Abstract
Background
Out-of-hospital cardiac arrest is the main issue for pre-hospital emergency care. There are several airway managements during the out-of-hospital cardiopulmonary resuscitation (CPR) such as endotracheal intubation (ETI) or alternative airway device: bag-valve mask (BVM). Data comparing both methods showed inconclusive results on survival and limited results on CPR outcome. This study aimed to add additional results on comparing the ETI and BVM in cardiac arrest outside hospitals; focused on the CPR outcome.
Methods
This study was a retrospective, analytical study. The inclusion criteria were adult patients (age of 18 years or over) with out-of-hospital cardiac arrest, who received emergency life support, and received either BVM or ETI. Data were retrieved from the Information Technology of Emergency Medical Service. The outcome was a return of spontaneous circulation (ROSC).
Results
During the study period, there were 1070 patients with out-of-hospital cardiac arrest who met the study criteria. Of those, 800 patients (74.77%) received BVM, while the other 270 patients (25.23%) received ETI. There were five significant factors between both groups including mean distance to scene, proportions of response time less than 8 mins, defibrillation, intravenous fluid administration, and adrenaline administration. There was no significant difference on the outcome: ROSC. The BVM group had slightly higher rate of ROSC than the ETI group (19.63% vs 15.56%; p value 0.148).
Conclusion
The BVM and ETI had comparable ROSC rate for out-of-hospital cardiac arrest victims. However, the study population of the BVM group had less severe conditions and received faster treatment than the ETI group.
Introduction
Cardiac arrest is an emergency condition and required prompt cardiopulmonary resuscitation (CPR). Out-of-hospital cardiac arrest is the main issue for pre-hospital emergency care. In the US, there were over 350,000 patients with cardiac arrest outside the hospitals.Citation1 The survival rate was below 10% for the cardiac arrest victim outside the hospitals.Citation2 The emergency medical service is primarily responder for out-of-hospital cardiac arrest care to perform the CPR. Airway management is one crucial step during the CPR and hospital transfer.
There are several airway managements during the out-of-hospital CPR such as endotracheal intubation (ETI) or alternative airway device: bag-valve mask (BVM).Citation3 The ETI is the standard procedure but it may require more skill and take more time to be successful. On the other hand, the BVM has several benefits including low complications or no interruption of cardiac massage.Citation4 There are several studies comparing the ETI with the BVM in out-of-hospital cardiac arrest victims. However, the results are still debating. In non-traumatic out-of-hospital cardiac arrest, the BVM had higher survival rate than the ETI (27% vs 15%) giving an adjusted odds ratio of 4.5 (95% CI of 2.3–8.9; p value < 0.0001).Citation5 A nationwide study from Korea showed different results.Citation6 The ETI had better survival rate compared with the BVM with adjusted odds ratio of 1.405 (95% CI of 1.001–1.971). After using a propensity score analysis, there were comparable survival rates between the ETI and BVM on the Korean database study.Citation3 Therefore, this study aimed to add additional results on comparing the ETI and BVM in cardiac arrest outside hospitals; focused on the CPR outcome. Additionally, the preference of ETI in this setting was evaluated.
Methods
This study was a retrospective, analytical study. The inclusion criteria were adult patients (age of 18 years or over) with out-of-hospital cardiac arrest, received emergency life support, and received either BVM or ETI. Pregnant women, patient’s relative refused advanced resuscitation at the scene, or those with incomplete data were excluded. Data were retrieved from the Information Technology of Emergency Medical Service (ITEMS). The study period was between November 2016 and October 2017. The study protocol was approved by institutional review board, Faculty of Medicine, Ramathibodi Hospital Mahidol University, Thailand (MURA2018/705).
The EMS in Thailand is set by the catchment area of the hospitals or EMS services by certified private sectors. The phone number to activate the EMS system is 1669. When the system is activated, the nearest EMS team comprised of certified EMS personnel is active. The record form includes gender, age, the response time, on scene time (minutes), distance from the scene, defibrillation, fluid therapy, adrenaline administration, and cause of cardiac arrest. Cardiac arrest was confirmed by ECG and causes of cardiac arrest was a presumptive diagnosis into three categories by the CPR team: internal medicine, surgery, or accident. The outcome was a return of spontaneous circulation (ROSC) at the scene or the transferred hospitals. Details of all events are submitted to the ITEMS. This study retrospectively searched the ITEMS database by using the code of cardiac arrest. The code used for cardiac arrest is RED1. Those who met with the inclusion criteria were enrolled. Clinical baseline characteristics, treatments, and outcome were recorded. Data were categorized by either BVM or ETI.
Sample Size Calculation
A pilot study compared the ROSC between out-of-hospital cardiac arrest patients who received BVM or ETI in October 2016. The ITEMS database was retrieved and recorded clinical data of eligible patients. There were 69 patients who received either BVM or ETI with a BVM: ETI ratio of 3:1. The ROSC rate in BVM and ETI group was 23% and 36%. By comparing two proportions, the required sample size for BVM and ETI group was 800 and 270 patients. These calculations were based on an alpha of 95% (one sided) and power of 90%.
Statistical Analyses
Clinical data were calculated by descriptive statistics and reported as mean ± SD for numerical data or number (percentage) for categorical data. Clinical data and outcome were compared between the BVM and ETI group. Student’s t-test or Wilcoxon rank sum test was used to compare the numerical data between both groups where appropriate, while Chi-square test or Fisher Exact test was used to compare categorical data between both groups where appropriate. Significant factors were defined if a p value was less than 0.05. Factors associated with ETI were executed by univariate and multivariate logistic regression analysis. The final model for ETI was tested for goodness of fit by the Hosmer–Lemeshow method. The goodness of fit was appropriate if the p value of the model was over 0.05. All statistical analyses were computed by the STATA software, version 10.1 (College Station, Texas, USA).
Results
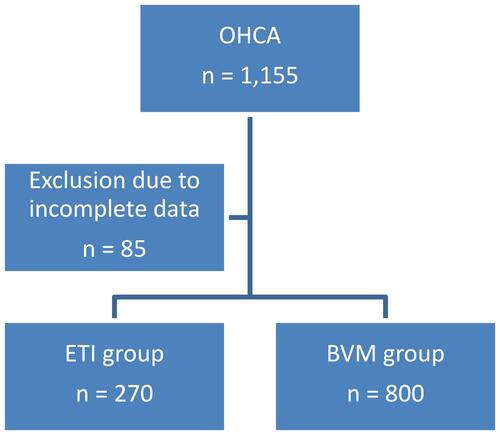
During the study period, there were 1155 patients with out-of-hospital cardiac arrest (). Of those, 85 patients were excluded due to incomplete data. In total, there were 1070 patients who included in the analysis: 800 patients (74.77%) received BVM, the other 270 patients (25.23%) received ETI. There were five significant factors between both groups including mean distance to scene and proportions of response time less than 8 mins, defibrillation, intravenous fluid administration, and adrenaline administration (). There was no significant difference on the outcome: ROSC. The BVM group had slightly higher rate of ROSC than the ETI group (19.63% vs 15.56%; p value 0.148).
Table 1 Baseline Characteristics, and Treatments Between the Bag-Valve Mask (BVM) and Endotracheal Intubation (ETI) Group
Figure 1 Study flow for patients with out-of-hospital cardiac arrest (OHCA) who received either bag-valve mask (BVM) or endotracheal intubation (ETI).
Factors associated with preference for ETI are shown in . There were three independent factors for ETI prediction including intravenous access, adrenaline administration, and defibrillation. The adjusted odds ratio (95% CI) of these factors was 3.373 (1.193, 9.531), 2.259 (1.684, 3.030), and 3.638 (1.171, 11.295), respectively. The Hosmer–Lemeshow Chi square for the final model was 7.74 (p value 0.4591).
Table 2 Factors Associated with Endotracheal Intubation in Patients with Out-of-Hospital Cardiac Arrest
Discussion
Several study evaluated the survival rate of out-of-hospital cardiac arrest between the ETI and BVM.Citation3–Citation6 There are inconclusive data on this issue. This current study found that both ETI and BVM were comparable in terms of ROSC (15.56% vs 19.63%; p value 0.148). There were at least two previous studies compared the ROSC rate between the ETI and BVM. Both studies found that the ETI had significantly higher ROSC rate than the BVM; 38.9% vs 34.2%; p value 0.03 in the French study and 18.6% vs 10.3%; p value 0.0352 in the Japanese study.Citation4,Citation7 However, one study from the US showed that survival may not be different between these two airway management in traumatic patients.Citation8
This current study found that the ROSC rates in this study were comparable with the Japanese study but the French study.Citation4,Citation7 The comparable ROSC rates of both BVM and ETI in this study may be due to different characters of study populations in both groups. The BVM group had less severe condition than the ETI group evidence by lower adrenaline treatment (44.88% vs 66.29%; p < 0.001) and defibrillation rate (0.75% vs 2.59%; p 0.025). Additionally, the BVM group received faster treatment than the ETI group; shorter distance to the scene (7.20 vs 8.10 km; p value 0.033). Sum up of the two studies and this current study, the BVM group had the ROSC rate of 26.39% (521/1974), while the ETI group had the ROSC rate of 31.92% (476/1491); p value 0.0004. However, several factors may affect the ROSC rate as in this study such as severity of patients or time to treatment (). Further stratified, randomized controlled trials may be needed.
Even though several studies did not show benefits of ETI over other airway managements such as BVM or extraglottic airway device.Citation8,Citation9 This study found that ETI is preferable if the patients had intravenous access, adrenaline administration, and defibrillation (). These factors may imply that the patients had more severe conditions and required more intervention. As previously reported, patients who received ETI had lower oxygenation (187 vs 213; p 0.034), higher incidence of septic shock (14.5% vs 4.2%; p 0.002), and higher mortality rate (69.1% vs 55.2%; p 0.011) than the control group.Citation10 Those with severe conditions may have more procedures as well.Citation11
The main strength of this study is that the database used is the national database and also showed the results of real-world condition. However, the main limitation of this study is lack of details of the emergency medical personnel: it can be either emergency physicians or emergency technologists. The emergency medical personnel in Thailand are certified by the National Institute for Emergency Medicine (NIEMS). However, this issue may have little effect on outcomes due to large study sample size. Another limitation of this study is the outcome. The EMS database has a record on only ROSC outcome. Long-term outcomes such as survival or neurologic outcomes and volume status of eligible patients are limited.Citation8
In conclusion, the BVM and ETI had comparable ROSC rate. However, the study population of the BVM group was less severe and received faster treatment than the ETI group.
Disclosure
The authors report no conflicts of interest in this work.
References
- Harnod D, Ma MHM, Chang WH, Chang RE, Chang CH. Mortality factors in out-of-hospital cardiac arrest patients. Int J Gerontol. 2013;7(4):216–220. doi:10.1016/j.ijge.2013.08.001
- American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee, Benjamin EJ, Virani SS, Callaway CW, et al. Heart disease and stroke statistics-2018update: are port from the American Heart Association. Circulation. 2018;137(12):e67–e492.
- Shin SD, Ahn KO, Song KJ, Park CB, Lee EJ. Out-of-hospital airway management and cardiac arrest outcomes: a propensity score matched analysis. Resuscitation. 2012;83(3):313–319. doi:10.1016/j.resuscitation.2011.10.028
- Jabre P, Penaloza A, Pinero D, et al. Effect of bag-mask ventilation vs endotracheal intubation during cardiopulmonary resuscitation on neurological outcome after out-of-hospital cardiorespiratory arrest: a randomized clinical trial. JAMA. 2018;319(8):779–787. doi:10.1001/jama.2018.0156
- Hanif MA, Kaji AH, Niemann JT. Advanced airway management does not improve outcome of out-of-hospital cardiac arrest. Acad Emerg Med. 2010;17(9):926–931. doi:10.1111/j.1553-2712.2010.00829.x
- Kang K, Kim T, Ro YS, Kim YJ, Song KJ, Shin SD. Prehospital endotracheal intubation and survival after out-of-hospital cardiac arrest: results from the Korean nationwide registry. Am J Emerg Med. 2016;34(2):128–132. doi:10.1016/j.ajem.2015.09.036
- Nagao T, Kinoshita K, Sakurai A, et al. Effects of bag-mask versus advanced airway ventilation for patients undergoing prolonged cardiopulmonary resuscitation in pre-hospital setting. J Emerg Med. 2012;42(2):162–170. doi:10.1016/j.jemermed.2011.02.020
- Stockinger ZT, McSwain NE. Prehospital endotracheal intubation for trauma does not improve survival over bag-valve-mask ventilation. J Trauma. 2004;56(3):531–536. doi:10.1097/01.TA.0000111755.94642.29
- Kempema J, Trust MD, Ali S, et al. Prehospital endotracheal intubation vs extraglottic airway device in blunt trauma. Am J Emerg Med. 2015;33(8):1080–1083. doi:10.1016/j.ajem.2015.04.046
- Karamanos E, Talving P, Skiada D, et al. Is prehospital endotracheal intubation associated with improved outcomes in isolated severe head injury? A matched cohort analysis. Prehosp Disaster Med. 2014;29(1):32–36. doi:10.1017/S1049023X13008947
- Spaite DW, Tse DJ, Valenzuela TD, et al. The impact of injury severity and prehospital procedures on scene time in victims of major trauma. Ann Emerg Med. 1991;20(12):1299–1305. doi:10.1016/S0196-0644(05)81070-4
