Abstract
Sleep–wake disturbances are common in liver cirrhosis and associated with impaired quality of life. The most common abnormalities are insomnia (difficulties falling asleep and maintaining sleep, or unrefreshing sleep), excessive daytime sleepiness, and sleep–wake inversion (disturbances of circadian rhythmicity). The underlying pathophysiological mechanisms for sleep disturbances in cirrhosis are complex and may include disturbed metabolism of melatonin and glucose, alterations in thermoregulation, and altered ghrelin secretion profiles. Sleep–wake abnormalities are related to the presence of hepatic encephalopathy (HE) and improvement in sleep parameters can be observed when HE is properly managed. A few non-specific treatments for sleep–wake abnormalities have been tried with encouraging results for hydroxyzine and modafinil. However, due to the potential for medication toxicity in these disabled patients, further studies are needed to address the potential role of non-drug therapies in this population (eg, cognitive behavioral therapy, mindfulness, yoga) that have demonstrated usefulness in insomnia disorders.
Introduction
Liver cirrhosis is a common life-threatening hepatic disorder. The main causes of cirrhosis are related to harmful alcohol consumption, viral hepatitis B and C, metabolic disorders, and non-alcoholic fatty liver disease. These causal factors explain the growing prevalence of the disorder which has reached 0.27% of the population in the United States.Citation1 Clinical manifestations of chronic cirrhosis are highly variable and include ascites, jaundice, gastrointestinal hemorrhage, and hepatic encephalopathy (HE). Fatigue and sleep disturbances have also been observed and this can lead to impairments in quality of life (QoL).Citation2,Citation3 Several sleep disturbances have been described in cirrhosis. However, the underlying pathophysiological mechanisms are complex and not yet fully understood.Citation4 The purpose of this review was to describe these different disorders, their impact, and current treatment options.
Clinical manifestations of sleep disturbances in liver cirrhosis
Sleep disturbances in liver cirrhosis are closely related to the presence of HE. HE has a broad spectrum of clinical severity, ranging from subclinical disorders (covert) to overt HE with coma.Citation5 Diagnosis of HE still remains difficult and is primarily based on clinical findings. In recent American and European guidelines, altered sleep rhythm is an essential factor in the diagnosis of HE.Citation6 In a recent study by Singh et al,Citation7 32% of patients with liver cirrhosis exhibited HE. In these patients, sleep disorders have serious implications for daytime functioning and are best described as a panel of sleep–wake abnormalities.Citation4 This was first described in 1954, by Sherlock et al, as a phenomenon of “sleep–wake inversion.”Citation8 The most common abnormalities include insomnia (difficulty falling asleep or maintaining sleep, or unrefreshing sleep), excessive daytime sleepiness (EDS), and sleep–wake inversion (disturbances of circadian rhythmicity).
If most sleep disturbances in cirrhotic patients are attributed to HE,Citation9 sleep disturbances seem to be already present in compensated cirrhosis. Indeed, Bajaj et al have observed EDS and poor quality of sleep in compensated cirrhotics compared to healthy controls.Citation10 Comparison of sleep in cirrhosis with prior HE vs without prior HE has also highlighted a further deterioration of sleep quality, with more non-restorative sleep.Citation11 Etiology of cirrhosis does not influence the occurrence/the clinical picture of sleep disturbances that have been observed both in series of patients affected exclusively or mainly by hepatitis CCitation2,Citation10,Citation11,Citation12 and in series including a majority of alcoholic cirrhosis.Citation13
Other common sleep disorders, such as obstructive sleep apnea syndrome or restless legs syndrome, are also more prevalent in patients with liver cirrhosis and will not be discussed in the present review.Citation14,Citation15
Characteristics and prevalence of sleep disturbances in liver cirrhosis
The reported prevalence of sleep–wake abnormalities in cirrhosis depends upon the diagnostic tools used to assess them. Subjective tools, such as questionnaires and sleep logs, can be used to collect sleep quality and daytime complaints. Objective methods classically applied in the sleep lab, such as polysomnography (PSG) and actigraphy, allow more precise assessment.
It should also be emphasized that correlations between subjective and objective sleep disturbances are not strong. This is due to the fact that patients, especially insomniacs, tend to underestimate their sleep quality.Citation16–Citation18 Therefore, it seems essential to rely on both subjective and objective methods to obtain a global picture of sleep in patients.
Prevalence estimates of sleep disturbances in liver cirrhosis based on questionnaires such as the Pittsburgh Sleep Quality Index (PSQI),Citation3,Citation13,Citation19–Citation24 hospital-specific questionnaires,Citation25 the Basic Nordic Sleep Questionnaire,Citation12 and the Sleep Timing and Sleep Quality Screening questionnaireCitation20 range from 48% to 81%. This is much higher than the prevalence observed in the general population.Citation26 Patient complaints include increased sleep latency (SL), reduced total sleep time (TST), and frequent awakenings.Citation4,Citation25 When compared to healthy subjects,Citation2,Citation13,Citation25,Citation27 the sleep of cirrhotic patients was worse in three out of four studies.
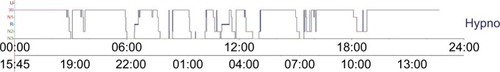
Objective measurements, by actigraphy, have confirmed the altered sleep quality in cirrhotic patients: reduced SL, and frequent awakenings.Citation2,Citation12,Citation25,Citation27–Citation29 PSG has also been performed, confirming the presence of short TST, decreased sleep effi-ciency (SE), frequent awakenings, and lower amounts of slow wave sleep (SWS) and rapid eye movement (REM) sleep in cirrhotic patients.Citation7,Citation28,Citation33 Animal studies in cirrhotic rat models have corroborated these findings.Citation34 Interestingly, when we performed 24h-PSG, we were able to show that the amount of objective sleep over 24 hours is much more important than nighttime sleep (575 vs 471 minutes), since a number of naps are recorded in this population ().Citation28
Figure 1 Typical 24h-hypno of a cirrhotic patient, showing four naps over day and a disturbed sleep with several wake periods after sleep onset.
Abbreviations: N1, sleep stage 1; N2, sleep stage 2; N3, sleep stage 3; W, wake; hypno, hypnogram; U, unknown sleep stage; R, rapid eye movement sleep.
When compared to healthy subjects, deteriorated sleep quality was confirmed by actigraphy in cirrhotic patients in all studies.Citation2,Citation25,Citation27
EDS, which is present in 21%–50% of cirrhotic patients, has also been well documented using the Epworth Sleepiness Score (ESS).Citation2,Citation12,Citation13,Citation21,Citation24 Compared to healthy subjects, cirrhotic patients show a higher degree of EDS.Citation2,Citation13
Objective and subjective sleep–wake measurements are summarized in and .
Table 1 Comparison of sleep–wake parameters between cirrhotic patients and healthy controls
Table 2 Polysomnographic parameters of cirrhotic patients
Chronotypology also seems to be disturbed in cirrhotic patients. Córdoba et alCitation25 showed a marked eveningness chronotype in these patients. In contrast, in comparison with healthy subjects, Montagnese et alCitation13 observed no significant difference. However, this team stressed that sleep quality was deteriorated in evening-type patients.
Impact of sleep disturbances in liver cirrhosis
Sleep disturbances have been shown to negatively impact QoL in cirrhotic patients and have been measured in the majority of studies by the SF-36Citation2,Citation13,Citation21,Citation28 or the Chronic Liver Disease Questionnaire.Citation3,Citation22 For example, QoL in patients with liver cirrhosis is worse than QoL in healthy controlsCitation2,Citation13 for both the Physical Component Summary and the Mental Component Summary. Samanta et al, in a study comparing 100 cirrhotic patients with minimal HE or no HE, showed that minimal HE was associated with poor sleep and EDS, but also that sleep disturbances aggravate neuropsychiatric impairment.Citation21 Sleep disturbances have also been shown to negatively impact psychological distress and depression.Citation35
Pathophysiological mechanisms of sleep disturbances in liver cirrhosis
Sleep disturbances have been associated with the presence of HE and also with disruptions of melatonin metabolism in cirrhotic patients. Some of the features of sleep–wake regulation disturbances may be attributable to melatonin metabolism impairments because melatonin is metabolized by the liver. In patients with cirrhosis, the daytime melatonin level is high,Citation4 the clearance of melatonin is lower at night,Citation36 and melatonin secretion patterns are modified so that the peak of secretion is delayed.Citation36,Citation37 The delayed peak of melatonin secretion is associated with the degree of hepatic failure.Citation29,Citation36 The clinical consequence of these changes is delayed sleep onset.Citation29
Animal studies in rats with portacaval anastomosis (a reliable model of HE) have reported impairment of circadian loco-motor activity and also disturbances in the rhythm of pineal melatonin content.Citation38 A dysfunction of the suprachiasmatic nuclei circadian clock has been also proposed to explain the alteration of melatonin secretion patterns.Citation4
However, EDS does not seem to be related to melatonin metabolism disturbancesCitation36 but rather to the degree of HE.Citation4 Indeed, researchers have shown an association between HE severity and EDS,Citation13,Citation21,Citation22 and the absence of EDS had a 92% negative predictive value for HE-triggered hospitalizations during an 8-month follow-up period in 58 cirrhotics.Citation39
The causal factors associated with deteriorated sleep in patients with liver cirrhosis are still under investigation, and the data are inconsistent. It has been shown, with PSQI, that sleep deterioration is not related to the presence/degree of HE.Citation13 However, another study, which assessed sleep by PSG, reported parallel improvements in sleep quality and HE.Citation28 In an animal model of HE in rats, Felipo et al showed that HE rats had more awakenings during sleep and more naps during active phase than controls,Citation40 supporting the association between sleep disturbances and HE. In another study, high levels of interleukin-6, and not the presence of HE, were associated with poor sleep, measured by PSQI.Citation14 Based on these contradictory observations, further studies are clearly needed.
A recent finding that might explain delayed sleep onset in cirrhotic patients has implicated alterations in thermoregu-lation. Heat loss through vasodilation is essential for sleep onset,Citation41 and it has been demonstrated, in cirrhotic patients compared to healthy controls, that the circadian variation of core body temperature is impaired, such that patients are unable to decrease their distal temperature at the end of the day.Citation42 Similar results have been observed in rats, confirming that alterations in body temperature rhythms are associated with HE.Citation40 The underlying pathophysiologic mechanism proposed by the authors is that this is provoked by the hyperdynamic circulatory syndrome caused by splanchnic and systemic vasodilation.Citation42
Another recent observation focused on glucose fluctuations in cirrhotic patients, highlighting that greater fluctuations were associated with higher PSQI scores.Citation43 Since 70% of cirrhotic patients suffer from glucose intolerance or diabetes,Citation44 this could also partly explain the disturbed sleep patterns in these patients.
Finally, Bajaj et al have also observed, in five cirrhotic men with minimal HE compared to matched controls, that low values of ghrelin in cirrhotic patients were associated with SWS loss on PSG.Citation31
Many lines of research remain to be explored in order to understand these complex pathophysiological mechanisms. A summary of current research in this area is shown in .
Table 3 Possible pathophysiological mechanisms explaining sleep–wake abnormalities in cirrhotic patients
Treatment for sleep disturbances in liver cirrhosis
As sleep disturbances and EDS are mainly related to HE, it has been hypothesized that HE treatment could positively influence these disorders. Other non-specific treatments for sleep disturbances have also been tried. They are detailed here.
Effectiveness of HE treatment on sleep disturbances
Non-absorbable disaccharides
Lactulose and lactitol aim to decrease ammonia absorption from the gut and are effective for improving HE.Citation9,Citation45,Citation46 Treatment improves neurocognition and QoL.Citation47 A recent work from Singh et al, comparison of cirrhotic patients without HE and those with minimal HE who were given lactulose for 3 months, showed that HE treatment led to improvements in EDS (measured by ESS), sleep quality (increases in TST, SE, SL, amount of REM sleep on PSG), and QoL (measured by the SF-36).Citation7
Rifaximin
Rifaximin is a non-absorbable oral antibiotic currently recommended for the treatment of refractory HE and to maintain remission of these episodes.Citation48 Its mechanism of action is complex and is thought to involve a decrease in the load of pathogenic microbial flora. Rifaximin improves neurocognitive function and QoL in HE.Citation31,Citation49 With regard to sleep, we have compared 15 recurrent HE patients before and after a rifaximin course. No changes in subjective nighttime sleep quality and daytime sleepiness were observed. REM sleep amounts were increased on PSG, but no changes were observed for EDS or the need for naps, despite improvements in HE scores.Citation28
Probiotics and l-ornithine l-aspartate
These medications have been proved to improve HE and QoL.Citation46,Citation50 However, no specific studies are currently focused on sleep disturbances.
Liver transplant
One retrospective study has assessed sleep changes before and after liver transplant in 83 patients using questionnaires. Curiously, sleep quality improvement was excellent in patients with alcoholic liver disease but almost nonexistent in hepatitis C patients.Citation51 It could be interesting to assess sleep disturbances and treatment effects according to the causal factors of cirrhosis.
Effectiveness of specific treatments on sleep disturbances
Light therapy
A single study on 12 decompensated cirrhotic patients assessed the effect of morning bright light therapy on sleep quality. Compared to controls, no effect was observed on sleep quality, EDS, or QoL.Citation52
Sedatives
One randomized controlled study using the antihistamine hydroxyzine has shown, after a 10-day course, an improvement in SE.Citation53
Stimulants
Modafinil, which is a usual treatment used to fight EDS in narcolepsy, has been tested in primary biliary cirrhosis in two studies. The medication was effective in 76% of 42 patients in terms of EDS, fatigue, and QoL.Citation54 In the second study, on 21 patients, the effects were excellent on EDS and fatigue after 2 months of treatment, with a good toxicity profile.Citation55
Conclusion
Sleep–wake abnormalities are common in liver cirrhosis and associated with impaired QoL. They should be properly addressed with objective measurements to rule out covert HE and to trigger specific adequate management.
Underlying pathophysiological mechanisms are complex and include disturbed metabolism of melatonin and glucose, alterations of thermoregulation, and altered ghrelin secretion. As sleep–wake abnormalities occur when HE is present, the cornerstone of treatment is based on HE treatment. A few non-specific treatments for sleep–wake abnormalities have been tried, with encouraging results for hydroxyzine and modafinil. However, due to the increased potential for medication toxicity in these disabled patients, further studies are needed to address the potential role of non-drug therapies in this population (eg, cognitive behavioral therapy, mindfulness, yoga) that have demonstrated usefulness in insomnia disorders.
Acknowledgments
The authors acknowledge the contribution of a medical writer, Sandy Field, PhD, to the preparation of this manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
- ScaglioneSKliethermesSCaoGThe Epidemiology of Cirrhosis in the United States: A Population-based StudyJ Clin Gastroenterol201549869069625291348
- HeerenMSojrefFSchuppnerRActive at night, sleepy all day--sleep disturbances in patients with hepatitis C virus infectionJ Hepatol201460473274024308991
- GhabrilMJacksonMGoturRMost Individuals With Advanced Cirrhosis Have Sleep Disturbances, Which Are Associated With Poor Quality of LifeClin Gastroenterol Hepatol201715812711278.e628167158
- MontagneseSDe PittàCDe RuiMSleep-wake abnormalities in patients with cirrhosisHepatology201459270571223744627
- AcharyaCBajajJSCurrent Management of Hepatic EncephalopathyAm J Gastroenterol Epub2018713
- American Association for the Study of Liver Disease; European Association for the Study of the LiverHepatic encephalopathy in chronic liver disease: 2014 practice guideline by the European Association for the Study of the Liver and the American Association for the Study of Liver DiseasesJ Hepatol201461364265925015420
- SinghJSharmaBCPuriVSachdevaSSrivastavaSSleep disturbances in patients of liver cirrhosis with minimal hepatic encephalopathy before and after lactulose therapyMetab Brain Dis201732259560528070704
- SherlockSSummerskillWHWhiteLPPhearEAPortal-systemic encephalopathy; neurological complications of liver diseaseLancet1954267683645445713193045
- BleiATCórdobaJPractice Parameters Committee of the American College of GastroenterologyHepatic EncephalopathyAm J Gastro-enterol200196719681976
- BajajJSThackerLRLeszczyszynDEffects of obstructive sleep apnea on sleep quality, cognition, and driving performance in patients with cirrhosisClin Gastroenterol Hepatol2015132390397.e125158922
- KappusMRLeszczyszynDJMosesLRamanSHeumanDMBajajJSEffect of obstructive sleep apnea on the sleep architecture in cirrhosisJ Clin Sleep Med20139324725123494006
- MostacciBFerlisiMBaldi AntogniniASleep disturbance and daytime sleepiness in patients with cirrhosis: a case control studyNeurol Sci200829423724018810597
- MontagneseSMiddletonBSkeneDJMorganMYNight-time sleep disturbance does not correlate with neuropsychiatric impairment in patients with cirrhosisLiver Int20092991372138219686311
- ChouTCLiangWMWangCBWuTNHangLWObstructive sleep apnea is associated with liver disease: a population-based cohort studySleep Med201516895596026116463
- FrancoRAAshwathnarayanRDeshpandeeAThe high prevalence of restless legs syndrome symptoms in liver disease in an academic-based hepatology practiceJ Clin Sleep Med200841454918350962
- NeuDMairesseOHoffmannGSleep quality perception in the chronic fatigue syndrome: correlations with sleep efficiency, affective symptoms and intensity of fatigueNeuropsychobiology2007561404617986836
- BackhausJJunghannsKBroocksARiemannDHohagenFTest-retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomniaJ Psychosom Res200253373774012217446
- SatoMYamaderaWMatsushimaMItohHNakayamaKClinical efficacy of individual cognitive behavior therapy for psycho-physiological insomnia in 20 outpatientsPsychiatry Clin Neurosci201064218719520132526
- TsaiCFChuCJWangYPIncreased serum interleukin-6, not minimal hepatic encephalopathy, predicts poor sleep quality in nonalcoholic cirrhotic patientsAliment Pharmacol Ther201644883684527518472
- GencdalGGunsarFMeralCESleep disorders in cirrhotics; how can we detect?Liver Int20143481192119724512086
- SamantaJDhimanRKKhatriACorrelation between degree and quality of sleep disturbance and the level of neuropsychiatric impairment in patients with liver cirrhosisMetab Brain Dis201328224925923494591
- LabenzCBaronJSToengesGProspective evaluation of the impact of covert hepatic encephalopathy on quality of life and sleep in cirrhotic patientsAliment Pharmacol Ther201848331332129863286
- De RuiMMiddletonBSticcaASleep and circadian rhythms in hospitalized patients with decompensated cirrhosis: effect of light therapyNeurochem Res201540228429225135598
- MarquesDMTeixeiraHRLopesARSleep Quality Assessment and Daytime Sleepiness of Liver Transplantation CandidatesTransplant Proc20164872356236027742297
- CórdobaJCabreraJLataifLPenevPZeePBleiATHigh prevalence of sleep disturbance in cirrhosisHepatology19982723393459462628
- MorphyHDunnKMLewisMBoardmanHFCroftPREpidemiology of insomnia: a longitudinal study in a UK populationSleep200730327428017425223
- BersagliereARaduazzoIDNardiMInduced hyperammonemia may compromise the ability to generate restful sleep in patients with cirrhosisHepatology201255386987821994139
- BruyneelMSerstéTLibertWImprovement of sleep architecture parameters in cirrhotic patients with recurrent hepatic encephalopathy with the use of rifaximinEur J Gastroenterol Hepatol201729330230827977438
- MontagneseSMiddletonBManiARSkeneDJMorganMYSleep and circadian abnormalities in patients with cirrhosis: features of delayed sleep phase syndrome?Metab Brain Dis200924342743919756996
- LiuCZhouJYangXLvJShiYZengXChanges in sleep architecture and quality in minimal hepatic encephalopathy patients and relationship to psychological dysfunctionInt J Clin Exp Med2015811215412154826885103
- BajajJSSaeianKSchubertCMFrancoRFrancoJHeumanDMDisruption of sleep architecture in minimal hepatic encephalopathy and ghrelin secretionAliment Pharmacol Ther201134110310521631553
- WatanabeACerebral changes in hepatic encephalopathyJ Gastroen-terol Hepatol1998137752760
- TeodoroVVBragagnoloMAJrLucchesiLMPolysomnographic sleep aspects in liver cirrhosis: a case control studyWorld J Gastroen-terol2013192234333438
- LlansolaMCanteroJLHita-YañezEProgressive reduction of sleep time and quality in rats with hepatic encephalopathy caused by portacaval shuntsNeuroscience201220119920822108612
- BianchiGMarchesiniGNicolinoFPsychological status and depression in patients with liver cirrhosisDig Liver Dis200537859360015869912
- MontagneseSMiddletonBManiARSkeneDJMorganMYOn the origin and the consequences of circadian abnormalities in patients with cirrhosisAm J Gastroenterol201010581773178120332771
- SteindlPEFinnBBendokBRothkeSZeePCBleiATDisruption of the diurnal rhythm of plasma melatonin in cirrhosisAnn Intern Med199512342742777611593
- ZeePCMehtaRTurekFWBleiATPortacaval anastomosis disrupts circadian locomotor activity and pineal melatonin rhythms in ratsBrain Res19915601–217221760725
- De RuiMSchiffSAprileDExcessive daytime sleepiness and hepatic encephalopathy: it is worth askingMetab Brain Dis201328224524823180317
- FelipoVPiedrafitaBBariosJARats with minimal hepatic encephalopathy show reduced cGMP-dependent protein kinase activity in hypothalamus correlating with circadian rhythms alterationsChronobiol Int201532796697926203935
- WeissNAttaliVBouzbibCThabutDAltered distal-proximal temperature gradient as a possible explanation for sleep-wake disturbances in cirrhotic patientsLiver Int201737121776177929149489
- GarridoMSaccardoDDe RuiMAbnormalities in the 24-hour rhythm of skin temperature in cirrhosis: Sleep-wake and general clinical implicationsLiver Int201737121833184228732130
- HaraguchiMMiyaakiHIchikawaTGlucose fluctuations reduce quality of sleep and of life in patients with liver cirrhosisHepatol Int201711112513127624504
- KruszynskaYTHomePDMcIntyreNRelationship between insulin sensitivity, insulin secretion and glucose tolerance in cirrhosisHepatol-ogy1991141103111
- WatanabeASakaiTSatoSClinical efficacy of lactulose in cirrhotic patients with and without subclinical hepatic encephalopathyHepatology1997266141014149397979
- MittalVVSharmaBCSharmaPSarinSKA randomized controlled trial comparing lactulose, probiotics, and L-ornithine L-aspartate in treatment of minimal hepatic encephalopathyEur J Gastroenterol Hepatol201123872573221646910
- PrasadSDhimanRKDusejaAChawlaYKSharmaAAgarwalRLactulose improves cognitive functions and health-related quality of life in patients with cirrhosis who have minimal hepatic encephalopathyHepatology200745354955917326150
- BassNMMullenKDSanyalARifaximin treatment in hepatic encephalopathyN Engl J Med2010362121071108120335583
- SidhuSSGoyalOMishraBPSoodAChhinaRSSoniRKRifaximin improves psychometric performance and health-related quality of life in patients with minimal hepatic encephalopathy (the RIME Trial)Am J Gastroenterol2011106230731621157444
- OngJPOehlerGKrüger-JansenCLambert-BaumannJYounossiZMOral L-ornithine-L-aspartate improves health-related quality of life in cirrhotic patients with hepatic encephalopathy: an open-label, prospective, multicentre observational studyClin Drug Investig2011314213220
- BhatMWyseJMMoodieEPrevalence and predictors of sleep disturbance among liver diseases in long-term transplant survivorsCan J Gastroenterol Hepatol201529844044426176212
- De RuiMMiddletonBSticcaASleep and circadian rhythms in hospitalized patients with decompensated cirrhosis: effect of light therapyNeurochem Res201540228429225135598
- SpahrLCoeytauxAGiostraEHadengueAAnnoniJMHistamine H1 blocker hydroxyzine improves sleep in patients with cirrhosis and minimal hepatic encephalopathy: a randomized controlled pilot trialAm J Gastroenterol2007102474475317222324
- Ian GanSde JonghMKaplanMMModafinil in the treatment of debilitating fatigue in primary biliary cirrhosis: a clinical experienceDig Dis Sci200954102242224619082890
- JonesDENewtonJLAn open study of modafinil for the treatment of daytime somnolence and fatigue in primary biliary cirrhosisAliment Pharmacol Ther200725447147617270003
