Abstract
Altered membrane permeability is a hallmark of inflammation and ischemia with systemic spreading. Renal dysfunction is a risk factor for cardiovascular, cerebrovascular, and metabolic diseases. The aim of the present study was to assess proteinuria and urinary polyclonal light chains in acute stroke and chronic cerebrovascular disease compared with other neurologic diseases. Our results showed significantly increased levels of urinary polyclonal light chains in cerebrovascular disease compared with other neurologic diseases. The highest values of urinary polyclonal κ chains were found in acute stroke compared with chronic cerebrovascular disease and other neurologic diseases, while the level of λ chains was mainly increased in chronic cerebrovascular diseases. The shift to chronic renal failure seems to be signaled by a decreased polyclonal light chain/creatinemia ratio. The absence of a significant correlation with blood pressure and other seric parameters suggests that polyclonal light chains are an early marker of reversible vascular impairment with renal dysfunction before progression to irreversible renal failure and need for dialysis and/or intensive care.
Introduction
Altered membrane permeability is a hallmark of inflammation and incipient ischemia, as demonstrated by experimental, radiologic, and pathologic studies. Often, this is a systemic condition, involving retinal, cerebral, cardiac, pulmonary, and renal vessels.
The presence of microalbuminuria is a risk factor both in the general population or in elderly people.Citation1–Citation3 Altered kidney function parameters further worsen the clinical course and prognosis of cardiovascular, cerebrovascular, and metabolic diseases.Citation2–Citation11 They are associated with white matter lesions,Citation12,Citation13 silent brain infarction,Citation14 a high prevalence of stroke,Citation15,Citation16 worse prognosis, in terms of both short- and long-term morbidity and mortality,Citation9,Citation10 and recurrence of vascular events (stroke, myocardial infarction, heart failure).Citation10 Pathologic renal findings are also described in young patients affected with stroke, mainly related to hypertensive cardiopathy, nephroangiosclerosis, and chronic pyelonephritis.Citation17 Lastly, renal dysfunction is related to cognitive impairment and dementia.Citation18–Citation21
Urinary polyclonal light chains are low to middle molecular weight proteins, filtered at the glomerular level and reabsorbed in the tubules by megalin-cubulin receptors.Citation22–Citation25 In diabetes, the presence of polyclonal light chains is predictive of nephropathy in the absence of albuminuria.Citation26 They herald systemic inflammation and progression of renal injury to chronic renal failure.Citation27 The aim of the present study was to evaluate proteinuria and urinary polyclonal light chains in acute and chronic cerebrovascular disease.
Materials and methods
Five-hundred and fifty patients came under our observation from August 2008 to February 2010, 36/553 (0.06%) of whom bounced back. They were recruited at the Department of Emergency and Assistance or through the Ambulatory Service. They or their family gave informed written consent at admission. The study was approved by the Institutional Review Board. All the patients underwent routine blood and urine examinations, and had an electrocardiogram and computed tomography within 24–48 hours. The diagnoses were acute stroke in 139 (58 males, mean age 75.01, standard deviation [SD] ± 10.85, 81 females, mean age 80.27 ± 9.04), Glasgow Coma Scale (GCS) 11.67 ± 2.94; chronic cerebral vascular disease in 361 (162 males, mean age 73.78 ± 10.33, 199 females, mean age 77.61 ± 8.67), GCS 13.8 ± 2.03; and other neurologic diseases in 50 patients (23 males, mean age 51.79 ± 4.24, 27 females, mean age 51.72 ± 20.43), GCS 14.56 ± 1.61. Seventeen of 139 acute stroke cases (12%) were hemorrhagic. Blood pressure values were measured at admission by mercury sphygmomanometer.
Laboratory tests
Erythrocyte sedimentation rate was performed using standard vials. Serum parameters, ie, natremia, kalemia, glycemia, urea nitrogen, and creatinemia (Cre) were detected by Cobas Integra 800 Analyzer. C-reactive protein was measured by Dade Behring BN ProSpec Nephelometer. Urinary samples were treated with 0.1 M Hepes 0.1 M and 0.2 g/L sodium azide, then frozen and stored at −20°C. Proteinuria and urinary light chains were analyzed by high-resolution agarose gel electrophoresis on Sebia Hydragel 2 IF and Hydragel 2 Bence Jones immunofixation with anti-light chain antibodies and detection by a semiautomatic Hydrasis system. Some samples were analyzed by nephelometric immunoassay with specific anti-free light chain antibodies. The assay sensitivity was <1 mg/L. Normal ranges for the studied parameters are reported in . Urinary tract infection and Bence Jones-positive samples were excluded from the statistical analysis.
Table 1 Normal ranges for the studied parameters
Statistical analysis
This was performed using the unpaired t-test, for standard description of baseline characteristics and differences among the study groups, and by Pearson correlation test and logarithmic regression analysis for identification of association between the study parameters. P values < 0.05 were considered significant.
Results
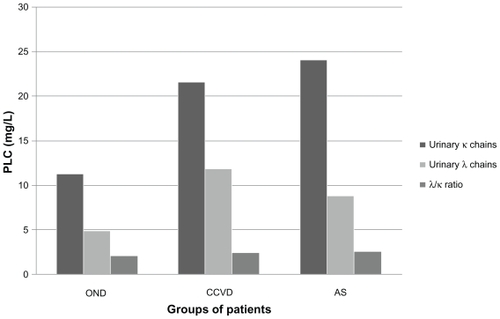
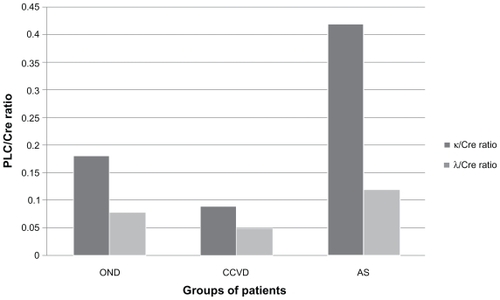
Our data showed proteinuria in 116/149 (78%) acute stroke patients (26.85 ± 42.39 mg/dL), 265/384 (69%) chronic cerebrovascular disease patients (21.49 ± 40.74 mg/dL), and 35/53 (66%) patients with other neurologic diseases (17.81 ± 37.17 mg/dL, see ). No statistically significant difference was found between proteinuria in acute stroke, chronic cerebrovascular disease, and other neurologic diseases. Urinary polyclonal light chains were mainly detected in cerebrovascular patients, with the highest significant levels of κ chains in acute stroke (24.16 ± 26 mg/L) compared with chronic cerebrovascular disease (21.65 ± 29.41 mg/L) and other neurologic diseases (11.34 ± 12.44 mg/L; acute stroke versus other neurologic diseases, P 0.001, and chronic cerebrovascular disease versus other neurologic diseases, P 0.01. The level of λ chains was 9.04 ± 9.19 mg/L in acute stroke, 11.97 ± 51.70 mg/L in chronic cerebrovascular disease, and 4.98 ± 4.27 mg/L in other neurologic diseases (acute stroke versus other neurologic diseases, P 0.004 and chronic cerebrovascular disease versus other neurologic diseases, P 0.02, ). A trend towards a difference in the urinary polyclonal light chain ratio was found between acute stroke and other neurologic diseases (acute stroke 2.62 ± 1.0, other neurologic diseases 2.15 ± 0.74, P 0.05). The polyclonal light chain/Cre ratio was increased in acute stroke (acute stroke κ/Cre 0.42 ± 0.47; acute stroke λ/Cre 0.12 ± 0.10), but was relatively decreased in chronic cerebrovascular disease (chronic cerebrovascular disease κ/Cre 0.09 ± 0.02; chronic cerebrovascular disease λ/Cre 0.05 ± 0.02) compared with acute stroke and other neurologic diseases (other neurologic diseases κ/Cre 0.17 ± 0.11; other neurologic diseases λ/Cre 0.06 ± 0.01; and acute stroke κ/Cre versus other neurologic diseases κ/Cre, P 0.001; acute stroke κ/Cre versus chronic cerebrovascular disease κ/Cre, not statistically significant; chronic cerebrovascular disease κ/Cre ratio versus other neurologic diseases κ/Cre, P 0.02; acute stroke λ/Cre versus other neurologic diseases λ/Cre, P 0.01; acute stroke λ/Cre versus chronic cerebrovascular disease λ/Cre, not statistically significant; chronic cerebrovascular disease λ/Cre versus other neurologic diseases λ/Cre, P 0.04, ). At case history, hypertension was referred by 127/149 (85.23%) of acute stroke patients, 293/384 (76.3%) of patients with chronic cerebrovascular disease, 18/53 (34%) patients with other neurologic diseases, and diabetes was present in 29/149 (19.46%) patients with acute stroke, 65/384 (16.92%) with chronic cerebrovascular disease, and 1/53 (0.01%) with other neurologic diseases. No significant correlation was found for proteinuria, urinary polyclonal light chains, systolic, diastolic, and mean arterial pressure values, and natremia, kalemia, glycemia, urea nitrogen, and creatinemia.
Conclusion
Our finding of a significant increase in urinary polyclonal light chains in acute and chronic vascular patients compared with those having other neurologic diseases, in the absence of a significant correlation with other systemic and renal parameters, suggests that urinary polyclonal light chains represent an early systemic marker of altered membrane permeability. The higher and more significant level of κ compared with λ chains in acute stroke can be explained by their higher physiologic production, up to twice the rate of λ.Citation22 Their further increase in pathologic conditions is counterbalanced by augmented elimination and reduced reabsorption at the tubular level. Λ chains more frequently form dimers that slow their renal clearance. We observed a relatively insignificant increase in urinary λ chains in chronic cerebrovascular disease compared with acute stroke. In tubular proteinuria, an increase of urinary low molecular weight proteins, as λ dimers, was detected. This is attributed to an increased excretion, a failure of proximal tubule reabsorption, and reduced catabolism.Citation23 Unfolding intermediates are found after exposure to denaturing conditions, such as urea, heat, and pH variation.Citation25 Higher seric concentrations of polyclonal light chains and a higher urinary polyclonal light chain/Cre ratio, together with increased glomerular filtration and reduced reabsorption at the tubular level have been reported.Citation24,Citation27 Serum and urinary concentrations of polyclonal light chains are related to the severity and progression of renal dysfunction.Citation27 Taken together, our data suggest that the increase in urinary polyclonal light chains may be a negative prognostic sign and represent the boundary between a reversible stage of renal dysfunction, namely nephrotic syndrome, in which there is still an opportunity for therapeutic intervention, and a definite progression to chronic kidney disease, indicated by a decreased polyclonal light chain/Cre ratio. This precedes an irreversible cascade of events characterized by reduction of glomerular filtration,Citation27 systemic interstitial and parenchymal edema, infection, tubular necrosis, progression to uremia and irreversible renal failure, and need for emergency treatment, such as ventilatory assistance and hemodialysis. Therefore, it is important to prevent systemic complications that threaten the lives of patients, prolong hospitalization, cause frequent bounce-backs, diminish quality of life, and add further costs for sanitary assistance. The sensibility and specificity of such an assay for urinary polyclonal free light chains, their predictive role concerning short- and long-term prognosis, and the association with cardiac and renal echographic and magnetic resonance imaging parameters are under evaluation.
Disclosure
The authors report no conflict of interest in this work.
References
- DamsgaardEMFrolandAJorgensenODMogensenCEMicroalbuminuria as predictor of increased mortality in elderly peopleBMJ19903002973002106959
- HillegeHLFidlerVDiercksGFPrevention of Renal and Vascular End Stage Disease (PREVEND) Study GroupUrinary albumin excretion predicts cardiovascular and non cardiovascular mortality in the general populationCirculation20021061777178212356629
- KlausenKBorch-JohnsenKFedt-RasmussenBVery low levels of microalbuminuria are associated with increased risk of coronary heart disease and death independently of renal function, hypertension and diabetesCirculation2004110323515210602
- BarzilayJIPetersonDCushmanMThe relationship of cardiovascular risk factors to microalbuminuria in older adults with or without diabetes mellitus or hypertension: The Cardiovascular Health StudyAm J Kidney Dis200444253415211434
- SeligerSLGillenDLLongstrethWTKestenbaumBStehman-BreenCOElevated risk of stroke among patients with endstage diseaseKidney Int20036460360912846756
- DiercksGFvan BovenAJHillegeHLMicroalbuminuria is independently associated with ischaemic electrocardiographic abnormalities in a large non-diabetic population. The PREVEND (Prevention of REnal and Vascular ENdstage Disease) studyEur Heart J2000211922192711071797
- GersteinHCMannJFYiQAlbuminuria and risk of cardiovascular events, death and heart failure in diabetic and nondiabetic individualsJAMA200128642142611466120
- JassalSKLangenbergCvon MuhlenDBergstromJBarrett-ConnorEUsefulness of microalbuminuria vs the metabolic syndrome as a predictor of cardiovascular disease in women and men > 40 years of age (from the Rancho Bernardo Study)Am J Cardiol20081011275128018435957
- MostofkyEWelleniusGANoheriaARenal function predicts survival in patients with acute ischemic strokeCerebrovasc Dis200928889419468220
- TsagalisGAkrivosTAlevizakiMLong-term prognosis of acute kidney injury after first acute strokeClin J Am Soc Nephrol2009461662219211666
- WachtellKIbsenHOlsenMHAlbuminuria and cardiovascular risk in hypertensive patients with left ventricular hypertrophy: The LIFE studyAnn Intern Med200313990190614644892
- KhatriMWrightCBNickolasTLChronic kidney diasease is associated with white matter hyperintensity volume. The Northern Manhattan StudyStroke2007383121312617962588
- WeinerDABartolomeiKScottTAlbuminuria, cognitive functioning and white matter hyperintensities in homebound eldersAm J Kidney Dis20095343844719070412
- KobayashiMHirawaNYatsuKRelationship between silent brain infarction and chronic kidney diseaseNephrol Dial Transplant20092420120718697797
- WannametheeSGShaperAGPerryIJSerum creatine concentration and risk of cardiovascular disease: A possible marker for increased risk of strokeStroke1997285575639056611
- AbramsonJLJurkovitzCTVaccarinoVWeintraubWSMcClellanWChronic kidney disease, anemia and incident stroke in a middle-aged, community-based population: The ARIC studyKidney Int20036461061512846757
- Arismendi-MorilloGFernandez-AbreuMCardozo-DuranJVilchez-BarriosGImportance and repercussions of renal and cardiovascular pathology on stroke in young adults: An anatomopathologic study of 52 clinical necropsiesClinics200863152018297202
- SeligerSLSiscovickDSStehman-BreenCOModerate renal impairment and risk of dementia among older adults: The Cardiovascular Health Cognition StudyJ Am Soc Nephrol2004151904191115213280
- Kurella-TamuraMWadleyVYaffeKKidney function and cognitive impairment in US adults: The REGARDS (Reasons for Geographic and Racial Differences in Stroke) StudyAm J Kidney Dis20085222723418585836
- KurellaMYaffeKShlipakMGWengerNKChertowGMChronic kidney disease and cognitive impairment in menopausal womenAm J Kidney Dis200545667615696445
- BarzilayJIFitzpatrickALLuchsingerJAlbuminuria and dementia in the elderly: A community studyAm J Kidney Dis20085221622618468749
- NezlinRNezlinRRoaldSHuman immunoglobulinsThe Immunoglobulins: Structure and FunctionNew YorkAcademic Press1998
- KlassenRBAllenPLBatumanVCrenshawKHammondTGLight chains are a ligand for megalinJ Appl Physiol20059825726315286052
- WaldmannTAStroberWMogielnickiRPThe renal handling of low molecular weight proteins. II. Disorders of serum protein catabolism in patients with tubular proteinuria, the nephrotic syndrome, or uremiaJ Clin Invest197251216221745054468
- ChungCMChiuJDConnorsLHThermodynamic stability of a kappal immunoglobulin light chain: Relevance to multiple myelomaBiophys J2005884232424215792972
- GroopLStenmanSGroopPHMakipernaaATeppoAMThe effect of exercise on urinary excretion of different size proteins in patients with insulin-dependent diabetes mellitusScand J Clin Lab Invest1990505255322122516
- HutchinsonCAHardingSHewinsPQuantitative assessment of serum and urinary polyclonal free light chains in patients with chronic kidney diseaseClin J Am Soc Nephrol200831684169018945993