Abstract
Objective
To determine feasibility and estimate the effect of a 10-week tai chi chuan (TCC) intervention on anxiety and sleep quality in young adults.
Participants
Seventy-five adults (18–40 years) from a predominately undergraduate midsized university.
Methods
This was an assessor blinded, randomized feasibility trial, and participants were randomized into one of three groups: 10 weeks of TCC meeting 2 times per week, 10 weeks of TCC with a DVD of the curriculum, and control group receiving a handout on anxiety management. Anxiety and sleep quality were assessed 4 times: baseline, 4 weeks, 10 weeks (immediate post-intervention), and 2 months post-intervention. Retention was defined as a participant attending the baseline assessment and at least one other assessment. Adherence to the intervention was set a priori as attendance at 80% of the TCC classes.
Results
Eighty-five percent of participants were retained during the intervention and 70% completed the 2 month follow-up assessments. To increase statistical power, the two TCC groups were combined in the analyses of anxiety and sleep quality measures. No significant changes in anxiety were found in the control group, while levels of anxiety decreased significantly over time in the two TCC groups. Sleep quality scores improved across time for all three groups, but adherent TCC participants reported greater improvement than control participants.
Conclusion
TCC may be an effective nonpharmaceutical means of improving anxiety and poor sleep quality in young adults.
Introduction
Sleep is critical for good health, and sleeping <7 h per day is associated with mortality risk and numerous chronic illnesses.Citation1,Citation2 More than one third of US respondents to the 2014 Behavioral Risk Factor Surveillance System of the Centers for Disease Control reported sleeping <7 h per night.Citation3 Young adults emerging from adolescence may be particularly vulnerable to having less sleep than needed. Their changing sleep/wake patterns are part of a wide range of complex developmental, physical, psychological, and social changes. Other factors such as use of electronic media and caffeine consumption can contribute to poor sleep quality in young adults.Citation4 People with poor sleep quality are 2–6 times more likely to develop anxiety disorders and 4 times more likely to develop psychiatric disorders in general.Citation5 In 2015, 22% of college students in the US reported that anxiety had affected their individual academic performance in the last 12 months, and 20% reported that sleep difficulties had affected their academic performance.Citation6
Pharmacological approaches to promote sleep are the most common treatment for sleep complaints. Approximately 60% of patients seeing their primary health care provider with complaints of insomnia receive a prescription for benzodiazepines or related medication.Citation7,Citation8 While medications are effective in enhancing sleep in the short run, there is limited evidence for their long-term effectiveness and little evidence that improved sleep quality persists when the medication is withdrawn.Citation9 Significant long-term risks include development of side effects or drug dependence.Citation10 As a result of the widespread recognition of psychological and behavioral influences on sleep, nonpharmacological treatments are an important part of addressing sleep complaints and include education, behavioral, and cognitive approaches. Studies have found cognitive behavioral therapy to be as effective as medication.Citation11 However, trained clinicians are not always available to young adults.
Recent reviews found supporting evidence for use of exercise as a treatment strategy for anxiety disorders and poor sleep quality.Citation12,Citation13 One exercise that may be effective in reducing anxiety and improving poor sleep quality is tai chi chuan (TCC), a Chinese martial art also transliterated as t’ai chi chuan, taijiquan, or shortened to tai chi or taiji. TCC is a mind–body exercise that has been recognized as an inherently complex intervention with multiple components that have potentially independent and synergistic therapeutic value.Citation14 The movements are characterized by complete weight shifts, deep relaxation, and mind–body integration through mental and/or visual concentration.
Evidence exists in English and Chinese research literature for the beneficial effects of TCC on physical and mental health of college students.Citation15 A recent meta-analysis found TCC to have a moderate effect on reducing anxiety symptoms (Hedges’ g=0.66; 95% confidence interval, 0.29–1.03), but the quality of the studies published in the literature is modest.Citation16 A systematic review of studies of the effects of TCC on sleep quality in adults found significantly improved sleep quality (Hedges’ g=0.89; 95% confidence interval, 0.28–1.50), but the studies reviewed included primarily middle-aged or older adults and did not use randomized controlled trials (RCTs) involving emerging young adults.Citation13 Several nonrandomized studies of college students have found improved self-reported sleep quality for those enrolled in TCC study.Citation17,Citation18 Before TCC can be widely recommended as an effective therapy for young adults suffering from anxiety and poor sleep quality, more research using proper randomized controlled and experimental methods is needed to support a causal link between TCC, anxiety symptom reduction, and improved sleep quality.
To address gaps in the current literature, a randomized feasibility study was conducted to examine the effectiveness of TCC on anxiety and sleep quality in young adults. Given the need to conduct a high-quality RCT to assess the extent that TCC can improve anxiety and sleep quality, the first objective of this study was to assess the feasibility of conducting a randomized controlled study of a TCC intervention with young adults. An important first step is collecting information regarding the ability of researchers to have participants attend TCC instruction, practice TCC outside of class time, and to return to the laboratory in a longitudinal study. Determining methods for optimizing TCC interventions are also needed. Thus, the second objective of the study was to determine whether TCC protocol adherence was improved by providing participants with an out-of-class practice aid (a DVD of the instruction). Lastly, the effect of TCC on anxiety and sleep quality was examined.
Methods
Study design
This is an assessor blinded, randomized feasibility trial, and participants were randomized into one of three groups: 10 weeks of TCC meeting 2 times per week, 10 weeks of TCC with a DVD of the curriculum, and control group receiving a handout on anxiety management. Anxiety and sleep quality were assessed 4 times: baseline, 4 weeks, 10 weeks (immediate post-intervention), and 2 months post-intervention. Approval for the study was secured from the Appalachian State University Institutional Review Board prior to initiation of any study procedures, and the protocol was registered with ClinicalTrials.gov (ID number: NCT01624168).
Participants
Participants were recruited from a college student population by email, and the surrounding community by flyers, from January 2013 to February 2014. They were invited to an initial interview to determine eligibility to participate in the study if they, 1) were 18–40 years of age, 2) were not currently involved in any mind–body exercise modality (ie, tai chi, yoga, pilates, or qigong), 3) reported mild to severe levels of anxiety on the Generalized Anxiety Disorder-7,Citation19 4) reported no greater than moderate depression symptoms (<4) on the Patient Health Questionnaire-2,Citation20 5) indicated willingness to accept randomization, and 6) were available during the blocks of time that the classes were offered. Exclusion criteria were: 1) currently receiving psychotherapy or medication for psychological problems, 2) current suicide or homicide risk, 3) current or history of psychosis, 4) current alcohol or substance dependence, 5) unstable medical condition requiring medical supervision while exercising, and 6) unwilling to maintain a stable dose of current prescription drugs.
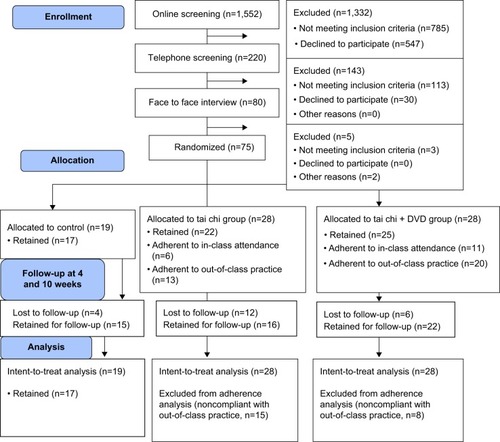
This feasibility study was powered a priori to demonstrate feasibility of recruiting and retaining the study population. With a sample size of 75, the study would be able to estimate retention rates of 80% with a margin of error of 5%. Participants were recruited to complete a brief online screening survey and then were further screened through a telephone interview and a face-to-face interview (). The initial face-to-face assessment session occurred at the beginning of the semester, within 3 weeks before the start of the TCC classes. At this session, written informed consent for participation in the study was secured before participants completed screening questionnaires and were engaged in the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental DisordersCitation21 to determine whether participants met the inclusion and exclusion criteria for the study.
Seventy-five eligible participants were randomized into one of three groups. They were randomized in a 2:3:3 ratio for control, TCC, and enhanced TCC groups, respectively. The groups were not statistically different in terms of age, gender, race, ethnicity, anxiety, or sleep quality (). All study personnel, with the exception of the study coordinator, were blind to group assignments. All the participants were compensated with $20 at each assessment period which occurred at pre-intervention, week 4 of the intervention, immediately after the 10-week intervention, and 2 months post-intervention.
Table 1 Baseline participant characteristics by group
Intervention to be evaluated
The 10-week Chen style TCC classes were taught by instructors certified in the Evidence Based Taiji™ program of Yang.Citation22 This program includes static and dynamic qigong exercises, and a 7-movement introductory form that is adaptable to persons of all ages and physical abilities. Classes were held twice a week for 1 h per class period. Participants were asked to practice 30 min daily outside of class and complete online daily logs of out-of-class practice time.
Feasibility and adherence measures
The proposed measures of feasibility and adherence were as follows:
Able to retain 80% of randomized participants during intervention period. A participant was considered to be retained if he/she attended the baseline assessment and at least one other assessment.
Able to retain 50% for 2 month follow-up assessments.
80% of retained participants will be adherent to in-class attendance (ie, attending ≥80% of classes) during the intervention.
80% of retained participants will be adherent to out-of-class practice (ie, practicing outside of class an average of ≥2 times per week) during the intervention.
50% of participants retained for follow-up will be adherent to practice (ie, practicing an average of ≥2 times per week) after the intervention.
The instructors will provide the TCC interventions according to study plan 90% of the time.
Anxiety was measured by the Spielberger state–trait anxiety inventory (STAI form Y),Citation23 a 40-item self-report inventory that differentiates between the temporary condition of “state anxiety” and the more general and long-standing quality of “trait anxiety” with higher scores indicating higher anxiety. Used in over 4,000 studies, normative data are available for this well-respected scale. Responses to the 20 state (STAI-S) questions were analyzed in this study. Cronbach’s alphas for the STAI-S for the current study across the four measurement points ranged from 0.90 to 0.93.
Sleep quality was measured by the Pittsburgh sleep quality index (PSQI),Citation24 a 19-item self-rated instrument related to normal sleep habits. The PSQI global score has a possible range of 0–21 points with higher scores indicating worse sleep quality. The global scores are a composite of seven-component scores measuring subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction. The PSQI has distinguished insomnia patients from controls, characterized the poor sleep quality of university students,Citation25,Citation26 and been positively associated with increased psychological disturbance and greater disturbance on sleep diaries.Citation27 Cronbach’s alphas for the PSQI for the current study across the four measurement points ranged from 0.53 to 0.63.
Analysis plan
Study data were collected and managed using Research Electronic Data Capture tools.Citation28 Data analyses were conducted using SPSS (SPSS Inc., Chicago, IL, USA). The main statistical objectives were to, 1) determine feasibility of the intervention, 2) optimize the intervention, and 3) examine the impact of TCC on levels of anxiety and sleep quality.
To determine study feasibility, the proportion of participants who were retained during the intervention (ie, completing the baseline and one other assessment) and after the intervention (ie, completing the 2 month follow-up assessment) was computed. In order to examine whether there were differences between anxiety and sleep measures at baseline, independent sample t-tests were conducted taking into account the differences between retained and non-retained participants. Data were examined for normality. If the data were found not to meet the assumptions of normality, both parametric and nonparametric tests were conducted. If the parametric and nonparametric test found a similar pattern of results, the results of the more familiar parametric tests were reported.
The feasibility of the intervention was determined by computing the percent of retained participants who attended class and were adherent to out-of-class practice. Specifically, two out-of-class practice proportions were computed: 1) the proportion of retained participants who, on average, practiced ≥2 times per week during the intervention, and 2) the proportion of participants retained for follow-up who averaged practicing ≥2 times per week after the intervention. Finally, the proportion of instructors that provided TCC training according to the study plan was computed.
Optimization of the intervention was examined by looking at differences in in-class and out-of-class adherence between the TCC and enhanced TCC groups using an independent samples t-test. Additionally, an exploratory supplementary analysis was conducted to determine the relationship between practice time and anxiety levels for retained participants using correlations.
To examine the impact of TCC on levels of anxiety and sleep quality, an intent-to-treat (ITT) analysis was first conducted. The ITT analysis included all participants who were randomized to the study’s conditions and provided outcome data beyond the baseline assessment. However, this analysis did not adequately test the effects of the treatment for participants who were adherent to the intervention protocol, in part due to the artificial amount of variability in the amount of practice time and attendance to classes caused by those who were not adherent to the protocol. Additionally, the smaller sample sizes of the two separate TCC groups could have resulted in type II errors. Thus, to increase statistical power and to compute a more accurate estimate of the intervention effect for those who engaged with the intervention, the two TCC groups were combined and compared to controls in a per-protocol analysis. This analysis included only the retained participants for the control group and participants in the TCC groups who were retained and adherent to out-of-class practice during the intervention.
Both the ITT and per-protocol analyses examined the differences between the groups regarding change in anxiety and sleep using a repeated measures mixed model controlling for baseline levels.Citation29,Citation30 The test of interest was the group effect (measuring an overall difference across the time points after baseline) and the group by time interaction. All mixed model analyses used an autoregressive covariance matrix, which represented the best fit of the data over time for all outcomes. While a lack of normality in the data could have an impact on the inferential tests, the estimation of the effects in linear mixed level model analyses is unbiased in the presence of the non-normality. To help supplement the inferential tests of effects, effect size estimates and post hoc power analyses were also conducted for the ITT and per-protocol analyses.
Results
Study feasibility and adherence
Of the 75 randomized participants who completed baseline measurements, 64 (85%) completed at least one other assessment period and thus met the study’s definition of a retained participant. Of the eleven participants who were not retained, three were lost to follow-up. One participant withdrew because she lost dependable transportation in a car accident, and one participant fell on ice prior to the start of TCC classes and was unable to walk. One participant gave no reason for discontinuing the study, but did notify research staff of her withdrawal from the study. The most frequently given reason for withdrawing from the study (n=5) was lack of time, often from an underestimation of how much work they had already committed themselves to in their school work and jobs.
Differences between retained and non-retained participants on anxiety and sleep measures were examined using independent samples t-tests. There were no statistically significant differences at baseline on anxiety (p=0.6, Hedges’ g=0.1) or overall sleep quality (p=0.06, Hedges’ g=0.6). No differences were found at baseline for individual components of the PSQI with the exception of habitual sleep efficiency (component 4, p=0.01, Hedges’ g=0.9). Those who withdrew had worse habitual sleep efficiency at baseline than those who were retained.
The normality distributions of the variables were examined using skewness and kurtosis statistics and comparing those values to their standard errors. Given the possible non-normal nature of the outcome data for sleep duration (component 3), habitual sleep efficiency (component 4), and use of sleeping medication (component 6), non-parametric Mann–Whitney U independent samples tests were also conducted. The patterns of parametric and non-parametric results were the same.
Seventy percent of randomized participants (n=53, 71%) responded to the online 2 month follow-up survey. None of the adverse events that were reported by study participants throughout the study were determined to be related to their participation in the study.
Intervention feasibility and adherence
With regard to the feasibility of the intervention, only 36% of retained participants were adherent to in-class attendance (ie, attended 80% of the classes). However, 68% of the participants were adherent to out-of-class practice during the intervention (ie, on average practiced 2 more times per week). Forty-five percent of the participants who were retained after the end of follow-up were adherent to out-of-class practice (ie, on average practiced 2 more times per week). All instructors were adherent to the instruction plan 100% of the time across all sections of the classes. Supplementary analyses revealed that for all TCC participants, the mean number of classes attended was ten (standard deviation, SD =6.6, range =0–20), the mean number of out-of-class practice sessions reported during the intervention was 27 (SD =22.2, range =0–70), and the mean number of practice sessions after the intervention was 12 (SD =17.8, range =0–55).
Optimization of instruction
In an ITT analysis, participants in the TCC group receiving a DVD attended on average more classes than the TCC group who did not receive a DVD (p=0.04, Hedges’ g=0.6). While receiving a DVD of TCC did not make a statistically significant difference in adherence to in-class attendance, results trended toward statistical significance (p=0.06, Hedges’ g=0.5) with participants receiving the DVD attending more classes. The supplementary practice aid did, however, have a statistically significant impact on adherence to out-of-class practice during the intervention (p=0.03, Hedges’ g=0.6) and after the intervention (p<0.01, Hedges’ g=0.7). Given the possible nonnormal nature of the outcome data, nonparametric Mann–Whitney U independent samples tests were also conducted. The pattern of results and conclusion of the study were exactly the same when either parametric or nonparametric tests were used. Thus, the study reported the more familiar parametric results. Specifically, individuals in the enhanced TCC group who received a DVD were more likely to practice outside of class during the intervention and after the intervention period than those in the group without the DVD.
An examination of the relationship between practice time and anxiety/sleep quality revealed that for all retained TCC participants regardless of intervention assignment (ie, TCC and enhanced TCC groups), greater practice time was related to lower anxiety levels at 4 weeks (r[47]=−0.3, p=0.04), but not at 10 weeks (r[42]=−0.3, p=0.06). Greater practice time was related to lower anxiety level again at 2 month follow-up (r[38]=−0.5, p<0.01). For retained TCC participants, greater practice time was not related to PSQI scores at 4 weeks (r[47]=−0.2, p=0.1) or 10 weeks (r[42]=−0.2, p=0.1) but was related to improved PSQI scores at 2 month follow-up (r[38]=−0.3, p=0.03). Minutes practiced displayed a slight positive skew, so Spearman rho correlations were also used to examine the relationship between practice time and anxiety levels. The pattern of results and conclusion of the study were the same when either Pearson or Spearman correlations were used. Thus, the study reported the more familiar Pearson correlations.
ITT estimation of effect
Using autoregressive covariance matrixes and linear mixed models, ITT analyses of changes in the STAI-S scores and PSQI across from baseline to time (4 week, 10 week, and 2 month follow-up) by group were examined. STAI-S failed to show significant improvement over the control group for either the TCC group (4 weeks: p=0.8, Hedges’ g=0.1; 10 weeks: p=0.3, Hedges’ g=0.3; 2-months: p=0.3, Hedges’ g=0.4) or the enhanced TCC group (4 weeks: p=0.6, Hedges’ g=0.2; 10 weeks: p=0.6, Hedges’ g=0.2; 2 months: p=0.6, Hedges’ g=0.2). When examining global PSQI scores, 4 week global PSQI scores were not different than control (TCC: p=0.6, Hedges’ g=0.2; enhanced TCC: p=0.7, Hedges’ g=0.1), showed mixed levels of improvement at 10 weeks (TCC: p=0.04, Hedges’ g=0.7; enhanced TCC: p=0.6, Hedges’ g=0.2), and consistent improvement at follow-up (TCC: p=0.01, Hedges’ g=0.9; enhanced TCC: p=0.04, Hedges’ g=0.4).
The results from the mixed models for the specific PSQI components showed some significant differences between the two intervention and control groups, but no clear pattern of p-values emerged. An examination of the effect size estimates suggested that the intervention groups were steadily improving from the 4 week to the 2 month follow-up compared to the control (4 week average Hedges’ g=0.2; 10 week average Hedges’ g=0.3; 2 month average Hedges’ g=0.4). Post hoc power analyses showed that the ITT tests had a weak ability to detect differences at the 3 time points (average 4 week power =0.1; average 10 week power =0.2; average 2 month follow-up power =0.3).
Given the trends in the ITT analyses and the artificial variability in practice time introduced by including those not adherent to the intervention protocol, a per-protocol analysis was conducted. Because the two TCC groups expressed similar trends in results, the two groups were combined in the per-protocol analysis. This per-protocol analysis was conducted to more accurately estimate the effect of the intervention.
Per-protocol estimation of effect
STAI-S
None of the changes from baseline in the STAI-S were significant for the control group, while levels of anxiety decreased at each of the three time points beyond baseline for the combined TCC group (). While these changes were not statistically significantly different between the control and TCC groups, an examination of the means of the two groups over time and their effect size estimates indicates that TCC had a small but increasingly positive effect on anxiety symptoms compared to the control group over time. In fact, the Hedges’ g values were within the 95% confidence interval reported in the previously mentioned meta-analysis of the effects of TCC on anxiety.Citation16
Table 2 Adherent participants’ baseline and change scores at 4 weeks, 10 weeks (immediate post-intervention), and at 2 month follow-up by treatment group
PSQI
Analyses revealed that both the control and TCC groups had improved global PSQI scores compared to baseline in week 10 and at the 2 month follow-up (). The TCC group also had statistically significant improvements from baseline in week 4. Furthermore, the improvement seen in TCC over the control group was statistically significant in week 10 and at the 2 month follow-up with effect size estimates consistent with those previously reported in the literature.Citation13
The PSQI components of sleep quality that improved at 2 months follow-up for the controls and combined TCC group were sleep quality, sleep latency, sleep duration, and daytime dysfunction (). In addition, the TCC group improved in sleep disturbances. The combined TCC group reported improvements in sleep disturbances and daytime dysfunction that were statistically significant in comparison with the controls (). The effect size estimates for these components were also consistent in magnitude to those reported in the literature.Citation13
Discussion
Overall TCC participants reported improved anxiety supporting the results of other studies on the effects of TCC on anxiety while adding to the literature as a carefully controlled randomized trial. The largest effects of TCC in this study seem to be related to self-reported improved sleep quality. The initial poor sleep quality reported by these young adult participants (65% scored in poor sleep quality range on the PSQI) is consistent with the high levels of poor sleep quality in college students reported by Lund et al.Citation25
Of particular interest is the observation that overall means in the PSQI for participants in all three groups improved over time. The extant literature is clear that part of the complexity of developmental changes in emerging adults involves changes in sleep patterns.Citation31 Some studies report worsening sleep quantity or quality over the course of a semester, while others report improvements.Citation32–Citation34 The significant improvements in self-reported sleep quality at follow-up reported by TCC participants in comparison with the control group suggest that TCC may be an effective nonpharmaceutical means of improving poor sleep quality in young adults in addition to a possible general developmental trend of improvement in sleep quality.
In terms of feasibility, the method of recruitment through an online survey resulted in a sample that had moderate to high levels of anxiety, and participants were largely willing to return for the laboratory sessions. The relatively low levels of class attendance may be explained in several ways, such as difficulty in managing competing demands on time or low motivation. Indeed, a number of participants reported difficulties in time management related to attending the instructional classes. This is consistent with the developmental tasks of young adulthood in that the transition from adolescence to young adulthood is often the first time that young adults are completely responsible for structuring their own schedules.Citation35 Earlier cohort control studies recruited students enrolled in TCC courses for academic credit.Citation17,Citation18 Over 80% of the students completed these courses, and the research measures at three time points during the semester. The requirement in the present study’s RCT design to randomize participants precluded the ability to offer academic credit to complete the TCC intervention. Improving adherence rates in college students participating in RCT research designs as an extracurricular activity is a challenge, but it is essential to find methods that increase adherence in order for the benefits of TCC to be effective.
In regard to motivation, self-determination theory defines intrinsic motivation as engaging in an activity because of its inherent satisfaction while extrinsic motivation refers to doing an activity for instrumental reasons or to comply with externally administered reward and punishment.Citation36,Citation37 Participants in a research study may be engaging in the exercises initially through extrinsic motivation (ie, identified regulation to meet the requirements of the study protocol or to receive academic credit). A recent systematic review of the literature on exercise and self-determination theory found a positive relation between more autonomous forms of motivation (ie, personally valued) and exercise.Citation38 Some evidence suggests that autonomous forms of motivation can predict initial/short-term adoption of an exercise program more than intrinsic motivation, while intrinsic motivation is more predictive of long-term exercise adherence.Citation38 Autonomy is an important aspect of intrinsic motivation, and provision of a DVD in this study may be an example of supporting the autonomy of participants.
Future study implications
While the majority of the differences found in the current study were in the expected direction, several failed to be “statistically significant” despite having effect size estimates suggesting that a meaningful difference between the groups existed. A post hoc power analysis revealed that the study was underpowered, especially with regard to detecting differences in the STAI-S (1−β=0.32). Assuming the estimates remain stable, adding 70 more participants would have provided the power needed to determine that the changes in the STAI-S measures in the TCC and control groups were statistically significant across all times. If 150 more participants were included in the study, group × time effects for the STAI-S would have been statistically significant. While better statistical power was found for the global PSQI measures (1–β=0.76), adding an additional 60 participants, assuming the estimates remain stable, would have resulted in a statistically significant group × time effect for global PSQI.
Limitations
There are several limitations to this study. The study was funded and designed as a pilot study. As such, the small sample size limited the power to find differences that might have been present. The positive results found for the influence of TCC on sleep quality were not statistically significant in the ITT model but only in the per-protocol model, thus resulting in potentially biased results. Subjective sleep quality measures often lack strong correlations with objective measures of sleep, and future research designs with objective sleep measures are needed. In addition, the adherence to class attendance was below expectations, which impacts the generalizability of the results.
The reports of worse sleep quality at baseline for the participants who withdrew from the study are important to consider in planning future research studies. The self-reported measure of sleep quality was based on sleep quality within the month prior to baseline, but it may be that participants’ trajectories of sleep quality prior to that could have influenced their energy levels and as such their ability to complete their tasks of daily living and add on the tasks of the research project. Future research designs are encouraged to take this variable into consideration.
Conclusion
This pilot study adds to the small but growing literature suggesting TCC as a possible nonpharmaceutical means for improving anxiety and poor self-reported sleep quality in young adults.
Acknowledgments
Thanks are due to the following individuals for their assistance in recruitment efforts, data collection, data entry, instruction, and safety monitoring (in alphabetical order): Jessica Alley, Ellen Androlewicz, Chris Anthony, Karen Arthur, Olumide Awelewa, Christa Brooks, Christopher Capps, Pankaj Desai, Samantha Forehand, Courtney Goodman, Stephanie Hale, Nickolas Jordan, Alex Kirk, Amanda Kosmata, Michael Landram, Bethany Malpass, Ashley Martin, John Mazzochi, Daniel Moretz, Daniel Payseur, Eric Petrie, Robert Schlagal, Rosalie Stewart, Emily Welch, Callie Whitney, Tim Winecoff, and Juliane Young. This work was supported by an Academic Research Enhancement Award (R15 AT006795) from The National Center for Complementary & Alternative Medicine (NCCAM). The content is solely the responsibility of the authors and does not necessarily represent the official views of NCCAM or the National Institutes of Health. The ClinicalTrials.gov identifier for this study is NCT01624168.
Disclosure
The authors report no conflicts of interest in this work.
References
- WatsonNFBadrMSBelenkyGJoint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society on the recommended amount of sleep for a healthy adult: methodology and discussionSleep20153831161118326194576
- GrandnerMAChakravortySPerlisMLOliverLGurubhagavatulaIHabitual sleep duration associated with self-reported and objectively determined cardiometabolic risk factorsSleep Med2014151425024333222
- LiuYWheatonAGChapmanDPCunninghamTJLuHCroftJBPrevalence of healthy sleep duration among adults – United States, 2014Morb Mortal Wkly Rep2016656137141
- OwensJAdolescent Sleep Working Group and Committee on AdolescenceInsufficient sleep in adolescents and young adults: an update on causes and consequencesPediatrics2014134e921e93225157012
- KesslerRCBerglundPDemlerOJinRMerikangasKRWaltersEELifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey ReplicationArch Gen Psychiatry200562659360215939837
- American College Health AssociationNational college health assessment II: reference group executive summaryspring2015 Available from: http://www.acha-ncha.org/docs/NCHA-II_WEB_SPRING_2015_REFERENCE_GROUP_EXECUTIVE_SUMMARY.pdfAccessed July 20, 2016
- HoebertJMSouvereinPCMantel-TeeuwisseAKLeufkensHGMvan DijkLReimbursement restriction and moderate decrease in benzodiazepine use in general practiceAnn Fam Med2012101424922230829
- MorinCMWootenVPsychological and pharmacological approaches to treating insomnia: critical issues in assessing their separate and combined effectsClin Psychol Rev1996166521542
- SmithMTPerlisMLParkAComparative meta-analysis of pharmacotherapy and behavior therapy for persistent insomniaAm J Psychiatry2002159151111772681
- MorinCMBencaRChronic insomniaLancet201237998211129114122265700
- MorinCMBootzinRRBuysseDJEdingerJDEspieCALichsteinKLPsychological and behavioral treatment of insomnia: update of the recent evidence (1998–2004)Sleep200629111398141417162986
- AsmundsonGJGFetznerMGDeboerLBPowersMBOttoMWSmitsJAJLet’s get physical: a contemporary review of the anxiolytic effects of exercise for anxiety and its disordersDepress Anxiety201330436237323300122
- RamanGZhangYMinichielloVJD’AmbrosioCWangCTai chi improves sleep quality in healthy adults and patients with chronic conditions: a systematic review and meta-analysisJ Sleep Disord Ther20132616
- WaynePMKaptchukTJChallenges inherent to t’ai chi research: part II – defining the intervention and optimal study designJ Altern Complement Med200814219119718446928
- WebsterCSLuoAYKrägelohCMoirFHenningMA systematic review of the health benefits of tai chi for students in higher educationPrev Med Rep2016310311226844196
- WangCBannuruRRamelJKupelnickBScottTSchmidCHTai chi on psychological well-being: systematic review and meta-analysisBMC Complement Altern Med20101023 Available from: http://bmccomple-mentalternmed.biomedcentral.com/articles/10.1186/1472-6882-10-23Accessed July 21, 201620492638
- CaldwellKEmeryLHarrisonMGreesonJChanges in mindfulness, well-being, and sleep quality in college students through taijiquan courses: a cohort control studyJ Altern Complement Med2011171093193821999153
- CaldwellKHarrisonMAdamsMQuinRHGreesonJDeveloping mindfulness in college students through movement based courses: effects on self-regulatory self-efficacy, mood, stress, and sleep qualityJ Am Coll Health201058543344220304755
- SpitzerRLKroenkeKWilliamsJBWLoweBA brief measure for assessing generalized anxiety disorderArch Intern Med2006166101092109716717171
- KroenkeKSpitzerRLWilliamsJBThe PHQ-9: validity of a brief depression severity measureJ Gen Intern Med200116960661311556941
- FirstMBGibbonMSpitzerRLWilliamsJUser’s Guide for the Structured Clinical Interview for DSM-IV-TR Axis I Disorders – Research VersionNew YorkBiometrics Research2002
- YangYVerkuilenJRosengrenKSEffects of a taiji and qigong intervention on the antibody response to influenza vaccine in older adultsAm J Chin Med200735459760717708626
- SpielbergerCDGorsuchRLLusheneREManual for the State-Trait Anxiety InventoryPalo Alto (CA)Consulting Psychologists Press1970
- BuysseDReynoldsCFMonkTHBermanSRKupferDThe Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and researchPsychiatry Res1989281932132748771
- LundHGReiderBDWhitingABPrichardJRSleep patterns and predictors of disturbed sleep in a large population of college studentsJ Adolesc Health20104612413220113918
- OrzechKMSalafskyDBHamiltonLAThe state of sleep among college students at a large public universityJ Am Coll Health201159761261921823956
- BuysseDJAngstJGammaAAjdacicVEichDRösslerWPrevalence, course, and comorbidity of insomnia and depression in young adultsSleep200831447348018457234
- HarrisPATaylorRThielkeRPayneJGonzalezNCondeJGResearch electronic data capture (REDCap) – a metadata-driven methodology and workflow process for providing translational research informatics supportJ Biomed Inform200942237738118929686
- LairdNWareJHRandom-effects models for longitudinal dataBiometrics1982389639747168798
- SingerJDWilletJBApplied Longitudinal Data AnalysisNew YorkOxford University Press2003
- WolfsonARAdolescents and emerging adults’ sleep patterns: new developmentsJ Adolesc Health2010462979920113914
- GreesonJMJubergMKMaytanMJamesKRogersHA randomized controlled trial of Koru: a mindfulness program for college students and other emerging adultsJ Am Coll Health201462422223324499130
- HawkinsJShawPSelf-reported sleep quality in college students: a repeated measures approachSleep19921565455491475569
- PilcherJJOttESThe relationships between sleep and measures of health and well-being in college students: a repeated measures approachBehav Med19982341701789494694
- CronceJMCorbinWRCollege and careerGrantJEPotenzaMNYoung Adult Mental HealthNew YorkOxford University Press20098095
- RyanRMDeciELSelf-determination theory and the facilitation of intrinsic motivation, social development, and well-beingAm Psychol2000551687811392867
- DeciELRyanRMHandbook of Self-determination ResearchRochester (NY)University Rochester Press2004
- TeixeiraPJCarraçaEVMarklandDSilvaMNRyanRMExercise, physical activity, and self-determination theory: a systematic reviewInt J Behav Nutr Phys Act2012978 Available from http://ijbnpa.biomedcentral.com/articles/10.1186/1479-5868-9-78Accessed July 21, 201622726453