Traumatic brain injury (TBI), the alteration of brain function or brain pathology following external force, is common in children. TBI affects the sleep of victims, and poor sleep itself can impair recovery from TBI. Due to the developing brains of children, it is especially important to understand the complex interactions between sleep and TBI. Such understanding could lead toward optimizing recovery from TBI in children. Thus, here, we introduce the main issues in this field with a specific focus on the pediatric population and point out the important gaps in knowledge that need to be filled.
TBI accounts for 60,000 pediatric hospitalizations in the USA annually.Citation1 Half of these children require critical care admission for serious injuries such as skull fractures and intracranial hemorrhage (critical TBI).Citation2 Injury and critical care hospitalization leave survivors with physical, cognitive, and psychosocial morbidities encompassed by the postintensive care syndrome.Citation3 Few studies have assessed these important morbidities in survivors of pediatric critical TBI, and interventions to improve outcomes are limited. Sleep wake disturbances (SWD) are increasingly recognized as an important morbidity following TBI and as a barrier to recovery in adult TBI and in concussion (the mildest form of TBI without identified intracranial pathology). SWD in pediatric survivors of critical TBI have been under-appreciated by clinicians and under-evaluated by researchers but may be key to improving the important myriad of sequelae suffered by these children.
Sleep is integral to many physiologic systems, and in children, it is critical for brain maturation and development.Citation4,Citation5 SWD during childhood brain development, through effects on synaptic plasticity and memory consolidation, may be particularly impactful on long-term pediatric health.Citation6,Citation7 SWD in otherwise healthy children are associated with physical, cognitive, and psychosocial impairments and may substantially compound the negative health consequences of pediatric diseases.Citation8–Citation10 SWD of any type are reported in over half of all TBI survivors, occur across all spectrums of severity and location of TBI, and persist for years after injury.Citation7,Citation11 SWD including insomnia, awakenings, daytime fatigue, and sleep disordered breathing are reported in adult TBI survivors though to date are poorly quantified in children.Citation12,Citation13 SWD after TBI are associated with impaired functional outcomes, decreased participation in activities, and reduced quality of life.Citation14,Citation15 Data from our Pediatric Neurocritical Care follow-up clinic show multiple types of SWD complicate recovery in more than half of survivors of pediatric critical TBI months after hospital discharge.Citation16 However, most pediatric critical TBI survivors do not receive this type of specialized follow-up that includes systematic evaluation of sleep or postintensive care syndrome. Currently, clinicians have little data guiding methods to identify SWD or to support therapeutic interventions for SWD following pediatric critical TBI.
While there has been a recent upswing in pediatric sleep literature, variable methodology is used in these studies and few focus on TBI.Citation17 Polysomnography is the gold standard for the diagnosis of some SWD but is not always feasible in clinical and research populations and may fail to diagnose disorders such as insomnia and excessive daytime sleepiness.Citation18 A recent review of available pediatric sleep questionnaires resulted in 183 tools reported, but only two fulfilled all appropriate psychometric criteria and only 11 fulfilled most criteria.Citation19 Actigraphy is increasingly utilized in children for sleep research providing objective data that have been validated against polysomnography for some SWD and also lacks standard methodology or accepted normative data for many measures in children.Citation20 It is likely that the combination of well-validated questionnaires and actigraphy is needed to evaluate the multidimensional aspects of SWD in pediatric critical TBI.
SWD literature is dominated by concussion patients in pediatric TBI cohorts, and available reports are often secondary evaluations of data not designed to collect sleep outcomes.Citation13 A systematic review in 2015 of SWD after pediatric TBI identified only eight studies exclusive of case reports that included children with critical TBI.Citation13 Only one study of 15 patients with critical TBI included objective actigraphy data evaluating sleep,Citation21 and only three studies used a validated sleep questionnaire.Citation8,Citation21,Citation22 A 2017 study evaluating fatigue after pediatric critical TBI showed that it remained a significant problem 12 months after injury but was not evaluated in conjunction with sleep measures.Citation23 Most prior reports do not delineate the specific type of SWD or the severity of SWD in the analysis. Additionally, prior reports stratifying injury severity by Glasgow Coma Scale did not find a significant association with SWD.Citation13,Citation24 Glasgow Coma Scale fails to incorporate other concurrent injuries, such as extremity fractures and abdominal trauma, that occur in the majority of pediatric critical TBI patients and have implications for sleep outcomes such as pain, medications, and casting.
The pathophysiology of SWD after critical TBI is unclear but has been attributed to structural and functional disruptions of sleep circuitry, circadian rhythm disturbances, hormonal dysfunction, and comorbidities such as pain and psychological disorders.Citation7 However, evaluation of disease mechanisms remains in its infancy, despite a rapidly growing body of literature.Citation7 A variety of neural networks, neurotransmitters, and neuropeptides are linked to normal and disordered sleep. After a critical TBI, many of these sleep-related systems are affected either through the primary injury or through the secondary injury related to inflammation and physiologic derangements.
Secondary injury related to inflammation has been under-evaluated in TBI with regard to sleep outcomes. TBI induces an acute systemic inflammatory response that increases neuroinflammation and directly injures the brain.Citation25–Citation28 Interleukins (ILs) and other proinflammatory cytokines, including IL-1β, IL-6, and tumor necrosis factor alpha (TNFα), are elevated in serum and cerebrospinal fluid after TBI, cross the blood–brain barrier freely after injury, and are evaluated as mediators of other TBI outcomes.Citation25–Citation28 Levels correlate with injury severity, increased intracranial pressure, increased mortality, and worsened Glasgow Outcome Score in TBI survivors.Citation28 Chronic elevations of TNFα, IL-6, and IL-1β levels weeks to months after TBI correlate with significantly worse Disability Ranking Scale, Glasgow Outcome Score, and slowed trajectory of cognitive recovery.Citation29–Citation31 The same inflammatory cytokines elevated after TBI influence sleep through damaging neurons in the hypothalamus, modifying astrocyte and microglial function, altering levels of melatonin and orexin, and impairing circadian regulation.Citation32–Citation36 SWD also potentiate chronic inflammation, and this is a proposed mechanism leading to many of the negative health consequences linked to SWD.Citation33,Citation34 Despite overlap between inflammation after critical TBI and inflammation in SWD reported separately in the literature, prior studies have not assessed the link between inflammation and SWD following critical TBI.
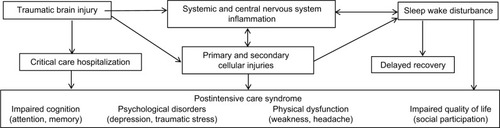
In sum, SWD after pediatric critical TBI are an important morbidity. There remain substantial gaps in available knowledge due to limited data. Research is needed to identify the incidence, risk factors, and pathophysiologic mechanisms underlying SWD. Untreated SWD delay recovery and compound other morbidities encompassed by postintensive care syndrome, including physical, neurocognitive, and psychosocial dysfunction after pediatric critical TBI (). Understanding the burden of SWD in critical TBI survivors is the first step toward identifying effective interventions for SWD and evaluating sleep as a modifiable target for other important morbidities plaguing pediatric survivors of critical TBI.
Disclosure
The authors report no conflicts of interest in this work.
References
- FaulMXLWaldMMCoronadoVG [webpage on the Internet]Traumatic Brain Injury in the United States: Emergency Department Visits, Hospitalizations and Deaths 2002–2006Atlanta (GA)Centers for Disease Control and Prevention, National Center for Injury Prevention and Control2010 Available from: https://www.cdc.gov/traumaticbrain-injuryAccessed May 10, 2017
- AsemotaAOGeorgeBPBowmanSMHaiderAHSchneiderEBCauses and trends in traumatic brain injury for United States adolescentsJ Neurotrauma2013302677522989254
- HerrupEAWieczorekBKudchadkarSRCharacteristics of postintensive care syndrome in survivors of pediatric critical illness: a systematic reviewWorld J Crit Care Med20176212413428529914
- VolkCHuberRSleep to grow smart?Arch Ital Biol20151532–39910926742664
- RingliMHuberRDevelopmental aspects of sleep slow waves: linking sleep, brain maturation and behaviorProg Brain Res2011193638221854956
- TononiGCirelliCSleep and the price of plasticity: from synaptic and cellular homeostasis to memory consolidation and integrationNeuron2014811123424411729
- SandsmarkDKElliottJELimMMSleep-wake disturbances after traumatic brain injury: synthesis of human and animal studiesSleep2017405
- ShayNYeatesKOWalzNCSleep problems and their relationship to cognitive and behavioral outcomes in young children with traumatic brain injuryJ Neurotrauma201431141305131224665961
- OwensJANeurocognitive and behavioral impact of sleep disordered breathing in childrenPediatr Pulmonol200944541742219382210
- GozalDKheirandish-GozalLNeurocognitive and behavioral morbidity in children with sleep disordersCurr Opin Pulm Med200713650550917901756
- BeebeDWKrivitzkyLWellsCTWadeSLTaylorHGYeatesKOBrief report: parental report of sleep behaviors following moderate or severe pediatric traumatic brain injuryJ Pediatr Psychol200732784585017442693
- SinghKMorseAMTkachenkoNKothareSVSleep disorders associated with traumatic brain injury-a reviewPediatr Neurol201660303627161048
- GagnerCLandry-RoyCLaineFBeauchampMHSleep-wake disturbances and fatigue after pediatric traumatic brain injury: a systematic review of the literatureJ Neurotrauma201532201539155225891946
- Aaro JonssonCCEmanuelsonIMCharlotte SmedlerAVariability in quality of life 13 years after traumatic brain injury in childhoodInt J Rehabil Res201437431732225153788
- ThamSWPalermoTMVavilalaMSThe longitudinal course, risk factors, and impact of sleep disturbances in children with traumatic brain injuryJ Neurotrauma201229115416122029569
- WilliamsCNKirbyAPiantinoJIf you build it, they will come: initial experience with a multi-disciplinary pediatric neurocritical care followup clinicChildren (Basel)20174983
- LamDJSheaSAA growth spurt in pediatric sleep researchNat Sci Sleep2016813313527199573
- MouthonALHuberRMethods in pediatric sleep research and sleep medicineNeuropediatrics201546315917025961599
- SpruytKGozalDPediatric sleep questionnaires as diagnostic or epidemiological tools: a review of currently available instrumentsSleep Med Rev2011151193220934896
- MeltzerLJMontgomery-DownsHEInsanaSPWalshCMUse of actigraphy for assessment in pediatric sleep researchSleep Med Rev201216546347522424706
- SumpterREDorrisLKellyTMcMillanTMPediatric sleep difficulties after moderate-severe traumatic brain injuryJ Int Neuropsychol Soc201319782983423601180
- OsorioMBKurowskiBGBeebeDAssociation of daytime somnolence with executive functioning in the first 6 months after adolescent traumatic brain injuryPM R20135755456223375631
- CrichtonAAndersonVOakleyEBiomarker and Quality of Life in Children with Traumatic Brain Injury GroupFatigue following traumatic brain injury in children and adolescents: a longitudinal follow-up 6 to 12 months after injuryJ Head Trauma Rehabil2017333200209
- BaumannCRWerthEStockerRLudwigSBassettiCLSleep-wake disturbances 6 months after traumatic brain injury: a prospective studyBrain2007130pt 71873188317584779
- KelleyBJLifshitzJPovlishockJTNeuroinflammatory responses after experimental diffuse traumatic brain injuryJ Neuropathol Exp Neurol20076611989100117984681
- DasMMohapatraSMohapatraSSNew perspectives on central and peripheral immune responses to acute traumatic brain injuryJ Neuroinflammation2012923623061919
- HinsonHERowellSMorrisCLinALSchreiberMAEarly fever after trauma: does it matter?J Trauma Acute Care Surg2018841192428640776
- HinsonHERowellSSchreiberMClinical evidence of inflammation driving secondary brain injury: a systematic reviewJ Trauma Acute Care Surg201578118419125539220
- LicastroFHreliaSPorcelliniEPeripheral inflammatory markers and antioxidant response during the post-acute and chronic phase after severe traumatic brain injuryFront Neurol2016718927853449
- KumarRGDiamondMLBolesJAAcute CSF interleukin-6 trajectories after TBI: associations with neuroinflammation, polytrauma, and outcomeBrain Behav Immun20154525326225555531
- KumarRGBolesJAWagnerAKChronic inflammation after severe traumatic brain injury: characterization and associations with outcome at 6 and 12 months postinjuryJ Head Trauma Rehabil201530636938124901329
- ClarkIAVisselBInflammation-sleep interface in brain disease: TNF, insulin, orexinJ Neuroinflammation2014115124655719
- KapsimalisFBastaMVarouchakisGGourgoulianisKVgontzasAKrygerMCytokines and pathological sleepSleep Med20089660361418024171
- WeschenfelderJSanderCKlugeMKirkbyKCHimmerichHThe influence of cytokines on wakefulness regulation: clinical relevance, mechanisms and methodological problemsPsychiatr Danub201224211212622706407
- OppMRCytokines and sleepSleep Med Rev20059535536416102986
- KapsimalisFRichardsonGOppMRKrygerMCytokines and normal sleepCurr Opin Pulm Med200511648148416217172