Abstract
The objective of this review was to explore parents’ experiences and information needs regarding management of their child with an intellectual and/or developmental disability (IDD) in the emergency department (ED). We searched six electronic databases and grey literature to identify primary studies in English published since 2000. We synthesized quantitative and qualitative outcome data simultaneously using a convergent integrated approach and used a Mixed Methods Appraisal Tool (MMAT) to assess methodological quality of the included studies. Nine articles derived from seven studies were included (3 qualitative, 3 quantitative, 1 mixed method). Four main themes related to parents’ self-reported experiences were identified: 1) appropriateness of the ED to manage and support their child; 2) acknowledgement/recognition of their child’s IDD and incorporation of those considerations into overall care and management; 3) managing and navigating the ED environment; and 4) decision to disclose their child’s condition when visiting the ED. Two articles provided data relevant to information needs, highlighting parents’ desire to have resources supporting ED orientation and access to services within and outside of the ED setting. From the limited number of studies, it was evident that parents wanted better communication with healthcare providers and a greater understanding by ED staff around physical space settings needed to support their child. Resources supporting ED staff and parents to communicate effectively and work together can ensure that children with IDDs care needs are met. Further research into understanding parents’ experiences and information needs related to managing a child with an IDD in the ED is needed to guide the development of effective resources.
Introduction
Visiting the emergency department (ED) with a child (0–18 years of age) can be overwhelming. This is especially so when the child has an intellectual and/or developmental disability (IDD).Citation1 IDDs are a subset of disabilities that cause limitations in intellectual, physical, neurological, and/or sensory functioning that can negatively affect the trajectory of a child’s physical, intellectual and/or emotional development.Citation2 Unfortunately, children with IDDs are more likely to use ED services compared to their peers without disabilities.Citation3–6
In high-intensity environments, such as the ED, communication, sensory and behavioral challenges pose risks for negative experiences and outcomes.Citation7 Children with IDDs have different capabilities regarding their ability to communicate and understand, and when faced with a strange and unfamiliar place may exhibit behaviors such as aggression,Citation8 hyperactivity,Citation9 self-injury,Citation10 sensitivity to sensory inputsCitation11 and escape behaviorsCitation12 while seeking care. Additionally, waiting to see a healthcare provider can be anxiety-provoking and contribute to behavior disturbances.Citation13
Subsequently, the management of children with IDDs in emergency care settings is increasingly recognized as complex and challenging. Visits to the ED can be stressful and difficult for patients, their caregivers, family and the healthcare staff.Citation7,Citation14–16 As these challenges continue to be documented, a deeper understanding of how parents and caregivers navigate the ED experience and what their information needs are is warranted.
By studying the care seeking experiences of parents of children with IDDs, areas of improvement for communication, physical space settings, care management and expectations can be identified and addressed. Likewise, understanding parent and caregiver information needs and preferences can elucidate gaps in parental health literacy, and guide the development of effective resources pertaining to the care and management of their child in the ED. Therefore, our aim was to perform a systematic review to address the following key research questions:
What are parents’ self-reported experiences surrounding seeking care for their child with an IDD diagnosis in the ED?
What are parents’ self-reported information needs related to seeking care for their child with an IDD diagnosis in the ED?
As children with IDDs are the highest users of emergency healthcare services among their peers, the experiences and perceived information gaps reported by their parents and caregivers should be incorporated into the services they receive.Citation5 To facilitate this, findings from this review and a qualitative study (currently underway) will be integrated to support the development of a tailored knowledge translation (KT) tool for parents. Additionally, a complementary KT tool for front-line healthcare providers, in the form of a Bottom Line Recommendation, has been developed to support the management of children with an IDD in the ED. These KT tools will support parents in understanding what to expect at the ED and how best their child can be supported during their visit. As well, this information will provide healthcare providers with an understanding of parents’ needs and perspectives regarding the support and management of their child with an IDD.
Material and Methods
We conducted a mixed studies systematic review,Citation17 following an a priori protocol (https://osf.io/dpyns), and reported the review following the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines.Citation18 The PRISMA checklist is available in Supplementary Table 1.
Search Strategy and Study Selection
We developed and refined the search strategy in collaboration with a medical librarian with systematic review experience, and in consultation with our clinical content experts, methodologists and parent partners. We combined subject headings and keywords for concepts related to IDD, children (0–18 years of age), parents, experiences, and information needs (complete search strategy in Supplementary Material 1).
The search was peer reviewed using the Peer Review of Electronic Search Strategies (PRESS) checklistCitation19 by a second research librarian with systematic review experience. The final search strategy was then translated for use into MEDLINE and the following electronic databases were searched from inception until January 2023: Ovid Embase, Cochrane Library, Ovid APA PsychINFO, and CINAHL Plus with Full Text via EBSCOhost and Scopus. We also searched ProQuest Dissertations and Theses Global to locate relevant grey literature. We manually scanned the reference lists of all included studies and relevant reviews to identify any additional studies that were not captured by our search. All records identified in our search strategy were exported into EndNote reference management software (v. X9 Clarivate Analytics), duplicates removed and imported into a structured Excel workbook for screening.
Eligibility Criteria and Screening
We included primary research studies if they met the eligibility criteria outlined in Supplementary Table 2. To be included, studies had to report on outcomes related to parents’ self-reported experiences or information needs, concerning the management of their child (0–18 years of age) with an IDD diagnosis in the ED, to be published after 2000 and in English. These date and language restrictions were used to ensure that our results were congruent with present day treatment guidelines and information seeking behaviors of parents in Canada and the USA. The language restriction was not expected to impact the results or conclusions of the systematic review.Citation20
IDD diagnosis refers to conditions related to developmental, learning, language and speech disorders, eg, autism spectrum disorder (ASD), behavior disorders, brain injury, cerebral palsy, Down syndrome, fetal alcohol syndrome, intellectual disability, and spina bifida, as well as conditions captured under the broad definition of intellectual disability, global developmental delay, and neurodevelopmental disabilities.Citation21
We defined “parent” to include familial caregivers, representing mother/father, grandmother/grandfather, aunt/uncle and any other individual living in the same household as the child, who acted as their guardian and was responsible for looking after the child.
To conceptualize experiences and information needs, we adopted the definitions used previously by our research team in similarly published reviews.Citation22–24 We defined experiences as how parents felt (eg, anxious, frightened, confident) and acted (eg, panicked, supportive, in-control) before, during, or after they visited the ED with the child; and information needs as the type, content or topic, quantity, frequency, and mode of delivery of information that parents required or desired to receive in order to support the management of their child in the ED.
Two reviewers independently screened titles and abstracts followed by full texts of studies marked as “include/unsure”. Any disagreements were resolved via consensus or deliberation with a third reviewer.
Data Extraction and Management
We extracted data relevant to study characteristics (eg, author(s)/organization, year of publication, country, study design, setting and objective), data collection tool (eg, questionnaire, survey, focus group, interview), participant characteristics including intersectionality data on social identities (eg, age, race, gender, parental role) where reported, and clinical condition (eg, ASD, Down Syndrome, Cerebral Palsy) and reported outcomes related to parents’ experiences and information needs directly into a structured Excel form (v. 2016, Microsoft Corporation, Redmond, WA). Qualitative data from study participants were extracted verbatim into NVivo data management software (v.10, QSR International, Melbourne, Australia).
All data were extracted by one reviewer and verified by a second reviewer. Any disagreements were discussed and resolved by a third, senior investigator.
Quality Assessment
We appraised the methodological quality of all included studies using the Mixed Methods Appraisal Tool (MMAT) (Supplementary Table 3).Citation25 Two reviewers independently assessed the quality of each included study and consensus was reached via Discussion by resolving any disagreements. An overall quality score for each study was obtained by summing up the “yes” responses for that study. We did not exclude studies based on low-quality assessment scores so as to provide a comprehensive picture of any presentation of parent-reported experiences or information needs related to their child’s management in the ED.
Data Synthesis
Qualitative outcome data reported in the included studies were analyzed thematically. One reviewer coded the qualitative data inductively by applying one or more codes to each line of text according to both its meaning and content. Quantitative outcome data were “qualitized” (ie, transformed into qualitative text) by one reviewer, with subsequent verification by a second reviewer,Citation26 and were coded in the same way as qualitative data. Themes and sub-themes were then developed by the codes until no additional themes emerged from the data. All preliminary codes developed from the qualitative data were verified by a second reviewer, and the final emergent themes and sub-themes were developed and finalized through discussion with the review team. Both the “qualitized” and qualitative data were then compared until no new themes were evident.Citation17 We used a convergent integrated approach to pool “qualitized” and qualitative data with similar meaning and content. An experienced, independent reviewer re-read, verified and discussed all final integrated themes and sub-themes with the review team.Citation27,Citation28
Results
Study Selection
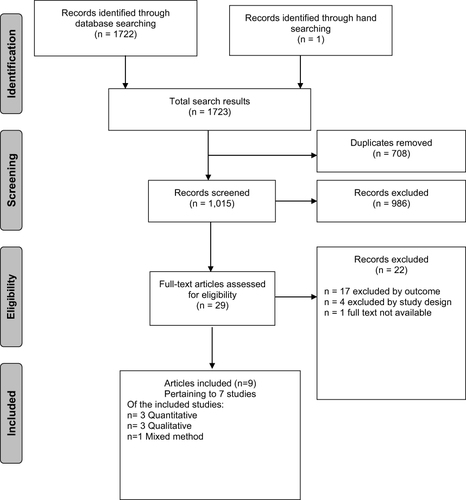
We identified and screened the titles and abstracts of 1015 unique articles, screened the full texts of 29 articles, and upon full-text review included nine articles from seven unique studies (). Two publications (Nicholas 2016a,Citation7 Nicholas 2020Citation15) were associated with a single studyCitation14 and utilized secondary data analysis.
Figure 1 PRISMA Flow Chart - Study selection flow diagram. Adapted from Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009;6(6): e1000097. Creative Commons.
The majority of studies focused on parents of children who have a diagnosis of ASD (n = 6, 86%). and Supplementary Table 4 provide detailed characteristics of the included studies (n = 7). Briefly, the majority (n = 4, 57%) of studies were from Canada,Citation14,Citation29,Citation30 two (29%) were from Australia,Citation31,Citation32 and one (14%) from the USA.Citation33 Most were conducted in pediatric specific EDs (n = 5, 71%). The mean year of publication was 2019, with the majority (71%) of studies published after 2016. Three studies were classified as quantitative design (n = 3, using cross-sectional surveysCitation30,Citation31,Citation33), three studies were classified as qualitative design (descriptive phenomenology,Citation32 grounded theory,Citation14 interpretive descriptionCitation34) and one as a mixed-method design,Citation29 utilizing interviews, journey mapping and surveys.
Table 1 Overview of Characteristics of the Studies Included in the Review (N = 7a)
Cumulatively, there were 523 participants in the included studies (note overlap in participants from three studiesCitation7,Citation14,Citation15), ranging from 14 to 421 across studies. The majority of participants were parents of children with IDDs, while only a few were grandparents or other caregivers (eg, aunts). Hence, for simplicity, we refer to all participants as parents. Parents’ age ranged between 18 to ≥65 years old; the average age reported in two of the studies was approximately 42 years old. The majority of parents (479/523 or 91.6%) reported were mothers. The time between the initial ED visit and data collection ranged from several weeks to a maximum of two years across the studies.
Quality Appraisal
Majority (86%) of included studies were of good quality and met at least 80% of the MMAT criteria. Two studies (29%) met 100% of MMAT criteria, four (57%) met 80% and one (14%) met 60% (Supplementary Table 3).
Parents’ Experiences
All seven studies (nine articles) provided data on parents’ experiences related to the management of their child in the ED. Four main themes related to parents’ self-reported experiences were identified by integrating the qualitative (ie, direct quotes from parents) and “qualitized” data (). Themes were categorized around parents’ experiences related to 1) appropriateness of ED to manage and support their child; 2) acknowledgement/recognition of their child’s IDD and incorporation of those considerations into overall care and management; 3) managing and navigating the ED environment; and 4) decision to disclose their child’s condition when visiting the ED.
Themes and subthemes are discussed in detail below.
Table 2 Summary of Integrated Findings Related to Parents’ Self-Reported Experiences and Information Needs
Role of ED and Lack of Appropriate Support
Parents reported being disappointed and frustrated about the role of the ED in managing their child’s problem due to the existing ED structure and policies and questioned whether it was the right place to seek care. Parents also worried about the impact of lengthy wait times and unnecessary restraint strategies used to manage their child. This theme was further categorized into the following subthemes:
Parents Felt That the Role of ED Was Limited in Managing Their Child’s Behaviors of Concern
This finding was illustrated by the qualitative data from three articlesCitation7,Citation30,Citation32 and the qualitized data from one.Citation31 Parents in these studies reported feeling that the ED staff were mainly trained in the medical management of an emergency situation and their role did not help parents with the management of their child’s behaviors of concern (BOC), such as self-injurious behaviors, verbal or physical aggression, etc., which forced them to seek help at the ED. Some parents were told that they cannot keep coming back to the ED and they should be able to manage their child’s BOC at home.Citation32 Parents in another studyCitation30 reported visiting the ED several times due to their child’s suicidal ideation, and each time they were sent home without any help. In contrast, Pillai et al noted that some parents were advised by the ED staff to access the ED when the need arose in the future.Citation32 However, parents felt uncertain if they would do that because they were disappointed in the care they received.Citation32 Having experienced the limited role of the ED in managing BOC, parents also reported that they will do almost anything to avoid going to the ED and considered the ED as a “last resort” when they felt exhausted and incapable of managing their child’s behavior.Citation7 The qualitized data based on descriptive analyses in Garrick 2022Citation31 further supported this theme by indicating that parents felt ED staff were often very busy and under pressure in their role and were not helpful in responding to their child’s BOC.
Parents Worried About Using a Special Resource Like ED for Behaviors of Concern
This finding was mainly revealed through the qualitative data reported in Pillai 2022.Citation32 Parents reported feeling “awful” in using a valuable resource like an ED to get help for their child’s BOC, especially when the service was needed for other critical medical emergencies (eg, during the COVID pandemic). Some parents reported feeling uncomfortable taking up a hospital bed after their child was managed and stabilized at the ED.
Parents Worried About the Lengthy Wait Times at the ED
Often long wait times at the ED were viewed as a significant source of stress for parents leading to negative experiences. This finding emerged from qualitative data reported in four articlesCitation7,Citation32,Citation34 and was further enriched by the qualitized data from Garrick 2022.Citation31 Some parents worried about the negative impact long wait times would have on their child and believed this would affect their decision and their child’s acceptability to visit the ED in future. Parents reported feeling anxious as they felt their child was not able to handle the crowded ED waiting rooms due to excessive noise, lighting, or other sensory stimuli in the environment. Additionally, the lack of appropriate distractions to keep their child entertained was a cause for concern for some parents.Citation7,Citation31 Others felt that they came to the ED unprepared (eg, did not have food/snacks for themselves or for their child, did not bring distractions to keep the child busy) not knowing how long they had to wait to be seen.Citation7,Citation34 The qualitized data from Garrick 2022Citation31 and Pillai 2022Citation32 also highlighted parents’ concerns about their child feeling “traumatized or stressed” about a future visit to the ED due to the long wait times that they had experienced.
Parents Traumatized by Seeing Restraint Strategies Used on Their Child
The qualitative data from participants in two included articlesCitation30,Citation34 indicated that the use of restraint strategies in special situations was traumatizing for parents. As reported by one parent, seeing her child physically restrained by the ED staff was a “very traumatic experience” for her and for the child.Citation34 She believed that there had to be a better way in managing the child’s behavior instead of using physical force. Another parent reported that knowing from past experience, sedatives alone were not going to be sufficient to keep his son calm. However, the ED staff did not listen to the parent’s advice. This ultimately ended up in security staff restraining the child which did not go well and was “extremely hard” on the parent and the child.Citation30
Staff Interaction and Knowledge of Their Child’s Condition
Data relevant to this theme highlighted parents’ experiences and concerns around their interactions with ED staff and staff’s knowledge/lack of knowledge around IDDs. The subthemes under this finding are discussed below.
Parents Felt They Were Judged/Criticized by the ED Staff Because of Their Child’s “Bad” Behavior
Qualitative and qualitized data from four articles contributed to this finding.Citation7,Citation14,Citation31,Citation32 Parents generally felt that because their child’s condition might not be medically recognized as a significant illness (unlike other well-known illnesses such as childhood asthma or allergic conditions), they were judged by the ED staff as being “bad” parents who were unable to manage their child’s “misbehavior”. Parents felt that they were being looked at as if they were not doing their job as a parent would, or they were not trying hard enough to calm their child down.Citation31 Some parents believed that if their child had a visible disability or a diagnosed clinical condition, they would have been treated differently when they walked into an ED.Citation7 Parents also reported being concerned that the ED staff misunderstood their child’s behavior as being “willful bad behavior” and they were mistreated because of that.Citation14
Parents Reported Their Child’s Disability Being Ignored/Disregarded by the ED Staff
Qualitative and qualitized data reported in five articlesCitation7,Citation15,Citation29,Citation31,Citation32 highlighted parents’ negative experiences around their child’s disability not being recognized as a special-need condition by ED staff. Some parents reported being told that the ED policy did not allow them to get special treatment or fast-tracked triage.Citation7 As illustrated by a quote from one parent “When we asked to be fast tracked, we were always told: no, it’s not fair”.Citation29 Other parents reported that “desired services” (eg, social worker) to support their ED visit were not initially offered to them,Citation15 or they were told off for using their child’s disability as an “excuse” to get some sort of a pass.Citation7 Qualitized data from Garrick 2022 also added to this, highlighting that some parents reported their child not receiving appropriate care or timely service, because their condition was not adequately recognized by the ED staff.Citation31 These experiences often ended up in delayed treatment for the child.
Parents Experiences with ED Staff’s Communication and Accommodation of Their Child’s Needs
Parents’ positive and negative experiences in relation to the ED staffs’ communication with them or their child and experiences around how much their child’s special needs were accommodated were highlighted through qualitative data from Nicholas 2016aCitation7 and qualitized data from Garrick 2022.Citation31 Some parents reported experiencing sympathy from the ED staff and the staff communicating positively with them. There were reports of the ED staff being very understanding of the fact that their child was not typical, therefore they attempted to communicate effectively or to minimize the sensory stimuli to help keep the child calm and relaxed.Citation31 Conversely, some other parents reported ED staff using medical jargon or providing instructions in a way that was incomprehensible to them and their child.Citation7 Additionally, it was reported that ED staff did not adequately explain to the family what was going on, what was to be expected during a treatment, or failed to gain their child’s trust before starting the treatment.Citation31
Parents Experiences Around ED Staff’s Knowledge of Their Child’s Condition
The qualitative and qualitized data from four articlesCitation7,Citation14,Citation15,Citation31 indicated that parents often lacked confidence in the ED staff’s knowledge and proficiency of managing children with IDDs. In general, parents felt that the ED staff often lacked clear knowledge and understanding of their child’s condition which in turn resulted in them being mistreated or not managed appropriately. Some parents reported feeling that the ED staff were not adequately trained or skilled in managing children with IDDs and this delayed their treatment.Citation7,Citation14,Citation15,Citation31,Citation34 On the other hand, some parents reported positive experiences with the openness of the staff in recognizing their child’s special needs and offering the right services. As illustrated by one parent, they understand that they’re dealing with an autistic kid, and they’ve had some training. Then they know certain things they can do and certain things they better not do.Citation7
Parents Want to Work in Partnership with ED Staff
This concept was a commonly reported finding emerging from qualitative and qualitized data across five articles.Citation7,Citation15,Citation29–31 The data related to this sub theme highlighted parents’ desire to take an active role in the ED and to be listened to by the ED staff, as they believed they knew their child’s condition and behavior best. Parents wanted to act as facilitators and wanted ED staff to listen and value their expertise when determining what techniques (eg, sedatives, role-playing, etc.) worked the best for their child.Citation7,Citation15 Some parents reported that their child’s pain was not taken seriously due to its atypical presentation or the child being non-verbal, subsequently they were sent home despite the parent’s input on where the pain was or how severe it was.Citation7 Other parents wanted the staff to ask them if the child is okay to be touched or how the child can be supported to self-regulate before using other techniques that might trigger a child’s anxiety.Citation29 In general, parents felt that they act as their child’s main support, therefore they believed it is critical to incorporate their knowledge into their child’s medical care.
Impact of ED Environment on Care Experiences
Many parents referred to challenges related to managing the physical atmosphere and navigating various environmental stimuli in the ED. Reported data related to this finding were further categorized into the following subthemes.
Parents Worried About the Impact of the ED Environment on Their Child While Waiting to Be Seen
Qualitative and qualitized data from three studiesCitation7,Citation31,Citation32 substantiated this finding. The uncomfortable environment of the ED and presence of unpleasant elements such as bright lights, loud noises, and overcrowded rooms were viewed by many parents as triggering factors for their child’s aggressiveness.Citation32 Some parents worried that the negative impact of the ED environment on their child would make future visits even more challenging and would lead to the child losing trust in the parent or the ED staff and become uncooperative.Citation7 Parents who had experience from their previous visits attempted to overcome this challenge by being prepared when visiting the ED and brought appropriate distractions (eg, sensory kits, iPhone, iPad) or noise cancelling headphones to manage their child.Citation31 Other parents tried to mitigate sensory overload by looking for a quiet place within the hospital where they could wait with their child or implementing techniques that they knew would help to relax their child and reduce anxiety.Citation31
Experiences with Sensory Kits and Accommodation of Their Child’s Sensory Needs in the ED
Litwin 2022 co-created and implemented a sensory equipment kit for children with ASD in the ED. Interviews with parents of children with ASD found that parents generally had a positive experience and reported high satisfaction with the sensory kit.Citation29 Further, Gupta et al implemented an ED clinical pathway that met the sensory needs of children in the ED of a pediatric hospital.Citation33 Parents believed that it helped their child to be cooperative when undergoing procedures or to agree to stay at the hospital.Citation33
The importance of sensory stimuli was also elucidated by the qualitized data from Garrick 2022.Citation31 Some of the parents in that study reported bringing their own sensory accommodations to the ED. Other parents reported that the ED staff tried to reduce the sensory stimuli in the environment (eg, by dimming the lights), although most parents expressed disappointment in the level of effort that the ED staff made to accommodate the child’s sensory needs.Citation31
Decision to Disclose Their Child’s Condition When Visiting the ED
Parents’ desire to disclose their child’s condition to the ED staff was another common finding which emerged from the qualitative data in several articles.Citation14,Citation15,Citation29,Citation31 Some parents preferred to disclose their child’s condition as soon as they arrived at the ED and did not feel embarrassed to let the healthcare staff know that their child had an IDD.Citation29 Parents also reported wanting to be upfront with the healthcare staff about their child’s condition (while hiding it from their family members and relatives) as they believed it was useful for the healthcare staff to know and manage their child appropriately, as well as ensure their child got the care they needed.Citation14,Citation29 Other parents wanted to disclose their child’s condition in hope of getting an expedited service because they knew waiting was hard on their child.Citation14 The desire to disclose was also viewed as a way to avoid getting criticized as a “bad parent” or their child misjudged as having bad behavior by the ED staff, as elucidated by a parent who felt staff were accommodating when they knew.Citation14
In contrast, some parents acknowledged the benefit of disclosing but did not want to disclose that their child was autistic/non-verbal because they feared the child would be “labelled” and “looked at differently”.Citation14 Further, some other parents felt that by disclosing their child’s diagnosis they would be questioned by healthcare staff at every step and their child’s medical care would get more complicated.
Parents’ Information Needs
Only two articles (associated with the same study) discussed what could be considered parent information needs, which related to the content of information that parents required or desired to receive at their ED visit. Nicholas 2020 discussed the importance of sharing information related to ED processes and access to services or amenities for families.Citation15 The authors noted that some parents felt it was important for the ED staff to let the families know how and where to access services and amenities related to the care process or environment while waiting at the ED. Similarly, Nicholas 2016a reported parents wanted improved information for easier access to community follow-up. Parents suggested that ‘existing services need to be advertised so that parents know what is available to them within the ED (eg, child life services), along with more direct links to support services outside the ED for families”.Citation7 Additionally, parents wanted improved communication in the ED around waiting times, and suggested signage needed to be clearer to help children feel more comfortable and oriented to the ED.
Data from other studiesCitation32,Citation34 indicated that parents felt there were practical information gaps related to IDD and lack of professional resources in general,Citation14,Citation30 but these data were not within the context of an ED visit. Therefore, we were unable to identify any themes related to information needs.
Discussion
We identified seven studies that investigated the self-reported experiences of parents seeking emergency care for their child with an IDD, helping elucidate their expectations of management and areas for improvement. However, only two articles (both associated with a single study) reported parents’ information needs in the context of an ED visit, therefore no conclusions as to the type, amount and delivery mode of information that would be most useful to parents could be drawn. Despite the limited available data to review, common themes emerged providing preliminary insight into parents’ experiences when seeking care for their child with an IDD. Parents’ self-reported experiences related to 1) utilizing the ED, 2) staff interaction and knowledge of their child’s condition, 3) management of sensory stimuli in the ED, and 4) disclosing their child’s condition.
Overall, many parents reported being disappointed with their ED care experiences, specifically related to interactions with staff and the appropriate management of their child. Parents felt that ED staff lacked specific skills and were too busy to take the time needed to manage and support a child with an IDD, especially when many ED visits were related to BOC.Citation7,Citation30–32 For many, much of their frustration was due to knowing the ED may not have been the best place to receive help for the given situation, but it was their only point of care when BOC issues arose. It has been previously documented that presentation to the ED for BOC is often a last resort, when parents cannot manage the situation themselves at home any longer.Citation35 Unfortunately, significant barriers exist for families trying to assess community care for the child’s BOC and mental health management prior to ED presentation.Citation36 This prompts the need for further investigation into different models of care or direct links to support services outside of the ED and resources for community follow-up to better support this highly vulnerable group.Citation7
Additionally, challenges related to a lack of understanding about their child’s behavior and ED staff’s knowledge and expertise caring for a child with an IDD left parent feeling frustrated.Citation31 This is similar to reports in the adult IDD population, which highlighted that emergency care was suboptimal from the perspective of patients and caregivers.Citation37–39 Adults with IDD and their caretakers reported negative experiences related to a lack of respect, expertise, knowledge of patients with an IDD and their support needs. According to Lunsky et al, investment in educating ED staff around the types of accommodations that can be made (eg, quiet rooms), as well as the diversity in presentations of IDDs can support families and create a more positive ED care experience.Citation30 Likewise, providing information to parents and increasing their awareness about options available in the ED setting (eg, quiet rooms, child life services) may empower parents to advocate on their child’s behalf.
While often parents are relied heavily upon as experts regarding their child’s condition,Citation40 included studies highlighted parents’ frustration with ED staff not listening or communicating with them, while their child was in the ED. Unlike parents of hospitalized children with an IDD who felt they were being relied on by staff to provide care and knowledge,Citation41 parents in the ED felt that they were at times ignored and underutilized when it came to understanding how best to support their child. Parents noted they wanted to work in partnership with ED staff and healthcare providers.
Further work exploring this notion is needed to understand how best to facilitate this within the ED, as well as what resources are needed to support its implementation. Perspectives from healthcare providers emphasized that being better informed and trained around the needs of children with IDDs can increase their confidence and create a more equitable partnership between parents and staff when discussing and providing care.Citation42 Developing resources or education materials for ED staff through accrediting agencies could support management of children with IDDs in the ED.Citation43 Parents and families should have an integral role in informing these resources specifically around environmental, sensory and communication needs. These findings were also noted in studies assessing parents’ experiences seeking emergency medical care for a child with medical complexity. Often communication gaps and insufficient information were reported as a point of frustration for parents.Citation44–46
A common finding across studies was the lack of transparency regarding the ED processes (specifically wait times and how children are triaged). Lengthy wait times in crowded waiting rooms could induce significant agitation and anxiety in individuals with IDD due to sensory stimuli.Citation13,Citation47 An understanding of how these environmental stimuli may contribute to anxiety and stress for children and parents and developing ways to mitigate them before problems arise is needed. Child-oriented resources, supports for families (eg, effective communication materials about wait timesCitation48), and environmental resources (eg, conducive and welcoming waiting room designs,Citation49 triage protocols to prioritize children with ASDCitation50) are recommended.Citation15
Another common experience for many parents was weighing the decision to disclose their child’s IDD diagnosis to ED staff. Some parents thought disclosing would allow staff to understand and accommodate their child’s needs, yet the decision was not always straightforward.Citation14 Understanding the intricacies of this decision process could help mitigate potential challenges before and after disclosure. Muskat et al identified potential strategies such as staff asking questions about a child’s needs and that these special needs be noted, and care be expedited.Citation14 There is a need for a greater understanding and improvement of communication between parents and ED staff to reduce barriers to care.Citation14,Citation51 Effective multidisciplinary programs have been implemented to address the disparity in care for persons with an IDD, with an understanding that incorporation of caregiver experiences and information needs is essential to the quality of patient management.Citation52 If strategies to improve parent and child experiences in the ED are developed to create a supportive environment, parents may be more inclined to disclose their child’s IDD diagnosis.
Practice Implications
While parents have numerous concerns around the management of their child with an IDD in the ED, initiatives to improve their experiences are currently in development. Sensory equipment kits and clinical pathways to meet sensory needs are being implemented, following precedents set in other healthcare spaces (eg, outpatient clinics, dental offices).Citation53–55 Additionally, the results of this review will provide context for a KT tool directed at healthcare providers. Translating Emergency Knowledge for Kids (a national network with a focus on improving children’s emergency care across Canada, trekk.ca) has developed a Bottom Line Recommendation to support management approaches in ED for children with IDDs.Citation56,Citation57 The tool encourages a partnership between parents and healthcare providers to better serve their children, and highlights the need for tailored communication strategies and the integral role of the caregiver in supporting care management in the ED. In light of the small number of studies, additional research is needed to support the development of a parent focused KT tool, addressing parents’ expectations and ensuring their information needs are considered during care management. Parents and healthcare providers can then work together to improve parents’ experiences when seeking care for their child with an IDD in the ED.
Strengths and Limitations
As we only identified seven studies, the generalizability of our findings may be limited. For example, parents that recruited into the individual studies may not have been representative of all parents seeking ED care for a child with IDD, and those wanting to participate may have only felt that they had negative experiences. However, we worked with an experienced research librarian who developed a comprehensive search covering multiple online databases. Many studies were excluded based on the reported experiences including only children’s experiences, parents reporting their child’s experiences, or parents’ experiences not being related to an ED encounter. The experiences and information needs from the perspective of parents who seek care in the ED for a child with IDD are invaluable. Not only for an understanding of the specific challenges they face but also what information and supports would ensure a better experience of receiving care in the future. Further, we could not assess how the age of the child or reason for presentation to the ED would have affected parents’ experiences and information needs. For example, the incidence of self-injury as a BOC has been shown to increase in the teenage years. Parents’ experiences at the ED for this may be very different to those whose child has sensory needs and is seeking care for a broken arm.
Conclusion
From the limited research that exists, it is evident that parents of children with an IDD are often disappointed and frustrated with ED care management practices and inadequate resources to support their child. While parents acknowledged that the ED may not be the optimal place to take their child, they were often unsure where else to seek care and support during a crisis, or when the child is acutely ill.
Parents want to work in partnership with ED staff to support their child’s care needs but are unsure as to whether to disclose their child’s diagnosis. Parents felt that there was a lack of educational resources to support both ED staff and parents navigate an ED visit and wanted improved communication in the ED around waiting times.
Understanding the drivers of parents’ expectations and care decisions in ED can help inform the development of KT tools that can be implemented to support caregivers and emergency care providers in the management of children with IDDs. Additionally, understanding parents’ information needs can identify what they require from healthcare staff to provide optimal care, and where there are gaps in health literacy. While initiatives are underway in North America to address some of their concerns, our findings call attention to the need for further research around parents’ experiences and specifically information needs related to the management of children with an IDD in the ED.
Abbreviations
ASD, autism spectrum disorder; BOC, behaviors of concern; ED, emergency department; IDD, intellectual and/or developmental disability; KT, knowledge translation; MMAT, Mixed Methods Appraisal Tool; PRESS, Peer Review of Electronic Search Strategies; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-analysis.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgments
We would like to thank Samantha Guitard and Salima Punja for their assistance with study selection, data extraction and data verification; Liz Dennett and Maria Tan for developing, reviewing and implementing the search strategy, respectively.
Data Sharing Statement
Data and forms associated with this manuscript are available upon reasonable request to the corresponding author.
Additional information
Funding
References
- Harwell C, Bradley E. Caring for children with autism in the emergency department. Pediatr Ann. 2019;48(8):e333–e336. doi:10.3928/19382359-20190725-01
- National Institutes of Health. About Intellectual and Developmental Disabilities (IDDs); 2021. Available from: https://www.nichd.nih.gov/health/topics/idds/conditioninfo. Accessed June 13, 2024.
- Beverly J, Giannouchos T, Callaghan T. Examining frequent emergency department use among children and adolescents with autism spectrum disorder. Autism. 2021;25(5):1382–1394. doi:10.1177/1362361321990925
- Gripko M, Joseph A, MohammadiGorji S. Effects of the physical environment on children and families in hospital-based emergency departments: a systematic literature review. J Environ Psychol. 2023;2013:86.
- Lindgren S, Lauer E, Momany E, et al. Disability, hospital care, and cost: utilization of emergency and inpatient care by a cohort of children with intellectual and developmental disabilities. J Pediatr. 2021;229:259–266. doi:10.1016/j.jpeds.2020.08.084
- Lokhandwala T, Khanna R, West-Strum D. Hospitalization burden among individuals with autism. J Autism Dev Disord. 2012;42(1):95–104. doi:10.1007/s10803-011-1217-x
- Nicholas DB, Zwaigenbaum L, Muskat B, et al. Experiences of emergency department care from the perspective of families in which a child has autism spectrum disorder. Soc Work Health Care. 2016a;55(6):409–426. doi:10.1080/00981389.2016.1178679
- Ambler PG, Eidels A, Gregory CA. Anxiety and aggression in adolescents with autism spectrum disorders attending mainstream schools. Res Autism Spectrum Disord. 2015;18:97–109. doi:10.1016/j.rasd.2015.07.005
- Sinzig J, Walter D, Doepfner M. Attention deficit/hyperactivity disorder in children and adolescents with autism spectrum disorder: symptom or syndrome? J Attention Disord. 2009;13(2):117–126. doi:10.1177/1087054708326261
- Blanchard A, Chihuri S, DiGuiseppi CG, Li G. Risk of self-harm in children and adults with autism spectrum disorder: a systematic review and meta-analysis. JAMA Network Open. 2021;4(10):e2130272–e2130272. doi:10.1001/jamanetworkopen.2021.30272
- Bruni M, Cameron D, Dua S, Noy S. Reported Sensory Processing of Children with Down Syndrome. Phys Occupat Therap Pediat. 2010;30(4):280–293. doi:10.3109/01942638.2010.486962
- Feeley K, Jones E. Preventing challenging behaviours in children with Down syndrome: attention to early developing repertoires. Down Synd Res Pract. 2008;12:11–14. doi:10.3104/case-studies.2008
- Centre for Addiction and Mental Health. Guidelines for Managing the Client with Intellectual Disability in the Emergency Room. Toronto, ON: Centre for Addiction and Mental Health, University of Toronto; 2002.
- Muskat B, Greenblatt A, Nicholas DB, et al. Parent and health care provider perspectives related to Disclosure of autism spectrum disorder in pediatric emergency departments. Autism. 2016;20(8):986–994. doi:10.1177/1362361315621520
- Nicholas DB, Muskat B, Zwaigenbaum L, et al. Patient- and family-centered care in the emergency department for children with autism. Pediatrics. 2020;145(Suppl 1):S93–s98. doi:10.1542/peds.2019-1895L
- Scarpinato N, Bradley J, Kurbjun K, Bateman X, Holtzer B, Ely B. Caring for the child with an autism spectrum disorder in the acute care setting. J Spec Pediatr Nurs. 2010;15(3):244–254. doi:10.1111/j.1744-6155.2010.00244.x
- Stern C, Lizarondo L, Carrier J, et al. Methodological guidance for the conduct of mixed methods systematic reviews. JBI Evidence Synth. 2020;18(10):2108–2118. doi:10.11124/JBISRIR-D-19-00169
- Page MJ, Moher D, Bossuyt PM, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160. doi:10.1136/bmj.n160
- McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol. 2016;75(75):40–46. doi:10.1016/j.jclinepi.2016.01.021
- Hartling L, Featherstone R, Nuspl M, Shave K, Dryden DM, Vandermeer B. Grey literature in systematic reviews: a cross-sectional study of the contribution of non-English reports, unpublished studies and dissertations to the results of meta-analyses in child-relevant reviews. BMC Med Res Methodol. 2017;17(1):64. doi:10.1186/s12874-017-0347-z
- Nicholson E, Conlon C, Mimmo L, Doherty E, Guerin S. Unscheduled healthcare for children with intellectual disabilities: a systematic scoping review. J Appl Res Intellect Disabil. 2022;35(3):736–751. doi:10.1111/jar.12994
- Gates A, Shave K, Featherstone R, et al. Procedural pain: systematic review of parent experiences and information needs. Clin Pediatr. 2018;57(6):672–688. doi:10.1177/0009922817733694
- Gates M, Shulhan-Kilroy J, Featherstone R, MacGregor T, Scott SD, Hartling L. Parent experiences and information needs related to bronchiolitis: a mixed studies systematic review. Patient Educ Couns. 2019;102(5):864–878. doi:10.1016/j.pec.2018.12.013
- Thompson AP, Nesari M, Hartling L, Scott SD. Parents’ experiences and information needs related to childhood fever: a systematic review. Patient Educ Couns. 2020;103(4):750–763. doi:10.1016/j.pec.2019.10.004
- Hong QN, Fàbregues S, Bartlett G, et al. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Educ Inf. 2018;34(4):285–291. doi:10.3233/EFI-180221
- Sandelowski M, Voils CI, Knafl G. On Quantitizing. J Mix Methods Res. 2009;3(3):208–222. doi:10.1177/1558689809334210
- Rahman S, Elliott SA, Scott SD, Hartling L. Children at risk of anaphylaxis: a mixed-studies systematic review of parents’ experiences and information needs. PEC Innovation. 2022;1:100018.
- Shulhan-Kilroy J, Elliott SA, Scott SD, Hartling L. Parents’ self-reported experiences and information needs related to acute pediatric asthma exacerbations: a mixed studies systematic review. PEC Innovation. 2022;1:100006. doi:10.1016/j.pecinn.2021.100006
- Litwin S, Sellen K. Designing a sensory kit to improve the environment for children with autism spectrum disorder in the pediatric emergency department. J Aut Develop Dis. 2022;53:3369–3379. doi:10.1007/s10803-022-05651-7
- Lunsky Y, Tint A, Weiss JA, Palucka A, Bradley E. A review of emergency department visits made by youth and adults with autism spectrum disorder from the parent perspective. Advan Autism. 2018;4(1):10–18. doi:10.1108/AIA-08-2017-0019
- Garrick A, Lee ML, Scarffe C, et al. An Australian cross-sectional survey of parents’ experiences of emergency department visits among children with autism spectrum disorder. J Aut Develop Dis. 2022;52(5):2046–2060. doi:10.1007/s10803-021-05091-9
- Pillai J, Dunn K, Efron D. Parent-reported factors associated with the emergency department presentation of children and adolescents with autism spectrum disorder and/or intellectual disability with behaviours of concern: a qualitative study. Arch Dischildhood. 2022;108:264–270. doi:10.1136/archdischild-2022-325002
- Gupta N, Brown C, Deneke J, Maha J, Kong M. Utilization of a novel pathway in a tertiary pediatric hospital to meet the sensory needs of acutely ill pediatric patients. Front Pediat. 2019;7(101615492):367. doi:10.3389/fped.2019.00367
- Nicholas DB, Zwaigenbaum L, Muskat B, et al. Toward practice advancement in emergency care for children with autism spectrum disorder. Pediatrics. 2016b;137(2):S205–211. doi:10.1542/peds.2015-2851S
- Efron D, Cull E, Fowler J, Dunn K, Prakash C. Patterns of presentation to a children’s hospital emergency department of patients with autism and/or intellectual disability with behaviours of concern. J Intellec Developm Disab. 2022;48(1):40–45. doi:10.3109/13668250.2022.2109824
- Hiscock H, Connolly AS, Dunlop K, et al. Parent perspectives on children and young people’s mental health services in Victoria – what’s wrong and how to fix it: a multi-site qualitative study. J Paediatr Child Health. 2020;56:1114–1120. doi:10.1111/jpc.14835
- Iacono T, Davis R. The experiences of people with developmental disability in Emergency Departments and hospital wards. Res Dev Disabil. 2003;24(4):247–264. doi:10.1016/S0891-4222(03)00041-6
- Lunsky Y, Lake JK, Durbin J, et al. Chapter One - understanding and improving care for individuals with intellectual and developmental disabilities in the emergency department. In: Hodapp RM, editor. International Review of Research in Developmental Disabilities. Academic Press; 2014: 1–37.
- Weiss JA, Lunsky Y, Gracey C, Canrinus M, Morris S. Emergency Psychiatric Services for Individuals with Intellectual Disabilities: caregivers’ Perspectives. J Appl Res Intellect Disabil. 2009;22(4):354–362. doi:10.1111/j.1468-3148.2008.00468.x
- Aarthun A, Øymar KA, Akerjordet K. Parental involvement in decision-making about their child’s health care at the hospital. Nurs Open. 2019;6(1):50–58. doi:10.1002/nop2.180
- Mimmo L, Harrison R, Hinchcliff R. Patient safety vulnerabilities for children with intellectual disability in hospital: a systematic review and narrative synthesis. BMJ Paediatrics Open. 2018;2(1):e000201. doi:10.1136/bmjpo-2017-000201
- Oulton K, Gibson F, Carr L, et al. Mapping staff perspectives towards the delivery of hospital care for children and young people with and without learning disabilities in England: a mixed methods national study. BMC Health Serv Res. 2018;18(1):203. doi:10.1186/s12913-018-2970-8
- McGonigle JJ, Migyanka JM, Glor-Scheib SJ, et al. Development and evaluation of educational materials for pre-hospital and emergency department personnel on the care of patients with autism spectrum disorder. J Autism Dev Disord. 2014;44(5):1252–1259. doi:10.1007/s10803-013-1962-0
- Pulcini CD, Belardo Z, Ketterer T, Zorc JJ, Mollen CJ. Improving emergency care for children with medical complexity: parent and physicians’ perspectives. Acad Pediatr. 2021;21(3):513–520. doi:10.1016/j.acap.2020.09.006
- Jonas D, Scanlon C, Bogetz JF. Parental decision-making for children with medical complexity: an integrated literature review. J Pain Symptom Manage. 2022;63(1):e111–e123. doi:10.1016/j.jpainsymman.2021.07.029
- Gallegos C, Cacchillo N. Experiences of parents of children with medical complexity in the pediatric intensive care unit: a scoping review. Crit Care Nurse. 2023;43(4):20–28. doi:10.4037/ccn2023774
- McGonigle JJ, Venkat A, Beresford C, Campbell TP, Gabriels RL. Management of agitation in individuals with autism spectrum disorders in the emergency department. Child Adoles Psychiat Clin North Am. 2014;23(1):83–95. doi:10.1016/j.chc.2013.08.003
- Kirsch SF, Meryash DL, González-Arévalo B. Determinants of parent satisfaction with emergency or urgent care when the patient has autism. J Dev Behav Pediatr. 2018;39(5):365–375. doi:10.1097/DBP.0000000000000573
- Wood EB, Halverson A, Harrison G, Rosenkranz A. Creating a sensory-friendly pediatric emergency department. J Emerg Nurs. 2019;45(4):415–424. doi:10.1016/j.jen.2018.12.002
- Andersson AK, Omberg M, Svedlund M. Triage in the emergency department–a qualitative study of the factors which nurses consider when making decisions. Nurs Crit Care. 2006;11(3):136–145. doi:10.1111/j.1362-1017.2006.00162.x
- Muskat B, Burnham Riosa P, Nicholas DB, Roberts W, Stoddart KP, Zwaigenbaum L. Autism comes to the hospital: the experiences of patients with autism spectrum disorder, their parents and health-care providers at two Canadian paediatric hospitals. Autism. 2015;19(4):482–490. doi:10.1177/1362361314531341
- Ervin DA, Hennen B, Merrick J, Morad M. Healthcare for persons with intellectual and developmental disability in the community. Front Public Health. 2014;2:83. doi:10.3389/fpubh.2014.00083
- Cermak SA, Stein Duker LI, Williams ME, et al. Feasibility of a sensory-adapted dental environment for children with autism. Am J Occup Ther. 2015;69(3):6903220020p1–6903220020p10. doi:10.5014/ajot.2015.013714
- Drake J, Johnson N, Stoneck AV, Martinez DM, Massey M. Evaluation of a coping kit for children with challenging behaviors in a pediatric hospital. Pediatr Nurs. 2012;38(4):215–221.
- O’Hagan B, Bays-Muchmore C, Friedman A, Bartolotti L, King S Building an autism-friendly hospital: how we started, what we have accomplished, and where we go from here. Association of University Centers on Disabilities; 2019. Available from: https://www.aucd.org/template/news.cfm?news_id=14472&id=17. Accessed June 13, 2024.
- Knisley L, Hartling L, Jabbour M, et al. Translating Emergency Knowledge for Kids (TREKK): using research evidence to improve outcomes for children and families in emergency departments across Canada. Cjem. 2022;24(1):12–15. doi:10.1007/s43678-021-00205-9
- TREKK. Bottom Line Recommendations: Caring for Children with Developmental and Intellectual Disabilities; 2021. Available from: https://trekk.ca/resources/bottom-line-recommendations-caring-for-children-with-developmental-and-intellectual-disabilities-in-the-ed. Accessed 17 June 2024.
