytes.Citation51,Citation52 From an immunological perspective, T-lymphocytes are known to produce neurotrophins in the skin, but the sub-populations of T-lymphocytes in normal and diseased skin are not clear.Citation53 In several skin diseases that are characterized by cell loss, hyper-proliferation, inflammation or autoimmune responses, there is increasing evidence that neurotrophins are involved in these pathogenic pathways. In acute psycho-emotional stress, it is known that nerve growth factor (NGF) is released into the bloodstream.Citation54 NGF triggers the release of neuropeptides from sensory nerve fibers in skinCitation55,Citation56 and can directly stimulate the release of proinflammatory cytokines.Citation57,Citation58 There has been some suggestion that NGF influences T-cell activation in psoriasis, but direct evidence is lacking. Neurotrophins can also influence numerous cellular functions in the skin with unknown cycles.Citation59
Compared to skin diseases, only a limited number of studies have investigated the role of serum BDNF in the etiology of various neuropsychiatric disorders.Citation60 Most research has focused on BDNF levels and BDNF gene polymorphism in atopic dermatitis and most report increased BDNF levels in patients with atopic dermatitis.Citation61,Citation62 Because of the protective effects of neurotrophins, specifically BDNF, on immunoglobulin E, increased serum BDNF is considered to be a potential etiologic factor in atopic dermatitis in an indirect manner. A German study that investigated the variation of BDNF and NGF genes in the German population found no significant association between atopic dermatitis and gene variations.Citation63 Increased serum BDNF levels have also been found to be associated with negative control signaling in androgenic alopecia.Citation64
The etiology of vitiligo is still unclear. However, suspected etiological factors include genetic, autoimmune, humoral immunity, cellular immunity, neurohumoral theory, auto-cytotoxic hypothesis, the biochemical theory of vitiligo, oxidative stress hypothesis, melanocytorrhagy hypothesis, and decreased melanocyte survival hypothesis.Citation2,Citation65–Citation72 Among these factors, the neurohumoral theory may pertain to our study. In this theory, dysregulation of the nervous system, either at a local or systemic level, may damage melanocytes in vitiligo. In support of this, both melanocytes and nerves arise from neural crest cells. Furthermore, some vitiligo is segmental, follows the distribution of nerves, and shows alterations during perspiration and changes in nerve structure.Citation67 Considering the regulatory role of BDNF within the nervous system, decreased serum BDNF in patients with vitiligo in our study may provide evidence to support the neurohumoral theory of vitiligo. As previously discussed, a high percentage of various psychiatric disorders exists in patients with vitiligo, which have often been explained as resulting from the cosmetic consequences of vitiligo. However, our preliminary results indicate that patients with vitiligo with no comorbid psychiatric disorder have decreased serum BDNF levels compared to age and sex matched healthy subjects. Thus, we propose that patients with vitiligo may have a predisposition to developing various psychiatric disorders compared with healthy subjects. Our study results suggest that a biomarker for psychosomatic disease may be present in patients with vitiligo, which may be significant in the field of psychosomatic disorders.
Our study has some limitations. BDNF is first produced as a precursor that is known as proBDNF. Although ELISA kits can measure BDNF, they are unable to distinguish between proBDNF and mature BDNF.Citation73,Citation74 Further studies that can measure both BDNF and proBDNF will be of great interest. Chronic diseases such as psychiatric disorders and skin diseases can impact the inflammatory process and alter the blood level of cytokines.Citation75 We did not measure serum interleukin (IL)2, IL6, and interferon-γ. However, future studies investigating these parameters would be of great interest.
Conclusion
To our knowledge, no study has investigated serum BDNF levels in patients with vitiligo. We suggest that our preliminary data seem to demonstrate a significant association between decreased serum BDNF levels and vitiligo. Our results suggest that reduced serum BDNF levels may be an etiologic factor in the development of vitiligo and may also be an indicator of future psychiatric comorbidity in patients with vitiligo. Further studies are needed to investigate BDNF and proBDNF in both serum and skin cells.
Disclosure
The authors report no conflicts of interest in this work.
References
- NjooMDWesterhofWVitiligo pathogenesis and treatmentAm J Clin Dermatol20012316718111705094
- AlikhanAFelstenLMDalyMPetronic-RosicVVitiligo: a comprehensive overview Part I. Introduction, epidemiology, quality of life, diagnosis, differential diagnosis, associations, histopathology, etiology, and work-upJ Am Acad Dermatol201165347349121839315
- TaiebAPicardoMClinical practice: VitiligoN Engl J Med2009360216016919129529
- SilvanMThe psychological aspects of vitiligoCutis200473316316715074343
- GielerUBrosigBSchneiderUVitiligo-coping behaviorDermatol Psychosom20001610
- MechriAAmriMDouarikaAAPsychiatric morbidity and quality of life in vitiligo: a case controlled studyTunis Med200684632635 French17193855
- PicardiAPasquiniPCattaruzzaMSStressful life events, social support, attachment security and alexithymia in vitiligo. A case-control studyPsychother Psychosom200372315015812707482
- SharmaNKoranneRVSinghRKPsychiatric morbidity in psoriasis and vitiligo: a comparative studyJ Dermatol200128841942311560158
- OngenaeKDierckxsensLBrochezLQuality of life and stigmatization profile in a cohort of vitiligo patients and effect of the use of camouflageDermatology2005210427928515942213
- ErfanGAlbayrakYYanikMEDistinct temperament and character profiles in first onset vitiligo but not in alopecia areataJ Dermatol201441870971525099156
- LuYChristianKLuBBDNF: a key regulator for protein synthesis dependent LTP and long-term memory?Neurobiol Learn Mem200889331232317942328
- AutryAEMonteggiaLMBrain-derived neurotrophic factor and neuropsychiatric disordersPharmacol Rev201264223825822407616
- AlghamdiKMKumarATaiebAEzzedineKAssessment methods for the evaluation of vitiligoJ Eur Acad Dermatol Venereol201226121463147122416879
- BeckATEpsteinNBrownGSteerRAAn inventory for measuring clinical anxiety: Psychometric propertiesJ Consult Clin Psychol19885668938973204199
- BeckATWardCHMendelsonMMockJErbaughJAn inventory for measuring depressionArch Gen Psychiatry1961456157113688369
- FinlayAYKhanGKDermatology life quality index (DLQI) – a simple practical measure for routine clinical useClin and Exp Dermatol1994193210216
- OzturkcanSErmertcanATEserESahinMTCross validation of the Turkish version of dermatology life quality indexInt J Dermatol200645111300130717076710
- PorterJBeufAHNordlundJJLernerABPsychological reaction to chronic skin disorders: a study of patients with vitiligoGen Hosp Psychiatry1979117377499777
- KentGAl’AbadieMPsychologic effects of vitiligo: a critical incident analysisJ Am Acad Dermatol19963568958988959947
- ParsadDDograSKanwarAJQuality of life in patients with vitiligoHealth Qual Life Outcomes200315814613564
- MattooSKHandaSKaurIGuptaNMalhotraRPsychiatric morbidity in vitiligo: prevalence and correlates in IndiaJ Eur Acad Dermatol Venereol200216657357812482039
- SukanMManerFVitiligo ve kronik ürtiker hastalarında psikiyatrik eş tan [The psychiatric diagnosis of vitiligo and chronic urticaria]Anadolu Psikiyatri Dergisi200783036 Turkish
- NohSKimMParkCOHannSKOhSHComparison of the psychological impacts of asymptomatic and symptomatic cutaneous diseases: vitiligo and atopic dermatitisAnn Dermatol201325445446124371393
- KrügerCSchallreuterKUStigmatisation, avoidance behavior and difficulties in coping are common among adult patients with vitiligoActa Derm Venereol Epub 2014101
- KentGal-AbadieMFactors affecting responses on Dermatology Life Quality Index items among vitiligo sufferersClin Exp Dermatol19962153303339136149
- BasraMKFenechRGattRMSalekMSFinlayAYThe Dermatology Life Quality Index 1994–2007: a comprehensive review of validation data and clinical resultsBr J Dermatol20081595997103518795920
- LohofAMIpNYPooMMPotentiation of developing neuromuscular synapses by the neurotrophins NT-3 and BDNFNature199336364273503538497318
- KosselAHCambridgeSBWagnerUBonhoefferTA caged Ab reveals an immediate/instructive effect of BDNF during hippocampal synaptic potentiationProc Natl Acad Sci U S A20019825147021470711724927
- YoshiiAConstantine-PatonMPostsynaptic BDNF-TrkB signaling in synapse maturation, plasticity, and diseaseDev Neurobiol201070530432220186705
- PillaiABrain-derived neurotropic factor/TrkB signaling in the pathogenesis and novel pharmacotherapy of schizophreniaNeurosignals2008162–318319318253057
- NagappanGLuBActivity-dependent modulation of the BDNF receptor TrkB: mechanisms and implicationsTrends Neurosci200528946447116040136
- ShimizuEHashimotoKOkamuraNAlterations of serum levels of brain-derived neurotrophic factor (BDNF) in depressed patients without or with antidepressantsBiol Psychiatry2003541707512842310
- SenSDumanRSanacoraGSerum brain-derived neurotrophic factor, depression, and antidepressant medications: meta-analyses and implicationsBiol Psychiatry200864652753218571629
- BrunoniARLopesMFregniFA systematic review and meta-analysis of clinical studies on major depression and BDNF levels: Implications for the role of neuroplasticity in depressionInt J Neuropsychopharmacol20081181169118018752720
- Bocchio-ChiavettoLBagnardiVZanardiniRSerum and plasma BDNF levels in major depression: a replication study and meta-analysesWorld J Biol Psychiatry201011676377320334574
- MolendijkMLBusBASpinhovenPSerum levels of brain-derived neurotrophic factor in major depressive disorder: state-trait issues, clinical features and pharmacological treatmentMol Psychiatry201116111088109520856249
- HashimotoKBrain-derived neurotrophic factor as a biomarker for mood disorders: a historical overview and future directionsPsychiatry Clin Neurosci201064434135720653908
- SulimanSHemmingsSMSeedatSBrain-Derived Neurotrophic Factor (BDNF) protein levels in anxiety disorders: systematic review and meta-regression analysisFront Integr Neurosci20132975523908608
- DumanRSMonteggiaLMA neurotrophic model for stress-related mood disordersBiol Psychiatry200659121116112716631126
- NibuyaMTakahashiMRussellDSDumanRSRepeated stress increases catalytic TrkBmRNA in rat hippocampusNeurosci Lett19992672818410400217
- RoceriMCirulliFPessinaCPerettoPRacagniGRivaMAPostnatal repeated maternal deprivation produce sage-dependent changes of brain-derived neurotrophic factor expression in selected rat brain regionsBiol Psychiatry200455770871415038999
- Kauer-Sant’AnnaMTramontinaJAndreazzaACTraumatic life events in bipolar disorder: impact on BDNF levels and psychopathologyBipolar Disord20079Suppl 112813517543031
- Grassi-OliveiraRSteinLMLopesRPTeixeiraALBauerMELow plasma brain derived neurotrophic factor and childhood physical neglect are associated with verbal memory impairment in major depression – a preliminary reportBiol Psychiatry200864428128518406398
- PausRPetersEMJEichmullerSBotchkarevVANeural mechanisms of hair growth controlJ Investig Dermatol Symp Proc1997216168
- PincelliCYaarMNerve growth factor: its significance in cutaneous biologyJ Investig Dermatol Symp Proc1997213136
- YaarMNeurotrophins in skinSieber-BlumMNeurotrophins and the neural crestLondonCRC Press1999117140
- BoniniSRasiGBracci-LaudieroMLProcoliAAloeLNerve growth factor: neurotrophin or cytokine?Int Arch Allergy Immunol20031312808412811015
- BotchkarevVABotchkarevaNVPetersEMPausREpithelial growth control by neuro-trophins: leads and lessons from the hair follicleProg Brain Res200414649351314699982
- BotchkarevVAYaarMPetersEMNeurotrophins in skin biology and pathologyJ Invest Dermatol200612681719172716845411
- BotchkarevVAMetzMBotchkarevaNVBrain-derived neurotrophic factor, neurotrophin-3, and neurotrophin-4 act as “epitheliotrophins” in murine skinLab Invest199979555757210334567
- ZhaiSYaarMDoyleSMGilchrestBANerve growth factor rescues pigment cells from ultraviolet-induced apoptosis by upregulating BCL-2 levelsExp Cell Res199622423353438612710
- StefanatoCMYaarMBhawanJModulations of nerve growth factor and Bcl-2 in ultraviolet-irradiated human epidermisJ Cutan Pathol200330635135712834482
- VegaJAGarcia-SuarezOHannestadJPerez- PerezMGermanaANeurotrophins and the immune systemJ Anat2003203111912892403
- AllevaEPetruzziSCirulliFAloeLNGF regulatory role in stress and coping of rodents and humansPharmacol Biochem Behav199654165728728540
- ArckPCHandjiskiBHagenEJoachimRKlappBFPausRIndications for a “brain-hair follicle axis (BHA)”: inhibition of keratinocyte proliferation and up-regulation of keratinocyte apoptosis in telogen hair follicles by stress and substance PFASEB J200115132536253811641256
- ArckPCHandjiskiBPetersEMStress inhibits hair growth in mice by induction of premature catagen development and deleterious perifollicular inflammatory events via neuropeptide substance P-dependent pathwaysAm J Pathol2003162380381412598315
- GronebergDASerowkaFPeckenschneiderNGene expression and regulation of nerve growth factor in atopic dermatitis mast cells and the human mast cell line-1J Neuroimmunol20051611–2879215748947
- RaapUKappANeuroimmunological findings in allergic skin diseasesCurr Opin Allergy Clin Immunol20055541942416131917
- RaychaudhuriSKRaychaudhuriSPWeltmanHFarberEMEffect of nerve growth factor on endothelial cell biology: proliferation and adherence molecule expression on human dermal microvascular endothelial cellsArch Dermatol Res20052966291295
- RaapUKappANeurotrophins in healthy and diseased skinG Ital Dermatol Venereol2010145220521120467394
- MaLGaoXHZhaoLPBrain-derived neurotrophic factor gene polymorphisms and serum levels in Chinese atopic dermatitis patientsJ Eur Acad Dermatol Venereol200923111277128119522715
- RaapUWerfelTGoltzCCirculating levels of brain derived neurotrophic factor correlate with disease severity in the intrinsic type of atopic dermatitisAllergy200661121416141817073871
- HoffjanSParwezQPetrasch-ParwezEStemmlerSVariation in the BDNF and NGFB genes in German atopic dermatitis patientsMol Cell Probes2009231353819038326
- PanchaprateepRKorkijWAsawanondaPBrain-derived nerve factor and neurotrophins in androgenetic alopeciaBr J Dermatol20111655997100221729031
- SunXXuAWeiXGenetic epidemiology of vitiligo: a study of 815 probands and their families from south ChinaInt J Dermatol200645101176118117040433
- OngenaeKVan GeelNNaeyaertJMEvidence for an autoimmune pathogenesis of vitiligoPigment Cell Res20031629010012622785
- OrecchiaGENeural pathogenesisHannSNordlundJVitiligoOxfordBlackwell Science Ltd2000142150
- Al’AbadieMSSeniorHJBleehenSSGawkrodgerDJNeuropeptide and neuronal marker studies in vitiligoBr J Dermatol199413121601657522512
- HannSKChunWAutocytotoxic hypothesis for the destruction of melanocytes as the cause of vitiligoHannSKNordlundJVitiligoOxfordBlackwell Science Ltd2000137141
- SchallreuterKUWoodJMPittelkowMRRegulation of melanin biosynthesis in the human epidermis by tetrahydrobiopterinScience19942635152144414468128228
- Le PooleICvan den WijngaardRMWesterhofWDasPKTenascin is overexpressed in vitiligolesional skin and inhibits melanocyte adhesionBr J Dermatol199713721711789292062
- LeeAYKimNHChoiWIYoumYHLess keratinocyte-derived factors related to more keratinocyte apoptosis in depigmented than normally pigmented suction blistered epidermis may cause passive melanocyte death in vitiligoJ Invest Dermatol2005124597698315854039
- YoshidaTIshikawaMIyoMHashimotoKSerum levels of mature brain-derived neurotrophic factor (BDNF) and its precursor proBDNF in healthy subjectsThe Open Clinical Chemical Journal20125712
- HashimotoKSigma-1 receptor chaperone and brain-derived neurotrophic factor: Emerging links between cardiovascular disease and depressionProg Neurobiol2013100152923044468
- TursichMNeufeldRWFrewenPAAssociation of trauma exposure with proinflammatory activity: a transdiagnostic meta-analysisTransl Psychiatry20144e41325050993
