Abstract
Introduction and Purpose
Dispatcher-assisted cardiopulmonary resuscitation (DA-CPR) increases the rate of bystander cardiopulmonary resuscitation (CPR). DA-CPR is recommended by resuscitation councils globally and it has been shown that the general public expects to receive pre-arrival instructions while waiting for help. A scientific advisory from the American Heart Association identifies standardized and structured DA-CPR protocols as important to increase bystander CPR rates. This study aims to investigate whether different International Liaison Committee on Resuscitation (ILCOR) member countries use DA-CPR protocols and to compare protocol contents between countries.
Methods
All resuscitation councils forming ILCOR were inquired by email to provide a copy of their DA-CPR protocol, and to state whether this protocol was used by all emergency dispatch centers in their country. The collected protocols were translated into English, and content was compared.
Results
A total of 60 countries were contacted (response rate: 83%). Of these, 46% stated to have a nationwide protocol, 30% reported to use local protocols, and 24% did not use a protocol. Overall, 54% provided a copy of their protocol. All translated protocols asked the rescuer to check for responsiveness and breathing, 35% to activate phone speaker function, half contained notes about agonal breathing and 59% included notes about integrating an automated external defibrillator.
Conclusion
Almost one quarter of ILCOR member countries did not use a protocol for DA-CPR. Half of the protocols included notes about agonal breathing. Activation of phone speaker function and protocolled encouragements during CPR were rarely included.
Introduction
Dispatcher-assisted cardiopulmonary resuscitation (DA-CPR) is important to strengthen the Chain of Survival; a metaphor describing a series of steps crucial for survival after out-of-hospital-cardiac arrest.Citation1 DA-CPR promotes rapid recognition of cardiac arrest, telephone cardiopulmonary resuscitation (CPR) instructions to the caller, and minimise time to shock delivery.Citation2 Standardized instructions in cardiopulmonary resuscitation (CPR) given by dispatchers before the arrival of Emergency Medical Services increase the rate of bystander CPR.Citation3,Citation4
DA-CPR is recommended globally by resuscitation councils.Citation5–Citation7 A scientific advisory from the American Heart Association identifies standardised and structured DA-CPR programs that provide real-time CPR instructions to rescuers as a part of an approach to increase bystander CPR rates.Citation8 Furthermore, the general public expects to receive pre-arrival instructions while waiting for professional help to arrive.Citation9,Citation10 No studies have investigated whether structured protocols for DA-CPR are used among emergency dispatch centres worldwide.
This observational study aims to investigate whether different International Liaison Committee on Resuscitation (ILCOR) member countries use DA-CPR protocols and to compare protocol contents between countries.
Materials and Methods
All national resuscitation councils forming ILCOR were inquired by email about: (1) providing a copy of the country’s protocols for DA-CPR; (2) whether this protocol was used by all emergency dispatch centers in the country. Furthermore, if the national resuscitation councils did not respond, authors of relevant scientific papers on DA-CPR and emergency dispatch centers in that particular country were emailed identical questions. If no answer was received within 3 weeks, the country was send a reminder email underlining the importance of their contribution to the study. This reminder was resend if no answer had been received within additionally 4 weeks after the first reminder. Protocols in Danish, English, Norwegian and Swedish were translated into English by the lead author (SER). Protocols in other languages were translated into English by volunteer adults, who were native speakers of the particular language. Subsequently, the protocol content was compared. According to the Danish Act on Research Ethics Review of Health Research Projects, Act number 593 of 14 July 2011 section 14, approval from the Danish National Committee on Biomedical Research Ethics was not required.
Results
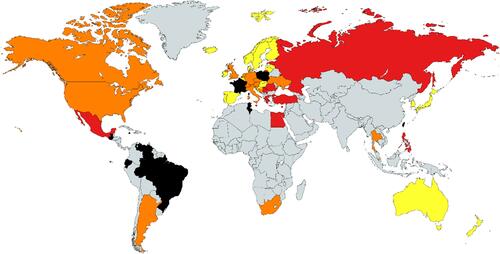
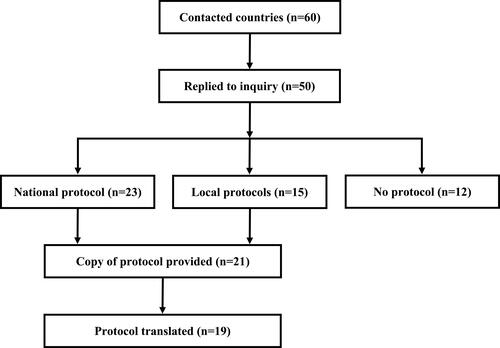
Of the 60 contacted countries, 50 replied to the inquiry (response rate: 83%). shows the contacted countries and their response including whether protocols were used nationwide or locally. Of those responding, 46% (n=23) stated to use a nationwide protocol, 30% (n=15) reported to use multiple local protocols, and 24% (n=12) did not use a protocol when handling cardiac arrest calls (). 2 of the countries not using a protocol reported to rely on doctors’ or nurses’ expertise knowledge when handling cardiac arrest calls. 21 of countries using a protocol (54%) provided a copy of their nationwide or local protocol and 19 of these were translated into English. 2 protocols were not translated due to a lack of volunteer translators (Thailand and Slovenia). All of the translated protocols instructed the rescuer to check for responsiveness and breathing and nearly half of the protocols had a note to the dispatcher about agonal breathing. One third of protocols instructed the caller to activate phone speaker function, the vast majority dictated chest compression-only CPR, and more than half included notes about integrating an automated external defibrillator. shows the content of the translated protocols.
Table 1 Content of Translated Protocols (n=19)
Discussion
The present study found major differences in the use of dispatch protocols among ILCOR countries. Less than half of the replying countries used a nationwide protocol. Moreover, one quarter of countries did not use a DA-CPR protocol when handling emergency cardiac arrest calls. Questions about check for responsiveness and breathing were included in all protocols, whereas notes about agonal breathing were used only by nearly 50% of the countries. Aspects as activation of phone speaker function and protocolled encouragements during CPR were rarely included.
This is the first study to compare approaches towards handling of cardiac arrest calls across national borders. A nationwide protocol was used by less than half of the participating countries. It is unknown whether a nationwide approach is superior to local initiatives and guidelines do not recommend one or the other.Citation5–Citation7 However, even small changes in protocol wording influence CPR performanceCitation11–Citation15 suggesting that a standardised protocol may be preferable. It is well known that survival after cardiac arrest varies greatly across countriesCitation16 and can be as high as 20% in communities with a strong Chain of Survival.Citation2 Importantly, continuous uniformed reporting of outcome from cardiac arrest may be a key element to compare the effect of DA-CPR protocols and to identify best practice.Citation17
It has been reported that even small differences in protocol wording and content result in significant changes in CPR quality.Citation11–Citation15 The optimal dispatch protocol is unknown, and current guidelines have few recommendations regarding the content of protocols, eg using a compression-only CPR approach.Citation5–Citation7 The importance of both agonal breathing and seizure-like activity occurring immediately after cardiac arrest has received increased attention as elements potentially inhibiting recognition of cardiac arrestCitation5 and dispatchers’ awareness hereof has been underlined in scientific statements and guidelines.Citation2,Citation5–Citation7 Almost half of the translated protocols had implemented notes about agonal breathing, and it has been shown that using a dispatch protocol focusing on the presence of agonal breathing significantly increases the identification of out-of-hospital cardiac arrest.Citation18
The minority of protocols included guiding in activation of phone speaker function, even though the European Resuscitation Council 2015 Guidelines on Resuscitation recommend rescuers to switch to phone speaker function in order to facilitate a continuous dialog with the dispatcher.Citation5 Previous studies have suggested a beneficial effect of such dialog consisting of protocolled encouragements during CPRCitation15,Citation19,Citation20 allowing the caller to adjust CPR technique and to be reminded of elements central for high-quality CPR, eg hand position and compression depth. Only 11% of the translated protocols included protocolled encouragements, which should be taken into consideration when developing future DA-CPR protocols because this may contribute to higher CPR quality.Citation15,Citation19,Citation20
Despite the fact that multinational resuscitation councils and ILCOR recommend the use of DA-CPR protocols such an approach has not yet been established in one quarter of the participating countries. It has been estimated that implementation of dispatch protocols with pre-arrival instructions has the potential to save thousands of lives each year in the United StatesCitation2 and the establishment of a well functional dispatch system is therefore essential. It is currently unknown why one quarter of countries do not use a DA-CPR protocol; however, differences in culture, resources and organisation of prehospital care may contribute to the observed differences. Development of an evidence-based DA-CPR protocol describing best practice should be prioritised and preferably led by recognised organisations such as ILCOR. Such a protocol could easily be translated and this may help further facilitate the implementation and use of DA-CPR protocols.
This study has a number of limitations. Data does not represent all countries worldwide and we only have limited data from countries in Africa, Asia and the Middle East. Moreover, our results regarding protocol content are based on only 19 protocols and it should be noted that protocols were translated without the use of certified professional translators. Importantly, protocol content was compared on a general level and we did not compare exact wording. It should be noted that we only investigated if the protocol was used by all emergency dispatch centres in the country and it is unknown if some parts of the countries are not covered by dispatch centres. This study did also not investigate whether continuous quality improvement programs for DA-CPR are active in each country. Further research should focus on the development of evidence-based protocols for DA-CPR and the establishment of united national strategies including uniformed reporting of outcome from out-of-hospital cardiac arrest.
Conclusion
Almost one quarter of ILCOR member countries did not use a protocol for DA-CPR. Half of the protocols included notes about agonal breathing. Activation of phone speaker function and protocolled encouragements during CPR were rarely included.
Acknowledgments
All countries participating in the study are thanked for sharing information about DA-CPR. We sincerely thank volunteers for assisting with protocol translation. The abstract of this paper was presented at the Resuscitation Science Symposium, American Heart Association as a poster presentation with interim findings. The poster’s abstract was published in Circulation. 2016;134:A15593.
Disclosure
Professor Bo Løfgren is a member of the ILCOR Basic Life Support Task Force (2017–2020). The authors report no other conflicts of interest in this work.
References
- Cummins RO, Ornato JP, Thies WH, Pepe PE. Improving survival from sudden cardiac arrest: the “chain of survival” concept. A statement for health professionals from the advanced cardiac life support subcommittee and the emergency cardiac care committee, American heart association. Circulation. 1991;83(5):1832–1847. doi:10.1161/01.CIR.83.5.1832
- Lerner EB, Rea TD, Bobrow BJ, et al. Emergency medical service dispatch cardiopulmonary resuscitation prearrival instructions to improve survival from out-of-hospital cardiac arrest: a scientific statement from the American heart association. Circulation. 2012;125(4):648–655. doi:10.1161/CIR.0b013e31823ee5fc
- Song KJ, Shin SD, Park CB, et al. Dispatcher-assisted bystander cardiopulmonary resuscitation in a metropolitan city: a before-after population-based study. Resuscitation. 2014;85(1):34–41. doi:10.1016/j.resuscitation.2013.06.004
- Vaillancourt C, Verma A, Trickett J, et al. Evaluating the effectiveness of dispatch-assisted cardiopulmonary resuscitation instructions. Acad Emerg Med. 2007;14(10):877–883. doi:10.1197/j.aem.2007.06.021
- Perkins GD, Handley AJ, Koster RW, et al. European resuscitation council guidelines for resuscitation 2015: section 2. adult basic life support and automated external defibrillation. Resuscitation. 2015;95:81–99. doi:10.1016/j.resuscitation.2015.07.015
- Kleinman ME, Brennan EE, Goldberger ZD, et al. Part 5: adult basic life support and cardiopulmonary resuscitation quality: 2015 american heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18 suppl 2):S414–S435. doi:10.1161/CIR.0000000000000259
- Nolan JP, Hazinski MF, Aickin R, et al. Part 1: executive summary: 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation. 2015;95:e1–31. doi:10.1016/j.resuscitation.2015.07.039
- Sasson C, Meischke H, Abella BS, et al. Increasing cardiopulmonary resuscitation provision in communities with low bystander cardiopulmonary resuscitation rates: a science advisory from the american heart association for healthcare providers, policymakers, public health departments, and community leaders. Circulation. 2013;127(12):1342–1350. doi:10.1161/CIR.0b013e318288b4dd
- Billittier AJ 4th, Lerner EB, Tucker W, Lee J. The lay public’s expectations of prearrival instructions when dialing 9-1-1. Prehosp Emerg Care. 2000;4(3):234–237. doi:10.1080/10903120090941254
- Clawson A, Stewart P, Olola C, Freitag S, Clawson J Public expectations of receiving telephone pre-arrival instructions from emergency medical dispatchers at 3 decades post origination at first scripted site. 2016. Available from: https://www.emergencydispatch.org/Public_Expectations. Accessed February 19, 2020.
- Mirza M, Brown TB, Saini D, et al. Instructions to “push as hard as you can” improve average chest compression depth in dispatcher-assisted cardiopulmonary resuscitation. Resuscitation. 2008;79(1):97–102. doi:10.1016/j.resuscitation.2008.05.012
- van Tulder R, Roth D, Havel C, et al. “Push as hard as you can” instruction for telephone cardiopulmonary resuscitation: a randomized simulation study. J Emerg Med. 2014;46(3):363–370. doi:10.1016/j.jemermed.2013.08.067
- Park SO, Hong CK, Shin DH, Lee JH, Hwang SY. Efficacy of metronome sound guidance via a phone speaker during dispatcher-assisted compression-only cardiopulmonary resuscitation by an untrained layperson: a randomised controlled simulation study using a manikin. Emerg Med J. 2013;30(8):657–661. doi:10.1136/emermed-2012-201612
- Eisenberg Chavez D, Meischke H, Painter I, Rea TD. Should dispatchers instruct lay bystanders to undress patients before performing CPR? A randomized simulation study. Resuscitation. 2013;84(7):979–981. doi:10.1016/j.resuscitation.2012.12.010
- Rasmussen SE, Nebsbjerg MA, Krogh LQ, et al. A novel protocol for dispatcher assisted CPR improves CPR quality and motivation among rescuers-a randomized controlled simulation study. Resuscitation. 2017;110:74–80. doi:10.1016/j.resuscitation.2016.09.009
- Sasson C, Rogers MA, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3(1):63–81. doi:10.1161/CIRCOUTCOMES.109.889576
- Castren M, Bohm K, Kvam AM, et al. Reporting of data from out-of-hospital cardiac arrest has to involve emergency medical dispatching–taking the recommendations on reporting OHCA the utstein style a step further. Resuscitation. 2011;82(12):1496–1500. doi:10.1016/j.resuscitation.2011.08.020
- Roppolo LP, Westfall A, Pepe PE, et al. Dispatcher assessments for agonal breathing improve detection of cardiac arrest. Resuscitation. 2009;80(7):769–772. doi:10.1016/j.resuscitation.2009.04.013
- Birkenes TS, Myklebust H, Neset A, Kramer-Johansen J. Quality of CPR performed by trained bystanders with optimized pre-arrival instructions. Resuscitation. 2014;85(1):124–130. doi:10.1016/j.resuscitation.2013.09.015
- Birkenes TS, Myklebust H, Neset A, Olasveengen TM, Kramer-Johansen J. Video analysis of dispatcher-rescuer teamwork-effects on CPR technique and performance. Resuscitation. 2012;83(4):494–499. doi:10.1016/j.resuscitation.2011.09.021