Abstract
Sleep has been described as being of the brain, by the brain, and for the brain. This fundamental neurobiological behavior is controlled by homeostatic and circadian (24-hour) processes and is vital for normal brain function. This review will outline the normal sleep–wake cycle, the changes that occur during aging, and the specific patterns of sleep disturbance that occur in association with both mental health disorders and neurodegenerative disorders. The role of primary sleep disorders such as insomnia, obstructive sleep apnea, and REM sleep behavior disorder as potential causes or risk factors for particular mental health or neurodegenerative problems will also be discussed.
Normal sleep physiology
Sleep is precisely defined by behavioral and electrophysiological measures. Electrophysiologically, sleep is distinguished from wake by distinct changes in the electroencephalogram (EEG), electrooculography, and muscle activity as measured by electromyography. Based on these measures, sleep has been divided into two states, rapid eye movement (REM) and non-REM (NREM) sleep. There are slow rolling movements on electrooculography during NREM sleep and rapid eye movements during REM sleep. REM sleep is characterized by higher-frequency EEG activity and an almost total loss of skeletal muscle tone seen on the electromyography.Citation1 NREM sleep accounts for 75%–80% of total sleep time, predominates during the early stages of sleep, and is subdivided into three stages: N1 (drowsiness), N2 (light sleep), and N3 (deep sleep).Citation2 The transition from wake to deep sleep through these stages is accompanied by a slowing of the EEG from high-frequency, low-voltage waves (beta waves) to low-frequency, higher-voltage (1–3 Hz) waves (delta waves), also called slow-wave activity, reflecting an increased cortical synchronicity.Citation1 NREM sleep rapidly transitions into REM sleep 60–90 minutes or more after onset. During REM sleep, the EEG shows higher frequency lower amplitude waves in the theta range.Citation1 There is regular transition between NREM and REM sleep in approximately 90–120 minute cycles with NREM sleep dominating during the early part of the night and REM later on. The timing and duration of sleep is controlled by two processes:Citation3 the homeostatic sleep drive (process S), which increases for each hour of wakefulness, and the circadian rhythm (process C), where, naturally, humans sleep during the night and are awake during the day.
Figure 1 Homeostatic sleep propensity (sleep load) increases through the waking day and is dissipated by sleep.
Reproduced from Physiology and Behaviour; 90, Beersma DGM and Gordijn MCM, Circadian Control of the Sleep-Wake Cycle 190–195, Copyright (2007), with permission from Elsevier.Citation221
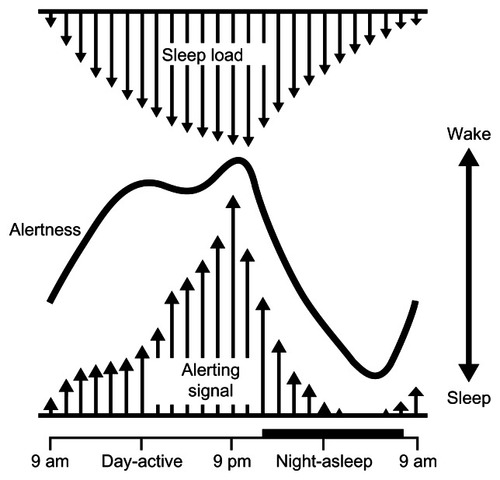
Figure 2 Representative actograms from healthy control (A and E), mildly demented (B and F) and moderately demented (C, G, D and H) subjects recorded first in year 1 (A ± D), and for the same subjects at follow-up in year 2 (E ± H).
From Hatfield CF et al. Disrupted daily activity/rest cycles in relation to daily cortisol rhythms of home-dwelling patients with early Alzheimer’s dementia, Brain, 2004, 27, part 5,1061–74, by permission of Oxford University Press.Citation178
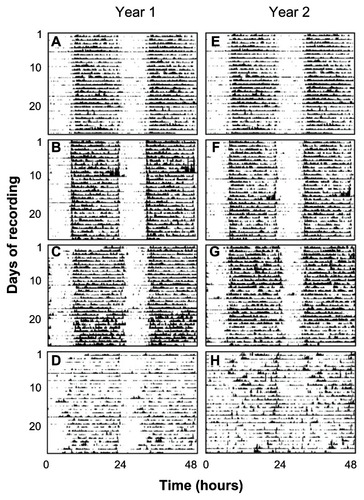
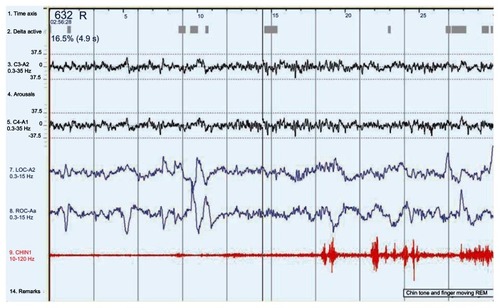
Figure 3 A 30-second epoch from a polysomnograph demonstrating the changes in REM behavior disorder.
Abbreviations: LOC, left outer canthus of the eye; REM, rapid eye movement; ROC, right outer canthus of the eye.
This sleep rhythm is driven by the central circadian pacemaker or master clock located in the suprachiasmatic nucleus (SCN) of the anterior hypothalamus. At the cellular level, the master clock is controlled by an array of clock genesCitation4 that ensure it runs at a period of just over 24 hours.Citation5 The clocks are entrained to the 24-hour cycle by both environmental and endogenous cues called zeitgebers. Light is the major environmental zeitgeber facilitated by photosensitive retinal ganglion cells which have a direct neuronal link from the retina to the SCN via the retinohypothalamic tract.Citation6
The role of sleep in mental health and cognition
Important clues about the role of normal sleep in both memory function and mental health are derived from studies of sleep deprivation (SD) and sleep restriction (SR) in healthy subjects.
In healthy subjects, experimentally induced sleep loss is associated with impairments in a broad range of cognitive functionsCitation7,Citation8 and people with primary sleep disorders such as insomniaCitation9 and sleep apneaCitation10 also suffer from cognitive impairments. Cognitive performance also follows a well characterized circadian rhythm,Citation11 and people suffering from circadian rhythm disorders also suffer from impairments in cognitive performance.Citation12
Both SD, involving complete loss of sleep over several days, and SR, involving partial sleep loss, have been used in experimental studies to examine the effects of sleep loss on cognitive function. During studies of SD and SR, a multitude of cognitive tests have been performed examining a broad range of cognitive domains. Several meta analyses have been performed on the data from studies examining the effects of SD and cognition in healthy subjects.Citation8,Citation13–Citation15 There are significantly fewer studies examining the effects of SR on cognition and no meta analyses performed to date.
To summarize the data from a large number of studies examining different aspects of attention, vigilance, and learning tasks under conditions of SD/SR, SD and SR consistently and significantly impair simple attention as evidenced by slowing of reaction time (RT) and increased lapses during simple vigilance tests. The effects of moderate SR accumulate substantially over time and can be equal to the effects of several days of total SD.
Performance within individuals demonstrates increasing variability over increasing time of SD, which is best explained by wake/sleep state instability and the interaction with circadian rhythm during sleep and wake. There is considerable variability between individuals with respect to their susceptibility to the effects of SD and SR, although the mechanisms are as yet unknown. Executive functions are less susceptible to the effects of SD and SR than simple attention and deficits are found less consistently in studies. Logic and rule-based tasks measuring crystallized abilities are not substantially affected by SD. In contrast, tasks involving more divergent and innovative thinking are significantly impaired by SD.
Sleep appears to be necessary for both memory encoding and consolidation and therefore learning and memory are significantly affected by SD both before and after learning. Emotional memory is also susceptible to the effects of SD, which may lead to relative preservation of negative compared to positive and neutral memories.
Sleep disturbance in mental health problems
Primary sleep disorders as causal factors in mental health disorders
Insomnia is the most common primary sleep disorder and is defined as difficulty falling asleep, staying asleep, or nonrestorative sleep despite adequate opportunity to sleep. Within population-based studies, these symptoms alone affect approximately 30% of adults.Citation16 When one adds associated daytime impairment or distress as a function of the insomnia and symptoms lasting over 1 month that are not secondary to another sleep disorder or mental disorder, then prevalence estimates range from 6%–10%.Citation17–Citation20 The place of insomnia within both the International Classification for Sleep Disorders and the Diagnostic and Statistical Manual of Mental Disorders highlights the interface between disturbed sleep and the psychological distress associated with that sleep disturbance.Citation21,Citation22 Primary insomnia, unrelated to another medical or psychiatric condition, is considered to be part of a psychophysiological hyperarousal process. Age and sex are the best established risk factors, with increased prevalence in women and older adults. However, comorbid medical conditions,Citation23 psychiatric illness,Citation24 and working night shifts or rotating shifts all represent independent risk factors for insomnia. These conditions are thought to be insomnia precipitants in those already predisposed to developing sleep disturbance. The most common comorbidities associated with insomnia are psychiatric disorders, and it is estimated that 40% of all insomnia sufferers have a coexisting psychiatric condition.Citation24,Citation25 Among these psychiatric disorders, depression is most common, and insomnia is a diagnostic symptom for depressive and anxiety disorders.Citation26 Insomnia is increasingly recognized as an independent risk factor for both dysthymia and major depressive disorder. A number of studies, including longitudinal studies in the young and elderlyCitation27–Citation30 and a subsequent meta-analysis,Citation31 have shown that those with insomnia are at least twice as likely to develop depression compared to people with no sleep difficulty over the subsequent 1–3 years of follow-up. Those with insomnia comorbid with depression are more likely to remain depressed despite standard treatments;Citation32 therefore, depression and anxiety may be consequences of as well as risk factors for disrupted sleep. In particular, the hypervigilance and increased arousal associated with both anxiety and insomnia often lead to bidirectionally intertwined disorders that interfere with both sleep onset and sleep maintenance.Citation33 This highlights a potentially underused treatment for depression. There is robust evidence base for cognitive behavioral therapy for insomnia, with many prospective controlled trials showing sustained benefit whether insomnia is primaryCitation34,Citation35 or comorbid with other medicalCitation36,Citation37 or psychiatricCitation38–Citation40 conditions. Importantly, a number of these studies in patients with associated depression and anxiety show an effect regardless of baseline depression levels and moderate treatment effects on both anxiety and depression outcomes as well as insomnia scores.
Obstructive sleep apnea (OSA)
Snoring and associated pauses in breathing (but not snoring alone) was strongly associated with major depression in a large US population study.Citation41 Depression and neurocognitive symptoms have been associated with OSA but the pathophysiology remains poorly understood and some but not all studies identify OSA as independently associated with depression when other variables are controlled for.Citation42 Many of the symptoms of OSA, such as fatigue, low energy, daytime sleepiness, poor concentration, and neurocognitive impairment, overlap with those of depression and may lead to diagnostic difficulty. Improvement of many of these symptoms, including depression measures and quality of life, can be demonstrated with continuous positive airway pressure treatmentCitation43,Citation44 making it important to consider OSA as a potential diagnosis or modifiable factor in those with mental health problems.
Schizophrenia
Disturbed sleep is found in 30%–80% of patients with schizophrenia, depending on the degree of psychotic symptomatology.Citation45,Citation46 Sleep disturbance is inversely correlated with quality of life,Citation47 and a large number of polysomnographic studies have shown increased sleep latency, reduced sleep consolidation, reduced total sleep time, and increased wake time after sleep onset. The sleep disturbances appear to be an important part of the pathophysiology of schizophrenia. These effects have been consistently reported in drug-naïve patients, those who have withdrawn from medication, and those being treated with antipsychotics and other psychotropic medication.Citation48,Citation49
Analysis of EEG and in particular dream sleep in schizophrenia patients has been of interest to psychiatrists as far back as 1955, when Dement first described a reduction in dream recall in patients with schizophrenia and abnormal REM parameters.Citation50 Further studies have shown reduced REM sleep latency, higher REM densities, and a failure of REM rebound after sleep deprivation.Citation51–Citation53 However, there are several contradictory results in these studies, and REM sleep variables are not consistently affected.
A number of sleep parameters, such as the amount of slow-wave sleep (SWS) and REM latency, are significantly correlated with clinical variables, including severity of illness, positive symptoms, negative symptoms, outcome, neurocognitive impairment, and brain structure.Citation52,Citation54–Citation56 Reduced SWS has been reported in patients with schizophrenia in a number of studies;Citation52,Citation57,Citation58 however, there have been contradictory results in patients who were off medication or had never been treated.Citation45 More detailed analyses of the spectral composition of the EEG have revealed a consistent and significant reduction of the higher-amplitude and lower-frequency delta waves, especially in the anterior frontal areas.Citation56 Significant negative correlations have been reported between reduced SWS or high-amplitude, low-frequency delta waves and both negative symptoms and neurocognitive impairment.Citation59 Given the need for SWS in the consolidation of memory, this offers a potential cause or contributory factor for the neurocognitive impairment in schizophrenia.
In schizophrenia patients, memory consolidation has been shown to be impaired compared to controls and to be positively correlated with the amount of SWS and sleep efficiency.Citation60 Manoach et alCitation61 measured the effects of sleep on procedural memory consolidation in schizophrenia patients. Daytime practice improved performance on a finger tapping motor sequence task equally in schizophrenia patients and controls whereas an improvement following overnight sleep was only found in the control group. In a subsequent study, consolidation in schizophrenia patients was dependent on both SWS and stage two sleep in the last quarter of the night.Citation62 Therefore, the sleep abnormalities present in schizophrenia may interfere with normal sleep-dependent memory consolidation and therefore have an influence on cognitive function.
The direct effect of antipsychotic medication is unclear, and the confounding effect of neuroleptics is a major problem with many studies. First-generation or typical antipsychotics are associated with increased total sleep time, increased sleep continuity, and increased REM latency but the reported effects on other sleep stages are variable.Citation63 Treatment withdrawal is followed by a change in sleep structure, mainly in the opposite direction, with a deterioration of sleep quality.Citation64 There are no consistent effects of first-generation antipsychotics on measures of sleep continuity and sleep structure, including the percentage of sleep stages or sleep and REM latency in healthy controls. Therefore, it is possible any effects of these high-potency typical antipsychotics may be indirect with improved sleep secondary to reduced stressful symptomatology.
In contrast, studies of the effects of the atypical antipsychotics (clozapine, olanzapine, quetiapine, risperidone, ziprasidone and paliperidone) in healthy controls and schizophrenia patients show a relatively consistent effect on measures of sleep continuity, with an increased total sleep time and/or sleep efficiency and individually varying effects on other sleep parameters, such as an increase in REM latency observed for olanzapine, quetiapine, and ziprasidone and an increase in SWS documented for olanzapine and ziprasidone.Citation65,Citation66 Additionally, clozapine and olanzapine demonstrate comparable influences on other sleep variables, such as SWS or REM density, in controls and schizophrenic patients.Citation67,Citation68 Therefore, it is possible that the effects of second generation antipsychotics observed on sleep in healthy subjects and schizophrenic patients might involve the action of these drugs on symptomatology, such as depression, cognitive impairment, and negative and positive symptoms.
Circadian rhythm abnormalities have been described in a number of small studies using actigraphy, often without matched controls. Mills et al showed robust circadian rhythms of both core body temperature and urinary electrolytes but a shorter than 24-hour sleep–wake cycle.Citation69 Wirz-Justice et al demonstrated normal rest activity cycles in clozapine-treated patients compared to disordered circadian rhythms in those on typical neuroleptics, and proposed that mechanisms of drug action directly affected circadian rhythm.Citation70 Decreased physical activity during the day was also shown using actigraphy in schizophrenia patients compared to both controls and depressive patients.Citation71 Bromundt et al showed highly variable sleep–wake cycles in 14 patients with more robust sleep–wake cycles correlating with better frontal lobe function, again highlighting a link between impaired sleep and worse cognition.Citation72 The most recent and detailed analysis of circadian rhythm, which included prolonged actigraphy and melatonin profiles in 20 schizophrenia patients compared to 21 unemployed controls, found marked circadian rhythm abnormalities, including both delayed sleep-phase syndrome and free-running, non-24-hour circadian rhythm in 50% of those studied, with no relationship to the neuroleptic used.Citation73 A very recent study demonstrating disrupted sleep–wake rhythms in a mouse model of schizophrenia demonstrated intact retinal inputs to the SCN, but suggested a possible impairment of synaptic connectivity modulating the output from the SCN.Citation74 Mouse models offer the potential for targeting the sleep and circadian rhythm disruption as a therapy for schizophrenia.Citation75
Disrupted sleep and wake in schizophrenia may be intrinsic to the disease itself or occur as a consequence of psychotropic medication, but it may also be due to a primary sleep disorder. This remains a somewhat neglected and potentially treatable aspect of sleep disturbance within this population. There is now increasing recognition of the association between schizophrenia and sleep-related breathing disorders, possibly related, in part, to the weight gain associated with atypical antipsychotics. Metabolic syndrome was found in 38% of a community-based psychiatric cohort on long-term antipsychotics.Citation76 A number of studies have found high rates of sleep apnea in both hospital and community-based populations.Citation77,Citation78 However, not all studies have used control groups, and it has been suggested that sleep apnea is so common in the increasingly obese general population that these rates may not differ to those of BMI matched controls.Citation79 To the authors’ knowledge, there have been no cross-sectional or prospective studies of psychiatric patients with metabolic syndrome to assess the prevalence of OSA. Previous inpatient studies have shown that obese patients with chronic psychiatric morbidity have high rates of OSA.Citation80 Occasional case reports have highlighted the benefits of continuous positive airway-pressure treatment on symptomatology in schizophreniaCitation81–Citation83 but there are no prospective trials to assess long-term benefit or tolerability of continuous positive airway-pressure therapy in comparison to normal controls.
There are some hypotheses that periodic limb movements are not increased in those with schizophrenia,Citation77 but there is very little data regarding the prevalence of other primary sleep disorders, including restless legs and parasomnias.
With regards to insomnia, symptoms are common in those with high degrees of paranoiaCitation84 and, recently, the first structured pilot trial of cognitive behavioral therapy for insomnia was carried out in 15 patients with fixed and treatment-resistant psychosis.Citation85 This showed a promising outcome with a significant improvement not just in sleep outcomes in two-thirds of subjects, but reduced persecutory delusions in 50%. Larger and longer-term trials are needed with control groups to assess the long-term benefits of such behavioral therapies.
Major depressive disorder
Sleep complaints and depression are bidirectionally related, and there has possibly been more general focus on the role of sleep disturbance in depression than in any other psychiatric disorder with sleep disturbance included within the Diagnostic and Statistical Manual of Mental Disorders Fourth Edition (DSM-IV) diagnostic criteria.Citation21 Epidemiologic studies confirm poor sleep quality in 50%–90% of those with diagnosed depression,Citation86,Citation87 and the high prevalence of depression in insomnia patients has already been discussed,Citation24 with insomnia emerging as a clear risk factor for subsequent depression and conferring a worse outcome in those already depressed. Despite methodological differences, sleep disturbance is one of the most important predictors of a subsequent depressive relapse. The discovery that complete SD exerts a potent antidepressant effect therefore seems paradoxical, but much of the original interest in the relationship between sleep and mood stemmed from experiments in the 1970s by Wirz-Justice and Van den Hoofdakker, among others, to show that a single night of complete SD leads to a rapid and dramatic improvement of mood in up to 60% of patients.Citation88 However, the effect is short-lived, with immediate relapse after normal sleep, sometimes after even a brief nap.
The polysomnography changes that occur during depression have been studied from the 1960s, and a number of studies have consistently shown a reduction in sleep efficiency, decreased SWS and disinhibited REM sleep with shortened REM latency, a longer first REM cycle, and increased REM density (the number of eye movements during REM).Citation89,Citation90 Decreased REM latency was initially thought to be a marker for primary rather than secondary depression, but subsequent studies failed to show the same result.Citation91 More detailed analysis of SWS has shown a reduction in delta waves, particularly in the first half of the night and correlated to symptom severity.Citation92 However, to date, no single sleep variable has been of sufficient specificity to be diagnostic for any one psychiatric illness.
One key question has been whether sleep abnormalities only occur acutely during depressive relapse as a “state-dependent” marker, or are present prior to symptom onset and confer a vulnerability to subsequent mood disorder as a “trait” marker. However, this area is complicated by the effects of medication on polysomnography studies. Researchers have shown REM sleep normalizes after depression treatment, but many of the pharmacotherapies and in particular the antidepressants are known to lengthen REM latency and improve sleep continuity in both patients and normal controls.Citation93,Citation94 However, increased sleep efficiency and REM sleep improvement has also been demonstrated after nonpharmacological therapies such as cognitive behavioral therapy.Citation95,Citation96 Conversely, several studies have shown that changes such as shortened REM latencies persist during remission, and longitudinal studies have shown a stable REM latency over time, suggesting at least some trait markers of at least some of the sleep changes.Citation97 In further support of a trait marker is the finding of similar REM sleep changes in subjects with a strong family history of depression but no symptoms at the time of study.Citation98
Although up to 20% of patients complain of hypersomnia, there are few polysomnographic studies of this group, and multiple sleep latency tests and measured total sleep time in this group are often normal.Citation99,Citation100 The same is true of seasonal affective disorder, despite complaints of hypersomnia,Citation101 suggesting that this is not the same sleepiness that can be objectively demonstrated in conditions such as idiopathic hypersomnia. Possible confounding factors include different subtypes of depression within studies and variable tools used to assess daytime sleepiness.
Effect of antidepressant therapies on sleep
Total SD has been mentioned earlier as the only therapy with proven effect within 24 hours; however, rapid relapse is the norm after a single night of recovery sleep, making it of little therapeutic benefit. Both timing and dose of SD have been used to try and obtain therapeutic benefit,with little success to date.Citation102 Selective REM suppression has been used, and one early study showed a treatment response comparable to imipramine,Citation103 but later studies still showed greater benefit with total SD.Citation104 Bright light may add some further benefit in depression, but there is better evidence for its benefit in seasonal affective disorder.Citation105,Citation106 Almost all antidepressant medications modify sleep architecture, making sleep changes in patients in remission hard to interpret. Most tricyclic antidepressants increase total sleep time and decrease wake time after sleep onset, while many selective serotonin reuptake inhibitors have the opposite effect. However, almost all antidepressants prolong REM sleep latency and reduce the amount of REM sleep. Both depressed patients and healthy volunteers have a decreased dream-recall frequency under treatment with antidepressants. This is a consistent effect in tricyclic antidepressants, less consistently documented for selective serotonin reuptake inhibitors/serotonin norepinephrine reuptake inhibitors. Withdrawal from antidepressants may cause nightmares and intensify dreaming;Citation107,Citation108 however, this antidepressant effect is not dependent upon REM sleep elimination and there is no clear evidence that the mechanism of action of antidepressants is dependent on REM sleep suppression.
The role of circadian rhythm abnormalities in the pathophysiology remains unclear. While elevated cortisol is consistently seen in at least 50% of depressed patients at night, levels fall in remission and the effect is not specific to depression.Citation109 Some advocate regular sleep–wake rhythms and avoidance of SD to avoid relapse.Citation110 One recent study showed that a chronotherapeutic regime (bright light and sleep stabilization) significantly improved outcomes over a 9-week period,Citation111 but there is a lack of longitudinal data. It is clearly an area that warrants further study with well-defined diagnostic groups.
Bipolar disorder
Sleep disturbance is a core feature of bipolar disorder (BD), being included in DSM-IVCitation21 diagnostic criteria for major depressive episodes, mania, and hypomania, and it is also commonly reported between mood episodes.Citation112 Disturbances in circadian rhythm are also present,Citation113 and it is now thought that sleep and circadian disturbances, rather than being an artifact of mood episodes, are a core part of the underlying etiology and maintenance of BD.Citation114 This view is supported by the evidence of sleep and circadian disturbances in the initial prodrome of the illness and in the prodrome of relapse. Children at high risk for developing BD have increased sleep disturbances preceding the first episode,Citation115–Citation119 including difficulty getting to sleep, fragmented sleep, and decreased sleep.Citation120,Citation121 Sleep disturbances are reported as an early symptom of bipolar depression (17%–57% of subjects [median 24%]) and are the most robust prodromal symptom of mania reported by 53%–90% (median 77%) of subjects preceding a manic episode.Citation122 Enforced SD can lead to the onset of manic or hypomanic episodes,Citation123 although the literature is inconsistent, probably due to poor characterization of unipolar and bipolar subjects and post hoc follow-up.Citation124 However, in a well-defined group of 206 inpatients with DSM-IIIR- and DSM-IV-defined bipolar depression, switch rates of 4.85% to mania and 5.83% to hypomania were observed following three cycles of total SD.Citation125
Sleep during mania
Polysomnography studies consistently found shortened sleep time, shorter REM latency, increased REM density, and more disturbed sleep.Citation126–Citation129 Manic patients report a decreased need for sleep in 69%–100% of subjects studied.
Sleep and bipolar depression
Sleep disturbances during bipolar depression are common but follow a less consistent pattern than during mania. Hypersomnia is reported in between 23% and 78% of subjects and rates of insomnia vary considerably, with one study of patients. Polysomnography studies comparing patients with bipolar depression to unipolar depression and healthy controls report inconsistent results with greater fragmentation of REM sleep, lower REM latency, no difference in REM latency, increased REM density, fewer minutes in stage 1 sleep, and prolonged SWS latency all reported.Citation126 The decrease in REM latency and higher REM density compared to healthy controls is probably the most consistent finding.Citation130–Citation133
Sleep during euthymia
Polysomnography studies show greater REM density in euthymic BD patients than in controls,Citation134,Citation135 as well as more overnight arousals with increased REM sleep.Citation134,Citation136 Clinically significant sleep disturbance was found in 70% of euthymic BD patients with 55% meeting diagnostic criteria for insomnia by Harvey et al.Citation112 Compared to insomniacs and good sleepers, BD patients had lower sleep efficiency and lower daytime activity levels. Subjectively, BD patients report sleep difficulties that are more severe than in controls but less severe than in the insomnia group, and suffer more daytime sleepiness according to the Epworth Sleepiness Scale.Citation137 Hypersomnia has also been reported in euthymic BD patients with 25% of patients meeting the criteria in one study.Citation138
In summary, studies of euthymic BD patients indicate that there are significant sleep disturbances and variability in sleep, present in the absence of major mood episodes.
Sleep function and course of illness in BD
Given the possibility that sleep disturbances may have a causal role in the relapse and maintenance of bipolar disorder, several studies have examined associations between sleep function and course of illness. In a polysomnography study, REM and stage 2 sleep were not found to correlate with current symptoms, but duration of the first REM period and amount of SWS did correlate positively with manic symptoms and impairment measured on the Work And Social Adjustment Scale 3 months later.Citation139 REM density was positively correlated with depressive symptoms and impairment at 3 months, and the amount of stage 2 sleep was negatively correlated with manic symptoms and impairment. In a study utilizing sleep diaries and semi-structured interviews,Citation135 lower and more variable sleep efficiency and more variable total wake time were associated with more lifetime depressive episodes. Variability in time to fall asleep was positively correlated with concurrent manic symptoms. Hypersomnia has also been found to correlate with future depressive symptoms at 6 months.Citation138 These studies suggest that sleep architecture may have a mechanistic role in disease process.
Circadian rhythms in BD
Circadian rhythm disturbance is reported in BD and may be at least partially responsible for the pattern of disturbed sleep evident in BD patients. Several actigraphy studies have found evidence of disturbed circadian rhythms in BD patients, including phase advances and greater variability in sleep patterns.Citation140,Citation141 A number of circadian genes have been linked to susceptibility to developing BD, including CLOCK, ARNTL 1-2, PER1-3, and CRY1-2.Citation142 Overall, however, findings associating circadian genes to BD are inconsistent. Several reports indicate BD patients are more likely to be evening types,Citation143–Citation146 suggesting a circadian phase delay in BD. However, actigraphy-based studies have found variable results, with advanced sleep phase, delayed sleep phase, and very irregular sleep–wake cycles all found, as well as some groups showing few abnormalities. One consistent finding was reduced total activity compared to controls.Citation141,Citation147 Poor social rhythm regularity predicted the time to the next mood episode.Citation148
Differences in the secretion of melatonin, and sensitivity of melatonin secretion to light, have also been reported in BD. Earlier studiesCitation149–Citation151 suggested a supersensitivity to light in BD patients, with nighttime melatonin levels falling more compared to controls; later, larger studies did not find these changes, but did consistently show lower peak levels of melatonin with and without light stimulus and a less robust circadian rhythm to melatonin secretion.Citation152–Citation154 Recent evidence of lower activity of a key enzyme involved in melatonin synthesis (acetyleserotonin O-methlytransferase) in BD patients compared to controls suggests a general role of melatonin as a susceptibility factor for the development of BD.Citation155 Ramelteon, a selective melatonin MT1/MT2 agonist, may be effective in preventing relapse in euthymic bipolar patients,Citation156 and agomelatine may be effective as an additional therapy for the treatment of bipolar depression.Citation157 Collectively, these studies demonstrate abnormalities in circadian rhythms in patients with BD. Therefore, chronotherapeutics (controlled exposure to environmental stimuli that act on biological rhythms), such as SD, light, and dark therapy may be useful interventions for BD and some small studies have shown this to be the case.Citation113,Citation158,Citation159 Studies have also demonstrated the efficacy of interpersonal social rhythm therapy, which aims to stabilize social rhythms in preventing BD relapse.Citation160,Citation161
Primary sleep disorders in BD
The prevalence of sleep apnea in BD patients has not been systematically evaluated, despite the high frequency of risk factors such as overweight and obesity.Citation162,Citation163 A recent study using a self-assessment tool to establish the risk of OSA found 54.1% of 72 bipolar I disorder patients were at a high risk of OSA. Despite a number of pharmacotherapies for BD being known to exacerbate restless legs, there have been very few studies of the prevalence of restless legs or periodic limb movements.
Neurodegenerative diseases
Aging and sleep
Given the strong association of neurodegenerative conditions with aging, it is important to understand the changes that occur within the sleep–wake cycle and circadian rhythm in an older population. As we age, total sleep time is slightly reduced compared to younger adults, with decreasing amounts of SWS, increased sleep latency, and increased sleep fragmentation during the night.Citation164
Disruptions in the sleep–wake cycle and sleep complaints are commonly found in community-based studies of older people. Over 50% of adults aged over 65 have at least one chronic sleep-related problem.Citation165,Citation166 Older adults also have high rates of primary sleep disorders. Sleep-related breathing disorders, in particular OSA, are estimated at rates of 10%–20%.Citation167–Citation170 Insomnia and restless legs are also increasingly frequent in the people over 65.Citation171,Citation172 Changes in circadian rhythms have also been demonstrated with advancing age, with a decline in the cortisol and melatonin rhythms that entrain day–night activity patterns.Citation173,Citation174 With aging there is reduced amplitude of the circadian rhythm, a phase shift (in particular a phase advance),Citation175 and a loss of the robustness of the rhythm (weakening of the rhythmic pattern). However, within older populations, there is significant circadian rhythm variability between individuals, with some hypothesizing that an age-related disruption to the SCN is responsible.Citation176
Alzheimer’s disease (AD)
Sleep disturbance is one of the most common reasons for institutionalization of demented elderly patients.Citation177 From 25%–50% of the demented elderly suffer from severe nocturnal restlessness, often called “sundowning,” at some stage of the disease. Activity monitoring (actigraphy) in both early and late ADCitation178–Citation180 and in other dementias in patients at home and in institutions confirms profoundly disrupted circadian rhythms in those with moderate and severe dementia.
A recent large trial of bright light therapy and melatonin in institutionalized patients showed modest benefits in measures of daytime function with light therapy alone and together with melatonin;Citation181 however, a further trial of melatonin alone showed no significant improvement in daytime function or night sleep.Citation182
In patients with AD, certain changes can be seen as an exaggeration of the normal aging changes with polysomnography showing increased numbers of awakenings and therefore increased stage 1 sleep. Compared to normal controls there is also reduced SWS.Citation183–Citation186 These changes are consistently reported across moderate to severe AD patients and sleep disturbance worsens with increasing severity of AD. The apolipoprotein status has been associated with progression of sleep–wake disturbance.Citation187 Another feature of the polysomnogram in AD that suggests accelerated aging is a loss of some of the distinctive features of stage 2 sleep with poorly formed sleep spindles that are of shorter duration and less numerous.Citation188 As the disease progresses, NREM sleep stages become progressively more difficult to stage, although REM sleep duration remains relatively stable and loss of REM atonia or significant REM sleep behavior disorder is uncommon.Citation189
Parkinson’s disease (PD)
In his elegant monograph published in 1817, James Parkinson gave his name to a progressive neurological disease characterized by stiffness, slowness, and tremor.Citation190 In the last 10 years, there has been increasing clinical and research interest in the nonmotor symptoms of the disease. Sleep disturbance, depression, and cognitive impairment are all frequently seen in PD and are often considered to be more disabling than the abnormal movement.Citation191,Citation192 Sleep disturbance is near universal in advanced disease and some sleep symptoms can predate all other motor phenomena.Citation193 Particular mention should be made of the association between REM behavior disorder (REMBD) and Parkinsonian syndromes.
Carlos Schenck first described a group of patients with apparently idiopathic REMBD who went on to develop Parkinsonian syndromes including dementia with Lewy bodies (DLB), PD, and multiple system atrophy.Citation194
REMBD affects approximately 0.5% of elderly males, with patients acting out increasingly violent with vivid dreams that often result in injury to themselves or their bed partners.Citation195 It is frequently well treated with long-acting hypnotics such as clonazepam. It is now known that a patient presenting to the sleep clinic with typical REMBD will have a 50% chance of developing a Parkinsonian syndrome within 5 years.Citation196,Citation197 A number of other symptoms can predate the onset of PD such as impaired olfaction, constipation, and mood disturbance but REMBD has the highest specificity as a biomarker raising the possibility of targeting coming neuroprotective agents at patients with this condition. Some patients, however, can develop symptoms many years before the development of any other neurodegenerative problem.Citation198 Conversely, 40% of patients in a movement disorders clinic with PD will have REMBD and 95% of those will have multiple system atrophy.Citation199 Interestingly, this association between REMBD and subsequent neurodegeneration is much more strongly associated with alpha synucleinopathies, including PD, multiple system atrophy, and DLB, but not with tauopathies, such as AD or progressive supranuclear palsy where a far smaller percentage of patients have loss of REM atonia or symptomatic REMBD and this diagnosis has been shown to improve differential diagnosis with these conditions.Citation189,Citation200 There is an increasingly clear association between REMBD and increased risk of the subsequent development of dementia and daytime visual hallucinations.Citation201
Daytime sleepiness was also highlighted in PD patients, particularly with the advent of newer dopamine agonists and the growing reports of “sleep attacks” in association with this group of drugs.Citation202 Patients with PD need to be cautioned about possible daytime sleepiness when they start dopamine agonists. However, daytime sleepiness in PD is often multifactorial with many case control studies highlighting a large number of potential causes including severe REMBD, nocturia, and nighttime pain caused by immobility and tremor.Citation191,Citation203 Increased rates of both central and OSA have been described in those with moderate and advanced PD and there is also an increase in periodic limb movements and restless legs.Citation204 Although some authors have suggested a possible disruption of the circadian rhythm in those with PD, to date, controlled studies are lacking. There is also a relative lack of prospective studies to determine which sleep disorders emerge at different stages of the disease and which therapies best improve night sleep and subsequent daytime function.
A careful sleep history should be taken in all patients with PD and sleep symptoms monitored throughout the disease. PD must be reported to the Driver and Vehicle Licensing Authority in the UK and clinicians must include an assessment of sleepiness. Recent data show that PD patients themselves are poor judges of their safety behind the wheelCitation205 but a recent review highlights the lack of standardized criteria to ensure safety behind the wheel.Citation206
Dementia with Lewy bodies (DLB)
There is less information on nocturnal sleep disturbance in DLB compared to AD, but recent studies suggest an even greater level of nighttime sleep disturbance with an increase in hallucinations, agitation, and apathy but a less clear relationship to disease progression.Citation207 RBD remains a distinguishing feature within the history of a dementing patient that allows for greater sensitivity in diagnosis when present, but there is very limited data on other primary sleep disorders within this group alone.Citation208–Citation210 A recent large cross-sectional study across a number of dementia subtypes highlights RBD as distinguishing DLB and PD dementia from vascular dementia and AD and also the need to look for other sleep disorders, such as sleep apnea, which were frequent, particularly in vascular dementia.Citation211
Frontotemporal dementia
A single study using actigraphy and sleep diaries showed disturbed circadian rhythms in frontotemporal dementia,Citation212 but this was less marked than that seen in AD and did not clearly relate to disease progression. Comparison between the polysomnography studies of those with AD compared to frontotemporal dementia showed greater REM sleep disruption in AD, again suggesting that sleep in frontotemporal dementia may be better preserved.Citation213
Huntington’s disease (HD)
HD is a well-described hereditary, neurodegenerative disease characterized by cognitive decline, behavioral change, and chorea, and patients often have particularly fragmented sleep, with up to 88% reporting sleep problems.Citation214 A wide range of sleep problems, including increased movements during sleep, prolonged sleep latency, and nocturnal waking and daytime sleepiness, have all been reported.Citation215 Unlike a number of other neurodegenerative conditions, patients with HD showed increased density of sleep spindles compared to healthy controls.Citation216 The sleep disturbance correlates with the degree of cognitive impairment and depression.Citation217
Studies looking at the frequency of sleep-disordered breathing have shown variable results. A small pathophysiological study of five patients showed a subtle reduction of hypocretinergic neurons (27%) postmortem but cerebrospinal fluid hypocretin levels were normal in two studies of HD patients.Citation218,Citation219 Polysomnography studies of HD patients have shown reduced REM sleep and delayed REM sleep latency in those with established disease but also in premanifest disease with an increase in periodic limb movements, sleep apnea, and daytime sleepiness.Citation220
Summary
Sleep is vital for normal brain function and there is a complex bidirectional relationship between disturbed sleep and cognitive and mental health disturbance. Much research still needs to be done to characterize the different sleep patterns that occur within different diseases to see whether sleep patterns can be used as specific biomarkers of disease or, possibly more importantly, as trait markers for subsequent illness. It is still unknown whether intervening to normalize sleep clearly improves the outcome of chronic mental health problems or neurodegenerative disease, and there is an urgent need for increasing recognition of the role of disturbed sleep in a disturbed brain.
Disclosure
The authors report no conflicts of interest in this work.
References
- FullerPMGooleyJJSaperCBNeurobiology of the sleep-wake cycle: sleep architecture, circadian regulation, and regulatory feedbackJ Biol Rhythms200621648249317107938
- IberCAncoli-IsraelSChessonAQuanSThe American Academy of Sleep Medicine Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical SpecificationsWestchester, IllinoisAmercian Academy of Sleep Medicine2007
- BorbélyAAA two process model of sleep regulationHum Neurobiol1982131952047185792
- TakahashiJSHongHKKoCHMcDearmonELThe genetics of mammalian circadian order and disorder: implications for physiology and diseaseNat Rev Genet200891076477518802415
- CzeislerCADuffyJFShanahanTLStability, precision, and near-24-hour period of the human circadian pacemakerScience199928454232177218110381883
- FreedmanMSLucasRJSoniBRegulation of mammalian circadian behavior by non-rod, non-cone, ocular photoreceptorsScience1999284541350250410205061
- GoelNRaoHDurmerJSDingesDFNeurocognitive consequences of sleep deprivationSemin Neurol200929432033919742409
- LimJDingesDFA meta-analysis of the impact of short-term sleep deprivation on cognitive variablesPsychol Bull2010136337538920438143
- Fortier-BrochuEBeaulieu-BonneauSIversHMorinCMInsomnia and daytime cognitive performance: a meta-analysisSleep Med Rev2012161839421636297
- BeebeDWGroeszLWellsCNicholsAMcGeeKThe neuropsychological effects of obstructive sleep apnea: a meta-analysis of norm-referenced and case-controlled dataSleep200326329830712749549
- BlatterKCajochenCCircadian rhythms in cognitive performance: methodological constraints, protocols, theoretical underpinningsPhysiol Behav2007902–319620817055007
- ReidKJMcGee-KochLLZeePCCognition in circadian rhythm sleep disordersProg Brain Res201119032021531242
- KoslowskyMBabkoffHMeta-analysis of the relationship between total sleep deprivation and performanceChronobiol Int1992921321361533178
- PilcherJJHuffcuttAIEffects of sleep deprivation on performance: a meta-analysisSleep19961943183268776790
- PhilibertISleep loss and performance in residents and nonphysicians: a meta-analytic examinationSleep200528111392140216335329
- Ancoli-IsraelSRothTCharacteristics of insomnia in the United States: results of the 1991 National Sleep Foundation Survey. ISleep199922Suppl 2S347S35310394606
- OhayonMMPrevalence of DSM-IV diagnostic criteria of insomnia: distinguishing insomnia related to mental disorders from sleep disordersJ Psychiatr Res19973133333469306291
- WeissmanMMGreenwaldSNiño-MurciaGDementWCThe morbidity of insomnia uncomplicated by psychiatric disordersGen Hosp Psychiatry19971942452509327253
- LegerDGuilleminaultCDreyfusJPDelahayeCPaillardMPrevalence of insomnia in a survey of 12,778 adults in FranceJ Sleep Res200091354210733687
- National Institutes of HealthNational Institutes of Health State of the Science Conference statement on Manifestations and Management of Chronic Insomnia in Adults, June 13–15, 2005Sleep20052891049105716268373
- American Psychiatric AssociationDiagnostic and Statistical Manual of Mental Disorders4th edArlington, VAAmerican Psychiatric Association2000
- American Academy of Sleep MedicineInternational Classification of Sleep Disorders2nd edArlington, VAAmerican Academy of Sleep Medicine2005
- KatzDAMcHorneyCAClinical correlates of insomnia in patients with chronic illnessArch Intern Med199815810109911079605781
- FordDEKamerowDBEpidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention?JAMA198926211147914842769898
- McCallWVA psychiatric perspective on insomniaJ Clin Psychiatry200162Suppl 10273211388587
- Ancoli-IsraelSThe impact and prevalence of chronic insomnia and other sleep disturbances associated with chronic illnessAm J Manag Care200612Suppl 8S221S22916686592
- ChangPPFordDEMeadLACooper-PatrickLKlagMJInsomnia in young men and subsequent depression. The Johns Hopkins Precursors StudyAm J Epidemiol199714621051149230772
- JaussentIBouyerJAncelinMLInsomnia and daytime sleepiness are risk factors for depressive symptoms in the elderlySleep20113481103111021804672
- FongSYWingYKLongitudinal follow up of primary insomnia patients in a psychiatric clinicAust N Z J Psychiatry200741761161717558624
- BuysseDJAngstJGammaAAjdacicVEichDRösslerWPrevalence, course, and comorbidity of insomnia and depression in young adultsSleep200831447348018457234
- BaglioniCBattaglieseGFeigeBInsomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studiesJ Affect Disord20111351–3101921300408
- PigeonWRHegelMUnutzerJIs insomnia a perpetuating factor for late-life depression in the IMPACT cohort?Sleep200831448148818457235
- JohnsonEOChilcoatHDBreslauNTrouble sleeping and anxiety/depression in childhoodPsychiatry Res20009429310210808035
- PigeonWRTreatment of adult insomnia with cognitive-behavioral therapyJ Clin Psychol201066111148116020853442
- MitchellMDGehrmanPPerlisMUmscheidCAComparative effectiveness of cognitive behavioral therapy for insomnia: a systematic reviewBMC Fam Pract2012134022631616
- KapellaMCHerdegenJJPerlisMLCognitive behavioral therapy for insomnia comorbid with COPD is feasible with preliminary evidence of positive sleep and fatigue effectsInt J Chrom Obstruct Pulmon Dis20116625635
- RitterbandLMBaileyETThorndikeFPLordHRFarrell-CarnahanLBaumLDInitial evaluation of an Internet intervention to improve the sleep of cancer survivors with insomniaPsychooncology201221769570521538678
- BellevilleGCousineauHLevrierKSt-Pierre-DelormeMÈMeta-analytic review of the impact of cognitive-behavior therapy for insomnia on concomitant anxietyClin Psychol Rev201131463865221482322
- LanceeJvan den BoutJvan StratenASpoormakerVIBaseline depression levels do not affect efficacy of cognitive-behavioral self-help treatment for insomniaDepress Anxiety201330214915623080373
- WagleyJNRybarczykBNayWTDanishSLundHGEffectiveness of abbreviated CBT for insomnia in psychiatric outpatients: sleep and depression outcomesJ Clin Psychol Epub October 26, 2012
- WheatonAGPerryGSChapmanDPCroftJBSleep disordered breathing and depression among US adults: National Health and Nutrition Examination Survey, 2005–2008Sleep201235446146722467983
- HarrisMGlozierNRatnavadivelRGrunsteinRRObstructive sleep apnea and depressionSleep Med Rev200913643744419596599
- GilesTLLassersonTJSmithBHWhiteJWrightJCatesCJContinuous positive airways pressure for obstructive sleep apnoea in adults [review]Cochrane Database Syst Rev20063CD00110616855960
- WellsRDFreedlandKECarneyRMDuntleySPStepanskiEJAdherence, reports of benefits, and depression among patients treated with continuous positive airway pressurePsychosom Med200769544945417556641
- TandonRShipleyJETaylorSElectroencephalographic sleep abnormalities in schizophrenia. Relationship to positive/negative symptoms and prior neuroleptic treatmentArch Gen Psychiatry19924931851941348923
- KeshavanMSTandonRSleep abnormalities in schizophrenia: pathophysiological significancePsychol Med19932348318358134508
- XiangYTWengYZLeungCMTangWKLaiKYUngvariGSPrevalence and correlates of insomnia and its impact on quality of life in Chinese schizophrenia patientsSleep200932110510919189785
- CaldwellDFDominoEFElectroencephalographic and eye movement patterns during sleep in chronic schizophrenic patientsElectroencaphalogr Clin Neurophysiol1967225414420
- GanguliRReynoldsCF3rdKupferDJElectroencephalographic sleep in young, never-medicated schizophrenics. A comparison with delusional and nondelusional depressives and with healthy controlsArch Gen Psychiatry198744136443800582
- DementWDream recall and eye movements during sleep in schizophrenics and normalsJ Nerv Ment Dis1955122326326913295829
- ZarconeVAzumiKDementWGulevichGKraemerHPivikTREM phase deprivation and schizophrenia IIArch Gen Psychiatry1975321114311436173254
- PoulinJDaoustAMForestGStipEGodboutRSleep architecture and its clinical correlates in first episode and neuroleptic-naive patients with schizophreniaSchizophr Res2003621–214715312765755
- ChouinardSPoulinJStipEGodboutRSleep in untreated patients with schizophrenia: a meta-analysisSchizophr Bull200430495796715954201
- MuellerTDierksTFritzeJMaurerKFunctional brain imaging (mapping of EEG) in relation to psychopathologic changes in schizophreniaPsychiatry Res19892934194202608806
- BensonKLSullivanEVLimKOLaurielloJZarconeVPJrPfefferbaumASlow wave sleep and computed tomographic measures of brain morphology in schizophreniaPsychiatry Res1996602–31251348723303
- SekimotoMKatoMWatanabeTKajimuraNTakahashiKCortical regional differences of delta waves during all-night sleep in schizophreniaSchizophr Res20111261–328429021112744
- KeshavanMSMiewaldJHaasGSweeneyJGanguliRReynoldsCFSlow-wave sleep and symptomatology in schizophrenia and related psychotic disordersJ Psychiatr Res19952943033148847657
- SarkarSKatshuMZNizamieSHPraharajSKSlow wave sleep deficits as a trait marker in patients with schizophreniaSchizophr Res20101241–312713320826077
- YangCWinkelmanJWClinical significance of sleep EEG abnormalities in chronic schizophreniaSchizophr Res2006822–325126016377158
- GoderRBoigsMBraunSImpairment of visuospatial memory is associated with decreased slow wave sleep in schizophreniaJ Psychiatr Res200438659159915458855
- ManoachDSCainMSVangelMGKhuranaAGoffDCStickgoldRA failure of sleep-dependent procedural learning in chronic, medicated schizophreniaBiol Psychiatry2004561295195615601605
- ManoachDSThakkarKNStroynowskiEReduced overnight consolidation of procedural learning in chronic medicated schizophrenia is related to specific sleep stagesJ Psychiatr Res201044211212019665729
- CohrsSSleep disturbances in patients with schizophrenia : impact and effect of antipsychoticsCNS drugs2008221193996218840034
- NofzingerEAvan KammenDPGilbertsonMWGurklisJAPetersJLElectroencephalographic sleep in clinically stable schizophrenic patients: two-weeks versus six-weeks neuroleptic-freeBiological Psychiatry19933311–128298358104041
- MillerDDAtypical antipsychotics: sleep, sedation, and efficacyPrim Care Companion J Clin Psychiatry20046Suppl 23716001094
- GoderRFritzerGGottwaldBEffects of olanzapine on slow wave sleep, sleep spindles and sleep-related memory consolidation in schizophreniaPharmacopsychiatry2008413929918484550
- GimenezSRomeroSGichISex differences in sleep after a single oral morning dose of olanzapine in healthy volunteersHum Psychopharmacol201126749850721953682
- ArmitageRColeDSuppesTOzcanMEEffects of clozapine on sleep in bipolar and schizoaffective disordersProg Neuropsychopharmacol Biol Psychiatry20042871065107015610918
- MillsJNMorganRMinorsDSWaterhouseJMThe free-running circadian rhythms of two schizophrenicsChronobiologia197744353360614123
- Wirz-JusticeAHaugHJCajochenCDisturbed circadian rest-activity cycles in schizophrenia patients: an effect of drugs?Schizophr Bull200127349750211596850
- BerleJOHaugeEROedegaardKJHolstenFFasmerOBActigraphic registration of motor activity reveals a more structured behavioural pattern in schizophrenia than in major depressionBMC Res Notes2010314920507606
- BromundtVKosterMGeorgiev-KillASleep-wake cycles and cognitive functioning in schizophreniaBr J Psychiatry2011198426927621263013
- WulffKDijkDJMiddletonBFosterRGJoyceEMSleep and circadian rhythm disruption in schizophreniaBr J Psychiatry2012200430831622194182
- OliverPLSobczykMVMaywoodESDisrupted circadian rhythms in a mouse model of schizophreniaCurr Biol201222431431922264613
- PritchettDWulffKOliverPLEvaluating the links between schizophrenia and sleep and circadian rhythm disruptionJ Neural Transm2012119101061107522569850
- MackinPWatonTWatkinsonHMGallagherPA four-year naturalistic prospective study of cardiometabolic disease in antipsychotic-treated patientsEur Psychiatry2012271505521036552
- Ancoli-IsraelSMartinJJonesDWSleep-disordered breathing and periodic limb movements in sleep in older patients with schizophreniaBiol Psychiatry199945111426143210356624
- AndersonKNWatonTArmstrongDWatkinsonHMMackinPSleep disordered breathing in community psychiatric patientsEuropean J Psychiat20022628695
- TakahashiKIShimizuTSugitaTSaitoYTakahashiYHishikawaYPrevalence of sleep-related respiratory disorders in 101 schizophrenic inpatientsPsychiatry Clin Neurosci19985222292319628167
- WinkelmanJWSchizophrenia, obesity, and obstructive sleep apneaJ Clin Psychiatry200162181111235938
- BoufidisSKosmidisMHBozikasVPDaskalopoulou-VlahoyianniEPitsavasSKaravatosATreatment outcome of obstructive sleep apnea syndrome in a patient with schizophrenia: case reportInt J Psychiatry Med200333330531015089011
- KarantiALandénMTreatment refractory psychosis remitted upon treatment with continuous positive airway pressure: a case reportPsychopharmacol Bull200740111311717285102
- SugishitaKYamasueHKasaiKContinuous positive airway pressure for obstructive sleep apnea improved negative symptoms in a patient with schizophreniaPsychiatry Clin Neurosci201064666521105956
- FreemanDPughKVorontsovaNSouthgateLInsomnia and paranoiaSchizophr Res20091081–328028419097752
- MyersEStartupHFreemanDCognitive behavioural treatment of insomnia in individuals with persistent persecutory delusions: a pilot trialJ Behav Ther Exp Psychiatry201142333033621367359
- CasperRCRedmondDEJrKatzMMSchafferCBDavisJMKoslowSHSomatic symptoms in primary affective disorder. Presence and relationship to the classification of depressionArch Gen Psychiatry19854211109811043863548
- RiemannDBergerMVoderholzerUSleep and depression – results from psychobiological studies: an overviewBiol Psychol2001571–36710311454435
- Wirz-JusticeAVan den HoofdakkerRHSleep deprivation in depression: what do we know, where do we go?Biol Psychiatry199946444545310459393
- KupferDJFosterFGInterval between onset of sleep and rapid-eye-movement sleep as an indicator of depressionLancet1972277796846864115821
- KempenaersCKerkhofsMLinkowskiPMendlewiczJSleep EEG variables in young schizophrenic and depressive patientsBiol Psychiatry19882478338383228569
- ThaseMEKupferDJSpikerDGElectroencephalographic sleep in secondary depression: a revisitBiol Psychiatry19841968058146743718
- PerlisMLGilesDEBuysseDJThaseMETuXKupferDJWhich depressive symptoms are related to which sleep electroencephalographic variables?Biol Psychiatry199742109049139359976
- CartwrightRDRapid eye movement sleep characteristics during and after mood-disturbing eventsArch Gen Psychiatry19834021972016824415
- BuysseDJFrankELoweKKCherryCRKupferDJElectroencephalographic sleep correlates of episode and vulnerability to recurrence in depressionBiol Psychiatry19974144064189034535
- NofzingerEASchwartzRMReynoldsCF3rdAffect intensity and phasic REM sleep in depressed men before and after treatment with cognitive-behavioral therapyJ Consult Clin Psychol199462183918034834
- ThaseMEFasiczkaALBermanSRSimonsADReynoldsCF3rdElectroencephalographic sleep profiles before and after cognitive behavior therapy of depressionArch Gen Psychiatry19985521381449477927
- RushAJErmanMKGilesDEPolysomnographic findings in recently drug-free and clinically remitted depressed patientsArch Gen Psychiatry19864398788843753165
- LauerCJSchreiberWHolsboerFKriegJCIn quest of identifying vulnerability markers for psychiatric disorders by all-night polysomnographyArch Gen Psychiatry19955221451537848050
- NofzingerEAThaseMEReynoldsCF3rdHypersomnia in bipolar depression: a comparison with narcolepsy using the multiple sleep latency testAm J Psychiatry19911489117711811882995
- BilliardMDolencLAldazCOndzeBBessetAHypersomnia associated with mood disorders: a new perspectiveJ Psychosom Res199438Suppl 141477799250
- AndersonJLRosenLNMendelsonWBSleep in fall/winter seasonal affective disorder: effects of light and changing seasonsJ Psychosomatic Res1994384323337
- DallaspeziaSBenedettiFChronobiological therapy for mood disordersExpert Rev Neurother201111796197021721914
- VogelGWThurmondAGibbonsPSloanKWalkerMREM sleep reduction effects on depression syndromesArch Gen Psychiatry1975326765777165796
- WiegandMHLauerCJSchreiberWPatterns of Response to repeated total sleep deprivations in depressionJ Affective Disorders20015642–3257260
- SandorPShapiroCMSleep patterns in depression and anxiety: theory and pharmacological effectsJ Psychosom Res199438Suppl 11251397799244
- PartonenTLönnqvistJSeasonal affective disorderLancet19983529137136913749802288
- SharpleyALCowenPJEffect of pharmacologic treatments on the sleep of depressed patientsBiol Psychiatry199537285987718684
- WilsonSArgyropoulosSAntidepressants and sleep: a qualitative review of the literatureDrugs200565792794715892588
- HerbertJCortisol and depression: three questions for psychiatryPsychol Med201343344946922564216
- LiSXLamSPChanJWYuMWWingYKResidual sleep disturbances in patients remitted from major depressive disorder: a 4-year naturalistic follow-up studySleep20123581153116122851811
- MartinyKRefsgaardELundVA 9-week randomized trial comparing a chronotherapeutic intervention (wake and light therapy) to exercise in major depressive disorder patients treated with duloxetineJ Clin Psychiatry20127391234124223059149
- HarveyAGSchmidtDAScarnàASemlerCNGoodwinGMSleep-related functioning in euthymic patients with bipolar disorder, patients with insomnia, and subjects without sleep problemsAm J Psychiatry20051621505715625201
- MurrayGHarveyACircadian rhythms and sleep in bipolar disorderBipolar Disord201012545947220712747
- HarveyAGSleep and circadian functioning: critical mechanisms in the mood disorders?Annu Rev Clin Psychol2011729731921166537
- StoleruSNottelmannEDBelmontBRonsavilleDSleep problems in children of affectively ill mothersJ Child Psychol Psychiatry19973878318419363582
- ShawJAEgelandJAEndicottJAllenCRHostetterAMA 10-year prospective study of prodromal patterns for bipolar disorder among Amish youthJ Am Acad Child Adolesc Psychiatry200544111104111116239857
- JonesSHTaiSEvershedKKnowlesRBentallREarly detection of bipolar disorder: a pilot familial high-risk study of parents with bipolar disorder and their adolescent childrenBipolar Disord20068436237216879137
- AnkersDJonesSHObjective assessment of circadian activity and sleep patterns in individuals at behavioural risk of hypomaniaJ Clin Psychol200965101071108619670448
- RitterPSMarxCLewtschenkoNThe characteristics of sleep in patients with manifest bipolar disorder, subjects at high risk of developing the disease and healthy controlsJ Neural Transm2012119101173118422903311
- SkjelstadDVMaltUFHolteASymptoms and signs of the initial prodrome of bipolar disorder: a systematic reviewJ Affect Disord20101261–211319883943
- RitterPSMarxCBauerMLeopoldKPfennigAThe role of disturbed sleep in the early recognition of bipolar disorder: a systematic reviewBipolar Disord201113322723721676126
- JacksonACavanaghJScottJA systematic review of manic and depressive prodromesJ Affect Disord200374320921712738039
- WehrTASackDARosenthalNESleep reduction as a final common pathway in the genesis of maniaAm J Psychiatry198714422012043812788
- PlanteDTWinkelmanJWSleep disturbance in bipolar disorder: therapeutic implicationsAm J Pscyhiatry20081657830843
- ColomboCBenedettiFBarbiniBCamporiESmeraldiERate of switch from depression into mania after therapeutic sleep deprivation in bipolar depressionPsychiatry Res199986326727010482346
- HarveyAGSleep and circadian rhythms in bipolar disorder: seeking synchrony, harmony, and regulationAm J Psychiatry2008165782082918519522
- HudsonJILipinskiJFFrankenburgFRGrochocinskiVJKupferDJElectroencephalographic sleep in maniaArch Gen Psychiatry19884532672733341881
- LinkowskiPMendlewiczJSleep electroencephalogram and rhythm disturbances in mood disordersCurr Opin Psychiatr1993613537
- HudsonJILipinskiJFKeckPEJrPolysomnographic characteristics of young manic patients. Comparison with unipolar depressed patients and normal control subjectsArch Gen Psychiatry19924953783831586273
- GillinJCDuncanWPettigrewKDFrankelBLSnyderFSuccessful separation of depressed, normal, and insomniac subjects by EEG sleep dataArch Gen Psychiatry19793618590216331
- JernajczykWLatency of eye movement and other REM sleep parameters in bipolar depressionBiol Psychiatry1986215–64654723697436
- LauerCJWiegandMKriegJCAll-night electroencephalographic sleep and cranial computed tomography in depression. A study of unipolar and bipolar patientsEur Arch Psychiatry Clin Neurosci19922422–359681486107
- ThaseMEHimmelhochJMMallingerAGJarrettDBKupferDJSleep EEG and DST findings in anergic bipolar depressionAm J Psychiatry198914633293332919689
- SitaramNNurnbergerJIJrGershonESGillinJCCholinergic regulation of mood and REM sleep: potential model and marker of vulnerability to affective disorderAm J Psychiatry198213955715767072840
- EidelmanPTalbotLSGruberJHarveyAGSleep, illness course, and concurrent symptoms in inter-episode bipolar disorderJ Behav Ther Exp Psychiatry201041214514920004888
- KnowlesJBCairnsJMacLeanAWThe sleep of remitted bipolar depressives: comparison with sex and age-matched controlsCan J Psychiatry19863142952983708522
- St-AmandJProvencherMDBelangerLMorinCMSleep disturbances in bipolar disorder during remissionJ Affect Disord Epub August 9, 2012
- KaplanKAGruberJEidelmanPTalbotLSHarveyAGHypersomnia in inter-episode bipolar disorder: does it have prognostic significance?J Affect Disord2011132343844421489637
- EidelmanPTalbotLSGruberJHairstonIHarveyAGSleep architecture as correlate and predictor of symptoms and impairment in inter-episode bipolar disorder: taking on the challenge of medication effectsJ Sleep Res201019451652420408930
- MillarAEspieCAScottJThe sleep of remitted bipolar outpatients: a controlled naturalistic study using actigraphyJ Affect Disord2004802–314515315207927
- JonesSHHareDJEvershedKActigraphic assessment of circadian activity and sleep patterns in bipolar disorderBipolar Disord20057217618615762859
- EtainBMilhietVBellivierFLeboyerMGenetics of circadian rhythms and mood spectrum disordersEur Neuropsychopharmacol201121Suppl 4S676S68221835597
- MansourHAWoodJChowdariKVCircadian phase variation in bipolar I disorderChronobiol Int200522357158416076655
- AhnYMChangJJooYHKimSCLeeKYKimYSChronotype distribution in bipolar I disorder and schizophrenia in a Korean sampleBipolar Disord200810227127518271906
- WoodJBirmaherBAxelsonDReplicable differences in preferred circadian phase between bipolar disorder patients and control individualsPsychiatry Res20091662–320120919278733
- GiglioLMMagalhãesPVAndersenMLWalzJCJakobsonLKapczinskiFCircadian preference in bipolar disorderSleep Breath201014215315519774406
- SalvatorePGhidiniSZitaGCircadian activity rhythm abnormalities in ill and recovered bipolar I disorder patientsBipolar Disord200810225626518271904
- ShenGHAlloyLBAbramsonLYSylviaLGSocial rhythm regularity and the onset of affective episodes in bipolar spectrum individualsBipolar Disord200810452052918452448
- LewyAJWehrTAGoodwinFKNewsomeDARosenthalNEManic-depressive patients may be supersensitive to lightLancet1981182163833846110011
- LewyAJNurnbergerJIJrWehrTASupersensitivity to light: possible trait marker for manic-depressive illnessAm J Psychiatry198514267257274003592
- NathanPJBurrowsGDNormanTRMelatonin sensitivity to dim white light in affective disordersNeuropsychopharmacology199921340841310457538
- WhalleyLJPeriniTSheringABennieJMelatonin response to bright light in recovered, drug-free, bipolar patientsPsychiatry Res199138113191658841
- LamRWBerkowitzALBergaSLClarkCMKripkeDFGillinJCMelatonin suppression in bipolar and unipolar mood disordersPsychiatry Res19903321291342243889
- NurnbergerJIJrAdkinsSLahiriDKMelatonin suppression by light in euthymic bipolar and unipolar patientsArch Gen Psychiatry200057657257910839335
- EtainBDumaineABellivierFGenetic and functional abnormalities of the melatonin biosynthesis pathway in patients with bipolar disorderHuman Mol Gen2012211840304037
- NorrisERKarenBCorrellJRA double-blind, randomized, placebo-controlled trial of adjunctive ramelteon for the treatment of insomnia and mood stability in patients with euthymic bipolar disorderJ Affect Disord20131441–214114722963894
- CalabreseJRGuelfiJDPerdrizet-ChevallierCAgomelatine Bipolar Study GroupAgomelatine adjunctive therapy for acute bipolar depression: preliminary open dataBipolar Disord20079662863517845278
- DallaspeziaSBenedettiFChronobiological therapy for mood disordersExpert Rev Neurother201111796197021721914
- WuJCKelsoeJRSchachatCRapid and sustained antidepressant response with sleep deprivation and chronotherapy in bipolar disorderBiol Psychiatry200966329830119358978
- FrankEKupferDJThaseMETwo-year outcomes for interpersonal and social rhythm therapy in individuals with bipolar I disorderArch Gen Psychiatry2005629996100416143731
- MiklowitzDJOttoMWFrankEPsychosocial treatments for bipolar depression: a 1-year randomized trial from the Systematic Treatment Enhancement ProgramArch Gen Psychiatry200764441942617404119
- MainaGSalviVVitalucciAD’AmbrosioVBogettoFPrevalence and correlates of overweight in drug-naïve patients with bipolar disorderJ Affect Disord20081101–214915518234351
- TaylorVMacdonaldKMcKinnonMCJoffeRTMacQueenGMIncreased rates of obesity in first-presentation adults with mood disorders over the course of four-year follow-upJ Affect Disord20081091–212713118221791
- BliwiseDLNormal agingKrygerMHRothTDementWCPrincipals and Practice of Sleep MedicinePhiladelphia, PAElsevier Sanders20052438
- Ancoli-IsraelSSleep and aging: prevalence of disturbed sleep and treatment considerations in older adultsJ Clin Psychiatry200566Suppl 92430 quiz 42–2316336039
- FoleyDJMonjanAABrownSLSimonsickEMWallaceRBBlazerDGSleep complaints among elderly persons: an epidemiologic study of three communitiesSleep19951864254327481413
- CookeJRLiuLNatarajanLThe effect of sleep-disordered breathing on stages of sleep in patients with Alzheimer’s diseaseBehav Sleep Med20064421922717083302
- Ancoli-IsraelSAyalonLSalzmanCSleep in the elderly: normal variations and common sleep disordersHarv Rev Psychiatry200816527928618803103
- CookeJRAncoli-IsraelSLiuLContinuous positive airway pressure deepens sleep in patients with Alzheimer’s disease and obstructive sleep apneaSleep Med200910101101110619699148
- MoraesWPoyaresDSukys-ClaudinoLGuilleminaultCTufikSDonepezil improves obstructive sleep apnea in Alzheimer disease: a double-blind, placebo-controlled studyChest2008133367768318198262
- Ancoli-IsraelSKripkeDFKlauberMRMasonWJFellRKaplanOPeriodic limb movements in sleep in community-dwelling elderlySleep19911464965001798881
- FoleyDAncoli-IsraelSBritzPWalshJSleep disturbances and chronic disease in older adults: results of the 2003 National Sleep Foundation Sleep in America SurveyJ Psychosom Res200456549750215172205
- MazzoccoliGVendemialeGLa ViolaMCircadian variations of cortisol, melatonin and lymphocyte subpopulations in geriatric ageInt J Immunopathol Pharmacol201023128929620378015
- LiebermanHRWurtmanJJTeicherMHCircadian rhythms of activity in healthy young and elderly humansNeurobiol Aging19891032592652664542
- MonkTHBuysseDJBillyBDCircadian type and bed-timing regularity in 654 retired seniors: correlations with subjective sleep measuresSleep201134223523921286245
- SchmidtCPeigneuxPCajochenCAge-related changes in sleep and circadian rhythms: impact on cognitive performance and underlying neuroanatomical networksFront Neurol2012311822855682
- ThomasPChantoin-MerletSHazif-ThomasCComplaints of informal caregivers providing home care for dementia patients: the Pixel studyInt J Geriatr Psychiatry200217111034104712404653
- HatfieldCFHerbertJvan SomerenEJHodgesJRHastingsMHDisrupted daily activity/rest cycles in relation to daily cortisol rhythms of home-dwelling patients with early Alzheimer’s dementiaBrain2004127Pt 51061107414998915
- Van SomerenEJActigraphic monitoring of movement and rest-activity rhythms in aging, Alzheimer’s disease, and Parkinson’s diseaseIEEE Trans Rehabil Eng1997543943989422465
- MostEIAboudanSScheltensPVan SomerenEJDiscrepancy between subjective and objective sleep disturbances in early- and moderate-stage Alzheimer diseaseAm J Geriatr Psychiatry201220646046722531105
- DowlingGABurrRLVan SomerenEJMelatonin and bright-light treatment for rest-activity disruption in institutionalized patients with Alzheimer’s diseaseJ Am Geriatr Soc200856223924618070004
- GehrmanPRConnorDJMartinJLShochatTCorey-BloomJAncoli-IsraelSMelatonin fails to improve sleep or agitation in double-blind randomized placebo-controlled trial of institutionalized patients with Alzheimer diseaseAm J Geriatr Psychiatry200917216616919155748
- BliwiseDLTinklenbergJYesavageJAREM latency in Alzheimer’s diseaseBiol Psychiatry19892533203282914155
- LoewensteinRJWeingartnerHGillinJCKayeWEbertMMendelsonWBDisturbances of sleep and cognitive functioning in patients with dementiaNeuro Aging198234371377
- ReynoldsCF3rdKupferDJTaskaLSHochCHSewitchDEGrochocinskiVJSlow wave sleep in elderly depressed, demented, and healthy subjectsSleep1985821551594012158
- VitielloMVPrinzPNAlzheimer’s disease. Sleep and sleep/wake patternsClin Geriatr Med1989522892992665912
- YesavageJAFriedmanLKraemerHSleep/wake disruption in Alzheimer’s disease: APOE status and longitudinal courseJ Geriatr Psychiatry Neurol2004171202415018693
- RauchsGSchabusMParapaticsSIs there a link between sleep changes and memory in Alzheimer’s disease?Neuroreport200819111159116218596620
- GagnonJFPetitDFantiniMLREM sleep behavior disorder and REM sleep without atonia in probable Alzheimer diseaseSleep200629101321132517068986
- ParkinsonJAn Essay on the Shaking PalsySherwoodNealyJonesLondonWhittingham and Rowland1817
- YongMHFook-ChongSPavanniRLimLLTanEKCase control polysomnographic studies of sleep disorders in Parkinson’s diseasePloS One201167e2251121799880
- KhedrEMEl FetohNAKhalifaHAhmedMAEl BehKMPrevalence of non motor features in a cohort of Parkinson’s disease patientsClin Neurol Neurosurg Epub August 16, 2012
- IranzoASleep-wake changes in the premotor stage of Parkinson diseaseJ Neurol Sci20113101–228328521880334
- BoeveBFREM sleep behavior disorder: Updated review of the core features, the REM sleep behavior disorder-neurodegenerative disease association, evolving concepts, controversies, and future directionsAnn N Y Acad Sci20101184155420146689
- ArnulfIREM sleep behavior disorder: motor manifestations and pathophysiologyMov Disord201227667768922447623
- FuldaSIdiopathic REM sleep behavior disorder as a long-term predictor of neurodegenerative disordersEPMA J20112445145823199180
- NomuraTInoueYKagimuraTNakashimaKClinical significance of REM sleep behavior disorder in Parkinson’s diseaseSleep Med201314213113523218532
- ClaassenDOJosephsKAAhlskogJESilberMHTippmann-PeikertMBoeveBFREM sleep behavior disorder preceding other aspects of synucleinopathies by up to half a centuryNeurology201075649449920668263
- Ferini-StrambiLMarelliSSleep dysfunction in multiple system atrophyCurr Treat Options Neurol201214546447322886854
- NomuraTInoueYTakigawaHNakashimaKComparison of REM sleep behaviour disorder variables between patients with progressive supranuclear palsy and those with Parkinson’s diseaseParkinsonism Relat Disord201218439439622115673
- PostumaRBBertrandJAMontplaisirJRapid eye movement sleep behavior disorder and risk of dementia in Parkinson’s disease: a prospective studyMov Disord201227672072622322798
- ChaudhuriKRPalSBrefel-CourbonC‘Sleep attacks’ or ‘unintended sleep episodes’ occur with dopamine agonists: is this a class effect?Drug Saf200225747348312093305
- FerreiraJJDesboeufKGalitzkyMSleep disruption, daytime somnolence and ‘sleep attacks’ in Parkinson’s disease: a clinical survey in PD patients and age-matched healthy volunteersEur J Neurol200613320921416618334
- ArnulfILeuSOudietteDAbnormal sleep and sleepiness in Parkinson’s diseaseCurr Opin Neurol200821447247718607209
- UcEYRizzoMJohnsonAMDastrupEAndersonSWDawsonJDRoad safety in drivers with Parkinson diseaseNeurology200973242112211920018639
- CrizzleAMClassenSUcEYParkinson disease and driving: An evidence-based reviewNeurology201279202067207423150533
- BliwiseDLMercaldoNDAvidanAYBoeveBFGreerSAKukullWASleep disturbance in dementia with Lewy bodies and Alzheimer’s disease: a multicenter analysisDement Geriatr Cogn Disord201131323924621474933
- FermanTJBoeveBFSmithGEDementia with Lewy bodies may present as dementia and REM sleep behavior disorder without parkinsonism or hallucinationsJ Int Neuropsychol Soc20028790791412405541
- FermanTJBoeveBFSmithGEInclusion of RBD improves the diagnostic classification of dementia with Lewy bodiesNeurology201177987588221849645
- DuggerBNBoeveBFMurrayMERapid eye movement sleep behavior disorder and subtypes in autopsy-confirmed dementia with Lewy bodiesMov Disord2012271727822038951
- GuarnieriBAdorniFMusiccoMPrevalence of sleep disturbances in mild cognitive impairment and dementing disorders: a multicenter Italian clinical cross-sectional study on 431 patientsDement Geriatr Cogn Disord2012331505822415141
- AndersonKNHatfieldCKippsCHastingsMHodgesJRDisrupted sleep and circadian patterns in frontotemporal dementiaEur J Neurol200916331732319170747
- MerrileesJHubbardEMastickJMillerBLDowlingGARest-activity and behavioral disruption in a patient with frontotemporal dementiaNeurocase200915651552619736599
- TaylorNBrambleDSleep disturbance and Huntingdon’s diseaseBr J Psychiatry19971713939373439
- VidenovicALeurgansSFanWJaglinJShannonKMDaytime somnolence and nocturnal sleep disturbances in Huntington diseaseParkinsonism Relat Disord200915647147419041273
- EmserWBrennerMStoberTSchimrigkKChanges in nocturnal sleep in Huntington’s and Parkinson’s diseaseJ Neurol198823531771792966851
- AzizNAAnguelovaGVMarinusJLammersGJRoosRASleep and circadian rhythm alterations correlate with depression and cognitive impairment in Huntington’s diseaseParkinsonism Relat Disord201016534535020236854
- BjörkqvistMPetersénANielsenJCerebrospinal fluid levels of orexin-A are not a clinically useful biomarker for Huntington diseaseClin Genet2006701787916813610
- GausSELinLMignotECSF hypocretin levels are normal in Huntington’s disease patientsSleep200528121607160816408421
- GoodmanAORogersLPilsworthSAsymptomatic sleep abnormalities are a common early feature in patients with Huntington’s diseaseCurr Neurol Neurosci Rep201111221121721103960
- BeersmaDGGordijnMCCircadian control of the sleep-wake cyclePhysiol Behav2007902–319019517055008