Abstract
Background
We aimed to discriminate individuals with depressive state from individuals with cognitive impairment among community-dwelling people using the subjective memory complaints (SMC) scale.
Methods
The study group consisted of 289 volunteers (over 60 years old; 104 males and 185 females). Participants’ SMCs were assessed using the SMC scale. The Japanese version of the Center for Epidemiologic Studies for Depression scale and the Mini-Mental State Examination were administered. Participants whose Center for Epidemiologic Studies for Depression scores were 16 or higher were defined as the depressive group and participants whose Mini-Mental State Examination scores were less than 24 were defined as the cognitive impairment group. Exploratory factor analysis was performed to identify the factor structure of the items of the SMC scale. A multiple logistic regression analysis of the association between depressive state and cognitive impairment and the score of each factor was performed.
Results
In the final factor analysis model, six items of the SMC scale remained, and a two-factor structure was adequate. Factor 1 included the items 8, 9, and 10 about thought or the ability to think; thus, Factor 1 was defined as “thought disturbance factor”. Factor 2 included the items 1, 2, and 4 about memory or forgetfulness; thus, Factor 2 was defined as “memory disturbance factor”. In the multiple logistic regression analysis, Factor 1 was significantly associated with depressive state and Factor 2 was significantly associated with cognitive impairment.
Conclusion
For individuals with SMCs, we might be able to discriminate depressive state or depression from cognitive impairment or dementia through a detailed investigation using the SMC scale.
Introduction
A recent study has investigated the concept of subjective memory complaints (SMC) and suggested that the understanding of these complaints is of great relevance.Citation1 Some studies indicate that the presence of any type of SMC may reflect objective memory impairment or be predictive of future dementia.Citation2–Citation5 Amariglio et al investigated the detail subjective symptoms of SMCs and suggested that difficulties following a group conversation or navigating familiar streets may be associated with severe memory impairment.Citation6 In a study that used the Memory Impairment Screen (MIS) to evaluate participants’ memory function, Modrego and Gazulla suggested that the MIS score might predict the conversion to Alzheimer’s disease.Citation7 By contrast, Silva et al reported that the severity of SMCs did not predict the future conversion to dementia.Citation8
According to recent studies, SMCs are associated with not only dementia or actual cognitive impairment but also depressive state or major depressive disorder (MDD). Fischer et al studied the presence of SMCs among participants with and without MDD and reported that the subgroup of patients with MDD had significantly more SMCs;Citation9 however, there were no significant differences between the two groups with respect to objective neuropsychological assessments. The decline in the self-evaluation of patients with MDD or their inhibition of thought may cause these patients’ SMCs. Similarly, Balash et al revealed an association between the presence of SMCs and subsyndromal depression in healthy elders.Citation10 Minett et al reported that in elderly participants, the presence of SMC was significantly associated with a higher score on the Geriatric Depression Scale.Citation11 By contrast, Mowla et al investigated the cognitive functioning of patients with MDD and revealed that there was no correlation between SMCs and objective memory performance.Citation12 Therefore, the meaning of SMCs among patients with MDD in this study is questionable.
In some studies that investigated SMCs, the SMC scale was used to evaluate the severity of SMCs. The SMC scale was advocated by Schmand et al and the items of SMC scale were derived from the Cambridge Examination for Mental Disorders of the Elderly.Citation13,Citation14 SMC scale consists of 10 items: item 1 “Do you have any complaints concerning your memory?”, item 2 “Do other people find you forgetful?”, item 3 “Do you ever forget names of family members or friends?”, item 4 “Do you often forget where things are left?”, item 5 “Do you often use notes to avoid forgetting things?”, item 6 “Do you ever have difficulties in finding particular words?”, item 7 “Did you ever lose your way in your neighborhood?”, item 8 “Do you think more slowly than you used to?”, item 9 “Do your thoughts ever become confused?”, and item 10 “Do you have concentration problems?” These items were associated with difficulties in memory tasks of daily life and its internal consistency was showed.Citation2,Citation14 Ginó et al investigated both of elderly and of young healthy people using SMC scale and showed frequency of SMC and scores and the differences the characteristics of reported SMC between elderly and young people.Citation15 Pires et al suggested that item 3 of the SMC scale was important and contributed to the variance of the total SMC score in clinical settings.Citation16 Schmand et al reported that SMCs evaluated by the SMC scale might predict future dementia by longitudinal study;Citation2,Citation14 however, Silva et al investigated SMCs using the SMC scale in a clinical setting and found that the severity of SMCs did not predict the future conversion to dementia.Citation8 There is no report to study the Japanese population or patients using SMC scale.
Thus, the current study examines the association between depression and dementia and utilizes the SMC scale to evaluate the severity and quality of SMCs. We previously reported that the presence of SMCs influences depressive symptoms and cognitive functioning.Citation17 In the present study, we investigated the association between the items of the SMC scale and depressive state and cognitive impairment in community-dwelling people in Japan and identified the items that predict depression and cognitive impairment.
Methods
Participants
The study group consisted of 289 volunteers (over 60 years old; 104 males and 185 females) who participated in the Iwaki Health Promotion Project in 2013. The participants were residents of Iwaki district, Hirosaki City, in northern Japan. Iwaki district is a stable community with a population of approximately 12,000. The age and occupational distributions of this population are representative of a Japanese countryside community. Data collection for the present study and the project were approved by the Ethics Committee of Hirosaki University School of Medicine, and all subjects provided written informed consent prior to participating in the project. Demographic data (age, sex, and years of education) and lifestyle factors (smoking and drinking) were obtained from self-questionnaires and interviews.
Assessment of SMCs
Participants’ SMCs were assessed using the SMC scale. The SMC scale consists of 10 items and its total score ranges from 0 to 21. The score range of the items varied: items 6 and 7 were scored on 0 or 1; items 2, 5, 8, 9, and 10 were scored on 0–2; and items 1, 3, and 4 were scored on 0–3.
Assessment of depressive state and cognitive impairment
The Japanese version of the Center for Epidemiologic Studies for Depression (CES-D) scale was administered to all participants to measure their depressive status.Citation18 The questionnaire has been widely used to measure depressive symptoms in community populations, and it is also used as a screening tool for depression.Citation19 The CES-D is a 20-item, self-report scale that focuses on depressive symptoms within the week prior to the administration of the questionnaire. The maximum score is 60, and higher scores are associated with depression. CES-D scores of 16 or higher have generally been thought to indicate clinically relevant depressive symptoms, including both minor or subthreshold depression and MDD.Citation20,Citation21 In the present study, the CES-D score of 16 or higher was defined as depressive state and the participants whose CES-D scores 16 or higher were defined as the depressive group.
The Mini-Mental State Examination (MMSE) was given to all participants to measure their global cognitive status. This test assesses orientation to place and time, short-term memory, episodic long-term memory, subtraction, ability to construct a sentence, and oral language ability. The maximum score is 30, and poor cognition is defined as a score less than 24.Citation22 In the present study, the MMSE score less than 24 was defined as cognitive impairment state and the participants with an MMSE score less than 24 were defined as the cognitive impairment group.
Statistical analysis
Descriptive statistical analyses were performed to describe the demographic and clinical variables. To compare the characteristics of the groups according to sex, depressive state, and cognitive impairment, an unpaired Student’s t-test or Fisher’s exact test was used to analyze variables.
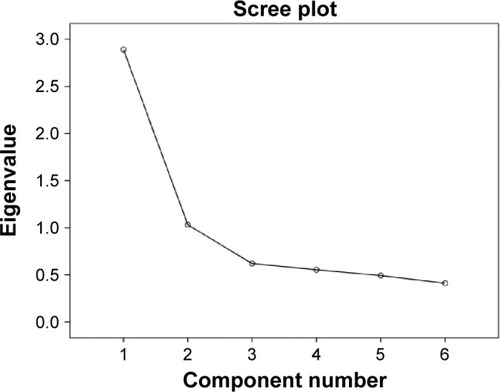
Exploratory factor analysis was performed to identify the factor structure of the items of the SMC scale. We used Bartlett’s test of sphericity to confirm the sufficient variability of the data for factor analysis. Estimation of the factors was performed by factoring the Pearson’s correlation matrix by the maximum likelihood method with an oblique Promax rotation. Factor loadings with a minimum value in the range of ±0.40 were defined as building criteria for the exploratory factor analysis model. The items that did not reach a factor loading of ±0.40 were deleted from the model, and the remaining items were reanalyzed. The number of factors was determined by a scree plot and the Kaiser–Guttman rule; we adapted the factors with eigenvalue >1 for the model.
A direct multiple logistic regression analysis of the association between depressive state and cognitive impairment and the score of each factor was performed. In addition to that, we used the models that included the variables that showed significance in the t-tests as the independent variables. We used Hosmer–Lemeshow (H–L) test to determine the model goodness-of-fit. The data were analyzed using SPSS version 22 for Windows (SPSS Japan Inc., Tokyo, Japan. A P-value of <0.05 was considered as statistically significant.
Results
Demographic data and scores
The means ± SDs of age, years of education, CES-D score, and MMSE score for all participants were 68.4±6.5, 10.8±2.0, 9.0±7.1, and 28.4±2.0, respectively. The participants consisted of 104 male (36.0%) and 185 female (64.0%) participants. Forty-six participants (15.9%) showed depressive state and ten participants (3.5%) showed cognitive impairment. shows the demographic data, the results of the depressive state and cognitive impairment assessments, and the scores of the items of the SMC scale.
Table 1 Demographic data and the SMC scale scores
There were no significant differences between male and female participants in terms of age and years of education. There were no significant differences between male and female participants in CES-D score and the prevalence rate of the depressive state, but the MMSE score and the prevalence rate of cognitive impairment were higher in male participants than in female participants. There were significant differences between the participants with and without depressive state in terms of age, MMSE score and the rate of the participants with cognitive impairment; the participants with depressive state were older and showed lower MMSE scores and higher cognitive impairment rates. There were significant differences between the participants with and without cognitive impairment in terms of age and sex; the participants with cognitive impairment were older and consisted of more male participants.
The score of item 5 of the SMC scale was significantly higher in female participants than in male participants. When comparing the participants with and without depressive state, the total score of the SMC scale and items 1, 3, 4, 6, 8, 9, and 10 were significantly higher in the participants with depressive state than in the participants without depressive state. When comparing the participants with and without cognitive impairment, item 2 was significantly higher in the participants with cognitive impairment than in the participants without cognitive impairment.
Factor analysis
shows the factor loadings of the SMC scale. According to the results of oblique Promax rotation, some items of the SMC scale were excluded according to the criteria shown above. In the final model, six items of the SMC scale remained. The Kaiser–Meyer–Olkin measure for sample adequacy was 0.797, and Bartlett’s test of sphericity was P<0.001. shows the scree plot. According to the Kaiser–Guttman rule and scree plot, a two-factor structure was adequate.
Table 2 Factor loadings of the SMC scale items
Factor 1 included the items about thought or the ability to think; thus, Factor 1 was defined as “thought disturbance factor”. Factor 2 included the items about memory or forgetfulness; thus, Factor 2 was defined as “memory disturbance factor”. The correlation coefficient between Factors 1 and 2 was 0.587.
Multiple logistic regression analysis
shows the results of the multiple logistic regression analysis that used Factors 1 and 2 to predict depressive state and cognitive impairment.
Table 3 Results of logistic regression analysis
Using depressive state as the dependent factor, Factor 1 was significantly associated with depressive state, but Factor 2 was not; model 1. Using cognitive impairment as the dependent factor, Factor 2 was significantly associated with cognitive impairment, but Factor 1 was not; model 2. Factors 1 and 2 showed different associations with depressive state and cognitive impairment; Factor 1 predicted depressive state, and Factor 2 predicted cognitive impairment. P-values of H–L tests of models 1 and 2 were 0.870 and 0.055, respectively.
According to the results of the t-tests shown above, age and sex were defined as the important variables, so these were included as the independent variables in further models of multiple logistic regression analysis. In model 3, which included age and sex as independent variables, Factor 1 was similarly and significantly associated with depressive state, but Factor 2 was not. In model 4, which included age and sex as independent variables, Factors 1 and 2 were not significantly associated with cognitive impairment, but age and sex showed a significant association. P-values of H–L tests of models 1 and 2 were 0.825 and 651, respectively.
Discussion
In the present study, we identified the SMC scale items and factors that are significantly associated with depressive state and cognitive impairment. This current report is the first to investigate the SMC items and discriminate the factors associated with depressive state and cognitive impairment. We might discriminate depressive state from cognitive impairment or screen for these diagnoses by administering the SMC scale and focusing on the items included in Factors 1 and 2 for patients with SMCs.
The SMC scale might have the potential to more easily discriminate depressive state from cognitive impairment than other tools, because the scale is a simple self-report questionnaire and participants might be able to complete it quickly. In a previous study, Monette and Leach investigated the discrimination of mild cognitive impairment and depression using the Kaplan–Baycrest Neurocognitive Assessment (KBNA).Citation23 They revealed that the assessment of KBNA had the potential to distinguish participants with depression from participants with mild cognitive impairment among participants with SMCs. Whereas we investigated community-dwelling people in the present study, Monette and Leach investigated only participants with SMCs; thus, their study was more clinical. Furthermore, it takes approximately 50–65 minutes to assess the KBNA.Citation23 A simpler and more clinical assessment tool is needed for the strict and useful discrimination of depression and dementia in clinical settings.
The items of the SMC scale refer to general subjective symptoms about memory, but in the present study, items 8 (“Do you think more slowly than you used to?”), 9 (“Do your thoughts ever become confused?”), and 10 (“Do you have concentration problems?”) were significantly associated with depressive state according to the results of the multiple logistic regression analysis. The symptoms that are presented in these items are frequent and common in depression and are included in the diagnostic criteria of major depressive episode in the Diagnostic and Statistical Manual of Mental Disorders-5; thus, it is easy to understand why these items (Factor 1) are associated with depressive state.
The meaning of discussing the association between depressive state and SMCs was questionable because the results of previous reports on the association were inconsistent.Citation9–Citation12 Typically, assessments of SMCs were very general and included symptoms other than memory symptoms or symptoms associated with only dementia. We might be able to show consistent results concerning the association between depression and SMCs by focusing on depression or depressive symptoms. According to the results of the present study, we should pay attention to depressive symptoms other than SMCs when we evaluate the neuropsychiatric symptoms of patients with SMCs using a scale.
Limitations
There were some limitations of the present study. First, we only investigated community-dwelling people. We believe that the SMC scale is useful for screening depressive state and cognitive impairment in individuals with SMCs, but we do not know whether the results of the present study are generalizable to patients visiting clinical settings due to their SMCs. Further investigation is needed to apply the SMC scale in clinical settings. Second, in the present study, we did not investigate cutoff values to distinguish between depressive state and cognitive impairment. The critical cutoff values are more useful in clinical settings than in determining the association between some items of the SMC scale and depressive state and cognitive impairment. Third, the results lack information about sex-specific effects on the association between factors or items of the SMC scale and depressive state and cognitive impairment. Many previous studies reported sex differences in the prevalence and characteristics of depressive state and cognitive impairment, and we previously reported sex differences in the association between the presence of SMCs and depressive symptoms and cognitive function and in the prediction of the effectiveness of treatment for patients with depression.Citation17,Citation24 The investigation of the effects of sex might increase the importance of the present results. Fourth, the reliability of discriminating depressive state from cognitive impairment by Factors 1 and 2 is limited because the correlation coefficient between two factors was 0.587, and Factors 1 and 2 did not show significant associations with cognitive impairment. Age and sex might be more important in predicting cognitive impairment than Factors 1 and 2. Further investigation is required to define more reliable factors or values to discriminate these two statements.
Conclusion
We investigated the association between the items of the SMC scale and depressive state and cognitive impairment and identified the specific items and factors that were associated with depressive state and cognitive impairment. For individuals with SMCs, we might be able to discriminate depressive state or depression from cognitive impairment or dementia through a detailed investigation using the SMC scale.
Author contributions
NY-F and KN designed the study and wrote protocol. TT managed the literature searches and analysis. NS managed analysis. IT and KS collected the data. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
This study was funded by a Grant-in-Aid for Scientific Research (KAKENHI) from the Japan Society for the Promotion of Research (JSPS, 15K19239, 15K19710, and 15H04754) and a grant from the Hirosaki Research Institute for Neurosciences. The authors would like to thank all of their coworkers on this study for their skillful contributions to collecting and managing the data.
Disclosure
NY-F has received grant/research support or honoraria from, and been on the speakers of Asteras, Dainippon, Eli Lilly, GSK, Janssen-Pharma, Meiji, Mochida, MSD, Otsuka, Pfizer, Takada, and Yoshitomi. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The other authors report no conflicts of interest in this work.
References
- RobertsJLClareLWoodsRTSubjective memory complaints and awareness of memory functioning in mild cognitive impairment: a systematic reviewDement Geriatr Cogn Disord2009289510919684399
- SchmandBJonkerCGeerlingsMILindeboomJSubjective memory complaints in the elderly: depressive symptoms and future dementiaBr J Psychiatry19971713733769373429
- ClarnetteRMAlmeidaOPForstlHPatonAMartinsRNClinical characteristics of individuals with subjective memory loss in Western Australia: results from a cross-sectional surveyInt J Geriatr Psychiatry20011616817411241722
- Benito-LeonJMitchellAJVegaSBermejo-ParejaFA population-based study of cognitive function in older people with subjective memory complaintsJ Alzheimers Dis20102215917020847410
- GenzianiMStewartRBejotYAmievaHArteroSRitchieKSubjective memory impairment, objective cognitive functioning and social activity in French older people: findings from the Three Cities studyGeriatr Gerontol Int20131313914522672286
- AmariglioRETownsendMKGrodsteinFSperlingRARentzDMSpecific subjective memory complaints in older persons may indicate poor cognitive functionJ Am Geriatr Soc2011591612161721919893
- ModregoPJGazullaJThe predictive value of the memory impairment screen in patients with subjective memory complaints: a prospective studyPrim Care Companion CNS Disord201315 pii:PCC.12m01435
- SilvaDGuerreiroMFariaCMarocoJSchmandBAMendoncaASignificance of subjective memory complaints in the clinical settingJ Geriatr Psychiatry Neurol20142725926524763068
- FischerCSchweizerTAAtkinsJHNeurocognitive profiles in older adults with and without major depressionInt J Geriatr Psychiatry20082385185618311855
- BalashYMordechovichMShabtaiHGiladiNGurevichTKorczynADSubjective memory complaints in elders: depression, anxiety, or cognitive decline?Acta Neurol Scand201312734435023215819
- MinettTSDa SilvaRVOrtizKZBertolucciPHSubjective memory complaints in an elderly sample: a cross-sectional studyInt J Geriatr Psychiatry200823495417520662
- MowlaAAshkaniHGhanizadehADehbozorgiGRSabayanBChohedriAHDo memory complaints represent impaired memory performance in patients with major depressive disorder?Depress Anxiety200825E92E9617592609
- RothMTymEMountjoyCQHuppertFACamdex: The Cambridge Examination for Mental Disorders of the ElderlyCambridge, CambridgeshireCambridge University Press1988
- SchmandBJonkerCHooijerCLindeboomJSubjective memory complaints may announce dementiaNeurology1996461211258559359
- GinóSMendesTMarocoJMemory complaints are frequent but qualitatively different in young and elderly healthy peopleGerontology20105627227719776545
- PiresCSilvaDMarocoJMemory complaints associated with seeking clinical careInt J Alzheimers Dis2012201272532922536537
- TomitaTNorioYFSatoYSex differences in the prediction of the effectiveness of paroxetine for patients with major depressive disorder identified using a receiver operating characteristic curve analysis for early responseNeuropsychiatr Dis Treat20141059960624748795
- ShimaSShikanoTKitamuraTNew self-rating scales for depressionClin Psychiatry198527717723 Japanese
- ZichJMAttkissonCCGreenfieldTKScreening for depression in primary care clinics: the CES-D and the BDIInt J Psychiatry Med1990202592772265888
- BerkmanLFBerkmanCSKaslSDepressive symptoms in relation to physical health and functioning in the elderlyAm J Epidemiol19861243723883740038
- BeekmanATDeegDJVan LimbeekJBraamAWDe VriesMZVan TilburgWCriterion validity of the Center for Epidemiologic Studies Depression scale (CES-D): results from a community-based sample of older subjects in The NetherlandsPsychol Med1997272312359122304
- FolsteinMFFolsteinSEMcHughPR“Mini-mental state”. A practical method for grading the cognitive state of patients for the clinicianJ Psychiatr Res1975121891981202204
- MonetteMCLeachLDiscrimination of the cognitive profiles of MCI and depression using the KBNACan J Neurol Sci20134067067723968940
- TomitaTSugawaraNKanedaASex-specific effects of subjective memory complaints with respect to cognitive impairment or depressive symptomsPsychiatry Clin Neurosci20146817618124895733