Abstract
Background
Postoperative delirium (POD) is a common neurological complication associated with valve replacement. Preoperative sleep disturbance is a risk factor for POD development, and nasal insulin modulates the sleep-wake cycle. This study investigated the beneficial effects of intranasal insulin pretreatment on preoperative sleep quality and reducing POD in patients undergoing valve replacement for rheumatic heart disease.
Patients and Methods
This prospective, single-center, randomized controlled trial (RCT) included 76 adult patients aged 18–65 years undergoing valve surgery with cardiopulmonary bypass who were randomly allocated to receive intranasal insulin or normal saline interventions two days before surgery. POD incidence was on postoperative days 1 (T3), 2 (T4), and 3 (T5). Before the first intervention (T0), 1 d before surgery (T1), and before anesthesia on the day of surgery (T2), sleep quality was assessed and serum cortisol concentrations were measured. At T1 and T2, sleep quality related indicators monitored by sleep monitoring watches from the previous night were recorded.
Results
Compared with the normal saline group, 3 days after surgery, the insulin group showed a significantly reduced incidence of POD; significantly increased deep sleep, REM sleep, deep sleep continuity, and total sleep quality scores at T1 and T2; and significantly reduced serum cortisol concentration, PSQI scale, light sleep ratio, and wakefulness at T1 and T2.
Conclusion
The administration of 20 U of intranasal insulin twice daily, from 2 days preoperatively until 10 minutes preanesthesia on the day of surgery, can improved preoperative sleep quality significantly and reduced POD incidence in patients with rheumatic heart disease undergoing valve replacement.
Clinical Trial Registration
This study was registered with the Chinese Clinical Trial Registry (www.chictr.org.cn, with the unique identifier ChiCTR2100048515; July 9, 2021).
Introduction
Rheumatic heart disease occurs when the mitral, tricuspid, aortic, or pulmonary valves develop lesions due to rheumatic fever that interfere with normal blood flow, resulting in abnormal heart function.Citation1 Currently, valve replacement is the most effective surgical treatment. Preoperative negative emotions such as fear and anxiety, in patients undergoing valve replacement surgery due to uncertainties regarding the operation procedure can seriously affect patient sleep quality.Citation2 Sleep is crucial for maintaining optimal brain function.Citation3 ResearchCitation4 has shown that insufficient sleep can lead to an increase in the release of inflammatory cytokines, thereby activating microglia. When microglia are activated, they release inflammatory cytokines, exacerbating damage to the nervous system. In addition, insufficient sleep can cause excessive excitement of the hypothalamic pituitary adrenal axis, leading to the transfer of a large amount of cortisol produced to the central nervous system, activating the BDNF/TrkB signaling pathway, causing neuronal apoptosis in the hippocampus, and thus causing cognitive impairment.Citation5 In patients with obstructive sleep apnea syndrome, sleep efficiency is often affected, leading to excessive sleepiness, fatigue during the day, and an increased risk of cardiovascular or neurodegenerative diseases.Citation6,Citation7 In recent years, sleep has gradually become a hot topic in clinical research owing to its potential impact on cognitive function. Among these research findings is that preoperative sleep disruption predicts postoperative delirium (POD).Citation8 Ibala et alCitation9 performed sleep polysomnography measurements the night before surgery in hospitalized elderly patients scheduled for elective major cardiac surgery for cardiopulmonary bypass and observed an association between longer sleep duration and POD. Liu et al’sCitation10 research indicates that preoperative sleep disorders make patients undergoing craniotomy more prone to POD. The study by Han et alCitation11 also suggests that preoperative sleep disorders may be an independent predictor of delirium in patients aged 60 years or older undergoing proximal femoral surgery. Therefore, the use of sleep-promoting drugs in the perioperative period may have a positive effect on POD prevention. New research has found that intranasal insulin may be a useful way to normalize the activity of the nocturnal hypothalamic-pituitary-adrenal (HPA) axis and improve sleep-related endocrine regulation.Citation12 We also previously reported that the repeated nasal administration of insulin before surgery can reduce the incidence of POD in patients undergoing radical gastrointestinal tumor resection.Citation13 However, no studies have investigated the combination of intranasal insulin, sleep, and POD. This study explored the effects of preoperative intranasal insulin administration on preoperative sleep quality and POD in patients undergoing valve replacement for rheumatic heart disease and discovered nasal insulin administered significantly improved preoperative sleep quality and reduced POD incidence. This result provides new ideas for preventing POD.
Materials and Methods
Study Design
This prospective, double-blind, randomized controlled study was approved by the Ethics Committee of the General Hospital of Western Theater Command (Ethics Approval No. 2019ky64), conducted in accordance with the principles in the Helsinki Declaration, and registered with the Chinese Clinical Trial Registry at www.chictr.org.cn (unique identifier ChiCTR2100048515, July 9, 2021) before patient enrollment. All participants provided written informed consent. This study was conducted at the General Hospital of the Western Theater Command between August 2021 and January 2022.
Study Participants
Patients aged 18–65 years who underwent heart valve replacement surgery with a procedure that took 2–6 h under cardiopulmonary bypass (CPB) were screened for the trial. Patients with an American Society of Anesthesiologists (ASA) physical status of II or III were included in this randomized study. The Mini-Mental State Examination (MMSE) was used to rule out cognitive dysfunction during the preoperative period. The exclusion criteria were: 1) preoperative rheumatic activities; 2) heparin resistance; 3) abnormal coagulation function; 4) severe liver or kidney or pulmonary damage; 5) difficulty in withdrawing from CPB; 6) preoperative left ventricular ejection fraction <30%; 7) previous hypertension and diabetes; 8) history of insulin allergy; 9) alcohol consumption; 10) preoperative inability to communicate (coma, profound dementia or language impairment, severe visual and hearing impairment); 11) history of neurological or psychiatric diseases; 12) chronic or recent use of melatonin or hypnotics. The withdrawal criteria included 1) insulin use via a non-nasal route during the trial, 2) reoperation within 3 days after the initial operation, 3) unpredicted adverse events (eg, drug allergies, surgical accidents, or anesthesia-related adverse events), and 4) loss to follow-up (patient discharge or death within 3 days postoperatively).
Randomization and Blinding
After admission, patients were selected based on inclusion and exclusion criteria and randomly divided into INS group and IN group in a 1:1 ratio using a random number table method. A random number table was generated by a researcher using IBM SPSS Statistics for Windows, version 26.0 (IBM Corp., Armonk, NY, USA). The second researcher placed random numbers and group numbers in opaque envelopes of the same size and color. Each envelope has a screening number written on the cover, which is the serial number of the subjects who entered the screening. Random allocation is performed by the third researcher, who hands an envelope with patient serial number and hospitalization number information to an anesthesiologist after the patient enters the operating room. All enrolled patients are managed during the perioperative period by this anesthesiologist, who conducts preoperative visits, is responsible for patient grouping information, records relevant basic information, and collects and keeps corresponding records of intraoperative conditions. The generation, concealment, and allocation of randomization were completed by three different researchers who did not participate in the subsequent part of the experiment. The trial was blinded to both the subjects and their families, and other personnel, including surgeons, nurses, follow-up personnel, and data statisticians, were unaware of the patient’s grouping. Postoperative follow-up and related data entry are conducted by trained researchers.
Anesthetic Management
The two groups of patients were prohibited from drinking or eating for 8 h before surgery according to the general anesthesia standards. Peripheral venous access was established and left radial artery and right deep vein punctures were performed under B-wave ultrasound guidance to monitor arterial and central venous pressures and to establish central venous access. Anesthesia was induced by intravenous injection of 0.03 mg/kg midazolam, 0.3 mg/kg etomidate, and 0.5u g/kg sufentanil. After the disappearance of the eyelid reflex, 0.2 mg/kg cisatracurium was administered intravenously for muscle relaxation, and tracheal intubation was performed. The pressure control volume guarantee (PCV-VG) mode was adopted during ventilation, using the following parameters: tidal volume, 6–8 mL/kg; concentration of inhaled oxygen (FIO2), 100%; ratio of inhalation to exhalation=1:2; and partial pressure end-tidal carbon dioxide (PETCO2), 35–45 mmHg maintained by adjusting the tidal volume and respiratory rate. During the surgery, anesthesia was maintained by continuous infusion of 0.5 μg/kg/h dexmedetomidine combined with inhalation of sevoflurane, with the lowest alveolar effective concentration of sevoflurane ≥0.6. In addition, during the surgery, intermittent intravenous injection of 0.08 mg/kg cisatracurium and 0.5 ug/kg sufentanil was used to maintain the bispectral index (BIS) at 40–60. Vascular active drugs such as norepinephrine, dobutamine, milrinone, nitroglycerin, and isoproterenol were used to maintain hemodynamic stability during the operation. During cardiopulmonary bypass (CPB), the temperature was maintained between 28°C and 30°C, the flow between 2.0 and 2.4 L/ (min/m2), and mean arterial pressure (MAP) between 50 and 80 mm Hg. Before discontinuing CPB, the patients were warmed back to 36–37°C. All patients received patient-controlled intravenous analgesia (PCIA) using the following formula: sufentanil (100 ug) + butorphanol tartaric acid injection (5 mg) + ondansetron (16 mg), diluted to 100 mL in normal saline, infused at a rate of 3 mL/h. All patients were transferred to the intensive care unit (ICU) with tracheal catheters after surgery. After arriving at the ICU, remimazolam and remifentanil were used for sedation and analgesia, respectively, until the tracheal catheter was removed according to the tracheal extubation standard.
Interventions
Starting 2 days preoperatively, patients in the NS and INS groups received 0.5 mL of intranasal saline (0.5 mL) or insulin (20 U), respectively, twice daily at 09:00 AM and 19:00 PM using a nasal mucosal atomization device with a syringe (Wuxi Good Life Technology Co., Ltd., Jiangsu, China). The final dose was administered 10 min before induction of anesthesia on the operative day for five administrations.
Data Collection and Measurements
The demographics and medical histories of the patients were recorded, including age, sex, body mass index (BMI), MMSE score, ASA classification, New York Heart Association (NYHA) grade, operation time, CPB time, intraoperative blood transfusion volume, total amount of crystalloids administered during surgery, intraoperative blood loss, urine volume, and numerical rating scale (NRS) score during the first three postoperative days.
Primary Endpoint
The patients completed a preoperative cognitive state test using the MMSE before the first intervention. The primary outcome was the incidence of delirium within the first three postoperative days.
In this study, the same researcher who was trained before the study and was not involved in the clinical care of the patients assessed delirium using the confusion assessment method for the intensive care unit (CAM-ICU) twice daily between 8:00–10:00 and 18:00–20:00. The CAM-ICU is a commonly used international scoring method that can help monitor the development and regression of delirium.Citation14 The first evaluated the patient’s sedation status using the Richmond Agitation Scale (RASS). If the patient was able to awaken (RASS ≥-3 points), we continued the evaluation for delirium using CAM-ICU. If the RASS score was −4 or −5, the delirium assessment was conducted in the next time period. The CAM-ICU evaluation included the following characteristics: a) acute changes or fluctuations in the consciousness state, b) attention deficit, c) changes in the level of consciousness, and d) disordered thinking. Delirium was defined as the presence of a and b combined with either c or d. We also evaluated the occurrence of POD using the Delirium Scale Analysis System (CAM-CR)Citation15 with reference to the diagnostic criteria for delirium in the Diagnostic and Statistical Manual of Mental Disorders (4th Edition) (DSMIV),Citation16 at the same time points as the CAM-ICU evaluation. The CAM-CR evaluation assigned a total possible score of 44 points according to the severity of 11 scoring items, including acute onset, attention disorder, confusion, change in consciousness level, disorientation, memory decline, perception disorder, psychomotor sexual arousal, psychomotor retardation, fluctuation, and change in sleep-wake cycle. Scores of ≤19, 20–22, and ≥22 points indicated no delirium, suspected delirium, and delirium, respectively.
Secondary Endpoints
Biochemical Tests
At three time points before the first intervention (T0), 1 d before surgery (T1), and before the anesthesia on the day of the surgery (T2), 3 mL of venous blood was extracted and centrifuged to obtain serum, which was frozen and stored at −80°C. Serum cortisol concentrations were measured using enzyme-linked immunosorbent assay (ELISA). The reagents were purchased from Shanghai Fanke Biotechnology Co., Ltd., and the measurements were performed according to the manufacturer’s instructions.
Assessment of Sleep Quality
The Pittsburgh Sleep Quality Index (PSQI)Citation17 includes seven scoring items: sleep quality, time to fall asleep, sleep time, sleep efficiency, sleep disorders, daytime dysfunction, and hypnotics. Each item is scored using four grades (0, 1, 2, and 3). The cumulative score for each scoring item is the total score of the PSQI (total score: 0–21), with higher scores indicating worse sleep quality.
The deep sleep ratio, light sleep ratio, rapid eye movement (REM) sleep ratio, number of awakenings, deep sleep continuity score, and total sleep quality score from the previous night were recorded using a sleep monitoring watch (HUAWEI WATCH GT 2e) and were summarized.
Assessment of Postoperative Pain
The NRSCitation18 score for pain was 0, 1–3, 4–6, and 7–1- points for no, mild, moderate, and severe pain, respectively.
Adverse Events
Continuous glucose monitoring system (Shenzhen Silicon-based Sensing Technology Co., Ltd., Shenzhen, China) was used to dynamically track blood glucose levels during the trial. The glucometer recorded the number of hypoglycemia events per day and the average blood glucose values of the patients. Hypoglycemia was defined as a blood glucose value on a continuous dynamic blood glucose monitor of <3.9 mmol/L.Citation19
Sample Size and Statistical Analysis
The sample size calculation was based on the total incidence of delirium within 3 days after surgery and was calculated using PASS 15 software. Research has shown that the incidence of postoperative delirium in cardiac surgery ranges from 4.1% to 54.9%.Citation16 Looking back at the past three years, the incidence of postoperative delirium in our hospital is approximately 46%.Citation16 Pre-trials showed a 15% incidence of POD in patients following repeated 20 U intranasal insulin interventions. Hence, this trial required 31 patients in each group with a power of 80% at a significance of α = 0.05. We recruited 76 patients (38 in each group, assuming a 20% dropout rate).
The collected data were analyzed using IBM SPSS Statistics for Windows, version 26.0 (IBM Corp., Armonk, NY, USA). Outcome analyzes were based on Per-Protocol. Continuous data were first tested using the Shapiro–Wilk test to verify a normal distribution. Continuous data with normal distributions are expressed as means ± standard deviation (SD) and analyzed using the independent t-test. Continuous data with non-normal distributions are expressed as medians (interquartile range) and analyzed using the Mann–Whitney U-test. Categorical variables are expressed as frequencies or percentages and analyzed using Pearson’s chi-square or Fisher’s exact tests. Repeated measures analysis of variance was used to determine the significance of the differences in the changes over time in mean serum cortisol across the groups, with a Dunnett’s t-test applied to each time point, separately for each group. P <0 0.05 was considered statistically significant.
Quality Control
Data accuracy was monitored by the Quality Control Division of the Clinical Research Ethics Committee of the General Hospital of Western Theater Command.
Results
Patient Inclusion
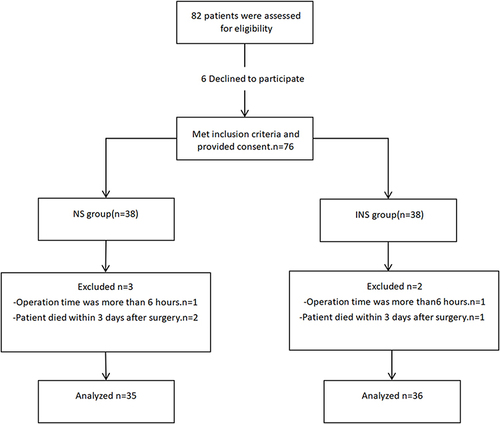
We initially enrolled 76 patients in this study. After considering the inclusion, exclusion, and withdrawal criteria, the final statistical analyses included data from 71 patients (). The two groups had similar demographics and medical histories. Patient age, sex, BMI, MMSE score, ASA classification, NYHA grade, operation time, CPB time, intraoperative blood transfusion volume, total amount of crystalloids administered during surgery, intraoperative blood loss, urine volume, or numerical rating scale (NRS) score during the first 3 postoperative days did not differ between the groups ().
Table 1 Patient Demographics and Clinical Data
POD Prevalence and CAM-CR Scores
Compared to the NS group, the INS group demonstrated a decreased POD prevalence within 3 days postoperatively [51.4% (95% CI, 34.28–68.28) vs 22.2% (95% CI, 10.72–39.58), respectively, P = 0.011]. Compared to the NS group, the CAM-CR scores of the INS group significantly decreased on the first and second postoperative days (P<0.05) ().
Table 2 Incidence of POD and CAM-CR Scores During the First Three Postoperative Day
PSQI Scores and Sleep Monitoring-Related Indicators Before Surgery
Compared with the NS group, the INS group showed significantly reduced PSOI scores, light sleep ratio, and number of awakenings and significantly higher deep sleep ratio, REM sleep ratio, deep sleep continuity score, and total sleep quality score (P<0.05) ().
Table 3 PSQI Scores and Sleep Monitoring-Related Indicators Before Surgery
Serum Cortisol Concentrations at Different Time Points
Compared to the baseline values at T0, the NS and INS groups showed significantly increased and decreased serum cortisol concentrations, respectively, at T1 and T2 (both P<0.05). Compared to the NS group, the serum cortisol concentration in the INS group at T1 and T2 was significantly reduced (P<0.05) ().
Table 4 Serum Cortisol Concentrations at Different Time Points (Mmol/L)
Adverse Events
During the trial, none of the patients experienced hypoglycemic reactions. The average blood glucose levels at T1 and T2 were similar between the two groups (P>0.05) ().
Table 5 Average Blood Glucose Values at Different Time Points (Mmol/L)
Discussion
In this study, the results show that In patients with rheumatic heart disease undergoing valve replacement, nasal insulin administered two days before surgery significantly improved preoperative sleep quality and reduced POD incidence.
POD in patients undergoing cardiac surgery is an acute psychiatric disorder that is a common, serious, and even fatal complication of CPB. POD may lead to patient intolerance of luminal drains and endotracheal intubation;Citation20 increased incidence of complications such as cardiovascular disease, pneumonia, and urinary tract infection; prolonged hospital stay; increased medical costs and mortality;Citation21,Citation22 and high incidence of negative clinical effects, seriously affecting postoperative recovery.Citation16,Citation23 The incidence of delirium after cardiac surgery ranges from 4.1% to 54.9%.Citation16 In this study, the incidence of POD in the NS group was as high as 51.4%; therefore, corresponding preventive measures should be implemented for such patients.
Multiple multifactorial intervention studies have reported that sleep disorders increase the risk of POD.Citation24,Citation25 Preoperative tension in patients often leads to disturbances in the sleep-awakening cycle (with a significant increase in the percentage of awakening time to total sleep time), leading to abnormal hyperactivity of the HPA axis (which plays an important role in maintaining alertness and regulating sleep), excessive cortisol secretion, and effects on cognitive function.Citation26 In addition, sleep disorders or decreased sleep quality may cause an increase in pro-inflammatory cytokine levels; a decrease in the number of central hippocampal neurons; changes in the density of hippocampal dendritic spines; changes in the number, morphology, and function of synapses; and a decrease in white matter volume and quality, leading to impaired memory function and spatial cognition in patients. Surgical trauma, pain, and other factors could further exacerbate the lack of concentration, emotional fluctuations, and cognitive decline caused by the disturbance of the sleep-awakening cycle before surgery, ultimately leading to POD.Citation27–29 In their meta-analysis of 12 studies on the relationship between preoperative sleep disorders and POD, Fadayomi et alCitation30 found that preoperative sleep disorders may be related to POD. The findings of these studies demonstrate the association between disordered sleep and POD risk. However, whether the treatment of patients with preoperative sleep disorders can reduce the morbidity, incidence rate, and medical costs of POD remains to be determined. Another systematic reviewCitation31 showed that some data support health strategies targeting sleep and circadian rhythm regulation as useful methods for preventing POD. Guo et alCitation32 randomly assigned 160 elderly patients with oral cancer who underwent tumor resection surgery divided into two groups. One group received routine treatment, while the other received non-drug interventions. The non-drug intervention improved some of the discomfort caused by sleep disorders and reduced the incidence of POD while reducing cortisol concentrations and increasing melatonin concentrations.
Insulin administered through the nose can cross the blood-brain barrier and reach the central nervous system. Insulin inhibits secretion by the HPA axis by acting on the hypothalamic nucleus and marginal structures (such as the hippocampus) that can express many insulin receptors, ultimately improving sleep cycle disorders.Citation33 Ritze et alCitation34 showed a decrease in serum cortisol concentration after 2 weeks of nasal administration of insulin before nighttime sleep, which was beneficial for memory formation. Feld et alCitation35 studied the effect of nasal insulin on sleep in 16 men and 16 women, in which brain insulin improved memory by inhibiting active forgetting during sleep and reducing interference by encoding new information. In the present study, compared with the saline group, patients in the insulin group had better preoperative sleep quality and lower serum cortisol concentration and POD incidence. These findings suggest that the nasal administration of insulin may inhibit the HPA axis, reduce cortisol release, and improve sleep, thereby reducing the occurrence of POD. This research result can provide strong evidence for perioperative nasal insulin preconditioning to prevent postoperative delirium. The specific mechanism by which intranasal insulin can reduce postoperative delirium by improving sleep needs to be further explored through animal experiments in the future.
However, this study has some limitations: 1) The sample size is relatively small, which may affect the results of some statistical analyses. These results require further validation in large-scale multicenter studies including a wider variety of patients. 2) The follow-up time for POD was relatively short, which can lead to omissions in the evaluation of postoperative delirium patients. 3) The type of valve replacement surgery was not determined. 4) The treatment plan for patients with POD was not tracked. 5) The duration of the reduction of serum cortisol concentration by intranasal insulin has not been followed up, and the exploration time can be extended in the future to more fully elucidate the benefits of intranasal insulin.
Conclusion
Our experimental results indicate that repeated nasal insulin administration before surgery may reduce the incidence of POD within 3 days after surgery, improve preoperative sleep quality, and reduce preoperative serum cortisol concentration in patients with rheumatic heart disease undergoing valve replacement surgery.
Abbreviations
ASA, American Society of Anesthesiologists; BIS, bispectral index; CAM-CR, Delirium Scale Analysis System; CAM-ICU, confusion assessment method for the intensive care unit; CPB, cardiopulmonary bypass; DSMIV, Diagnostic and Statistical Manual of Mental Disorders (4th Edition); HPA, hypothalamic-pituitary-adrenal; FIO2, concentration of inhaled oxygen; ICU, intensive care unit; INS, insulin; MAP, mean arterial pressure; MMSE, Mini-Mental State Examination; NRS, numerical rating scale; NS, normal saline; PCIA, patient-controlled intravenous analgesia; PCV-VG, pressure control volume guarantee; PETCO2, partial pressure end-tidal carbon dioxide, POD, postoperative delirium; PSQI, Pittsburgh Sleep Quality Index; RASS, Richmond Agitation Scale; REM, rapid eye movement; SD, standard deviation; T0, before the first intervention; T1, 1 day before surgery; T2, before anesthesia on the day of surgery; T3, postoperative day 1; T4, postoperative day 2; T5, postoperative day 5.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgments
We thank the medical staff who participated in this study. We would also like to thank the English editor (www.Editage.com).
Data Sharing Statement
The raw data for this study have been uploaded to www.medresman.org.cn and are also available from the corresponding author on reasonable request.
Additional information
Funding
References
- Panduranga VT, Gorantla A, Ahmed A, Sabu J, Mallappallil M, John S. A rare case of congestive heart failure due to isolated aortic valve disease in a middle-aged man secondary to rheumatic fever. J Med Cases. 2023;14(5):149–154. doi:10.14740/jmc4090
- Lin Y, Xu S, Peng Y, Li S, Huang X, Chen L. Preoperative slow-wave sleep is associated with postoperative delirium after heart valve surgery: a prospective pilot study. J Sleep Res. 2023;e13920. doi:10.1111/jsr.13920
- Gao L, Li P, Gaykova N, et al. Circadian rest-activity rhythms, delirium risk, and progression to dementia. Ann Neurol. 2023;93(6):1145–1157. doi:10.1002/ana.26617
- Ni P, Dong H, Zhou Q, et al. Preoperative sleep disturbance exaggerates surgery-induced neuroinflammation and neuronal damage in aged mice. Mediators Inflamm. 2019;2019:8301725. doi:10.1155/2019/8301725
- Gray JD, Milner TA, McEwen BS. Dynamic plasticity: the role of glucocorticoids, brain-derived neurotrophic factor and other trophic factors. Neuroscience. 2013;239:214–227. doi:10.1016/j.neuroscience.2012.08.034
- Maniaci A, Di Luca M, Lechien JR, et al. Lateral pharyngoplasty vs. traditional uvulopalatopharyngoplasty for patients with OSA: systematic review and meta-analysis. Sleep Breath. 2022;26(4):1539–1550. doi:10.1007/s11325-021-02520-y
- Maniaci A, Riela PM, Iannella G, et al. Machine learning identification of obstructive sleep apnea severity through the patient clinical features: a retrospective study. Life. 2023;13(3):702. doi:10.3390/life13030702
- O’Gara BP, Gao L, Marcantonio ER, Subramaniam B. Sleep, pain, and cognition: modifiable targets for optimal perioperative brain health. Anesthesiology. 2021;135(6):1132–1152. doi:10.1097/ALN.0000000000004046
- Ibala R, Mekonnen J, Gitlin J, et al. A polysomnography study examining the association between sleep and postoperative delirium in older hospitalized cardiac surgical patients. J Sleep Res. 2021;30(5):e13322. doi:10.1111/jsr.13322
- Liu Y, Zhang X, Jiang M, et al. Impact of Preoperative Sleep Disturbances on Postoperative Delirium in Patients with Intracranial Tumors: a Prospective, Observational, Cohort Study. Nat Sci Sleep. 2023;15:1093–1105. doi:10.2147/NSS.S432829
- Han F, Liu X, Huang H, Chu H, Feng W. Effect of preoperative sleep disorders on delirium in proximal femoral surgery patients aged 60 or older. BMC Anesthesiol. 2023;23(1):376. doi:10.1186/s12871-023-02331-6
- Thienel M, Wilhelm I, Benedict C, Born J, Hallschmid M. Intranasal insulin decreases circulating cortisol concentrations during early sleep in elderly humans. Neurobiol Aging. 2017;54:170–174. doi:10.1016/j.neurobiolaging.2017.03.006
- Huang Q, Li Q, Qin F, et al. Repeated preoperative intranasal administration of insulin decreases the incidence of postoperative delirium in elderly patients undergoing laparoscopic radical gastrointestinal surgery: a randomized, placebo-controlled, double-blinded clinical study. Am J Geriatr Psychiatry. 2021;29(12):1202–1211. doi:10.1016/j.jagp.2021.02.043
- Durlach M, Khoury M, Donato CL, et al. Delirium and subsyndromal delirium in the intensive care unit: in-hospital outcomes and prognosis at discharge. Med Clin. 2023;S0025-7753(23). doi:10.1016/j.medcli.2023.05.012
- Wang JH, Liu T, Bai Y, et al. The effect of parecoxib sodium on postoperative delirium in elderly patients with Hip arthroplasty. Front Pharmacol. 2023;14:947982. doi:10.3389/fphar.2023.947982
- Chen H, Mo L, Hu H, Ou Y, Luo J. Risk factors of postoperative delirium after cardiac surgery: a meta-analysis. J Cardiothorac Surg. 2021;16(1). doi:10.1186/s13019-021-01496-w
- Mazgelytė E, Valatkevičiūtė A, Songailienė J, Utkus A, Burokienė N, Karčiauskaitė D. Association of hair glucocorticoid levels with sleep quality indicators: a pilot study in apparently healthy perimenopausal and menopausal women. Front Endocrinol. 2023;14:1186014. doi:10.3389/fendo.2023.1186014
- Campbell A, Wang D, Martin K, Côté P. The one-week prevalence of neck pain and low back pain in post-secondary students at two Canadian institutions. Chiropr Man Therap. 2023;31(1):23. doi:10.1186/s12998-023-00496-y
- Frias JP, Deenadayalan S, Erichsen L, et al. Efficacy and safety of co-administered once-weekly cagrilintide 2·4 mg with once-weekly semaglutide 2·4 mg in type 2 diabetes: a multicentre, randomised, double-blind, active-controlled, Phase 2 trial. Lancet. 2023;402(10403):720–730. doi:10.1016/S0140-6736(23)01163-7
- Liu L, Yuan Q, Wang Y, et al. Effects of dexmedetomidine combined with sufentanil on postoperative delirium in young patients after general anesthesia. Med Sci Monit. 2018;24:8925–8932. doi:10.12659/MSM.911366
- Ushio M, Egi M, Fujimoto D, Obata N, Mizobuchi S. Timing, threshold, and duration of intraoperative hypotension in cardiac surgery: their associations with postoperative delirium. J Cardiothorac Vasc Anesth. 2022;36(11):4062–4069. doi:10.1053/j.jvca.2022.06.013
- Hulde N, Zittermann A, Tigges-Limmer K, et al. Preoperative risk factors and early outcomes of delirium in valvular open-heart surgery. Thorac Cardiovasc Surg. 2022;70(7):558–565. doi:10.1055/s-0041-1740984
- Soh S, Shim JK, Song JW, Choi N, Kwak YL. Preoperative transcranial Doppler and cerebral oximetry as predictors of delirium following valvular heart surgery: a case-control study. J Clin Monit Comput. 2020;34(4):715–723. doi:10.1007/s10877-019-00385-x
- Wang H, Zhang L, Luo Q, Li Y, Yan F. Effect of sleep disorder on delirium in post-cardiac surgery patients. Can J Neurol Sci. 2020;47(5):627–633. doi:10.1017/cjn.2020.62
- Evans JL, Nadler JW, Preud’homme XA, et al. Pilot prospective study of post-surgery sleep and EEG predictors of post-operative delirium. Clin Neurophysiol. 2017;128(8):1421–1425. doi:10.1016/j.clinph.2017.05.004
- Buckley TM, Schatzberg AF. On the interactions of the hypothalamic-pituitary-adrenal (HPA) axis and sleep: normal HPA axis activity and circadian rhythm, exemplary sleep disorders. J Clin Endocrinol Metab. 2005;90(5):3106–3114. doi:10.1210/jc.2004-1056
- He E, Dong Y, Jia H, Yu L. Relationship of sleep disturbance and postoperative delirium: a systematic review and meta-analysis. Gland Surg. 2022;11(7):1192–1203. doi:10.21037/gs-22-312
- Li R, Chen N, Wang E, Tang Z. Correlation between preoperative sleep disorders and postoperative delayed neurocognitive recovery in elderly patients. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2021;46(11):1251–1259. English, Chinese.doi:10.11817/j.issn.1672-7347.2021.210015
- Cerejeira J, Batista P, Nogueira V, Vaz-Serra A, Mukaetova-Ladinska EB. The stress response to surgery and postoperative delirium: evidence of hypothalamic-pituitary-adrenal axis hyperresponsiveness and decreased suppression of the GH/IGF-1 Axis. J Geriatr Psychiatry Neurol. 2013;26(3):185–194. doi:10.1177/0891988713495449
- Fadayomi AB, Ibala R, Bilotta F, Westover MB, Akeju O. A systematic review and meta-analysis examining the impact of sleep disturbance on postoperative delirium. Crit Care Med. 2018;46(12):e1204–e1212. doi:10.1097/CCM.0000000000003400
- Lu Y, Li YW, Wang L, et al. Promoting sleep and circadian health may prevent postoperative delirium: a systematic review and meta-analysis of randomized clinical trials. Sleep Med Rev. 2019;48:101207. doi:10.1016/j.smrv.2019.08.001
- Guo Y, Sun L, Li L, et al. Impact of multicomponent, nonpharmacologic interventions on perioperative cortisol and melatonin levels and postoperative delirium in elderly oral cancer patients. Arch Gerontol Geriatr. 2016;62:112–117. doi:10.1016/j.archger.2015.10.009
- Mamik MK, Asahchop EL, Chan WF, et al. Insulin treatment prevents neuroinflammation and neuronal injury with restored neurobehavioral function in models of HIV/AIDS neurodegeneration. J Neurosci. 2016;36(41):10683–10695. doi:10.1523/JNEUROSCI.1287-16.2016
- Ritze Y, Kern W, Ebner EM, Jahn S, Benedict C, Hallschmid M. Metabolic and cognitive outcomes of subchronic once-daily intranasal insulin administration in healthy men. Front Endocrinol. 2018;9:663. doi:10.3389/fendo.2018.00663
- Feld GB, Wilhem I, Benedict C, et al. Central nervous insulin signaling in sleep-associated memory formation and neuroendocrine regulation. Neuropsychopharmacology. 2016;41(6):1540–1550. doi:10.1038/npp.2015.312