Abstract
Background
Gynecological cancer generally refers to malignant tumors in gynecology, commonly including cervical cancer, endometrial cancer, and ovarian cancer. Patients with gynecological cancer often suffer from sleep disorders after clinical treatment. Except for serious sleep disorders, female characteristics, family roles, and feudal beliefs make their self-stigma at a medium to high level, leading to huge pressure. This study aims to identify potential categories of sleep disorders, and analyze the relationship between self-stigma, perceived stress, and sleep disorders.
Methods
A cross-sectional study was conducted in 2021–2022. Two hundred and two patients’ data were collected from ShengJing Hospital Affiliated to China Medical University in Liaoning, Shenyang by using paper questionnaires for face-to-face surveys. The survey tools included the Pittsburgh Sleep Quality Index (PSQI), the Perceived Stress Scale (PSS), and the Social Impact Scale (SIS). Potential profile analysis (LPA), multiple logistic regression analysis, and structural equation modeling (SEM) were performed by Mplus 8.3, SPSS 26.0, and Amos 24.0 statistical tools, respectively.
Results
Three latent patterns of sleep disorders were found: “Good Sleep group (42.5%)”, “Sleep Deficiency group (32.4%)”, and “Sleep Disturbance group (25.1%)”. Patients with high perceived stress were more likely to report a moderate (OR=1.142, 95% CI: 1.061–1.230) or high (OR=1.455, 95% CI: 1.291–1.640) level of sleep disorders. Self-stigma did not have a direct effect on sleep disorders (0.055, P>0.05), but it could have indirect effect on sleep disorders through perceived stress (0.172, P<0.01).
Conclusion
The perceptions of sleep disorders among gynecological cancer patients varies and exhibits individual differences. Gynecological cancer patients who feels alienated or discriminated may cause high pressure. This internal pressure can exacerbate sleep disorders.
Background
According to the 2020 global cancer data released by the World Health Organization, there were 604,000 new cases of cervical cancer, 420,000 cases of endometrial cancer and 310,000 cases of ovarian cancer in women all over the world, ranking among the top 10.Citation1 In China, there were 110,000 new cases of cervical cancer, 80,000 endometrial cancer and 60,000 ovarian cancer in 2020, seriously threatening women’s health.Citation1 The clinical treatment of gynecological malignant tumors is mainly surgical resection plus radiotherapy and chemotherapy. However, the psychological state of patients during radiotherapy and chemotherapy was affected, especially the sleep state.Citation2 Compared with men, women were twice as likely to have sleep disorders or insomnia at some time in their lives, so sleep disorders were considered to have more serious consequences for women.Citation3 Sleep disorders caused by gynecological cancer, such as difficulty falling asleep, sleep interruption, and easy early awakening, are more common and severe compared to other cancers.Citation4,Citation5 Therefore, it was particularly important to solve the sleep problems of gynecological cancer patients, because 30–88% of these patients were affected by sleep disorders, affecting their daily life, course of disease and even prognosis.Citation6 Sleep played an important role in promoting health.Citation7 Women with stable sleep quality had a lower risk of ovarian cancer, while women with insomnia have the opposite.Citation8 Studies have reported that among gynecological cancer patients over a third of women likely experienced insomnia after diagnosis.Citation9 And 75.4% to 80.0% of women had poor sleep quality.Citation10 Insomnia, sleep interruption and drowsiness were the features of sleep disorders, that was, sleep could not meet the needs of the body, causing adverse effects to health outcome.Citation11 The National Comprehensive Cancer Network (NCCN) recommended that cancer survivors regularly screen for sleep disorders, and advocated behavior therapy instead of drug therapy as the first-line treatment of sleep disorders.Citation12 It could be seen that sleep disorders in postoperative gynecological cancer patients might greatly threaten their survival and health, and it should be alleviated from the behavioral and psychological directions.
Self-Stigma and Sleep Disorders
Cancer-related stigma referred to an inner stigma experience that patients felt devalued, alienated, discriminated and avoided due to the cancer diagnosis.Citation13 The theoretical model of social psychology pointed out that stigma was good at affecting the individual’s health state caused by the internalization of stigma, even if the individual has not suffered obvious unfair treatment.Citation14 Stigma helped define the social identity of specific groups. Accepting a stigmatized identity made patients feel ashamed in their interactions with family and medical personnel. From a cross-cultural perspective, although stigma was a common phenomenon and a shared existence experience, the causes and maintenance mechanism of stigma in a specific culture needed to be found in the local moral world.Citation15 In Chinese culture, not only patients, but also their family members, relatives and even the whole relationship network were stigmatized. The concepts of face and shame were of great significance in understanding the stigma as a moral experience.Citation15 Previous studies have shown that some traditional Chinese beliefs believed that cancer was the result of karma or punishment for previous mistakes made by individuals.Citation16,Citation17 It could be seen that patients with physical changes or defects and obvious disease characteristics were more likely to have a sense of shame.Citation16 Especially in Chinese gynecological cancer patients, due to the lack of female characteristics after operation, family roles and feudal thoughts, the stigma of them was at a medium high level.Citation18 Most studies focus on the effect of neighborhood-, weight-, and HIV-related stigma on poor sleep quality.Citation19–21 Few studies indicated that cancer stigma was positively associated with sleep disorders, while negatively associated with sleep quality.Citation22 In the study of gynecologic oncology patients, the influence of stigma on sleep disorders was only verified in breast cancer patients.Citation18 In view of the strong cultural beliefs around cancer, it was necessary to identify and understand the relationship between self-stigma and sleep disorders in Chinese gynecological cancer patients.
Stress and Sleep Disorders
To understand the relationship between self-stigma and sleep disorders, the potential psycho-social mechanisms were essential, and stress might be a potential mediator. Stress was defined as a complex psycho-biological process which was experienced when the individual perceived a threat or danger in the environment.Citation23 According to the cognitive- affective-behavioral model, when patients felt biased while revealing cancer-related thoughts and feelings, they were more likely to assess the situation as highly stressful and threatening.Citation24 One research supported this idea that patients with high self-stigma might experience shame related to the diagnosis, fear of social ostracism, and judgment from others, which increased stress.Citation25 More specifically, during the case of significant stigma, feeling belittled, alienated and discriminated-regulating, limiting or changing their emotions, cognition or behavior - might lead to gynecological cancer patients’ frustration and psychological conflict, producing psychological stress.Citation23 The cognitive model of insomnia suggested that people were prone to sleep problems, which was related to their stress response.Citation26 Evidence from prior research supported the assertion that stress was a strong predictor for poor sleep quality.Citation27 Gynecological cancer patients generally suffered from high perceived stress, leading to the disorders of individual sleep physiological process and the change of sleep structure.Citation28
Theoretical Basis
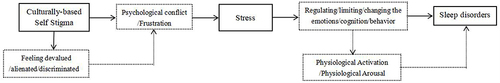
This paper integrated three theoretical models to explain the mechanism of stigma on sleep. A cognitive model of insomnia explained how stressors affected biological arousal systems that regulated sleep/wake patterns.Citation27 A cognitive- affective-behavioral model about stigma outlined the dynamic interaction of thought, feeling and behavior in the context of prominent stigma.Citation29 A stress and coping model explained the role of culturally based psycho-social stressors in sleep suppression in stressful situations.Citation30 In , the integrated model showed that culture-based disease cognition, such as self-stigma, increased stress, and physiological activation caused by stress led to sleep disorders. The comprehensive conceptual model drew on some theories and outlined an intermediary model, that was, stress could also be regarded as a mediating factor – The third variable, mediating the relationship between stigma and sleep. We conceptualize stress as a mediator because ambivalence was more likely to be experienced in situations related to stigma. However, previous studies have mainly focused on the direct effects of stigma and sleep, ignoring potential indirect effects and failing to analyze their mechanisms of action, leading to the conclusion that stigma has no direct impact on sleep.
Latent Profile Analysis
Latent profile analysis (LPA) was a person-focused analytical technique used to identify individuals based on similar features and classify similar individuals into latent discrete populations, which was an ideal method.Citation31,Citation32 LPA can identify different characteristics among individuals through different responses to scale entries, classify samples based on these characteristics, determine the subgroups included in the sample population, and test the relationships between variables in different populations. LPA is widely used in psychology to study the qualitative differences between individual psychology.Citation31,Citation32 Individual psychology not only varies horizontally, but may also have structural differences, so latent profile analysis can be used to diagnose and classify psychological and behavioral problems. Previous studies on sleep disorders often used variable focus analysis techniques, which assumed a uniform distribution of patients’ psychological states. Other studies have shown that this distribution was heterogeneous after trauma (such as cancer diagnosis), indicating that studies using variable focus analysis techniques might not reflect psychological responses related to patient heterogeneity, as it ignored individual differences.Citation33 Therefore, a person-focused analytical technique was used to explore the patterns of sleep disorders in gynecological cancer patients.
Purpose of the Study
Understand the distribution of sleep disorders in gynecological tumor patients.
Identify the profiles of sleep disorders by using LPA as well as explore the sociodemographic, clinical, and psychological characteristics related to these profiles.
Examine the mediating effect of perceived stress between self-stigma and sleep disorders, clarifying the mechanism by which self-stigma affected sleep disorders.
Materials and Methods
Ethics Approval and Informed Consent
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of China Medical University. The procedures of this study were reviewed and approved. Written informed consent for the investigation was obtained from each participant. We protected personal privacy when handling personal data and kept personal records confidential.
Study Design and Sample
A cross-sectional study was conducted during 2021–2022, and a total of 230 patients with gynecological cancer were collected from ShengJing Hospital Affiliated to China Medical University in Liaoning, Shenyang. Inclusion criteria: pathological diagnosis of gynecological cancer at any stage of the disease; all operations were completed and radiotherapy or chemotherapy continues; a stable postoperative condition, with clear consciousness and no serious complications; voluntary participants. The attending physician guided participants to fill out questionnaires through face-to-face surveys, with each questionnaire lasting 10 minutes. Finally, 202 patients were included in the analysis, and the effective recovery rate was 87.8%. Informed consent was obtained from all participants included in the study.
Measurement of General Characteristics of Patients
In our study, marital status was divided into “Married/cohabited” and “Single/separated”. Monthly family income (CNY:1CNY≈0.1367USD) included “≤2000”, “2001–4000”, and “>4000”. Education level included “Middle school or under”, “High or secondary school”, and “Undergraduate or above”. Exercise frequency was classified as “Never”, “1–2times/week”, “≥3times/week”. Residence was divided into “Urban area” and “Rural area”. Regularly drinking coffee was categorized as “No” and “Yes”. Hypertension was divided into “No” and “Yes”. The study divided cancer stage into four types according to the International Federation of Gynecology and Obstetrics (FIGO). In addition, we also investigated age, height, and weight.
Measurement of Sleep Disorders
The Pittsburgh Sleep Quality Index (PSQI) is a self-report measure assessing type and frequency of sleep disorders experienced over the last month with 18 questions form seven component (subjective sleep quality, sleep latency, sleep time, sleep efficiency, sleep disturbance, sleep medication use, daytime dysfunction),Citation34 including “In the past month, overall, do you think your sleep quality is good?”, “Have you been using medication to hypnotize in the past month?”, “Have you had insufficient energy to do things in the past month?” and so on. PSQI uses a 0–3 point Likert scale, with 0=Very good/Never, 1=Good/<1 time/week, 2=Poor/1-2 times/week, 3=Very poor/≥3 times/week. The total scores ranges from 0 to 21, and higher scores represent worse sleep results. Cronbach’s alpha for PSQI is 0.9, and confirmatory factor analysis (CFA) showed that RMSEA (root mean square error of approximation)=0.090, NFI (normal goodness-of-fit index)=0.960, GFI (goodness of fit index)=0.970, CFI (comparative fit index)=0.980, which indicates that PSQI has good reliability and validity.
Measurement of Perceived Stress
The Perceived Stress Scale (PSS) is a global measure of stress.Citation35 In our study, we used the PSS-10 scale with higher internal consistency and construct validity and is thus psycho-metrically superior. The PSS-10 asks respondents about their thoughts and feelings over the last month, including “Feeling restless and agitated due to unexpected events happening”, “Feeling nervous, uneasy, and stressed”, “Unable to handle the troubles in life” and so on. PSS uses a 0–4 point Likert scale, with 0=Never, 1=Occasionally, 2=Sometimes, 3=Often, 4=Always. The total scores range from 0 to 40, with higher scores indicating greater perceived stress. Cronbach’s alpha for the PSS-10 is 0.84, and CFA showed that RMSEA=0.076, NFI=0.941, GFI=0.942, CFI=0.952, which indicates that PSS-10 has good reliability and validity.
Measurement of Self-Stigma
The Social Impact Scale (SIS) was used to measure the self-stigma of patients.Citation36 SIS includes 24 question, including “I feel isolated from healthy individuals”, “I feel that some friends reject me because of my illness”, “Because of my illness, I have encountered some embarrassing things” and so on. SIS uses a 1–4 point Likert scale, with 1= Strongly disagree, 2=Disagree, 3=Agree, 4=Strongly agree. The total scores range from 24 to 96, and the higher the total score of the scale, the stronger the level of stigma feels by patients. Cronbach’s alpha for the SIS is 0.94, and CFA showed that RMSEA=0.039, NFI=0.868, GFI=0.901, CFI=0.969, which indicates that SIS has good reliability and validity.
Statistical Analysis
Firstly, we conducted a series of LPA models with an increasing number of potential classes using Mplus8.3 software (1–5 classes) to determine the optimal class solution. Several fitting indicators were used to evaluate the quality of different models, including the lower Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC), adjusted Bayesian Information Criterion (aBIC), and higher entropy values (>0.8), indicating good model fitting.Citation37 In addition, Lo Mendel Rubin (LMR) and Bootstrap Likelihood Ratio Test (BLRT) were used to compare solutions with class k and solutions with class k-1, and statistically significant p-values showed an improvement in fit due to the inclusion of additional classes.Citation38 Previous studies have shown that BLRT was the most consistent category indicator among all considered models, followed by BIC.Citation39
Secondly, we used SPSS26 software for chi-square tests and analysis of variance (ANOVA) to determine whether all measurement variables had differences between categories. The chi-square test was used to determine demographic and clinical factors that could be used to distinguish categories. ANOVA was used to evaluate the differences between continuous variables. Then we performed multiple logistic regression to determine the factors that predicted different properties of sleep disorders. A two-tailed P<0.05 was considered to be statistically meaningful.
Finally, we used the Structural Equation Modeling (SEM) constructed by Amos 24 software to examine the mediating effect of perceived stress. The bias corrected percentile Bootstrap method was used to verify the significance of mediating effects. If the 95% confidence interval (CI) does not include 0, it indicates that the effect value is statistically significant.Citation40 The indirect effect is significant while the direct effect is also significant, indicating that the variable plays a partial mediating role; If the indirect effect is significant but the direct effect is not significant, it indicates that the variable plays a complete mediating role.Citation40
Results
Sleep Characteristics of Participants
The results showed that the proportion of patients with poor and very poor subjective sleep quality was 47.5%, and only 18.8% of patients never experienced sleep disturbance. The distribution of the seven components of sleep disorders is detailed in .
Table 1 Distribution of the Sleep Disorders
Latent Profile Analysis of Sleep Disorders
The fitting indices of the five LPA models are shown in . The LMR value of the 5-class pattern model is >0.05, indicating that it should be excluded. The AIC, BIC, and aBIC values of the 3-class pattern model are lower than those of the 2-class pattern model, indicating a higher fitting degree of the model. The Entropy value of the 3-class pattern model is higher than that of the 2-class pattern model, indicating that the model classification is more accurate. Therefore, we excluded the 2-class pattern model. Although the 4-class pattern model has the lowest AIC, BIC, and aBIC values, and the highest Entropy value, its latent class contains too few samples. Therefore, based on the actual significance of the model and the number of samples contained in latent class, this study selects the 3-class pattern model as the optimal model after comprehensive consideration.
Table 2 Latent Class Model Fit Comparison
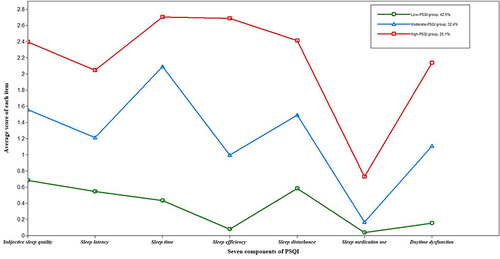
shows these three profiles of sleep disorders. Low-PSQI group (n=85, 42.5%) is characterized by the lowest level of sleep disorders (PSQI score: mean=2.47, SD=0.97), and all components score low, hence it is named the “Good Sleep group”. Moderate-PSQI group (n=66, 32.4%) is characterized by a moderate level of sleep disorders (PSQI score: mean=7.43, SD=2.23), and mainly reflects in high sleep time scores, therefore, we named it the “Sleep Deficiency group”. High-PSQI group (n=51, 25.1%) is characterized by the highest level of sleep disorders (PSQI score: mean=15.09, SD=1.92), and reflects in all components, therefore, we named it the “Sleep Disturbance group”. Therefore, among gynecological cancer patients, there are three categories of sleep disorders, namely “Good Sleep group”, “Sleep Deficiency group”, and “Sleep Disturbance group”.
Multiple Logistic Regression Analysis of the Identified Latent Classes
and show the results of univariate analysis. There are significant differences between the latent classes identified by sleep disorders in terms of exercise frequency, age, perceived stress, and self-stigma (P<0.05). Based on these results, the multiple logistic regression analysis was conducted using the latent classes as dependent variables and the significant factors in the univariate analysis as independent variables.
Table 3 Differences in Demographic and Clinical Characteristics Among the Latent Classes (n, %)
Table 4 Differences in Continuous Variables Among the Latent Classes (Mean±SD)
displays the results of the multiple logistic regression analysis of these factors, and the Nagelkerke R2 is 0.490. It identifies different patterns of sleep disorders, and the reference group is the “Good Sleep group”. Our study find that older patients are more likely to report high level of sleep disorders (OR=1.082, 95% CI=1.026–1.140). Compared to the group whose exercise frequency was ≥3 times/week, patients who never exercised reported a moderate level of sleep disorders (OR=3.824, 95% CI=1.460–10.011) or a high level of sleep disorders (OR=8.028, 95% CI=1.885–34.188), and patients whose exercise frequency was 1–2 times/week reports a high level of sleep disorders (OR=3.824, 95% CI=1.460–10.011). Patients with higher level of perceived stress are more likely to report a moderate level of sleep disorders (OR=1.142, 95% CI=1.061–1.230) or a high level of sleep disorders (OR=4.135, 95% CI=1.121–15.255).
Table 5 Factors in Differentiating Distinct PSQI Groups
Mediation Effect Test
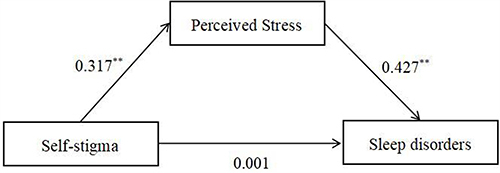
In the SEM, we used age and exercise frequency as control variables. shows the effect values between variables. The effect of self-stigma on perceived stress is 0.317 (P<0.05), the effect of perceived stress on sleep disorders is 0.427 (P<0.05), but the effect of self-stigma on sleep disorders is 0.001 (P>0.05).
displays the mediating effect. We find that the indirect effects of self-stigma on sleep disorders is statistically meaningful (0.172, 95% CI: 0.101–0.172), but the direct effect is not statistically meaningful (0.055, 95% CI:-0.054–0.055), which means that perceived stress plays a complete mediating role between self-stigma and sleep disorders. This means that self-stigma first affects perceived stress, and then perceived stress affects sleep disorders, clarifying the mechanism by which self-stigma affected sleep disorders.
Table 6 The Mediating Effect Test of Perceived Stress
Discussion
This study is one of the few to understand the distribution of sleep disorders and to use LPA to identify specific patterns of sleep disorders in gynecological cancer patients. It is also the first study to investigate the mechanism of stigma on sleep disorders among gynecological cancer patients.
The basic situation of sleep disorders in gynecological tumor patients
The results show that sleep disorders are common among gynecological cancer patients in China. Previous studies have estimated 24.3% to 80.0% of women with gynecological cancer had poor sleep quality.Citation10,Citation41 Our study shows that 47.5% report that the subjective sleep quality is poor/very bad, which is at a moderate level. 17.9% of patients in our study report using prescription or over-The-counter sleeping medication at least once in the past month, lower than estimated in other studies of gynecologic cancer patients (36.7%).Citation17 Of those, 5.5% of patients regularly take sleeping medication, a lower percentage than in previous studies of the same population (13%).Citation9 Specifically, in the past month, 34.1% of patients report a lack of energy, a lack of awareness, an inability to maintain passion, etc., at least once during the day. Finally, overall, 57.5% of patients have moderate and high sleep disturbances. Although it is lower than previous studies of the same population (58–80%),Citation41,Citation42 more than half of the population still suffer from sleep disorders, which is also a serious phenomenon.
Profiles of Sleep Disorders and Associated Factors
The results show there are three profiles of sleep disorders (Good Sleep group, Sleep Deficiency group, and Sleep Disturbance group) among gynecological cancer patients, which is different from previous studies.Citation42 This also precisely indicates that patients have different feelings of sleep disorders and exhibit individual differences. Our research shows that as age increases, the risk of sleep disorders increases, consistent with previous studies.Citation43 The secretion of melatonin gradually decreases with age, leading to a decrease in sleep quality and an increasing probability of developing sleep disorders.Citation44 Similarly, the decline in emotional and cognitive functions in the elderly population also leads to sleep disorders.Citation45 Our study also shows that patients who exercised regularly are less likely to exhibit sleep disorders. Exercise has long been proven to effectively improve sleep quality.Citation46 Exercise increases the body’s oxygen consumption and affects the secretion of metabolic products such as inorganic phosphates, regulating individual’s sleep quality.Citation47 Exercise is beneficial for the structure and function of the brain, especially in the elderly, and the improvement of sleep quality through exercise is the foundation for improving cognitive function.Citation44,Citation48 Our research suggests that perceived stress is a risk factor for sleep disorders, which has been proven in previous studies.Citation49 Long-term stress level is associated with hyperactivity of the hypothalamic-pituitary-adrenal pathway, shortened sleep time, and reduced deep sleep, leading to poor sleep quality, impaired memory, and poor emotional regulation, which in turn lead to more stress.Citation50 Therefore, the greater the stress, the more likely it is to experience sleep disorders.
The Mediating Effect of Perceived Stress Between Self-Stigma and Sleep Disorders
Our results show that the effect of self-stigma on sleep disorders is 0.001 (P>0.05), and there is no correlation between the two, suggesting that self-stigma does not have a significant direct effect on decreased sleep disorders. The effect of self-stigma on perceived stress is 0.317 (P<0.05), and there is a positive correlation between the two, meaning as self-stigma increases, perceived stress increases. The effect of perceived stress on sleep disorders is 0.427 (P<0.05), and there is a positive correlation between the two, meaning as perceived stress increases, sleep disorders increases. The above results indicate that self-stigma indirectly affects sleep disorders through perceived stress. That means perceived stress plays a complete mediating role. Firstly, the self-stigma among gynecologic cancer patients in China might be due to traditional beliefs in China, such as that cancer results from moral transgression and the result of retribution or punishment for past mistakes.Citation14 Especially for gynecological cancer patients, due to the loss of postoperative female characteristics, family roles, and feudal thoughts, patients will feel ashamed in their interactions with their families and medical staff. This is a particularly important issue for gynecological cancer patients in China because they are worried about their self-image and public opinion around cancer.Citation51 Despite growing awareness of gynecologic cancer, perceptions of discrimination might still be widespread.Citation52 Secondly, the findings suggest that gynecologic cancer patients who struggled with stigmatized beliefs are under significant stress due to sensitivities related to their cancer diagnosis and experience, consistent with previous results in other populations.Citation53 Studies of stigma among individuals with chronic health conditions have shown that they experienced significant social isolation, anxiety and stress as a result of internalized negative beliefs about their health conditions.Citation54 According to the cognitive-affective- behavioral model of concealing stigma, the significant situation of stigma might lead to avoidance of discovery, inner conflict, negative emotions, etc., thus leading to great stress.Citation22 Thirdly, self-stigma might cause or exacerbate psychological stress that interferes with sleep behavior. That is, patients with high levels of self-stigma might experience shame associated with diagnosis, fear of social rejection, and judgment from others, all of which add to stress. Cognitive model of insomnia suggests that people are prone to sleep problems because of their stress response.Citation24 High sensory stress is common in gynecologic cancer patients, which leads to disturbance of sleep physiological process, change of sleep structure, and then sleep disorders.Citation50
Limitations
There are several limitations in our study. Firstly, the current research was conducted at one institution in Liaoning Province, China, which might limit its generalizability. Second, Self filled questionnaire might bring bias problems to this study, such as recall bias, measurement bias, etc. Third, we only included few variables that might affect sleep disorders.
Conclusion
Our study is few to use LPA technology to determine specific patterns of sleep disorders in gynecological cancer patients. Our findings indicate three latent patterns of sleep disorders, ie, “Good Sleep group”, “Sleep Deficiency group”, and “Sleep Disturbance group”, which are significantly associated with age, exercise, and perceived stress. And this is the first to examine the mediating effect of perceived stress between self-stigma and sleep disorders, clarifying the mechanism by which self-stigma affects sleep disorders, that is, gynecological cancer patients who feels alienated or discriminated might cause high pressure, which exacerbates sleep disorders.
Author Contributions
All authors made a significant contribution to the work reported, whether that was in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; agreed on the journal to which the article has been submitted; and agreed to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests in this work.
Acknowledgments
The authors would acknowledge the services of staffs in the Department of Gynecology, ShengJing Hospital Affiliated to China Medical University, who helped to get the written informed consent about the conduct of this survey and distribute the questionnaires to the concerned patients.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Additional information
Funding
References
- Sung H, Ferlay J, Siegel RL. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249.
- Mo Y, Zhu X, Lai X, et al. Sleep in nasopharyngeal carcinoma patients before chemotherapy, after induction chemotherapy, and after concurrent chemoradiotherapy. Med Hypotheses. 2020;144:109840.
- Mong JA, Cusmano DM. Sex differences in sleep: impact of biological sex and sex steroids. Philos Trans R Soc Lond B Biol Sci. 2016;371(1688):20150110. doi:10.1098/rstb.2015.0110
- Li W, Li C, Liu T, et al. Self-reported sleep disorders and the risk of all cancer types: evidence from the Kailuan Cohort study. Public Health. 2023;223:209–216. doi:10.1016/j.puhe.2023.08.007
- Kairaitis K, Madut AS, Subramanian H, et al. Cancer sleep symptom-related phenotypic clustering differs across three cancer specific patient cohorts. J Sleep Res. 2022;31(5):e13588. doi:10.1111/jsr.13588
- Tian J, Chen GL, Zhang HR. Sleep status of cervical cancer patients and predictors of poor sleep quality during adjuvant therapy. Support Care Cancer. 2015;23:1401–1408. doi:10.1007/s00520-014-2493-8
- Irwin MR. Why sleep is important for health: a psychoneuroimmunology perspective. Annu Rev Psychol. 2015;66:143–172. doi:10.1146/annurev-psych-010213-115205
- Liang X, Harris HR, Hendryx M, et al. Sleep characteristics and risk of ovarian cancer among postmenopausal women. Cancer Prev Res. 2021;14:55–64. doi:10.1158/1940-6207.CAPR-20-0174
- Ross TL, DeFazio A, Friedlander M, et al. Insomnia and its association with quality of life in women with ovarian cancer. Gynecol Oncol. 2020;158:760–768. doi:10.1016/j.ygyno.2020.06.500
- Wu HJ, Chuang CM, Chien CH, et al. Changes in depression and sleep quality and associated factors in women receiving chemotherapy for ovarian cancer: an observational study. Cancer Nurs. 2021;1:24.
- Doherty AM, Lorenz L, Jabbar F, et al. Sleep Disturbance in Adjustment Disorder and Depressive Episode. Int J Environ Res Public Health. 2019;16(6):1083. doi:10.3390/ijerph16061083
- National Comprehensive Cancer Network: survivorship (Version 1.2019). Available from: https://www.nccn.org/professionals/physician_gls/pdf/survivorship.pdf. Accessed May 25, 2024.
- Pescosolido BA, Martin JK. The stigma complex. Annu Rev Sociol. 2015;41:87–116. doi:10.1146/annurev-soc-071312-145702
- Esses VM. Prejudice and discrimination toward immigrants. Annu Rev Psychol. 2021;72:503–531. doi:10.1146/annurev-psych-080520-102803
- Molloy L, Beckett P, Chidarikire S, et al. Culture, the stigma of mental illness, and young people. J Psychosoc Nurs Ment Health Serv. 2020;58(11):15–18. doi:10.3928/02793695-20201013-03
- Tang PL, Mayer DK, Chou FH, et al. The experience of cancer stigma in Taiwan: a qualitative study of female cancer patients. Arch Psychiatr Nurs. 2016;30(2):204–209. doi:10.1016/j.apnu.2015.08.015
- Ihc W, Tsai W, McNeill LH, et al. The associations of self-stigma, social constraints, and sleep among Chinese American breast cancer survivors. Support Care Cancer. 2020;28(8):3935–3944. doi:10.1007/s00520-019-
- Dong Y. “Premature” Girls with “Illegitimate” diseases: a qualitative exploration of the stigma of gynecological diseases for unmarried young women in China. J Health Commun. 2023;28(2):111–120. doi:10.1080/10810730.2023.2185322
- Ruff RR, Ng J, Jean-Louis G, et al. Neighborhood stigma and sleep: findings from a pilot study of low-income housing residents in New York City. Behav Med. 2018;44(1):48–53. doi:10.1080/08964289.2016.1203
- Craven MP, Fekete EM. Internalized weight stigma, psychological well-being, and sleep in women. Int J Behav Med. 2022;29(2):199–208. doi:10.1007/s12529-021-10008-y
- Jiang T, Jianhua H, Wei J, et al. A moderated serial mediation analysis of the association between HIV stigma and sleep quality in people living with HIV: a cross-sectional study. Transl Behav Med. 2023;13(1):25–33.
- Tang WZ, Yusuf A, Jia K, et al. Correlates of stigma for patients with breast cancer: a systematic review and meta-analysis. Support Care Cancer. 2022;31(1):55. doi:10.1007/s00520-022-07506-4
- Rom O, Reznick AZ. The stress reaction: a historical perspective. Adv Exp Med Biol. 2016;905:1–4. doi:10.1007/5584_2015_195
- Pizzagalli DA. A new chapter for cognitive, affective & behavioral neuroscience. Cogn Affect Behav Neurosci. 2021;21(2):267–268. doi:10.3758/s13415-021-00867-z
- Warmoth K, Wong CCY, Chen L, et al. The role of acculturation in the relationship between self-stigma and psychological distress among Chinese American breast cancer survivors. Psychol Health Med. 2020;25(10):1278–1292. doi:10.1080/13548506.2020.1734638
- Redeker NS, Conley S, Anderson G, et al. Effects of cognitive behavioral therapy for insomnia on sleep, symptoms, stress, and autonomic function among patients with heart failure. Behav Sleep Med. 2020;18(2):190–202. doi:10.1080/15402002.2018.1546709
- Hu Y, Visser M, Kaiser S. Perceived stress and sleep quality in midlife and later: controlling for genetic and environmental influences. Behav Sleep Med. 2020;18(4):537–549. doi:10.1080/15402002.2019.1629443
- Yeung NCY, Ramirez J, Lu Q. Perceived stress as a mediator between social constraints and sleep quality among Chinese American breast cancer survivors. Support Care Cancer. 2017;25(7):2249–2257. doi:10.1007/s00520-017-3632-9
- Callender KA. Understanding antigay bias from a cognitive-affective-behavioral perspective. J Homosex. 2015;62(6):782–803. doi:10.1080/00918369.2014.998965
- Arvind A, Pandya A, Amin L, et al. Social strain, distress, and gender dysphoria among transgender women and Hijra in Vadodara, India. Int J Transgend Health. 2021;23(1–2):149–163.
- Chen C, He Z, Xu B, et al. A latent profile analysis of sleep disturbance in relation to mental health among college students in China. Front Public Health. 2023;11:1107692. doi:10.3389/fpubh.2023.1107692
- Zhang L, Sasser J, Doane LD, et al. Latent profiles of sleep patterns in early adolescence: associations with behavioral health risk. J Adolesc Health. 2024;74(1):177–185. doi:10.1016/j.jadohealth.2023.08.021
- Liu X, Zhang Q, Yu M, et al. Patterns of posttraumatic stress disorder and posttraumatic growth among breast cancer patients in China: a latent profile analysis. Psycho-oncology. 2020;29(4):743–750. doi:10.1002/pon.5332
- Chang Q, Xia Y, Bai S, et al. Association between Pittsburgh sleep quality index and depressive symptoms in Chinese resident physicians. Front Psychiatry. 2021;12:564815. doi:10.3389/fpsyt.2021.564815
- Katsarou A, Panagiotakos D, Zafeiropoulou A, et al. Validation of a Greek version of PSS-14; a global measure of perceived stress. Cent Eur J Public Health. 2012;20(2):104–109. doi:10.21101/cejph.a3698
- Eichhorn S, Mehnert A, Stephan M. Die deutsche Version der Social Impact Scale (SIS-D)--Pilottestung eines Instrumentes zur Messung des Stigmatisierungserlebens an einer Stichprobe von Krebspatienten [German Version of the Social Impact Scale (SIS-D)--Pilot Testing of an Instrument for Measuring Experienced Stigmatization in a Sample of Cancer Patients]. Psychother Psychosom Med Psychol. 2015;65(5):183–190. German. doi:10.1055/s-0034-1398523
- Vrieze SI. Model selection and psychological theory: a discussion of the differences between the Akaike information criterion (AIC) and the Bayesian information criterion (BIC). Psychol Methods. 2012;17(2):228–243. doi:10.1037/a0027127
- Kim SY. Determining the number of latent classes in single- and multi-phase growth mixture models. Struct Equation Model. 2014;21(2):263–279. doi:10.1080/10705511.2014.882690
- Liu Q, Charleston MA, Richards SA, et al. Performance of akaike information criterion and bayesian information criterion in selecting partition models and mixture models. Syst Biol. 2023;72(1):92–105. doi:10.1093/sysbio/syac081
- Ullman JB. Structural equation modeling: reviewing the basics and moving forward. J Pers Assess. 2006;87(1):35–50. doi:10.1207/s15327752jpa8701_03
- Clevenger L, Schrepf A, Degeest K, et al. Sleep disturbance, distress, and quality of life in ovarian cancer patients during the first year after diagnosis. Cancer. 2013;119(17):3234–3241. doi:10.1002/cncr.28188
- Pozzar RA, Hammer MJ, Paul SM, et al. Distinct sleep disturbance profiles among patients with gynecologic cancer receiving chemotherapy. Gynecol Oncol. 2021;163(2):419–426. doi:10.1016/j.ygyno.2021.09.002
- Yoon JE, Oh D, Hwang I, et al. Association between older subjective age and poor sleep quality: a population-based study. Behav Sleep Med. 2023;21(5):585–600. doi:10.1080/15402002.2022.2144860
- Moon E, Kim K, Partonen T, et al. Role of melatonin in the management of sleep and circadian disorders in the context of psychiatric illness. Curr Psychiatry Rep. 2022;24(11):623–634. doi:10.1007/s11920-022-01369-6
- Pearson O, Uglik-Marucha N, Miskowiak KW, et al. The relationship between sleep disturbance and cognitive impairment in mood disorders: a systematic review. J Affect Disord. 2023;327:207–216. doi:10.1016/j.jad.2023.01.114
- Solis-Navarro L, Masot O, Torres-Castro R, et al. Effects on sleep quality of physical exercise programs in older adults: a systematic review and meta-analysis. Clocks Sleep. 2023;5(2):152–166. doi:10.3390/clockssleep5020014
- Nakagawa T, Fukui T, Ohsumi Y, et al. Association between oxygen consumption and stepping exercise standardized with a triaxial accelerometer. Gen Thorac Cardiovasc Surg. 2023;71(1):27–32.
- Stillman CM, Esteban-Cornejo I, Brown B, et al. Effects of exercise on brain and cognition across age groups and health states. Trends Neurosci. 2020;43(7):533–543. doi:10.1016/j.tins.2020.04.010
- Chen R, Slopen N, Lee S. Perceived stress, recent stressors, and distress in relation to sleep disturbance and duration among middle-aged and older Asian immigrants. Sleep Health. 2023;9(2):211–217. doi:10.1016/j.sleh.2022.11.005
- Simon L, Admon R. From childhood adversity to latent stress vulnerability in adulthood: the mediating roles of sleep disturbances and HPA axis dysfunction. Neuropsychopharmacology. 2023;48(10):1425–1435. doi:10.1038/s41386-023-01638-9
- Zhuang H, Wang L, Yu X, et al. Effects of decisional conflict, decision regret and self-stigma on quality of life for breast cancer survivors: a cross-sectional, multisite study in China. J Adv Nurs. 2022;78(10):3261–3272. doi:10.1111/jan.15250
- Paneru B, Karmacharya A, Bharati A, et al. Association between cancer stigma and cervical cancer screening uptake among women of Dhulikhel and Banepa, Nepal. PLoS One. 2023;18(5):e0285771. doi:10.1371/journal.pone.0285771
- Eccles FJR, Sowter N, Spokes T, et al. Stigma, self-compassion, and psychological distress among people with Parkinson’s. Disabil Rehabil. 2023;45(3):425–433. doi:10.1080/09638288.2022.2037743
- Trigueros R, Navarro N, Mercader I, et al. Self-stigma, mental health and healthy habits in parent of children with severe mental disorder. Psychol Res Behav Manag. 2022;15:227–235. doi:10.2147/PRBM.S342780