Abstract
Patient–provider family planning discussions and preconception counseling can reduce maternal and neonatal risks by increasing adherence to provider recommendations and antiretroviral medication. However, HIV-infected women may not discuss reproductive intentions with providers due to anticipation of negative reactions and stigma. This study aimed to identify correlates of patient–provider family planning discussions among HIV-infected women in rural South Africa, an area with high rates of antenatal HIV and suboptimal rates of prevention of mother-to-child transmission (PMTCT) of HIV. Participants were N=673 pregnant HIV-infected women who completed measures of family planning discussions and knowledge, depression, stigma, intimate partner violence, and male involvement. Participants were, on average, 28 ± 6 years old, and half of them had completed at least 10–11 years of education. Most women were unemployed and had a monthly income of less than ~US$76. Fewer than half of the women reported having family planning discussions with providers. Correlates of patient–provider family planning discussions included younger age, discussions about PMTCT of HIV, male involvement, and decreased stigma (p < 0.05). Depression was indirectly associated with patient–provider family planning discussions through male involvement (b = −0.010, bias-corrected 95% confidence interval [bCI] [−0.019, −0.005]). That is, depression decreased male involvement, and in turn, male involvement increased patient–provider family planning discussions. Therefore, by decreasing male involvement, depression indirectly decreased family planning discussions. Study findings point to the importance of family planning strategies that address depression and facilitate male involvement to enhance communication between patients and providers and optimize maternal and neonatal health outcomes. This study underscores the need for longitudinal assessment of men’s impact on family planning discussions both pre- and postpartum. Increasing support for provision of mental health services during pregnancy is merited to ensure the health of pregnant women living with HIV and their infants.
Introduction
Preventing unintended pregnancies and increasing family planning are an essential element in the prevention of mother-to-child transmission (PMTCT) of HIV.Citation1 South African PMTCT guidelines advise that pregnant HIV-infected women should be counseled on family planning, including postnatal contraception, in clinical consultations.Citation2 Preconception counseling and family planning discussions between HIV-infected women and health care providers can improve maternal and neonatal health outcomes by increasing adherence to preconception health care recommendations, e.g., vitamins, nutrition,Citation3 and antiretroviral medications for HIV treatment or prophylaxis.Citation4–Citation6 However, women in South Africa often have short inter-pregnancy intervalsCitation7 and may access antenatal health care infrequently,Citation8 suggesting that health care visits during a current pregnancy may represent the only opportunity available to providers to discuss family planning with women before a subsequent pregnancy. Pregnancy rates within 1 year of pregnancy do not differ between women who intend to have children and those who do not,Citation9 and antenatal counseling has been found to increase postnatal contraceptive intentions.Citation10 As such, antenatal family planning appears necessary when attending clinical consultations during a current pregnancy, even when women do not express a desire to conceive.
Despite the need to increase family planning and contraception education in support of PMTCT goals, HIV-infected women in South Africa are generally less likely to share reproductive intentions with providers than HIV-negative women and may delay seeking provider guidance until already pregnant.Citation11–Citation13 This failure to disclose reproductive intentions to health care staff decreases the likelihood of addressing family planning in clinical consultations. Lack of trust in providers may arise from concerns regarding limited confidentiality and continuity of care in the clinic setting.Citation5 Internalized stigma and anticipation of negative reactions from health care providers, such as promotion of abortionCitation14 and discouraging women from having children,Citation13 may also contribute to reluctance to discuss reproductive intentions.Citation12–Citation15
Male partners play an important role in reproductive decision-making and may be a source of emotional support for women during and after pregnancy.Citation16,Citation17 However, men may also be a source of distress,Citation16 and depression may negatively affect both interpersonal relationshipsCitation18 and the capacity for future-oriented thinking,Citation19 decreasing the likelihood of family planning. As such, women experiencing both depression and relationship stressCitation18,Citation20 may be less likely to consider future pregnancies and to involve their partners in the process of pregnancy, diminishing the potentially beneficial impact of male involvement in reproductive care.Citation21 Similarly, violence against women in intimate relationships (intimate partner violence [IPV]) can further limit women’s reproductive autonomy, decreasing the willingness to address reproductive issues with providers as well as adherence to treatment and participation in antenatal care.Citation22,Citation23
This study was designed to identify psychosocial correlates of patient–provider family planning discussions among HIV-infected pregnant women in rural Mpumalanga Province, South Africa, an area with high HIV antenatal prevalence rates and suboptimal rates of PMTCT of HIV,Citation24,Citation25 and to assess the impact of male partner involvement on the relationship between depression and family planning discussions. It was anticipated that the results could provide programmatic guidance addressing family planning discussions in clinical consultations with HIV-infected women and the role of male involvement during pregnancy.
Methods
Participants and procedures
Prior to study onset, Institutional Review Board and Research Ethics Committee approval was obtained from the University of Miami Miller School of Medicine, the Human Sciences Research Council, and the Mpumalanga Provincial Government. Cross-sectional data for this manuscript were drawn from a larger, ongoing study, Protect Your Family. The study protocol, including procedures, recruitment, and sample size determination, has been previously described in detail.Citation26 Participants (N=673) were recruited from 12 rural antenatal clinics (ANCs) in the Gert Sibande and Nkangala districts of Mpumalanga province, South Africa. Eligible candidates were HIV-infected pregnant women, aged 18 years or older, and having a male sexual partner, although male partners were not enrolled. Exclusion criteria included being HIV negative, not being pregnant, and not having a male partner. Women were referred to study staff by ANC nurses and enrolled in the study in a private office after providing verbal and written informed consent in English or local language (isiSesotho, isiZulu). Participants were guided in the use of an Audio Computer-Assisted Self-Interview (ACASI), which presented both written and audio interview questions over headphones in the participant’s preferred language (English, isiSesotho, isiZulu) to which the participant responded on a touch screen. ACASI was used to reduce social desirability bias and to facilitate the inclusion of women across all levels of literacy.Citation27 To familiarize participants with the ACASI system, the study staff completed the initial demographic questionnaire together with participants; all other assessments included in the ACASI were completed individually, with study staff personnel available nearby to respond to any questions. The interview was ~30 to 45 minutes in duration, and participants were compensated 50 South African Rand (~US$5) for time and transportation associated with the assessment.
All study personnel received in-depth training regarding responding to participants self-identifying as depressed or suicidal, and information (leaflets, placards) on suicide and depression was posted in ACASI interview rooms.Citation26 A trained health care provider was designated and available at all clinics for respondents endorsing severe depression, suicidal ideation, and IPV. Clinic health care providers were trained to assess risk and provide triage for further assessment, hospitalization, or outpatient counseling/treatment by licensed psychiatric nurses, social workers, and mental health professionals at associated district hospitals.
Measures
All measures were translated and back translated into local language and adapted to local settings.
Demographics
Demographic information included age, education, employment status, income, relationship status, number of children, infant HIV serostatus, and whether the participant had been diagnosed with HIV during pregnancy.
Patient–provider family planning discussions
Per South African PMTCT protocol, pregnant HIV-infected women are counseled on family planning and strategies to prevent MTCT.Citation2 Based on guidelines in the South African PMTCT protocol,Citation2 three questions were used to assess patient–provider family planning discussions: “have you talked with a health care provider about planning to get pregnant in the future?”, “have you talked with a health care provider about taking medication to avoid transmitting HIV to your baby?”, and “do you plan to have more children in the future?”. Response options were “Yes/No”, and all questions were used as individual items.
Depression
The Edinburgh Postnatal Depression Scale 10 (EPDS-10)Citation28 is a 10-item instrument that was used to evaluate the frequency of symptoms of depression experienced in the past week. Adequate internal consistency has been reported for this scale (α=0.80),Citation29 and reliability in this sample was adequate (α=0.75).
Stigma
The AIDS-Related Stigma Scale (ARSS)Citation30 is a nine-item scale that was used to assess stigma, presenting statements representative of HIV stigma, e.g., “People who have AIDS should be ashamed”. Higher scores reflected greater levels of internalized, stigma-related attitudes. Adequate internal reliability (α=0.75) for this scale has been reported previously.Citation31 The reversed coded item for this scale (“It is safe for people who have AIDS to work with children”) was excluded, as the scale demonstrated poor internal reliability (α=0.58) with its inclusion. Excluding the item, reliability was adequate (α=0.74) for this sample.
IPV
IPV was assessed using an adaptation of the Conflict Tactics Scale 18 (CTS-18),Citation32 an 18-item scale that assesses reasoning, psychological IPV, mild physical IPV, and severe physical IPV. For the purposes of this study, only the psychological IPV subscale was used; internal reliability for this subscale was adequate (α=0.82). Nearly all women in this study who report physical IPV report psychological IPV.
Family planning knowledge
It was believed that women who were more knowledgeable about family planning would be more motivated to discuss family planning with providers. Therefore, family planning knowledge was measured using eight questions that pertained to HIV-affected couples with varied response choices by item; questions were adapted from the Safer Conception Knowledge, Attitudes and Practices (SCKAP) and Family Planning survey.Citation33 For each correct response, 1 point was assigned, out of a possible total score of 8; the resulting continuous score was utilized (). As such, greater scores indicated greater knowledge of family planning. Reliability for this scale in this sample was acceptable (α=0.72).
Table 1 Family planning knowledge questionnaire and scoring
Male involvement
Male involvement during pregnancy was assessed using a modified version of the Male Involvement Index.Citation29,Citation34 Questions included “Does your male partner attend antenatal care visits with you?”, which were then scored as 1 (Yes) or 0 (No), with a range of 0–11. In this sample, internal consistency for this scale was adequate (α=0.83).
Statistical analyses
Descriptive statistics were used to analyze demographic and psychosocial variables. To identify psychosocial correlates of family planning discussions between women and providers, bivariate and multivariable analyses were used. To identify bivariate associations, independent samples t tests and chi squares were used to compare women who had discussed family planning with their provider (1) compared to those who had not (0) by demographic and psychosocial characteristics. A non-parametric alternative to the t test, the Mann–Whitney test, was used when distributional assumptions were violated. Given the exploratory nature of this study, all variables found to be associated with family planning discussions at p < 0.15 on bivariate analyses were included in a subsequent multivariable logistic regression model using backward elimination to identify multivariable associations, which excluded variables not significant at p < 0.15 from the final model. Then, a simple mediation modelCitation35 was developed, using family planning discussions as the dependent variable, depression as the independent variable, and male involvement as a mediator, while controlling for the variables retained in the reduced multivariable model. Mediation analysis was conducted using the PROCESS macro developed by Hayes for Statistical Package for the Social Sciences (SPSS) (model 4), specifying 5,000 bootstrap samples as recommended by Hayes.Citation33,Citation36 A cutoff of p < 0.05 level was used as the threshold for significance. Results from the mediation analysis are presented using Baron and Kenny’sCitation37 four-step approach, and the presence of an indirect effect was identified through the absence of zero in the bootstrapped bias-corrected 95% confidence interval (bCI).Citation36 SPSS v22 for Windows was used for all analyses.
Results
Participants were HIV-infected women between 6 and 30 weeks pregnant (M=17.8), none of whom had attended the Protect Your Family intervention. Of 709 HIV-infected pregnant women asked to participate, eight declined, and 28 had unusable data due to technical difficulties or having participated in some element of the intervention before completion of the baseline assessment, which resulted in a total sample of 673 participants (94.9% [95% bCI 93.2, 96.5]). Participants were, on average, 28±6 years old. Half of them (50%) had completed at least 10–11 years of education, and most (78%) were unemployed. Most participants (68%) had a monthly income of <949 ZAR (~US$76). Although all women had a partner, less than one-fifth (19%) reported being married. The majority (79%) of women had at least one child, and 95% reported that the serostatus of all of their children was negative. Approximately half of the women were diagnosed with HIV during the current pregnancy. Fewer than half (47%) of the women reported having family planning discussions with providers; most (85%) reported discussing MTCT. Further demographic detail and comparisons are presented in .
Table 2 Patient–provider family planning discussions by demographic and psychosocial characteristics: bivariate associations (N=673)
Psychosocial correlates of patient–provider family planning discussions
Engaging in family planning discussions with a provider was associated with discussing HIV transmission to the baby, increased male involvement, greater family planning knowledge, lower levels of stigma, and lower levels of depression and psychological IPV in bivariate analyses. In the reduced multivariable model, family planning discussions were associated with younger age, discussions with provider about MTCT, increased male involvement, and decreased stigma and marginally associated with lower levels of both depression and psychological IPV ().
Table 3 Multivariable associations with patient–provider family planning discussions: reduced multivariable analysis (N=673)
Mediation model: depression, male involvement, and family planning discussions
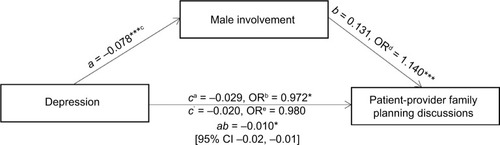
Variables retained in the reduced multivariable model (age, discussions with provider about MTCT, stigma, and psychological IPV) were included as covariates in the following analyses testing the potential for male involvement to mediate the relationship between depression and patient–provider family planning discussions. In the first model, excluding the proposed mediator and after adjusting for covariates, lower depression scores were associated with family planning discussions, b = −0.029, odds ratio (OR) = 0.972, p < 0.001. In the second model, depression was associated with reduced male involvement (b = −0.078, p = 0.001), accounting for the aforementioned covariates. In the third model, male involvement was associated with family planning discussions (b = 0.131, OR = 1.140, p < 0.001) after controlling for depression in addition to the other identified covariates. After controlling for male involvement and the covariates previously described, the effect of depression on family planning discussions was no longer significant, b = −0.020, OR = 0.980, p = 0.135. The indirect effect of depression on patient–provider family planning discussions was statistically significant according to a 95% CI for 5,000 bootstrap samples, b = −0.010, bCI [−0.019, −0.005]. That is, male involvement fully mediated the relationship between depression and family planning discussions, as illustrated in .
Figure 1 Mediation model: indirect effect of depression on patient–provider family planning discussions through male involvement.
Abbreviations: MTCT, mother-to-child transmission; IPV, intimate partner violence; OR, odds ratio; CI, confidence interval.
Discussion
This study of HIV-infected pregnant women in rural South Africa sought to identify psychosocial correlates of family planning discussions between women and providers and to assess the role of male partner involvement on family planning discussions when women are depressed. Emerging correlates of family planning discussions included younger age, discussions with provider about MTCT, increased male involvement, decreased stigma, lower levels of both depression, and psychological IPV. Decreased male involvement was associated with decreased patient–provider family planning discussions; male involvement fully explained the relationship between depression and family planning discussions. As such, being depressed did not impact family planning discussions directly; rather, depression decreased male involvement. In turn, male involvement increased patient–provider family planning discussions. Therefore, by decreasing male involvement, depression indirectly decreased family planning discussions.
Family planning, including postnatal contraception, can reduce maternal and neonatal risksCitation6,Citation38 and is one of the key components of PMTCT protocols.Citation1,Citation2 Whereas only half of the women discussed family planning, the majority discussed MTCT with their providers, and discussions regarding MTCT were associated with family planning discussions, both of which support the integration of family planning in the context of PMTCT counseling. Given that women in this study were all pregnant, the high rates of MTCT discussions confirm that women and providers may not address the potential risks of HIV transmission until after women are pregnant, as suggested by previous research.Citation13 As many women in rural South Africa access reproductive health care only once during pregnancy, the potential for discussions before they may become pregnant again is limited.Citation8 In addition, HIV-infected women are also more likely to miscarry during pregnancy, increasing the likelihood of new pregnancies before women have an opportunity to visit a health care provider.Citation39 Mandated health care visits by women during and following pregnancy provide a window of opportunity to discuss family planning. Given the reported limitations to health reproductive care access in Africa,Citation40 protocol elements aimed to ensure family planning, which includes postnatal contraceptive counseling, may be better provided during antenatal visits rather than only prior to conception, since antenatal counseling increases postnatal contraceptive intentions.Citation10
Consistent with existing literature describing younger women as having a more positive outlook regarding childbearing,Citation41 younger women were more likely to discuss family planning with providers. Similarly, in line with existing literature on HIV stigma,Citation14 this study found patient–provider family planning discussions to be more likely among women reporting less stigma. Interventions aimed at increasing provider- or patient-initiated conception counseling should address women’s concerns regarding provider reactions,Citation12–Citation15,Citation42 confidentiality of HIV serostatus, and continuity in care.Citation5 Training providers in safer conception strategies for HIV-infected women may also enhance clinical practice.Citation43 Addressing these concerns may encourage and facilitate an environment conducive to better family planning discussions by helping providers establish a client-centered therapeutic alliance with their patients.
The effect of depression on reproductive health discussions was mediated by male involvement, indicating that although male involvement does increase the rates of engaging in reproductive health discussions, depression was associated with lower rates of male involvement, thereby indirectly decreasing rates of family planning discussions. These results are consistent with previous studiesCitation18 illustrating that depression may affect interpersonal interactions and result in social rejection, potentially leading to relationship conflict or isolation.Citation20 Thus, depression may inhibit male partner involvement and lead to decreased levels of family planning discussions with providers and potentially other positive benefits of male involvement.Citation16,Citation17 However, as the cross-sectional design of this study limits causal interpretation, the temporal order of events presented here must be confirmed longitudinally.
When interpreting the results of this study, there are certain limitations to bear in mind. First, causal relationships cannot be drawn because of the study’s cross-sectional design. Second, only one item was used to assess family planning discussions. Future studies should address other aspects of family planning discussions with providers that may arise in conjunction with other services or in association with the PMTCT protocol. Third, all of the women in the sample were pregnant, and this manuscript did not assess family planning discussions postnatally. As the rapidly changing antenatal protocol may generate some confusion among HIV-infected women seeking to conceive,Citation26 future clinical initiatives should identify alternative opportunities for family planning discussions in clinical consultations to enhance existing pregnancy protocols. The method and frequency of provider–patient communication within clinics should be examined, as well as the potential long-term indirect effect of depression and male involvement on patient–provider family planning discussions.
While the prevalence of MTCT of HIV in South Africa has decreased from 3.5% in 2010Citation24 to 2.2% in 2016 among exclusive breastfeeding mothers on antiretroviral therapy,Citation44 HIV ANC prevalence rates remain higher in some regions of South Africa.Citation25 This study identified factors associated with antenatal patient–provider family planning discussions and highlighted the importance of family planning strategies to counteract depressionCitation45 and facilitate male involvement as a strategy to enhance communication between patients and providers and optimize maternal and neonatal health outcomes. Evidence to support the contribution of men during pregnancy continues to accumulate, and this study underscores the need for longitudinal assessment of men’s impact on family planning discussions both pre- and postpartum. Similarly, increasing support is evident for provision of mental health services during pregnancy to ensure the health of pregnant women living with HIV and their infants.
Acknowledgments
This study was funded by a grant from the National Institutes of Health (NIH), R01HD078187, and made possible with support from the University of Miami Miller School of Medicine Center for AIDS Research, NIH grant P30AI073961, and from the participating families.
Disclosure
The authors report no conflicts of interest in this work.
References
- BaekCRutenbergNAddressing the Family Planning Needs of HIV-Positive PMTCT Clients: Baseline Findings from An Operations Research StudyWashington, DCPopulation Council2005
- Department of Health: Republic of South AfricaNational Consolidated Guidelines for the Prevention of Mother-to-Child Transmission of HIV (PMTCT) and the Management of HIV in Children, Adolescents, and Adults Available from: http://www.sahivsoc.org/Files/ART%20Guidelines%2015052015.pdfAccessed February 07, 2017
- JeanJCollAMondaMPotterJJonesDPerspectives on safer conception practices and preconception counseling among women living with HIVHealth Care Women Int201637101096111826492078
- AudetCMBlevinsMChireYMEngagement of men in antenatal care services: increased HIV testing and treatment uptake in a community participatory action program in MozambiqueAIDS Behav20162092090210026906021
- GourlayAWringeABirdthistleIMshanaGMichaelDUrassaM“It is like that, we didn’t understand each other”: exploring the influence of patient-provider interactions on prevention of mother-to-child transmission of HIV service use in rural TanzaniaPLoS One201499e10632525180575
- SteinerRJDariotisJKAndersonJRFinocchario-KesslerSPreconception care for people living with HIV: recommendations for advancing implementationAIDS201327suppl 1S113S11924088677
- HungKJScottJRicciottiHAJohnsonTRTsaiACCommunity-level and individual-level influences of intimate partner violence on birth spacing in sub-Saharan AfricaObstet Gynecol2012119597598222525908
- MyerLHarrisonAWhy do women seek antenatal care late? Perspectives from rural South AfricaJ Midwifery Womens Health200348426827212867911
- SmithKBvan der SpuyZMChengLEltonRGlasierAFIs post-partum contraceptive advice given antenatally of value?Contraception200265323724311929646
- KeoghSCUrassaMKumogolaYKalongojiSKimaroDZabaBPostpartum contraception in Northern Tanzania: patterns of use, relationship to antenatal intentions, and impact of antenatal counselingStud Fam Plann201546440542226643490
- KaidaALaherFStrathdeeSAChildbearing intentions of HIV-positive women of reproductive age in Soweto, South Africa: the influence of expanding access to HAART in an HIV hyperendemic settingAm J Public Health2011101235035820403884
- KawalePMindryDPhoyaAJansenPHoffmanRMProvider attitudes about childbearing and knowledge of safer conception at two HIV clinics in MalawiReprod Health2015121725771719
- MindryDLCrankshawTLMaharajP“We have to try and have this child before it is too late”: missed opportunities in client-provider communication on reproductive intentions of people living with HIVAIDS Care2015271253025202986
- CooperDHarriesJMyerLOrnerPBrackenHZweigenthalV“Life is still going on”: reproductive intentions among HIV-positive women and men in South AfricaSoc Sci Med2007651021862186 vol 65, p. 274, 2007
- MyerLMorroniCRebeKPrevalence and determinants of fertility intentions of HIV-infected women and men receiving antiretroviral therapy in South AfricaAIDS Patient Care STDS200721427828517461723
- JonesDChakhtouraNCookRReproductive and maternal healthcare needs of HIV infected womenCurr HIV/AIDS Rep201310433334123918674
- MamanSMoodleyDGrovesAKDefining male support during and after pregnancy from the perspective of HIV-positive and HIV-negative women in Durban, South AfricaJ Midwifery Womens Health201156432533121733102
- HamesJLHaganCRJoinerTEInterpersonal processes in depressionAnnu Rev Clin Psycho20139355377
- BjarehedJSarkohiAAnderssonGLess positive or more negative? Future-directed thinking in mild to moderate depressionCogn Behav Ther2010391374519714541
- CoyneJCThompsonRPalmerSCMarital quality, coping with conflict, marital complaints, and affection in couples with a depressed wifeJ Fam Psychol2002161263711915407
- JonesDPeltzerKVillar-LoubetOReducing the risk of HIV infection during pregnancy among South African women: a randomized controlled trialAIDS Care201325670270923438041
- JewkesRKLevinJBPenn-KekanaLAGender inequalities, intimate partner violence and HIV preventive practices: findings of a South African cross-sectional studySoc Sci Med200356112513412435556
- HatcherAMStocklHChristofidesNMechanisms linking intimate partner violence and prevention of mother-to-child transmission of HIV: a qualitative study in South AfricaSoc Sci Med201616813013927643847
- BarronPPillayYDohertyTEliminating mother-to-child HIV transmission in South AfricaBull World Health Organ2013911707423397353
- Mpumalanga Provincial AIDS CouncilAnnual Progress Report 2014–2015: Provincial Strategic Plan 2012–2016 Available from: http://sanac.org.za/wp-content/uploads/2016/04/MP_PSP-ANNUAL-PROGRESS-REPORT_Final-Report.pdfAccessed February 07, 2017
- JonesDPeltzerKWeissSMImplementing comprehensive prevention of mother-to-child transmission and HIV prevention for South African couples: study protocol for a randomized controlled trialTrials20141541725348459
- MetzgerDSKoblinBTurnerCRandomized controlled trial of audio computer-assisted self-interviewing: utility and acceptability in longitudinal studies. HIVNET Vaccine Preparedness Study Protocol TeamAm J Epidemiol200015229910610909945
- CoxJLHoldenJMSagovskyRDetection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression ScaleBr J Psychiatry19871507827863651732
- PeltzerKSikwaneEMajajaMFactors associated with short-course antiretroviral prophylaxis (dual therapy) adherence for PMTCT in Nkangala district, South AfricaActa Paediatr201110091253125721366691
- KalichmanSCSimbayiLCCloeteAMthembuPPMkhontaRNGinindzaTMeasuring AIDS stigmas in people living with HIV/AIDS: the Internalized AIDS-Related Stigma ScaleAIDS Care2009211879319085224
- KalichmanSCSimbayiLCJoosteSDevelopment of a brief scale to measure AIDS-related stigma in South AfricaAIDS Behav20059213514315933833
- StrausMMeasuring intrafamily conflict and violence: the conflict tactics (CT) scalesJ Marriage Fam19794117588
- IdonijeBOlubaOOtamereHA study on knowledge, attitude and practice of contraception among secondary school students in Ekpoma, NigeriaJPCS201122227
- ByamugishaRTumwineJKSemiyagaNTylleskarTDeterminants of male involvement in the prevention of mother-to-child transmission of HIV programme in Eastern Uganda: a cross-sectional surveyReprod Health201071220573250
- PreacherKJHayesAFSPSS and SAS procedures for estimating indirect effects in simple mediation modelsBehav Res Methods Instrum Comput200436471773115641418
- HayesMStatistical Digital Signal Processing and ModelingNew York, NYJohn Wiley & Sons2009
- BaronRMKennyDAThe moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerationsJ Pers Soc Psychol1986516117311823806354
- MyerLRabkinMAbramsEJRosenfieldAEl-SadrWMColumbia University MTCT-Plus InitiativeFocus on women: linking HIV care and treatment with reproductive health services in the MTCT-Plus InitiativeReprod Health Matters2005132513614616035607
- KimHKasondePMwiyaMPregnancy loss and role of infant HIV status on perinatal mortality among HIV-infected womenBMC Pediatr2012121122208358
- ScorgieFNakatoDHarperE‘We are despised in the hospitals’: sex workers’ experiences of accessing health care in four African countriesCult Health Sex201315445046523414116
- NdunaMFarlaneLWomen Living with HIV in South Africa and their concerns about fertilityAIDS Behav200913suppl 1S62S65
- SchwartzSRMehtaSHTahaTEReesHVVenterFBlackVHigh pregnancy intentions and missed opportunities for patient–provider communication about fertility in a South African cohort of HIV-positive women on antiretroviral therapyAIDS Behav2012161697821656145
- OkororTABelueRZunguNAdamAMAirhihenbuwaCOHIV positive women’s perceptions of stigma in health care settings in Western Cape, South AfricaHealth Care Women Int2014351274923514440
- GogaAEDinhTHJacksonDJSouth Africa PMTCT Evaluation (SAPMCTE) TeamPopulation-level effectiveness of PMTCT Option A on early mother-to-child (MTCT) transmission of HIV in South Africa: implications for eliminating MTCTJ Glob Health20166202040527698999
- RossDASouthAWellerIHakimJHIV treatment and care systems: the way forwardAIDS201226suppl 2S147S15223303436
