Abstract
Rapid eye movement (REM) sleep behavior disorder (RBD) is a parasomnia characterized by a history of recurrent nocturnal dream enactment behavior and loss of skeletal muscle atonia and increased phasic muscle activity during REM sleep: REM sleep without atonia. RBD and associated comorbidities have recently been identified as one of the most specific and potentially sensitive risk factors for later development of any of the alpha-synucleinopathies: Parkinson’s disease, dementia with Lewy bodies, and other atypical parkinsonian syndromes. Several other sleep-related abnormalities have recently been identified in patients with RBD/Parkinson’s disease who experience abnormalities in sleep electroencephalographic frequencies, sleep–wake transitions, wake and sleep stability, occurrence and morphology of sleep spindles, and electrooculography measures. These findings suggest a gradual involvement of the brainstem and other structures, which is in line with the gradual involvement known in these disorders. We propose that these findings may help identify biomarkers of individuals at high risk of subsequent conversion to parkinsonism.
Introduction
Rapid eye movement (REM) sleep behavior disorder (RBD) is a parasomnia characterized by a history of recurrent nocturnal dream enactment behavior and loss of skeletal muscle atonia and increased phasic muscle activity during REM sleep: REM sleep without atonia (RSWA). RBD was first described in animals by Jouvet in 1965Citation1 and in humans by Schenck et al in 1986 and Sforza et al in 1988.Citation2–Citation4 RBD is a complex, multidimensional parasomnia that is frequently linked with other sleep disorders (eg, untreated sleep apnea, narcolepsy with cataplexy of hypocretin-deficient type), a wide range of neurodegenerative disorders, and the pharmacotherapy of psychiatric and medical disorders (eg, antidepressants, beta-blockers). Imaging studies, clinico-electrophysiological and experimental models of RBD in cats and rats, and transgenic RBD mouse modelsCitation5 have increased our knowledge of the underlying brainstem mechanisms of REM-atonia and REM sleep phasic motor activity. RSWA has been closely associated with hypocretin-deficient narcolepsy,Citation6,Citation7 and very strong associations have been identified between RBD and the alpha-synucleinopathies, primarily Parkinson’s disease (PD), dementia with Lewy bodies (DLB), and multiple system atrophy (MSA).Citation8–Citation10 Schenck et al were the first to perform a follow-up study and reported that 38% of their original cohort of 29 patients had developed parkinsonism.Citation11 Twenty years after diagnosis, 81% of that cohort had parkinsonism.Citation8 Subsequent studies have reported that approximately half of the patients with idiopathic RBD (iRBD) develop a synucleinopathy within ∼12 years of diagnosis of RBD.Citation9,Citation10 These studies include highly selected patients undergoing full video-polysomnography (PSG) recording from neurological sleep centers.
The finding that iRBD often heralds future parkinsonism has stimulated research on predictors of imminent parkinsonism in RBD. The most elusive goal is to enroll high-risk patients in therapeutic studies with promising neuroprotective (ie, disease-modifying) agents that could prolong, or ideally halt, the progression of iRBD to clinical parkinsonism/dementia.
Comorbid findings in RBD
Patients with iRBD typically present with a varying degree of nonmotor symptoms, including impaired olfactory function, cognitive function,Citation12 and autonomic function determined by heart rate changes;Citation13 cardiac 123I-metaiodobenzylguanidine (MIBG) uptake reduction;Citation14,Citation15 gastrointestinal abnormalitiesCitation16; and electroencephalographic slowing.Citation17 Although all of these nonmotor symptoms have been associated with parkinsonism, each of these symptoms individually has a too low specificity and sensitivity of predicting later development of parkinsonism. Hyposomnia and constipation, for instance, are often observed in the preclinical disease stage, but have a too low specificity for predicting PD.Citation18 However, a combination of nonmotor symptoms, especially hyposomnia and RBD, has been found to increase risk of developing PD.Citation18–Citation20
Nevertheless, these findings generally support the assumption that RBD is part of a general progressive neurodegenerative process primarily involving the brainstem area, with later involvement of other brain structures.
Neurophysiology of REM sleep
REM sleep is characterized by: 1) tonic components: electroencephalogram (EEG), muscle atonia, and loss of thermoregulation; and 2) phasic components: REMs, muscle twitches occurring against a background of atonia, ponto-geniculo-occipital waves, as well as irregularities in breathing, heart rate, and blood pressure.
The EEG during REM sleep resembles that during wakefulness, which is characterized by low voltage and mixed frequency in the cerebral cortex, with 5–9 Hz waves in the hippocampus. Therefore, REM sleep is also called as “active” or “paradoxical” sleep.
There is sustained low muscle tone during REM sleep in most of the somatic muscles except those of the inner ear, eye, and diaphragm.Citation21 Cranial muscles of the eyes, ears, and jaw, as well as muscles of the limb extremities may show phasic twitches/movements against a background of atonia during REM sleep. However, phasic activity in postural muscles is rarely seen.Citation22
The orchestration of these tonic and phasic REM sleep suggests the existence of an “executive mechanism” that generates and maintains REM sleep.Citation21,Citation23,Citation24
In the brainstem, there are at least two systems involved in wakefulness and nonrapid eye movement (NREM) and REM sleep: REM-off and REM-on systems.Citation21,Citation23,Citation24
Neurons belonging to the REM-off system include the ventrolateral periaqueductal gray (vlPAG) and the dorsal deep mesencephalic reticular nucleus (dDpMe). These nuclei are active during wakefulness and NREM sleep, and are activated by projections from the wake-active noradrenergic locus coeruleus, serotonergic raphe nucleus, and the hypocretinergic neurons from the lateral thalamus. Furthermore, the REM-off vlPAG and dDpMe are the only pontomedullary structures containing a large number of GABAergic neurons projecting to the sublaterodorsal (SLD) nucleus, the structure critical for generating and maintaining REM sleep.Citation25,Citation26 When the vlPAG/dDpMe is inhibited by GABAergic projections from the ventrolateral preoptic nucleus and the lateral hypothalamus,Citation23,Citation27 a marked increase in REM sleep is seen in ratsCitation25 and cats.Citation28,Citation29
The REM-off system has reciprocal interactions with the REM-on system, and these two systems mutually inhibit each other by means of the neurotransmitter GABA.Citation27 During wakefulness and NREM, the REM-off neurons send inhibitory GABAergic projections to structures belonging to the REM-on system to prevent the occurrence of REM sleep. During REM sleep, the REM-on neurons send inhibitory GABAergic/glycinergic projections to structures belonging to the REM-off system.Citation30
Neurons in the caudal laterodorsal tegmental nucleus (cLDT) and SLD (cLDT-SLD) are regarded as critical sites for the generation and maintenance of REM sleep, the “executive mechanism”.Citation5,Citation31,Citation32 These neurons activate the precoeruleus and parabrachial nucleus, which are involved in REM-EEG. In addition, the ventral part of the SLD induces sensory inhibition and motor atonia during REM sleep. The SLD contains glutamatergic neurons that directly project to inhibitory interneurons in lamina VIII of the spinal cord and to nuclei, inducing atonia in the ventromedial medulla.Citation27,Citation33 In turn, the spinal interneurons and the ventromedial medulla project GABAA/B/glycine to the spinal and cranial motoneurons, thereby hyperpolarizing the motor-facilitatory neurons and inducing atonia.Citation5,Citation27,Citation31,Citation34,Citation35 Nuclei in the ventromedial medulla, belonging to the REM-on system, include the magnocellular reticular nucleus, gigantocellular nucleus (GiA, GiV), paragigantocellular nucleus (DPGi, LPGi), parvicellular nucleus, and the raphe magnus.Citation26,Citation31,Citation36
Lesions of the SLD, such as a deletion of the Vglut2 in the cLDT-SLD, result in REM fragmentation, which is characterized by reductions in REM sleep epoch duration and an increase in the number of REM episodes. The SLD has direct projections to lamina VIII in the spinal cord, where they excite GABA/glycinergic interneurons. Elimination of GABA/glycinergic transmission from these interneurons in the ventral horn at the C3–C4 level in mice results in brief twitching and jerking movements, predominantly in the upper body and sporadically in the lower body.Citation37 In addition, lesions of the SLD result in complex behaviors during REM sleep, symptoms consistent with the human syndrome of RBD.Citation27 Therefore, it has been hypothesized that the SLD specifically functions to antagonize the phasic activity of postural muscles of complex behaviors driven by the motor cortex.Citation38 In contrast, cell-body lesions of the ventromedial medulla seem to cause simple behaviors, such as rapid phasic jerking and twitching movements, during REM sleep in rats and cats.Citation39,Citation40 However, more complex behaviors, as seen with lesions of the SLD, are not observed. Therefore, the ventromedial medulla only partially mediates the SLD control of REM atonia.
Recent findings have revealed that glutamatergic neurons in the rostral parvocellular reticular formation are critical for phasic masseter activity during REM sleep.Citation41
As SLD lesions apparently do not affect phasic masseter activity during REM sleep,Citation41 it was hypothesized that the SLD is not the generator of phasic activity in this muscle and that it specifically antagonizes the complex activity of postural muscles driven by the motor cortex and simple behaviors controlled by the ventromedial medulla–spinal projections.Citation38
Brainstem areas other than the SLD and the ventromedial medulla may be involved in the control of REM atonia. A study performed by Lai et al reported that lesions in the mesopontine junction cause periodic limb movements during REM sleep in cats.Citation42 In addition to glutamate and GABA/glycine, other neurotransmitter systems may mediate REM atonia, by direct projections to the spinal cord or by acting on the vlPAG matter, lateral pontine tegmentum, SLD, or ventromedial medulla neurons, including monoaminergic, orexinergic, and melanin-concentrating hormones.Citation33,Citation43–Citation45 In summary, animal studies indicate that the SLD is the critical region for the control of REM atonia, and lesions of the SLD give rise to the full phenotype of RBD, whereas lesions to the ventromedial medulla produce muscle jerks and twitches.
The occurrence of RBD is consistent with the findings of a study in 2003 by Braak et al,Citation46 who described a staging system for the neuropathological development of PD. The aggregation of Lewy bodies is hypothesized to arise from the dorsal motor nucleus of the vagal nerve in the medulla and in the olfactory bulb, and to emerge through the coeruleus/subcoeruleus complex and the magnocellularis reticular nucleus until it involves the substantia nigra, which has been associated with the daytime motor symptoms of PD. Neuropathological studies of iRBD reveal the presence of Lewy bodies in the brain.Citation47
Generally, the staging suggests that the accumulation of aggregated intracytoplasmic proteins has a general distribution, primarily including the upper area of the medulla oblongata and lower brainstem region with progressive involvement of other parts of the brainstem and midbrain. The joint involvement of the olfactory area suggests that specific parts of the brain are more prone to this, but the specific mechanism is not known in detail. The spreading pattern partly explains the progressive distribution of the involvement of nonmotor symptoms and other characteristics, eg, initial gastrointestinal symptoms (vagal nuclei/autonomic function) and loss of REM atonia (SLD nuclei).Citation48 The picture of neuropathological spreading of Lewy bodies is probably more complex, as not all diagnosed PD patients have a history of recurrent dream enactment behavior and RBD and as other nonmotor symptoms occur with varying intensities prior to and in PD and other alpha-synucleinopathies.
RBD diagnosis
According to the third edition of the International Classification of Sleep Disorders (2012), the following criteria are required to make a diagnosis of RBD:
Repeated episodes of sleep-related vocalization and/or complex motor behaviors;
These behaviors are documented by PSG to occur during REM sleep, or based on clinical history of dream enactment, and are presumed to occur during REM sleep;
Polysomnographic recordings demonstrating RSWA; and
The disturbance not better explained as another sleep disorder, mental disorder, medication, or substance use.
According to the American Academy of Sleep Medicine, RSWA is defined by sustained muscle activity in REM sleep (Stage R) with 50% of the epoch having increased chin electromyography (EMG) amplitude, and/or excessive transient muscle activity, defined by the presence of five or more mini-epochs (a 30-second epoch is divided into ten 3-second mini-epochs) in an epoch featuring transient muscle activity lasting at least 0.5 seconds.Citation22
A diagnosis of RBD cannot be made unless dream enactment and RSWA are both present, so a PSG is required to make the diagnosis. RBD has a wide spectrum of overt symptoms, such as twitching, jerking, shouting, and screaming, as well as more complex behaviors, including punching and escape behaviors, that may cause harm to some patients or bedpartners. The simultaneous video-PSG recording is essential for evaluating these movements and vocalizations appearing during REM sleep and to discount the presence of epileptiform activity in the EEG derivations in order to make a diagnosis of RBD.Citation49
While violent and complex dream enactment behavior is rarely observed during a single night’s PSG recordings, an abnormal state of increased EMG tone during REM sleep and sparse limb jerks are common events.
Polysomnographic findings in RBD
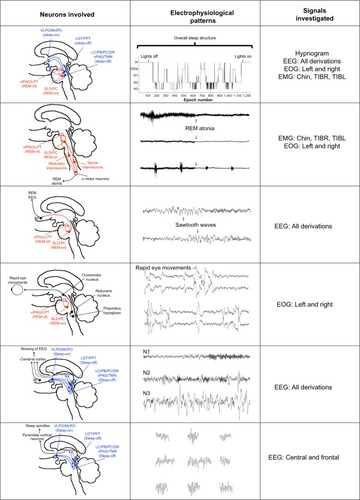
PSG consists of a comprehensive and simultaneous recording of various body functions, including brain activity (electroencephalogram [EEG]), eye movements (electrooculography [EOG]), muscle activity (electromyogram [EMG]), and heart rhythm (electrocardiogram [ECG]) during sleep. Several studies have evaluated the involvement of different PSG findings. These abnormalities are presented later. A schematic representation of these PSG abnormalities and their potential neurophysiological and neuroanatomical findings is presented in .
Figure 1 Examples of potential PD biomarkers expressed in polysomnographic signals and their neuroanatomical correlates.
Abbreviations: PD, Parkinson’s disease; REM, rapid eye movement; NREM, nonrapid eye movement; EEG; electroencephalogram; EOG, electrooculography; EMG, electromyography; SLD, sublaterodorsal region; VLPO/MnPO, ventrolateral/median preoptic nucleus; LDT, laterodorsal tegmental nucleus; PPT, pedunculopontine tegmental nucleus; LC, locus coeruleus; PC, precoeruleus area; DR, dorsal raphe nucleus; vPAG, ventral periaqueductal gray; TMN, tuberomammillary nucleus; vlPAG, ventrolateral periaqueductal gray matter; LPT, lateral pontine tegmentum; BF, basal forebrain.
Scoring RBD
Lapierre and Montplaisir were the first to present an objective scoring method, based on visual analysis of PSG studies.Citation50 Since this initial description of RSWA, several methods for scoring of RBD have been proposed, analyzing RSWA with semiautomated or fully automated algorithms. Frauscher et al suggested a PSG montage quantifying “any” EMG activity (tonic, phasic, or both) in the mentalis muscle and phasic EMG activity in the right and left flexor digitorum superficialis muscles in the upper limbs, with a cutoff of 32% (when using 3-second mini-epochs) for the diagnosis of RBD.Citation51 Ferri et al measured the amplitude of the submentalis muscle during sleep in 21 patients with iRBD, ten patients with MSA, and ten healthy controls, and provided practical indices for the objective evaluation of EMG atonia and EMG activations by means of a sleep atonia index.Citation52 A subsequent study by Montplaisir et alCitation53 attempted to identify cutoff values for tonic and phasic EMG activity in submentalis muscle and to assess the sensitivity and specificity of these values, taken separately or in combination, to diagnose patients with iRBD. They studied 80 patients with iRBD and 80 age- and sex-matched controls. Tonic and phasic EMG activities were visually identified in the chin, but not in the limbs. Completely correct classification of 81.9% was found for tonic chin EMG density ≥30%; 83.8% for phasic chin EMG density ≥15%, and 75.6% for ≥24 leg movements/hour of REM sleep. Another study by Frandsen et al defined a method for establishing a baseline in automatic quantifying submental motor activity during REM sleep in iRBD, PD, and controls.Citation54 They found that no control had >30% of REM sleep with increased motor activity. However, patients with known RBD had activity as low as 4.5%. There is currently no comparison between the two methods, especially with respect to emphasizing the accuracy and the association with later neurodegenerative development.
The studies differ in their methods and definition of RBD EMG activity in the separation between patients with (i)RBD and healthy controls. Some studies differentiate between tonic and phasic EMG activity and use 20-second epochs for tonic and 2-second epochs for phasic,Citation53 whereas others have included any EMG activity but use different methods to analyze EMG activity, either by separating sleep into 30-second and 3-second epochsCitation51 or by distinguishing it from the background EMG activity.Citation54 Although there is consensus that brief bursts of EMG activity and muscle twitches are phasic events, the challenge arises as to how to classify more complex behavioral events, such as a patient with RBD defending himself. It is possible that the difference between tonic and phasic may be more quantitative than qualitative, as suggested by Ramaligam et al, who proposed that the phasic movements are disinhibited in humans with RBD and that RBD results more from failure of the suppression of phasic activity of postural muscles than from dysfunction of tonic control.Citation38 Other studies identified RSWA using the EEG and EOG channels for REM sleep detection, while the abnormally high muscle activity was detected from the EMG channels, and the submental was combined with the left and right anterior tibialis. RSWA was identified by considering it as an outlier problem, in which the number of outliers during REM sleep was used as a quantitative measure of muscle activity.Citation55 There is no consensus in the medical literature about the scoring of EMG activity in iRBD, which suggests that a task-force is needed, especially as studies are beginning to focus on the role of RSWA without subjective complaints of dream-enactment behavior as a subclinical symptom of iRBD.
Is RSWA a marker for RBD?
In 2015, Stefani et al reported results of a follow-up study of subjects with isolated RSWA without dream enactment.Citation56 After a mean of 8.6 years (SD =0.9), one of 14 participating subjects (7.3%) had progressed to RBD. Ten of 14 RSWA subjects (71.4%) were positive for at least one neurodegenerative biomarker. Substantia nigra hyperechogenicity and the presence of mild cognitive impairment (MCI) were both present in four of 14 subjects with isolated RSWA. Electromyographic activity measures increased significantly from baseline to follow-up PSG (any mentalis and both anterior tibialis muscles). The authors concluded that isolated RSWA may be an early biomarker of synuclein-mediated neurodegeneration.
A recent study reported the prevalence of iRBD to be 2.01% and subclinical RBD (ie, patients with isolated RSWA without dream enactment behavior) to be 4.95% in elderly Koreans.Citation57 Whether RSWA without dream enactment is in fact a marker and comparable and as such a potential marker for later neurodegenerative conversion is not resolved and needs additional electrophysiological, clinical, and follow-up studies.
Periodic limb movements in RBD
Few studies have investigated the clinical significance of periodic leg movements of sleep (PLMS) in patients with RBD and the pathological association between these disorders. A high prevalence of PLMS is observed in patients with PD as well as with atypical parkinsonism.Citation58 The occurrence of PLMS has been associated with the dopaminergic system, and the first-line treatment of idiopathic PLMS consists of dopaminergic medications, the same as in PD. In addition, studies with positron emission tomography (PET) and SPECT imaging suggest that sleep abnormalities in PD, including an increased prevalence of PLMS, are indirect manifestations of the primary striatal dopamine deficiency.Citation59 Happe et al reported a negative correlation of PLMS and striatal [123I]β-CIT SPECT binding in patients with PD, which supports the hypothesis that the occurrence of excessive nocturnal movements in PD is dependent on the severity of the presynaptic dopaminergic dysfunction.Citation60 Sasai et al compared iRBD patients with and without PLMS. RSWA/REM was found to be a factor significantly associated with the existence of PLMS during NREM and REM stages, but the duration of RBD morbidity was associated with PLMS only during the REM stage.Citation61 Whether PLMS during REM sleep in iRBD involves the same structures mediating atonia needs to be explored further.
REMs during REM sleep
Electrolytic lesions of the pedunculopontine tegmental nucleus (PPT) reduce the phasic activity of eye movements and other phasic REM features in cats ().Citation62 Although this study did not determine which type of neurotransmitter (cholinergic or glutamatergic) is involved in REMs, it demonstrated that the PPT and surrounding regions contain the generators of REMs.Citation62 A clinical study applying video-oculography in patients with clinically probable RBD showed that ∼24% of these patients have abnormal eye movements compared with only 7% of patients without clinically the condition,Citation63 suggesting brainstem or cerebellar dysfunction. This confirms the results of other studies that analyzed eye movements during REM sleep in iRBD and PD using an automatic algorithm.Citation64
EEG-slowing
Animal studies have implicated the reciprocal projections between the glutamatergic projections of the SLD and the cholinergic projections of the PPN/LDT in initiating REM sleep. It is known that these structures initiate ponto-geniculo-occipital waves, which involve distinct cortical areas (). Several studies have reported that patients with iRBD present with a slowing of the EEG during wakefulness and REM sleep. Fantini et al were the first to analyze the EEG in iRBD by doing a quantitative EEG analysis during wakefulness and REM sleep. In their study, patients with iRBD showed considerably higher theta power in frontal, temporal, and occipital regions, with lower beta power in the occipital region. During REM sleep, the patients with iRBD presented with lower beta power in the occipital regions than in controls, although the sleep architecture was similar in the two groups. They suggested that their results reflect an early sign of impaired cortical activity.Citation65 In a subsequent study, Massicotte-Marquez et al obtained similar results from analyzing EEG recordings during wakefulness in patients with iRBD and controls.Citation66 They reported higher delta and theta power in iRBD during wakefulness in all brain areas compared with controls. These results are in line with imaging studies showing decreased blood flow in the frontal, temporal, and parietal lobes in patients with iRBD.Citation67 Moreover, Iranzo et al evaluated spectral power EEG activity during both wakefulness and REM sleep in iRBD subjects who later developed MCI, a transitional stage between normal cognitive function and dementia.Citation68 They analyzed the right and left hemispheres and found that increased delta and theta activity was more marked in the central than in the occipital region and in the right than in the left hemisphere. Moreover, they observed that patients who went on to develop MCI had more severe EEG-slowing than those patients with iRBD who remained idiopathic. A subsequent study have confirmed the relation between EEG-slowing and the occurrence of MCI.Citation69
The EEG spectral pattern of patients with iRBD, who developed MCI, as well as the cortical hypoperfusion, corresponds to the observations in early stage PD and DLB.Citation70,Citation71 Cortical EEG-slowing and the cognitive impairment occurring in patients with iRBD may be caused by damage of the brainstem structures that regulate REM sleep and activity in the neocortex.
On the other hand, NREM sleep does not seem to be affected. Latreille et al investigated slow wave characteristics in iRBD and controls based on automatic slow wave detection. They measured the slow wave density, amplitude, frequency, slope, and duration of negative and positive phases and found similar results in patients with iRBD and controls. They concluded that the level of synchronization of thalamocortical neurons during NREM sleep was similar in both groups.Citation72
Sleep spindles
Changes have been reported in relation to the microstructure of sleep, especially in relation to sleep spindles. Christensen et al assessed sleep spindles in patients with iRBD, PD patients with RBD, PD patients without RBD, and controls. They measured the density of sleep spindles with an automatic algorithm in REM and NREM sleep, and found that patients with iRBD and PD patients with and without RBD had a markedly lower density of sleep spindles in NREM than did controls.Citation73 They suggested that the lower density in sleep spindles in these patients might involve dysfunction in prethalamic fibers in alpha-synucleinopathies. However, in another study based on manually identified spindles, they found no association in PD patients between spindle density or morphology and disease duration or severity.Citation74
Several studies suggest that sleep spindles and slow waves play a role in brain plasticity and are associated with cognitive function. Latreille et al investigated whether alterations in sleep spindles and slow waves at the baseline visit could predict development of dementia at follow-up in PD.Citation75 They investigated 68 nondemented PD patients and 47 healthy controls with baseline-PSG and comprehensive neuropsychological assessment. Sleep spindles and slow waves were automatically detected during NREM sleep throughout the entire night. At follow-up, an average of 4.5 years later, 18 PD patients had developed dementia and 50 remained dementia free. Sleep spindle density and amplitude were lower in PD patients who converted to dementia compared with the patients who remained dementia free and controls, mostly in posterior cortical regions. Dementia-free PD patients were intermediate between dementia patients and controls, with lower baseline sleep spindle density in all cortical areas compared with controls. Moreover, the authors found that in demented PD patients, lower sleep spindle amplitude in parietal and occipital areas was associated with poorer visuospatial abilities. Although slow wave amplitude was lower in PD patients than in controls, no difference was observed between those who developed or did not develop dementia.
The aforementioned results demonstrate that there are NREM sleep EEG abnormalities in PD patients. Sleep spindle activity was particularly impaired in PD patients who developed dementia, with a more posterior topographic pattern. Sleep spindle alterations are associated with later development of dementia in PD, and thus, may serve as an additional marker of cognitive decline in these patients.
Sleep instability
The SLD is critical for inducing cortical activation and atonia during REM sleep. Although lesions of the SLD induce the RBD-like phenotype in rats, they do not seem to affect REM sleep time and sleep transitions.Citation27 Instead, lesions involving the caudal part of the LDT, which lies dorsal to the SLD, lead to severe sleep fragmentation involving both REM and NREM sleep, and reduction in the amount of REM sleep.Citation27 Sleep-wake fragmentation and reduction in REM sleep have also been reported in mice with lesions of the glutamatergic neurotransmission in this area and after large lesions of the PPT-LDT and SLD in cats.Citation37,Citation76 As the brainstem is affected in the early stages of the PD disease process,Citation77 this may explain the sleep fragmentation seen in this disorder. Christensen et al evaluated sleep characteristics such as sleep stability and sleep transitions in patients with iRBD and PD.Citation78 They determined the transitions and the stability measures based on the manually scored hypnogram as well as by a data-driven method. They found that the patients had less stable REM and NREM sleep, and more REM/NREM transitions than controls, and suggested that these are affected in iRBD and PD.Citation78
Pathophysiologically, sleep fragmentation and abnormalities in sleep architecture in PD might originate from nocturnal motor phenomena, such as increased muscle tone, akinesia or tremor, or drug side-effects. Since iRBD is considered as a premotor stage to alpha-synucleinopathies, these motor phenomena do not occur, and hence, this instability may be explained by the neurodegenerative process itself, which involves the neurochemical systems responsible for sleep organization.
Heart rate variability
Lanfranchi et al studied heart rate variability (HRV) during REM and NREM sleep in ten patients with iRBD and found that differences normally observed between these sleep stages were not present in patients with iRBD, indicating a loss of cardiac autonomic innervation.Citation79 Sorensen et al investigated heart rate response in relation to arousals and leg movements during sleep in eleven patients with iRBD, 14 PD patients with RBD, 16 PD patients without RBD, and 17 controls, and found a significantly lower heart rate response to leg movements, whereby the heart rate response in iRBD was intermediate with respect to the control and the parkinsonian groups.Citation80
Cardiac function in iRBD has also been measured during waking ECG. A study by Valappil et al measured ECG during wakefulness in eleven patients with iRBD and eleven control subjects with idiopathic insomnia without RBD. HRV was determined from 5-minute segments of a single-channel ECG during PSG evaluations, using automatically detected R–R intervals during wakefulness. The authors were able to correctly classify 77.3% of subjects using discriminant analysis featuring the leave-one-out cross-validation method and suggested that HRV measured by routine ECGs could be used to screen for Lewy body disorders such as PD.Citation81 These findings are in agreement with studies showing decreased cardiac autonomic dysfunction by means of MIBG-scanning.
Miyamoto et al used 123I-MIBG cardiac scintigraphy to investigate cardiac sympathetic denervation in patients with iRBD and observed reduced uptake in all 13 patients.Citation82 These changes were also found in patients with PD and DLB,Citation15 adding to the evidence supporting the hypothesis that iRBD is part of a continuum including PD and DLB.
Although cardiac denervation is shown in iRBD and in PD, the course of cardiac denervation over time seems to be heterogeneous and independent of the development of motor symptoms.Citation83,Citation84 Postuma et al analyzed PSG trace measures of beat-to-beat R–R variability in 21 patients with iRBD who developed neurodegenerative disease, including PD (eleven patients), MSA (one patient), and dementia (nine patients). They found that despite clear differences between patients with iRBD and controls, there were none for any measure between those who did or did not develop disease.Citation85
The results from these studies suggest that HRV during both wakefulness and sleep is lower in patients with iRBD compared with control subjects, suggesting abnormalities of sympathetic and parasympathetic functions. Cardiac autonomic dysfunction is also impaired in PD, suggesting that impaired HRV may be an early sign of PD.
Brainstem reflexes
As the pathophysiology of RBD involves dysfunction of brainstem structures, neurophysiological investigation of brainstem reflexes may reveal abnormalities in patients with alpha-synucleinopathies presenting with RBD. The electric blink reflex is a neurophysiological technique measuring brainstem function through a reflex arc involving the fifth to seventh cranial nerves.Citation86 Besides the trigeminofacial reflex arc, this reflex involves the brainstem reticular formation. Several investigations of the blink reflex have been performed in patients with neurodegenerative disorders. In patients with DLB, the electric blink reflex latency is delayed relative to controls, independent of the presence of RBD. The amplitude of the auditory blink reflex has been found to be normal in patients with MSA.Citation87 However, these patients present with an exaggerated startle response based on the other muscles Kofler et al investigated.Citation88 Abnormal startle responses have also been found in other parkinsonian disorders, including DLB.Citation88 A case report of a patient with RBD had concurrent excessive startle response to visual stimuli,Citation89 probably caused by a pontine lesion and subsequent affection of the bulbopontine reticular formation. Other methods have documented the involvement of brainstem. Zoetmulder et al evaluated the use of prepulse inhibitionCitation90,Citation91 and found that the sensorimotor gating, as measured with prepulse inhibition, is markedly reduced in patients with MSA but not in patients with iRBD or PD, suggesting that striatal and brainstem dysfunction is more severely affected in these patients. There are, however, limited data relating to this topic.
Imaging
Functional imaging techniques, such as SPECT and PET, have been used in an attempt to detect abnormal functional alterations in patients with RBD predicting evolution toward the onset of alpha-synucleinopathies. A reduced striatal binding of radioligands, such as 123I-FP-CIT and 11C-DTBZ, has revealed subclinical nigrostriatal dopaminergic degeneration in patients with RBD before the appearance of PD.Citation92–Citation95 Iranzo et alCitation96 reported that in patients with iRBD, serial (123) FP-CIT SPECT shows a decline in striatal tracer uptake that reflects progressive nigrostriatal dopaminergic dysfunction. The mean reduction in striatal (123) FP-CIT uptake from baseline to 3 years was 19.36% in the right putamen, 15.57% in the left putamen, 10.81% in the left caudate, and 7.14% in the right caudate. They suggested that serial (123) FP-CIT SPECT can be used to monitor the progression of nigrostriatal degeneration in iRBD and could be useful in studying the potential disease-modifying compounds in these patients. A 6-[18F]fluoro-L-dopa PET study assessing the rate of disease progression in PD scanning patients twice with a 5-year interval suggested that the disease process first affects the posterior putamen, followed by the anterior putamen and caudate nucleus.Citation97 Brain imaging of iRBD patients with PET showed lower levels of dopamine transporters in the nigrostriatal pathways that further decreased over time until reaching the level when parkinsonism appeared.Citation98 It is not clear to what extent the nigrostriatal dopamine system is directly associated with increased motor activity during REM sleep. A (123) FP-CIT SPECT by Eisensehr et alCitation95 reported that muscle activity during REM sleep lasting persistently longer than 0.5 seconds was independently associated with reduction of striatal dopamine transporters. However, these results could not be reproduced in a subsequent (123) FP-CIT SPECT study by Kim et al,Citation99 which indicates that this topic needs more investigation.
In addition to SPECT and PET scanning, imaging applying combined neuromelanin-sensitive, structural, and diffusion magnetic resonance imaging at 3T in PD patients with and without RBD showed a relationship between damage to the locus subcoeruleus and abnormal muscle tone during REM sleep.Citation100
Imaging with [18F]-fluorodeoxyglucose PET in iRBD revealed a higher metabolic rate in the hippocampus/parahippocampus, cingulate, supplementary motor area, and pons, but a lower rate in the occipital cortex/lingual gyrus.Citation101 This suggests that region-specific metabolic abnormalities exist in patients with RBD and regional metabolic activities are associated with clinical measures such as RBD duration and chin EMG activity. Few studies have investigated the brain regions that are active during RBD.
An investigation applying ictal SPECT with simultaneous PSG recordings showed increased perfusion in the supplementary motor area during a REM sleep behavior episode.Citation102 These findings were confirmed in a subsequent study using ictal SPECT and simultaneous PSG reporting bilateral activation of the premotor (supplementary motor) areas, the interhemispheric cleft, the periaqueductal area, the dorsal and ventral pons, and the anterior lobe of the cerebellum in the four patients examined.Citation103 These studies suggest a common motor pathway in RBD and localize the motor generators responsible for dream enactment behavior to include the supplementary motor pathway bypassing the basal ganglia. These findings confirm a previous study reporting the “normalization” of movements during REM sleep in patients with RBD, which suggests that the movements during RBD could be generated by the motor cortex and would involve the pyramidal tract bypassing the extrapyramidal system.Citation104
Biomarkers
According to Stern, preclinical PD is suspected when genetic, molecular, or imaging biomarkers support the presence of PD-specific pathology, but when no clinical signs and symptoms are yet evident.Citation105 However, identifying PD patients in the preclinical stage is very challenging.Citation3 Premotor PD is defined by the presence of early nonmotor signs and symptoms due to extranigral PD pathology.Citation3,Citation49 On account of this, the challenge is to identify reliable biomarkers to confirm the diagnosis of premotor PD. Several biomarkers have already been identified in the preclinical stage of PD, including RBD, hyposmia, MCI, autonomic dysfunction, and imaging. However, it is still a matter of debate which combination of screening tests is most sensitive to predict conversion from iRBD to PD.
Moreover, there is limited data concerning the identification of molecular markers in RBD. In one study, elevated alpha-synuclein levels in cerebrospinal fluid and serum were suggested to correlate with probable RBD, but the presence of RSWA was not documented by video-PSG. As iRBD is a strong predictor of the later development of an alpha-synucleinopathy, the development of alpha-synuclein ligands used in imaging and the development of drugs antagonizing this protein should receive more focus. There are limited data regarding other neurodegenerative biomarkers, eg, Tau protein (t-Tau), phosphorylated Tau (p-Tau181) protein, α-synuclein, neurofilament light, and chitinase-3-like protein-1, also known as YKL-40. The inflammatory marker YKL-40 has been found to be lower in PD and atypical PD,Citation106,Citation107 whereas other studies have only found elevated levels in AD but not PD.Citation108 RSWA/RBD is strongly associated with hypocretin-deficient narcolepsy type 1,Citation7 but in nonnarcoleptic RBD and in LBD, hypocretin levels were found to be normal.Citation109,Citation110 However, this does not imply that the hypocretin system is not involved in the neurodegenerative process as a lower frequency of neurons has been identified in PD patients;Citation111,Citation112 the cerebrospinal fluid (CSF)-hcrt-1 level reflects the general cerebrospinal level, and it is likely that the CSF concentration may be normal or subnormal, despite the significant loss of hypothalamic hypocretinergic neurons.
Treatment of RBD episodes
The medical literature on the treatment of RBD reflects a lack of randomized, double-blind controlled trials. Clonazepam and melatonin have been the most commonly used drugs for the nocturnal treatment of RBD. The use of these drugs is justified on the basis of small case series,Citation113 and a small controlled trial has been conducted only for melatonin,Citation114 in which only a limited effect was proved. Studies have most frequently focused on clonazepam. However, side effects may limit the use of clonazepam, especially in elderly and demented patients.Citation113 A single case report has been presented regarding the positive effect of hypnotics and sodium oxybate,Citation115,Citation116 but its findings are very limited. In addition, there is little information about the efficacy of medication for RBD in narcolepsy type 1. We also know little about other drugs.
The effect of antidepressants (SSRI, TCA) and sodium oxybate on RBD varies from positive to negative,Citation117 although the evidence is limited. As depression is associated with RBD, it is a strong confounder. Future studies need to address the effect of medications on outcome measures such as the improvement of the PSG features of RBD including RSWA, improvement of the quality of sleep, and prevention of injury.
In PD, a number of pathways and mechanisms have been the target for pharmacological intervention, including mitochondrial dysfunction, oxidative stress, inflammation, protein handling, and prion-like processes.Citation118 However, none of these interventions appear to be effective in delaying the disease process in PD.Citation119 Therefore, increased understanding about the pathophysiological mechanism in both iRBD and PD is necessary to be able to develop effective treatment regimens. As follow-up studies have convincingly shown that iRBD is a strong marker for later development of an alpha-synucleinopathy, patients with iRBD may be enrolled in future neuroprotective pharmacological studies.
Physical activity, physiotherapy, and social activities have been shown to modify the symptoms of PD.Citation120–Citation122 However, there are currently no controlled studies investigating the potential effect of these activities in reducing the conversion rate from iRBD to PD. Therefore, these treatment options are not considered in the management of RBD at present.
Discussion
The current identification of sleep-related abnormalities and the possible relation to neurodegenerative disorders raises a significant number of research questions. One of the most important issues is that the current studies identifying RBD as a risk factor for later parkinsonian conversion are based on identifying and defining the population at risk. The current studies have identified patients in high-level neurological sleep clinics. It has still not been settled whether this may influence the potential effect on the conversion, eg, if patients identified in broader clinical settings with simpler methods influence the diagnostic pattern and prognosis. The presence of other factors, eg, medication, alcohol, and comorbidities, may also influence the risk association.
Although there are currently no drugs available to prevent or delay the disease process for parkinsonian conversion, any sensitive and specific biological markers would be important in the future for identifying high-risk individuals with the aim of managing the risk. Owing to the complex mechanism of wake–sleep regulation, knowledge of these mechanisms and abnormalities is central to our understanding of the progressive nature of alpha-synucleinopathies. Owing to the early involvement and specific physiological pattern, identification of RBD and probably RSWA is crucial for the development and identification of biomarkers and potential development of disease-modifying medication and interventions.
A number of other symptoms and methods have been identified in RBD/PD, including imaging techniques, testing for olfactory and autonomic abnormalities, molecular techniques, and other sleep measures. It is likely that combinations of such approaches may enable patients to be stratified into specific risk associations that are of use in risk management.
One of the major challenges in defining those at risk is the potential relation between RBD (as defined by video-confirmed evaluation of REM sleep-associated behavior and the presence of simultaneous RSWA) and minor episodes of muscle activity and RSWA. Recently, it was suggested that these minor episodes be identified as REM behavior events.Citation123 Questionnaires’ information may show up intra- and inter-individual variations.Citation124 Current prospective studies and most of the comorbidity studies rely on the classic definition of video-confirmed RBD. The extent to which dream content influences the diagnostic value of RBD is not known, but it may reflect the extent of pathology in the brainstem. Recent studies of day-to-day variation suggest that not only sleep patterns but also motor activity varies between the recorded days. NREM motor phenomena in patients with RBD are not taken into consideration,Citation125 and in many patients with advanced neurodegenerative diseases, the EEG shows major abnormalities, with slowing, pathological microevents (eg, K-complexes, sleep spindles). As a consequence, sleep scoring is often difficult and subject to significant interscorer variability.Citation126
PD, DLB, and MSA are complex neurodegenerative disorders, and their progress, severity, and symptom profile vary greatly between patients. It is not fully established whether iRBD is a precursor of only one PD subgroup. In analyzing iRBD patients with the aim of identifying those at the highest risk of developing PD, it might be unrealistic to expect that a single biomarker will be sufficient. By combining multiple biomarkers, the sensitivity of identifying a person with preclinical PD will increase, due to the fact that more aspects of this complex disease will be revealed. Optimally, a combination of biomarkers expressing alterations in different areas or mechanisms of the brain would indicate the stage of the disease and the pace and direction in which it is progressing. This would not only help identify the patients at the highest risk of developing PD, and thereby possibly facilitate PD treatment before PD diagnosis, but also provide insight into treatment efficiency and thereby help personalized treatment.
We believe that several additional research questions need to be addressed in order to understand brainstem involvement and the associated physiological, imaging, and molecular findings. This is fundamental to our understanding of how to identify high-risk individuals and to the development of risk-reducing agents, including protective medication, for these devastating diseases.
Author contributions
PJ conceived the study, and all authors (PJ, JAEC, and MZ) contributed substantially to the article. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
There was no funding for this study.
Disclosure
The authors declare no conflicts of interest in this work and have no further financial disclosures.
References
- JouvetMParadoxical sleep – a study of its nature and mechanismsProg Brain Res196518206214329040
- SchenckCHBundlieSREttingerMGMahowaldMWChronic behavioral disorders of human REM sleep: a new category of parasomniaSleep198692933083505730
- SchenckCHMontplaisirJYFrauscherBRapid eye movement sleep behavior disorder: devising controlled active treatment studies for symptomatic and neuroprotective therapy – a consensus statement from the International Rapid Eye Movement Sleep Behavior Disorder Study GroupSleep Med20131479580623886593
- SforzaEZucconiMPetronelliRLugaresiECirignottaFREM sleep behavioral disordersEur Neurol1988282953003224627
- BrooksPLPeeverJHImpaired GABA and glycine transmission triggers cardinal features of rapid eye movement sleep behavior disorder in miceJ Neurosci2011317111712121562273
- MattarozziKBellucciCCampiCClinical, behavioural and polysomnographic correlates of cataplexy in patients with narcolepsy/cataplexySleep Med2008942543317681883
- KnudsenSGammeltoftSJennumPJRapid eye movement sleep behaviour disorder in patients with narcolepsy is associated with hypocretin-1 deficiencyBrain201013356857920129934
- SchenckCHBoeveBFMahowaldMWDelayed emergence of a parkinsonian disorder or dementia in 81% of older males initially diagnosed with idiopathic REM sleep behavior disorder (RBD): 16 year update on a previously reported seriesSleep Med201314874474823347909
- IranzoAFernández-ArcosATolosaENeurodegenerative disorder risk in idiopathic REM sleep behavior disorder: study in 174 patientsPLoS One20149e8974124587002
- PostumaRBGagnonJFVendetteMFantiniMLMassicotte-MarquezJMontplaisirJQuantifying the risk of neurodegenerative disease in idiopathic REM sleep behavior disorderNeurology2009721296130019109537
- SchenckCHBundlieSRMahowaldMWDelayed emergence of a parkinsonian disorder in 38% of 29 older men initially diagnosed with idiopathic rapid eye movement sleep behaviour disorderNeurology1996463883938614500
- TerzaghiMZucchellaCRustioniVSinforianiEManniRCognitive performances and mild cognitive impairment in idiopathic rapid eye movement sleep behavior disorder: results of a longitudinal follow-up studySleep2013361527153224082312
- SorensenGLMehlsenJJennumPReduced sympathetic activity in idiopathic rapid-eye-movement sleep behavior disorder and Parkinson’s diseaseAuton Neurosci201317913814124021939
- KashiharaKImamuraTShinyaTCardiac 123I-MIBG uptake is reduced more markedly in patients with REM sleep behavior disorder than in those with early stage Parkinson’s diseaseParkinsonism Relat Disord20101625225520097595
- MiyamotoTMiyamotoMSuzukiKNishibayashiMIwanamiMHirataK123I-MIBG cardiac scintigraphy provides clues to the underlying neurodegenerative disorder in idiopathic REM sleep behavior disorderSleep20083171772318517041
- UngerMMMöllerJCMankelKPatients with idiopathic rapid-eye-movement sleep behavior disorder show normal gastric motility assessed by the 13C-octanoate breath testMov Disord2011262559256322147682
- PetitDGagnonJFFantiniMLFerini-StrambiLMontplaisirJSleep and quantitative EEG in neurodegenerative disordersJ Psychosom Res20045648749615172204
- PostumaRBGagnonJFMontplaisirJClinical prediction of Parkinson’s disease: planning for the age of neuroprotectionJ Neurol Neurosurg Psychiatry2010811008101320562452
- RossGWAbbottRDPetrovitchHTannerCMWhiteLRPre-motor features of Parkinson’s disease: the Honolulu-Asia Aging Study experienceParkinsonism Relat Disord201218suppl 1S199S20222166434
- NoyceAJBestwickJPSilveira-MoriyamaLPREDICT-PD: identifying risk of Parkinson’s disease in the community: methods and baseline resultsJ Neurol Neurosurg Psychiatry201485313723828833
- SaperCBFullerPMPedersenNPLuJScammellTESleep state switchingNeuron2010681023104221172606
- IberCThe American Academy Sleep Medicine Manual for the Scoring of Sleep and Associated EventsWestchester, ILAmerican Academy of Sleep Medicine2007
- LuppiPHClementOFortPParadoxical (REM) sleep genesis by the brainstem is under hypothalamic controlCurr Opin Neurobiol201323578679223490549
- SaperCBThe neurobiology of sleepContinuum (Minneap Minn)201319193123385692
- SapinELaprayDBérodALocalization of the brainstem GABAergic neurons controlling paradoxical (REM) sleepPLoS One20094e427219169414
- VerretLLegerLFortPLuppiPHCholinergic and noncholinergic brainstem neurons expressing Fos after paradoxical (REM) sleep deprivation and recoveryEur J Neurosci2005212488250415932606
- LuJShermanDDevorMSaperCBA putative flip-flop switch for control of REM sleepNature200644158959416688184
- SastreJPBudaCKitahamaKJouvetMImportance of the ventrolateral region of the periaqueductal gray and adjacent tegmentum in the control of paradoxical sleep as studied by muscimol microinjections in the catNeuroscience1996744154268865193
- CrochetSOnoeHSakaiKA potent non-monoaminergic paradoxical sleep inhibitory system: a reverse microdialysis and single-unit recording studyEur J Neurosci2006241404141216987225
- VerretLFortPGervasoniDLégerLLuppiPHLocalization of the neurons active during paradoxical (REM) sleep and projecting to the locus coeruleus noradrenergic neurons in the ratJ Comp Neurol200649557358616498678
- BoissardRGervasoniDSchmidtMHBarbagliBFortPLuppiPHThe rat ponto-medullary network responsible for paradoxical sleep onset and maintenance: a combined microinjection and functional neuroanatomical studyEur J Neurosci2002161959197312453060
- ClementOSapinEBerodAFortPLuppiPHEvidence that neurons of the sublaterodorsal tegmental nucleus triggering paradoxical (REM) sleep are glutamatergicSleep20113441942321461384
- SiegelJMThe neurobiology of sleepSemin Neurol20092927729619742406
- LaiYYSiegelJMPontomedullary glutamate receptors mediating locomotion and muscle tone suppressionJ Neurosci199111293129371679125
- MileykovskiyBYKiyashchenkoLIKodamaTLaiYYSiegelJMActivation of pontine and medullary motor inhibitory regions reduces discharge in neurons located in the locus coeruleus and the anatomical equivalent of the midbrain locomotor regionJ Neurosci2000208551855811069963
- LuppiPHGervasoniDBoissardRBrainstem structures responsible for paradoxical sleep onset and maintenanceArch Ital Biol200414239741115493544
- KrenzerMAnacletCVetrivelanRBrainstem and spinal cord circuitry regulating REM sleep and muscle atoniaPLoS One20116e2499822043278
- RamaligamVChenMCSaperCBLuJPerspectives on the rapid eye movement sleep switch in rapid eye movement sleep behavior disorderSleep Med20131470771323768838
- VetrivelanRFullerPMTongQLuJMedullary circuitry regulating rapid eye movement sleep and motor atoniaJ Neurosci2009299361936919625526
- WebsterHHFriedmanLJonesBEModification of paradoxical sleep following transections of the reticular formation at the pontomedullary junctionSleep198691233961365
- AnacletCPedersenNPFullerPMLuJBrainstem circuitry regulating phasic activation of trigeminal motoneurons during REM sleepPLoS One20105e878820098748
- LaiYYHsiehKCNguyenDPeeverJSiegelJMNeurotoxic lesions at the ventral mesopontine junction change sleep time and muscle activity during sleep: an animal model of motor disorders in sleepNeuroscience200815443144318487021
- VetrivelanRChangCLuJMuscle tone regulation during REM sleep: neural circuitry and clinical significanceArch Ital Biol201114934836622205588
- HassaniOKHennyPLeeMGJonesBEGABAergic neurons intermingled with orexin and MCH neurons in the lateral hypothalamus discharge maximally during sleepEur J Neurosci20103244845720597977
- MileykovskiyBYKiyashchenkoLISiegelJMMuscle tone facilitation and inhibition after orexin-a (hypocretin-1) microinjections into the medial medullaJ Neurophysiol2002872480248911976385
- BraakHDel TrediciKRübUde VosRAJansen SteurENBraakEStaging of brain pathology related to sporadic Parkinson’s diseaseNeurobiol Aging2003Mar-Apr24219721112498954
- BoeveBFSilberMHFermanTJClinicopathologic correlations in 172 cases of rapid eye movement sleep behavior disorder with or without a coexisting neurologic disorderSleep Med20131475476223474058
- BoeveBFREM sleep behavior disorder: updated review of the core features, the REM sleep behavior disorder-neurodegenerative disease association, evolving concepts, controversies, and future directionsAnn N Y Acad Sci20101184155420146689
- BoeveBFPredicting the future in idiopathic rapid-eye movement sleep behaviour disorderLancet Neurol201091040104220869916
- LapierreOMontplaisirJPolysomnographic features of REM sleep behavior disorder: development of a scoring methodNeurology199242137113741620348
- FrauscherBIranzoAGaigCNormative EMG values during REM sleep for the diagnosis of REM sleep behavior disorderSleep20123583584722654203
- FerriRManconiMPlazziGA quantitative statistical analysis of the submentalis muscle EMG amplitude during sleep in normal controls and patients with REM sleep behavior disorderJ Sleep Res2008178910018275559
- MontplaisirJGagnonJFFantiniMLPolysomnographic diagnosis of idiopathic REM sleep behavior disorderMov Disord2010252044205120818653
- FrandsenRNikolicMZoetmulderMKempfnerLJennumPAnalysis of automated quantification of motor activity in REM sleep behaviour disorderJ Sleep Res201524558359025923472
- KempfnerJSorensenGLNikolicMFrandsenRSorensenHBJennumPRapid eye movement sleep behavior disorder as an outlier detection problemJ Clin Neurophysiol201431869324492451
- StefaniAGabeliaDHöglBLong-term follow-up investigation of isolated rapid eye movement sleep without atonia without rapid eye movement sleep behavior disorder: a pilot studyJ Clin Sleep Med201511111273127926156949
- KangSHYoonIYLeeSDHanJWKimTHKimKWREM sleep behavior disorder in the Korean elderly population: prevalence and clinical characteristicsSleep2013361147115223904674
- TerzaghiMArnaldiDRizzettiMCAnalysis of video-polysomnographic sleep findings in dementia with Lewy bodiesMov Disord2013281416142323744574
- HilkerRBurghausLRazaiNJacobsAHSzeliesBHeissWDFunctional brain imaging in combined motor and sleep disordersJ Neurol Sci200624822322616753181
- HappeSPirkerWKloschGSauterCZeitlhoferJPeriodic leg movements in patients with Parkinson’s disease are associated with reduced striatal dopamine transporter bindingJ Neurol2003250838612527997
- SasaiTInoueYMatsuuraMClinical significance of periodic leg movements during sleep in rapid eye movement sleep behavior disorderJ Neurol20112581971197821509428
- ShouseMNSiegelJMPontine regulation of REM sleep components in cats: integrity of the pedunculopontine tegmentum (PPT) is important for phasic events but unnecessary for atonia during REM sleepBrain Res199257150631611494
- KimYEYangHJYunJYKimHJLeeJYJeonBSREM sleep behavior disorder in Parkinson disease: association with abnormal ocular motor findingsParkinsonism Relat Disord20142044444624495707
- ChristensenJAKochHFrandsenRClassification of iRBD and Parkinson’s disease patients based on eye movements during sleepConf Proc IEEE Eng Med Biol Soc2013201344144424109718
- FantiniMLGagnonJFPetitDSlowing of electroencephalogram in rapid eye movement sleep behavior disorderAnn Neurol20035377478012783424
- Massicotte-MarquezJCarrierJDécaryASlow-wave sleep and delta power in rapid eye movement sleep behavior disorderAnn Neurol20055727728215668971
- HanyuHInoueYSakuraiHRegional cerebral blood flow changes in patients with idiopathic REM sleep behavior disorderEur J Neurol20111878478821143707
- IranzoAIsettaVMolinuevoJLElectroencephalographic slowing heralds mild cognitive impairment in idiopathic REM sleep behavior disorderSleep Med20101153453920462792
- SasaiTMatsuuraMInoueYElectroencephalographic findings related with mild cognitive impairment in idiopathic rapid eye movement sleep behavior disorderSleep2013361893189924293764
- BonanniLThomasATiraboschiPPerfettiBVaraneseSOnofrjMEEG comparisons in early Alzheimer’s disease, dementia with Lewy bodies and Parkinson’s disease with dementia patients with a 2-year follow-upBrain200813169070518202105
- MoritaAKameiSMizutaniTRelationship between slowing of the EEG and cognitive impairment in Parkinson diseaseJ Clin Neurophysiol20112838438721811128
- LatreilleVCarrierJMontplaisirJLafortuneMGagnonJFNon-rapid eye movement sleep characteristics in idiopathic REM sleep behavior disorderJ Neurol Sci201131015916221714973
- ChristensenJAKempfnerJZoetmulderMDecreased sleep spindle density in patients with idiopathic REM sleep behavior disorder and patients with Parkinson’s diseaseClin Neurophysiol201412551251924125856
- ChristensenJANikolicMWarbySCSleep spindle alterations in patients with Parkinson’s diseaseFront Hum Neurosci2015923325983685
- LatreilleVCarrierJLafortuneMSleep spindles in Parkinson’s disease may predict the development of dementiaNeurobiol Aging2015361083109025442116
- WebsterHHJonesBENeurotoxic lesions of the dorsolateral pontomesencephalic tegmentum-cholinergic cell area in the cat. II Effects upon sleep-waking statesBrain Res19884582853022905197
- BraakHDel TrediciKRübUde VosRAJansen SteurENBraakEStaging of brain pathology related to sporadic Parkinson’s diseaseNeurobiol Aging20032419721112498954
- ChristensenJAJennumPKochHSleep stability and transitions in patients with idiopathic REM sleep behavior disorder and patients with Parkinson’s diseaseClin Neurophysiol2015127153754325843013
- LanfranchiPAFradetteLGagnonJFColomboRMontplaisirJCardiac autonomic regulation during sleep in idiopathic REM sleep behavior disorderSleep2007301019102517702272
- SorensenGLKempfnerJZoetmulderMSorensenHBJennumPAttenuated heart rate response in REM sleep behavior disorder and Parkinson’s diseaseMov Disord20122788889422555939
- ValappilRABlackJEBroderickMJExploring the electrocardiogram as a potential tool to screen for premotor Parkinson’s diseaseMov Disord2010252296230320976736
- MiyamotoTMiyamotoMInoueYUsuiYSuzukiKHirataKReduced cardiac 123I-MIBG scintigraphy in idiopathic REM sleep behavior disorderNeurology2006672236223817190953
- MiyamotoTMiyamotoMIwanamiMHirataKFollow-up study of cardiac 123 I-MIBG scintigraphy in idiopathic REM sleep behavior disorderEur J Neurol2011181275127821914050
- OguriTTachibanaNMitakeSKawanishiTFukuyamaHDecrease in myocardial 123I-MIBG radioactivity in REM sleep behavior disorder: two patients with different clinical progressionSleep Med2008958358517921052
- PostumaRBLanfranchiPABlaisHGagnonJFMontplaisirJYCardiac autonomic dysfunction in idiopathic REM sleep behavior disorderMov Disord2010252304231020669316
- BassoMAEvingerCAn explanation for reflex blink hyperexcitability in Parkinson’s disease. II Nucleus raphe magnusJ Neurosci199616731873308929438
- ValldeoriolaFValls-SoléJTolosaENobbeFAMuñozJEMartíJThe acoustic startle response is normal in patients with multiple system atrophyMov Disord1997126977009380050
- KoflerMMüllerJWenningGKThe auditory startle reaction in parkinsonian disordersMov Disord200116627111215594
- PeterAHansenMLMerklAVoigtländerSBajboujMDanker-HopfeHREM sleep behavior disorder and excessive startle reaction to visual stimuli in a patient with pontine lesionsSleep Med2008969770018060836
- ZoetmulderMBiernatHBNikolicMKorboLFribergLJennumPJPrepulse inhibition is associated with attention, processing speed, and 123I-FP-CIT SPECT in Parkinson’s diseaseJ Parkinsons Dis20144778724366928
- ZoetmulderMBiernatHBNikolicMKorboLJennumPJSensorimotor gating deficits in multiple system atrophy: comparison with Parkinson’s disease and idiopathic REM sleep behavior disorderParkinsonism Relat Disord20142029730224355363
- AlbinRLKoeppeRAChervinRDDecreased striatal dopaminergic innervation in REM sleep behavior disorderNeurology2000551410141211087796
- IranzoAValldeoriolaFLomeñaFSerial dopamine transporter imaging of nigrostriatal function in patients with idiopathic rapid-eye-movement sleep behaviour disorder: a prospective studyLancet Neurol20111079780521802993
- MiyamotoMMiyamotoTNeuroimaging of rapid eye movement sleep behavior disorder: transcranial ultrasound, single-photon emission computed tomography, and positron emission tomography scan dataSleep Med20131473974323648146
- EisensehrILinkeRNoachtarSSchwarzJGildehausFJTatschKReduced striatal dopamine transporters in idiopathic rapid eye movement sleep behaviour disorder. Comparison with Parkinson’s disease and controlsBrain2000123pt 61155116010825354
- IranzoAValldeoriolaFLomeñaFSerial dopamine transporter imaging of nigrostriatal function in patients with idiopathic rapid-eye-movement sleep behaviour disorder: a prospective studyLancet Neurol2011910979780521802993
- NurmiERuottinenHMBergmanJRate of progression in Parkinson’s disease: a 6-[18F]fluoro-L-dopa PET studyMov Disord20011660861511481683
- MiyamotoTOrimoSMiyamotoMFollow-up PET studies in case of idiopathic REM sleep behavior disorderSleep Med20101110010119592301
- KimYKYoonIYKimJMThe implication of nigrostriatal dopaminergic degeneration in the pathogenesis of REM sleep behavior disorderEur J Neurol20101748749219968708
- García-LorenzoDLongo-Dos SantosCEwenczykCThe coeruleus/subcoeruleus complex in rapid eye movement sleep behaviour disorders in Parkinson’s diseaseBrain20131362120212923801736
- GeJWuPPengSAssessing cerebral glucose metabolism in patients with idiopathic rapid eye movement sleep behavior disorderJ Cereb Blood Flow Metab201535122062206926219593
- DauvilliersYBoudousqVLopezRIncreased perfusion in supplementary motor area during a REM sleep behaviour episodeSleep Med20111253153221489868
- MayerGBitterlichMKuwertTRittPStefanHIctal SPECT in patients with rapid eye movement sleep behaviour disorderBrain20151381263127025732183
- De CockVCVidailhetMLeuSRestoration of normal motor control in Parkinson’s disease during REM sleepBrain200713045045617235126
- SternMBThe preclinical detection of Parkinson’s disease: ready for prime time?Ann Neurol20045616917115293267
- OlssonBConstantinescuRHolmbergBAndreasenNBlennowKZetterbergHThe glial marker YKL-40 is decreased in synucleinopathiesMov Disord2013281882188523847144
- MagdalinouNKPatersonRWSchottJMA panel of nine cerebrospinal fluid biomarkers may identify patients with atypical parkinsonian syndromesJ Neurol Neurosurg Psychiatry2015861240124725589779
- WennströmMSurovaYHallSThe inflammatory marker YKL-40 is elevated in cerebrospinal fluid from patients with Alzheimer’s but not Parkinson’s disease or dementia with Lewy bodiesPLoS One201510e013545826270969
- AndersonKNVincentASmithIEShneersonJMCerebrospinal fluid hypocretin levels are normal in idiopathic REM sleep behaviour disorderEur J Neurol2010171105110720113337
- BaumannCRDauvilliersYMignotEBassettiCLNormal CSF hypocretin-1 (orexin A) levels in dementia with Lewy bodies associated with excessive daytime sleepinessEur Neurol200452737615256827
- ThannickalTCLaiYYSiegelJMHypocretin (orexin) cell loss in Parkinson’s diseaseBrain20071301586159517491094
- FronczekROvereemSLeeSYHypocretin (orexin) loss in Parkinson’s diseaseBrain20071301577158517470494
- AuroraRNZakRSMagantiRKStandards of Practice CommitteeAmerican Academy of Sleep MedicineBest practice guide for the treatment of REM sleep behavior disorder (RBD)J Clin Sleep Med20106859520191945
- KunzDMahlbergRA two-part, double-blind, placebo-controlled trial of exogenous melatonin in REM sleep behaviour disorderJ Sleep Res20101959159620561180
- AndersonKNShneersonJMDrug treatment of REM sleep behavior disorder: the use of drug therapies other than clonazepamJ Clin Sleep Med2009523523919960644
- ShneersonJMSuccessful treatment of REM sleep behavior disorder with sodium oxybateClin Neuropharmacol20093215815919483483
- OnofrjMLucianoALThomasAIaconoDD’AndreamatteoGMirtazapine induces REM sleep behavior disorder (RBD) in parkinsonismNeurology20036011311512525729
- SchapiraAHOlanowCWGreenamyreJTBezardESlowing of neurodegeneration in Parkinson’s disease and Huntington’s disease: future therapeutic perspectivesLancet201438454555524954676
- HenchcliffeCSevertWLDisease modification in Parkinson’s diseaseDrugs Aging20112860561521812497
- CruickshankTMReyesARZimanMRA systematic review and meta-analysis of strength training in individuals with multiple sclerosis or Parkinson diseaseMedicine (Baltimore)201594e41125634170
- TomlinsonCLHerdCPClarkeCEPhysiotherapy for Parkinson’s disease: a comparison of techniquesCochrane Database Syst Rev20146CD00281524936965
- ShanahanJMorrisMEBhriainONSaundersJCliffordAMDance for people with Parkinson disease: what is the evidence telling us?Arch Phys Med Rehabil20159614115325223491
- Sixel-DoringFTrautmannEMollenhauerBTrenkwalderCRapid eye movement sleep behavioral events: a new marker for neurodegeneration in early Parkinson disease?Sleep20143743143824587564
- Sixel-DoringFSchweitzerMMollenhauerBTrenkwalderCIntraindividual variability of REM sleep behavior disorder in Parkinson’s disease: a comparative assessment using a new REM sleep behavior disorder severity scale (RBDSS) for clinical routineJ Clin Sleep Med20117758021344049
- MayerGKesperKPlochTQuantification of tonic and phasic muscle activity in REM sleep behavior disorderJ Clin Neurophysiol200825485518303560
- JensenPSSorensenHBLeonthinHLJennumPAutomatic sleep scoring in normals and in individuals with neurodegenerative disorders according to new international sleep scoring criteriaJ Clin Neurophysiol20102729630220634706
