Abstract
Purpose
The coexistence of insomnia and obstructive sleep apnea (OSA) is very prevalent. Hypoglossal nerve stimulation (HGNS) is an established second-line therapy for patients suffering OSA. Studies investigating the effect of the different aspects of insomnia on the therapeutic outcome are largely missing. Therefore, this study aimed to understand the impact of the different aspects of insomnia on the therapeutic outcome under HGNS therapy in clinical routine.
Patients and Methods
This is a retrospective study including 30 consecutive patients aged 55.40 ± 8.83 years (8 female; 22 male) undergoing an HGNS implantation in our tertiary medical center between 2020 and 2023. All patients underwent preoperative polysomnography (PSG) according to AASM. First follow-up PSG was performed 95.40 ± 39.44 days after activation (30 patients) and second follow-up PSG was performed 409.89 ± 122.52 days after activation (18 patients). Among others, the following PSG-related parameters were evaluated: apnea–hypopnea index (n/h) (AHI) and oxygen desaturation index (n/h) (ODI). Insomnia was assessed by the insomnia severity index (ISI) questionnaire. Preoperatively, all patients included filled out each ISI item. Spearman's-rho correlation coefficient was calculated for correlations.
Results
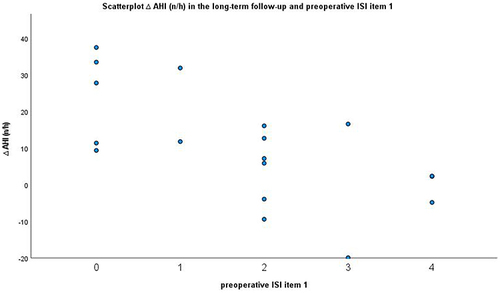
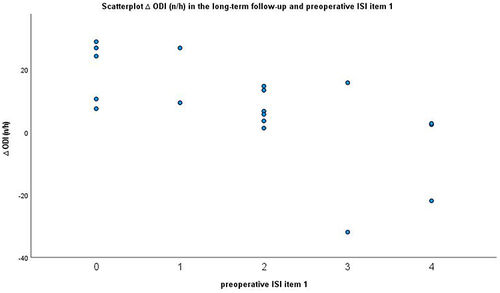
Preoperative score of ISI item 1 (difficulty falling asleep) was 1.93 ± 1.34 and preoperative cumulative ISI score (item1-7) was 18.67 ± 5.32. Preoperative AHI was 40.61 ± 12.02 (n/h) and preoperative ODI was 38.72 ± 14.28 (n/h). In the second follow-up, the mean difference in AHI was ∆ 10.47 ± 15.38 (n/h) and the mean difference in ODI was ∆ 8.17 ± 15.67 (n/h). Strong significant correlations were observed between ISI item 1 (difficulty falling asleep) and both ∆ AHI (r: −0.65, p=0.004) and ∆ ODI (r: −0.7; p=0.001) in the second follow-up.
Conclusion
Difficulty falling asleep may hence negatively influence HGNS therapeutic outcome. Insomnia-related symptoms should be considered in the preoperative patient evaluation for HGNS.
Introduction
Obstructive sleep apnea (OSA) is a highly prevalent sleep disorder. OSA is characterized by recurrent episodes of partial and/or complete upper airway obstructions during sleep that lead to apnea and hypopnea.Citation1 Besides OSA, insomnia is another highly prevalent sleep disorder. Insomnia is defined as an individually reported difficulty with sleep.Citation2 Even though both are considered as separate diseases, they often occur concomitantly. Insomnia-related symptoms are reported by up to 50% of patients suffering OSA and up to 40% of patients suffering from chronic insomnia also meet the diagnostic criteria for OSA.Citation3 The coexistence of insomnia and obstructive sleep apnea (COMISA) is clinical highly relevant. COMISA is associated with worse therapeutic outcomes and higher costs compared to the treatment of either OSA or insomnia.Citation4,Citation5 The standard in OSA therapy is continuous positive airway pressure (CPAP) therapy.Citation6 Hypoglossal nerve stimulation (HGNS) is an established therapeutic options for patients not tolerating PAP-therapy.Citation7 PAP-therapy compliance is especially reduced in patients suffering COMISA.Citation8 Previous studies have reported an association between insomnia and poorer apnea–hypopnea index (AHI) reductionCitation9 as well as shorter usage of HGNS during the nightCitation10 and patient-reported outcomes such as daytime sleepiness.Citation9,Citation11 In contrast, one study showed no significant difference in therapy adherence and efficacy between ISI severity subgroups.Citation12 Insomnia is a complex sleeping disorder involving different symptoms such as difficulty falling asleep, difficulty staying asleep and/or waking too early, and is often related to hyperalertness and fatigue.Citation13 Insomnia may be suspected by a brief screening seven‐item questionnaire named the insomnia severity index (ISI) addressing all aforementioned aspects.Citation14 A few studies already aimed to investigate the impact of insomnia on objective and patient-reported outcomes such as AHI reduction, therapy adherence and daytime sleepiness.Citation9–12 However, studies investigating the effect of the different aspects of insomnia on the therapeutic outcome are largely missing. Therefore, this exploratory study aimed to understand the impact of the different aspects of insomnia on the therapeutic outcome under HGNS therapy in clinical routine.
Materials and Methods
This study included 30 consecutive patients undergoing an implantation of inspiration-coupled HGNS (Inspire Medical Systems, Inc., Golden Valley, MN, USA) between 2020 and 2023. Patients included had to fulfil the indication criteria for HGNS therapyCitation15 such as intolerance to PAP therapy, body mass index (BMI) < 35 kg/m2, absence of complete velar concentric collapse on drug-induced sleep endoscopy (DISE), apnea–hypopnea index (AHI) 15–65/h with <25% central apneas on polysomnography (PSG), and the absence of chronic major psychiatric or neurodegenerative disease. All patients included had filled in a complete preoperative ISI questionnaire. The German version of the ISI questionnaire was used.Citation16 The following questions are included and must be voted on a five-point Likert scale:
Please rate the CURRENT (ie LAST 2 WEEKS) SEVERITY of your insomnia problem(s)
Difficulty falling asleep
Difficulty staying asleep
Problems waking up too early
How satisfied/dissatisfied are you with your current sleep pattern?
How NOTICEABLE to others do you think your sleep problem is in terms of impairing the quality of your life?
How worried/distressed are you about your current sleep problem?
To what extent do you consider your sleep problem to INTERFERE with your daily functioning (eg daytime fatigue, mood, ability to function at work/daily chores, concentration, memory, mood, etc). currently?
An increasing score indicates an increasing clinically relevant insomnia.Citation14 All patients underwent preoperative polysomnography (PSG) according to the AASM standard. Furthermore, a velar concentric collapse was ruled out by preoperative DISE. First PSG follow-up was performed 95.40 ± 39.44 days after activation and second follow-up was performed 409.89 ± 122.52 days after activation. First follow-up was performed in all 30 patients, second follow-up was performed in 18 patients. All follow-up PSGs were performed without any in-laboratory titration. Stimulation parameters under PSG were identical to the patient’s stimulation parameters as used at the patients’ homes for at least one week before in-laboratory PSG.
The following PSG-related parameters were investigated: apnea–hypopnea index (n/h) (AHI), cumulative time under apnea and hypopnea (min), snoring index (n/h) (SI), oxygen desaturation index (n/h) (ODI), percentage of total sleep time under oxygen saturation lower than 90% (t90) and total number of arousal events per hour (arousal index (n/h)). PSG was evaluated by our team's experts in the field of sleep medicine.
All patients provided informed consent to the use of their data for research purposes. The data were evaluated in a pseudonymized fashion. Only health data that are collected in the clinical routine were analyzed retrospectively. So-called “third parties” did not have access to the data and publication occurs exclusively in anonymized form. The Ethics Committee of the Rhineland-Palatinate Medical Association refrains from providing advice in such cases, citing the State Hospital Act (§36 and §37) (see also: https://www.laek-rlp.de/ausschuesse-kommissionen/ethikkommission/).
Statistical Analysis
Statistical analysis was performed using SPSS 27 (IBM, Armonk, NY, USA). All data were expressed as mean ± standard deviation. Wilcoxon’s signed-rank test was performed for inner-group comparison. Preoperative as well as for the short-term follow-up all patients included filled out each ISI item. Only 12 patients filled out each ISI item in the long-term follow-up. Spearman's-rho correlation coefficient was calculated for correlations. p<0.05 was considered a statistically significant result. For correlation coefficients Bonferroni correction was performed. Therefore p<0.004 was considered a statistically significant result. Post-hoc power calculation was performed using an online power calculatorCitation17 with α=0.05 and n=18.
Results
Patients were aged M = 55.40 ± 8.83 years at the time of implantation of the HGNS system with an average BMI of M = 29.69 ± 4.32 kg/m2. Eight patients were female, 22 patients were male. Preoperative AHI was M = 40.61 ± 12.02 (n/h), preoperative complete time of apnoea and hypopnea was M = 86.2 ± 40.2 (min), preoperative snoring index M = 244.26 ± 181.14 (n/h), preoperative ODI was M = 38.72 ± 14.28 (n/h), preoperative t90 (%) was M = 8.85 ± 10.35 and preoperative arousal index was M = 23.68 ± 15.59 (n/h).
Preoperative scores of the separate ISI questionnaire were as follows: Question 1 was M = 1.93 ± 1.34, question 2 was M = 2.8 ± 1.00, question 3 was M = 1.97 ± 1.27, question 4 was M = 3.5 ± 0.73, question 5 was M = 2.33 ± 1.21, question 6 was M = 3.20 ± 1.03, question 7 was M = 2.97 ± 1.13. Mean of cumulative preoperative ISI was M = 18.67 ± 5.32 (). Mean of cumulative ISI was M = 12.7 ± 6.62 in the short-term follow-up and M = 10.08 ± 7.13 in the long-term follow-up. Preoperative cumulative ISI and cumulative ISI in the short-term follow-up differed (p<0.001) significantly as well as in the long-term follow-up (p=0.003). Preoperative Cronbach’s Alpha for items 1–7 was α=0.8 ().
Table 1 ISI Score in the Preoperative, Short-Term Follow-Up and Long-Term Follow-Up
In the short-term follow-up, the mean difference in AHI was ∆ 15.01 ± 12.15 (n/h), the mean difference in complete time of apnea and hypopnea was ∆ 34.40 ± 36.31 (min), the mean difference in snoring index was ∆ 89.68 ± 115.43 (n/h), the mean difference in ODI was ∆ 9.18 ± 13.21 (n/h), the mean difference in t90 was ∆ 2.49 ± 11.47 (%) and the mean difference in arousal index was ∆ 8.38 ± 16.51 (n/h) ().
Table 2 Patients and PSG Parameters
In the long-term follow-up, the mean difference in AHI was ∆ 10.47 ± 15.38 (n/h), the mean difference in complete time of apnea and hypopnea was ∆ 25.78 ± 34.23 (min), the mean difference in snoring index was ∆ 65.81 ± 158.75 (n/h), the mean difference in ODI was ∆ 8.17 ± 15.67 (n/h), the mean difference in t90 was ∆ 3.94 ± 10.44 (%) and the mean difference in arousal index was ∆ 1.23 ± 14.32 (n/h) ().
In the short-term follow-up, no significant correlations were shown between the separate score for each one out of the seven ISI items and ∆ AHI, ∆ cumulative time of apnea and hypopnea, ∆ snoring index, ∆ ODI, ∆ t90 or ∆ arousal index ().
Table 3 Correlation Between ISI Score and Each ISI Item and ∆ PSG Parameter (Short-Term)
In the long-term follow-up, significant strong negative correlations were shown between question one of the ISI questionnaire and ∆ AHI (r: −0.65, p=0.004), ∆ ODI (r: −0.7; p= 0.001), ∆ t90 (r: −0.51; p=0.03) and ∆ arousal index (r: −0.64; p=0.04) ( and and ).
Table 4 Correlation Between ISI Score and Each ISI Item and ∆ PSG Parameter (Long-Term)
A post-hoc power of 0.87 for the correlation coefficient between question one of the ISI questionnaire and ∆ AHI (r: −0.65) and a post-hoc power of 0.93 for the correlation coefficient between question one of the ISI questionnaire and ∆ ODI (r: −0.70) were calculated.
Discussion
We provide evidence for strong significant negative correlations between patient-reported scores to item one of the ISI questionnaire (i.e. difficulty falling asleep) and objective HGNS therapy outcome metrics such as the AHI, ODI and arousal index in long-term follow-up.
This is one of the first studies investigating the association between the different insomnia-related symptoms on PSG-related metrics. A strong negative correlation between preoperative difficulty falling asleep and important PSG-related metrics in the one-year follow-up could be shown. One possible explanation for this fact could be a reduced therapy compliance (reduced device usage) in patients suffering some specific insomnia-related symptoms. The co-occurrence of OSA and insomnia may impair OSA treatment by reducing compliance with PAP therapy.Citation18,Citation19 Further studies demonstrated especially insomnia-related symptoms associated with lower PAP therapy adherence.Citation8,Citation20 PAP adherence is reduced in patients with initial and late insomnia at baseline.Citation21 Even if PAP adherence is reduced in patients suffering COMISA, insomnia-related symptoms are reduced under PAP therapyCitation21 as well as under HGNS therapy.Citation9,Citation12,Citation22 Insomnia symptoms are reported by up to 50% of patients suffering OSA and up to 40% patients suffering chronic insomnia also meet the diagnostic criteria for OSA.Citation8 PAP-intolerance is a key indication criterion for considering HGNS treatment. Therefore, patients who are HGNS therapy candidates may actually be patients with more pronounced insomnia-related symptoms. Adherence to HGNS therapy may therefore be higher in patients without comorbid insomnia. However, two studies investigated the effect of insomnia on the HGNS therapy adherence.Citation12,Citation23 Both reported no association between insomnia and HGNS therapy adherence. There was no significant difference between HGNS adherence in patients with OSA only compared to COMISA.Citation23 Furthermore, in the ADHERE registry no significant difference in therapy adherence between the group with preoperative ISI<15 and preoperative ISI>15 was observed.Citation12 However, a general reduction in HGNS-therapy adherence over time was observed.Citation24 This is a potential explanation of why a significant negative correlation was observed between preoperative difficulty falling asleep and important PSG-related metrics in the one-year follow-up but not in the short-term follow-up. Patients with increased difficulty falling asleep could therefore be more affected by reduced therapy adherence over time.
There are different studies investigating the impact of insomnia on the therapeutic outcome under HGNS therapy measured by PSG-related parametersCitation9,Citation12 as well as on patient-reported outcomesCitation11 and vice versa.Citation22 However, the results are to date inconsistent. One study proved no significant difference in AHI reduction between a group with a preoperative ISI score <15 and a group with a preoperative ISI score >15.Citation12 Another study could prove a significant negative correlation between preoperative ISI score and postoperative AHI reduction in the short-term follow-up after three months.Citation9
Most of the existing studies reported an improved ISI score under HGNS therapy. One study demonstrated a clinically relevant ISI score reduction in a higher percentage of those patients treated with a HGNS therapy compared to PAP therapy.Citation22 A significant ISI score reduction under HGNS therapy in the short-term follow-up has been reported before.Citation9 In the ADHERE registry all patients had an improved ISI score at follow-up visits (p<0.001). These patients with higher preoperative ISI scores showed a greater reduction in insomnia-related symptoms compared to those with lower preoperative ISI scores, ISI≥15 compared with ISI<15 (p<0.05).Citation12 The same study showed significant improvement for the ISI score and for each item in the ISI score from baseline to post-titration (PT) and baseline to final visit:Citation12 ISI was reduced by −7 ± 6.17 from baseline to the first PSG-based titration and by −8.06 ± 7.27 from baseline to final visit. These results are comparable to the results of our study. We are reporting here a preoperative ISI score of 18.67 ± 5.32, a post-operative short-term ISI score of 12.7 ± 6.62 and a long-term post-operative ISI score of 10.08 ± 7.13 points. Furthermore, each item of the ISI score was improved from baseline to the first PSG-based titration post-titration with a further improvement post-titration to final visit.Citation12 Our study also showed an improvement in each item in the short-term follow-up with a further improvement in the long-term follow-up, except for item 3. Of note, our patients did not receive any in-laboratory HGNS device titration during the PSG night. Therefore, our reported results may more closely depict the respective metrics at the patients’ home.
The result of our study with greater improvement in insomnia-related symptoms with longer therapy seems to be counterintuitive to the result of more improvement of PSG-related parameters in the short-term follow-up compared to long-term follow-up in our study. This indicates that not only PSG-related parameters are associated with insomnia-related patient-reported outcomes. Previously, one study provided evidence that cognitive behavioural therapy combined with PAP is superior to PAP alone on insomnia-related outcomes.Citation25 Other authors showed an improvement in PAP therapy adherence and insomnia-related symptoms in patients suffering COMISA under cognitive behavioural therapy for insomnia.Citation26 We therefore suggest that comorbid insomnia in OSA patients under consideration for or after HGNS implantation should gain more attention. Further studies, especially investigating the added value of any additional behavioural therapy for patients suffering comorbid OSA and insomnia under HGNS therapy, may provide clinical insight on this important issue.
Limitations
Relevant limitations of our study are the relatively small sample size and the retrospective nature of this study. However, a sufficient post-hoc power of 0.87 for the correlation coefficient between question one of the ISI questionnaire and ∆ AHI (r: −0.65) in the long-term follow-up and a post-hoc power of 0.93 for the correlation coefficient between question one of the ISI questionnaire and ∆ ODI (r: −0.70) in the long-term follow-up were calculated. Furthermore, not all patients filled out the ISI questionnaire in the long-term follow-up. Data on therapy adherence were not available. Therefore, a possible association between difficulty falling asleep and therapy adherence cannot be proven, based on our available data. However, the gained data are of high quality and provide new information about the therapeutic outcome of patients treated by HGNS.
Conclusion
To the best of our knowledge this is one of the first studies investigating the association between the different separate insomnia-related symptoms on PSG-metrics in patients undergoing HGNS implantation. A strong significant correlation between question one of the ISI questionnaire (difficulty falling asleep) and both ∆ AHI (r: −0.65, p=0.004) and ∆ ODI (r: −0.7; p= 0.001) in the long-term follow-up could be shown. Difficulty falling asleep seems to be a significant and relevant clinical factor, associated with worse HGNS therapeutic outcome. Therefore, insomnia-related symptoms should be considered both at the time point of decision to implant a HGNS as well as postoperatively after implantation. Further studies are necessary to understand the impact of insomnia on HGNS therapeutic outcome and to investigate the potential benefits of further therapies, such as behavioral therapies, on HGNS therapeutic outcome in patients with PAP-intolerance suffering from COMISA.
Abbreviations
COMISA, coexistence of insomnia and obstructive sleep apnea; OSA, obstructive sleep apnea;
HGNS, hypoglossal nerve stimulation; CPAP, continuous positive airway pressure; PAP, positive airway pressure; PSG, polysomnography; ISI, insomnia severity index; AHI, apnea–hypopnea index; BMI, body mass index; DISE, drug-induced sleep endoscopy; ODI, oxygen desaturation index (n/h).
Ethics Approval and Consent to Participate
All patients provided informed consent to the use of their data for research purposes. The data were evaluated in a pseudonymized fashion. Only health data that are collected in the clinical routine were analyzed retrospectively. So-called “third parties” did not have access to the data and publication occurs exclusively in anonymized form. The Ethics Committee of the Rhineland-Palatinate Medical Association refrains from providing advice in such cases, citing the State Hospital Act (§36 and §37) (see also: https://www.laek-rlp.de/ausschuesse-kommissionen/ethikkommission/).
Disclosure
H.G. reports research grants by Inspire Medical Systems, Inc. (MN, USA) that are unrelated to this study. The other authors have no conflicts of interest to declare in this work.
Data Sharing Statement
The data underlying this article cannot be shared publicly for the privacy of individuals that participated in the study. The data will be shared on reasonable request to the corresponding authors.
Additional information
Funding
References
- Rundo JV. Obstructive sleep apnea basics. Cleve J Med. 2019;86(9 Suppl 1):2–9. doi:10.3949/ccjm.86.s1.02
- Roth T. Insomnia: definition, prevalence, etiology, and consequences. J Clin Sleep Med. 2007;3(5 Suppl):1.
- Sweetman A, Lack L, McEvoy RD, et al. Bi-directional relationships between co-morbid insomnia and sleep apnea (COMISA). Sleep Med Rev. 2021;60:101519. doi:10.1016/j.smrv.2021.101519
- Krakow B, Melendrez D, Ferreira E, et al. Prevalence of insomnia symptoms in patients with sleep-disordered breathing. Chest. 2001;120(6):1923–1929. doi:10.1378/chest.120.6.1923
- Tasbakan MS, Gunduz C, Pirildar S, Basoglu OK. Quality of life in obstructive sleep apnea is related to female gender and comorbid insomnia. Sleep Breath. 2018;22(4):1013–1020. doi:10.1007/s11325-018-1621-y
- Qaseem A, Holty J-EC, Owens DK, Dallas P, Starkey M, Shekelle P. Management of obstructive sleep apnea in adults: a clinical practice guideline from the American College of Physicians. Ann Internal Med. 2013;159(7):471–483. doi:10.7326/0003-4819-159-11-201312030-00009
- Strollo PJ, Soose RJ, Maurer JT, et al. Upper-airway stimulation for obstructive sleep apnea. N Engl J Med. 2014;370(2):139–149. doi:10.1056/NEJMoa1308659
- Wickwire EM, Smith MT, Birnbaum S, Collop NA. Sleep maintenance insomnia complaints predict poor CPAP adherence: a clinical case series. Sleep Med. 2010;11(8):772–776. doi:10.1016/j.sleep.2010.03.012
- Pordzik J, Ludwig K, Seifen C, et al. Insomnia in patients undergoing hypoglossal nerve stimulation therapy for obstructive sleep apnea. Biology. 2023;12(1):98. doi:10.3390/biology12010098
- Kaffenberger TM, Chandna M, Kaki P, et al. Reduced usage of upper airway stimulation therapy in patients with comorbid insomnia and obstructive sleep apnea. J Clin Sleep Med. 2023;19(12):1997–2004. doi:10.5664/jcsm.10752
- Steffen A, Baptista P, Ebner EM, Jeschke S, Konig IR, Bruchhage KL. Insomnia affects patient-reported outcome in sleep apnea treated with hypoglossal nerve stimulation. Laryn Iinves otolar. 2022;7(3):877–884. doi:10.1002/lio2.761
- Dhanda Patil R, Ishman SL, Chang JL, Thaler E, Suurna MV. Impact of insomnia on hypoglossal nerve stimulation outcomes in the adhere registry. Laryngoscope. 2023;134(1):471–479. doi:10.1002/lary.30933
- Ong JC, Crawford MR. Insomnia and obstructive sleep apnea. Sleep Med Clini. 2013;8(3):389–398. doi:10.1016/j.jsmc.2013.04.004
- Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297–307. doi:10.1016/S1389-9457(00)00065-4
- Steffen A, Heiser C, Galetke W, et al. Die Stimulation des Nervus hypoglossus in der Behandlung der obstruktiven Schlafapnoe–Aktualisiertes Positionspapier der Arbeitsgemeinschaft Schlafmedizin der DGHNO-KHC. Laryngo-Rhino-Otologie. 2021;100(01):15–20. doi:10.1055/a-1327-1343
- Gerber M, Lang C, Lemola S, et al. Validation of the German version of the insomnia severity index in adolescents, young adults and adult workers: results from three cross-sectional studies. BMC Psychiatry. 2016;16(1):1–14. doi:10.1186/s12888-016-0876-8
- Hemmerich W. Poweranalyse für Korrelationen. StatistikGuru Re. 2018;6:2020.
- Wickwire EM, Collop NA. Insomnia and sleep-related breathing disorders. Chest. 2010;137(6):1449–1463.
- Bahr K, Cámara RJ, Gouveris H, Tuin I. Current treatment of comorbid insomnia and obstructive sleep apnea with CBTI and PAP-therapy: a systematic review. Front Neurol. 2018;9:804. doi:10.3389/fneur.2018.00804
- Pieh C, Bach M, Popp R, et al. Insomnia symptoms influence CPAP compliance. Sleep Bre. 2013;17(1):99–104. doi:10.1007/s11325-012-0655-9
- Bjornsdottir E, Janson C, Sigurdsson JF, et al. Symptoms of insomnia among patients with obstructive sleep apnea before and after two years of positive airway pressure treatment. Sleep. 2013;36(12):1901–1909. doi:10.5665/sleep.3226
- Pascoe M, Wang L, Aylor J, et al. Association of Hypoglossal Nerve Stimulation With Improvements in Long-term, Patient-Reported Outcomes and Comparison With Positive Airway Pressure for Patients With Obstructive Sleep Apnea. JAMA otolaryngology-- head & neck surgery. JAMA Otolaryngology-- Head & Neck Surgery. 2022;148(1):61–69. doi:10.1001/jamaoto.2021.2245
- Dhanda Patil R, Hong MP, Ishman SL. Hypoglossal nerve stimulation in veterans with comorbid insomnia and sleep apnea. Otolar Neck Surg. 2021;164(6):1345–1353. doi:10.1177/0194599820982638
- Coca KK, Heiser C, Huntley C, et al. Hypoglossal nerve stimulation usage by therapy nonresponders. Otolar Head and Neck Surg. 2022;166(4):786–790. doi:10.1177/01945998211036867
- Ong JC, Crawford MR, Dawson SC, et al. A randomized controlled trial of CBT-I and PAP for obstructive sleep apnea and comorbid insomnia: main outcomes from the MATRICS study. Sleep. 2020;43(9): doi:10.1093/sleep/zsaa041.
- Alessi CA, Fung CH, Dzierzewski JM, et al. Randomized controlled trial of an integrated approach to treating insomnia and improving the use of positive airway pressure therapy in veterans with comorbid insomnia disorder and obstructive sleep apnea. Sleep. 2021;44(4): doi:10.1093/sleep/zsaa235.