Abstract
Background
Depression is a global health concern with significant consequences, especially for women. Hormonal changes and gender disparities contribute to its prevalence. Hormonal contraceptives are widely used among women of reproductive age, but some users report mood-related side effects.
Purpose
This study aims to investigate the relationship between hormonal contraceptive use and depression among women in Mogadishu, Somalia.
Methods
An analytical cross-sectional study was conducted at two hospitals in Mogadishu, targeting married women aged 15–49 using hormonal contraceptives. A sample size of 227 participants was determined, and data was collected using semi-structured questionnaires, including the Patient Health Questionnaire-9 (PHQ-9) to assess depression. The data were analyzed using SPSS version 25, including multivariate logistic regression.
Results
The prevalence of depression among participants was 33.5%, with significant associations observed between depression and occupation, income level, type of hormonal contraceptive used, and duration of contraceptive use. Housewives, individuals with lower income, users of oral pills and implant methods, as well as those with shorter durations of contraceptive use, constituted the high-risk groups for depression.
Conclusion
Depression poses a concern among women using hormonal contraceptives in Mogadishu, Somalia. Healthcare providers should educate women about potential side effects and consider individualized contraceptive recommendations. Mental health support initiatives and awareness campaigns should be introduced. Future research is recommended to further understand and address depression in this context.
Introduction
Depression has significant consequences for women and their families, often leading to increased rates of anxiety, social isolation, drug abuse, and child and spouse relationships.Citation1 Globally, depression ranks as the fourth most prominent cause of disability, and it is projected to become the second major cause of disability.Citation2 Hormonal changes are believed to play a role in depression, with specific brain alterations leading to hormonal imbalances that contribute to depressive symptoms.Citation3 Depression represents an immense problem that affects a vast number of women all over the world, such as those who use hormonal contraceptive drugs.Citation4
Depression poses a significant global health burden, estimated to impact 350 million people worldwide.Citation1 A global mental health study across seventeen nations found that around one in twenty individuals experienced an episode of depression in recent years, with onset often occurring at a young age and leading to substantial disability.Citation5 Depression’s impact is particularly pronounced among women in both high-income and low- and middle-income countries.Citation6
Hormonal contraception is widely used among women of childbearing age, with over 100 million women using hormonal contraceptive pills (HC) worldwide.Citation7 Among 80% of women in the United States report using Oral Contraceptive Pills daily. These contraceptives, including combined oral pills, progestogen-only pills, vaginal rings, hormonal injectables, contraceptive skin patches, and hormone-releasing intrauterine devices (IUDs), are highly effective and practical for family planning.Citation8,Citation9 Approximately 99% of sexually active women have used some form of contraception in their lifetime.Citation10 Combined oral contraceptives (COCs) are particularly popular due to their efficacy and tolerability.Citation11 Hormonal contraceptives are prevalent birth spacing methods in many countries, used by more than 80% of women at some point in their reproductive lives.Citation12 They are also associated with a lowered risk of endometrial and ovarian cancer.Citation13
Although depression affects women of all ages worldwide, its incidence is reported to be twice as high in females compared to males, including in neighboring country EthiopiaCitation1 The commonly used contraceptive method among young women is the combined oral contraceptive pill.Citation14 While most women using combined oral contraceptives report stable or improved moods, some individuals experience mood-related side effects, such as irritability, mood swings, and depressive symptoms. These side effects can lead to discontinuation of contraceptive use, with rates varying by age.Citation15 Gender differences in the lifetime prevalence of depression have been observed, with women being more than twice as likely as men to experience depression.Citation16 However, depression is a complex disorder influenced by various factors, including genetic, and a definitive explanation for this gender difference remains elusive.Citation17 Additionally, combined hormonal contraceptives and progestin-only hormonal contraceptives are available globally; effectively preventing pregnancy and achieving proper cycle control.Citation18 The type of hormonal contraceptive used, the combination of estrogen and progestin, and the specific progestin type can all influence the side effects experienced.Citation19 Studies conducted in various countries, including Ethiopia,Citation20 Kenya,Citation21 Saudi Arabia,Citation22 Tanzania,Citation23 NigeriaCitation24, Iran,Citation8 and Somalia,Citation25,Citation26 have reported associations between hormonal contraceptive use and mood changes, as well as concerns about side effects leading to discontinuation.
In Somalia, limited studies have explored the relationship between depression and hormonal contraceptives among women. This study aims to investigate the connection between the use of hormonal contraceptive methods and depression.
Methods and Materials
Study Design and Site
This study was an analytical cross-sectional study design, which assessed the prevalence of depression among women using hormonal contraceptive drugs in Mogadishu, Somalia. This study was conducted at two selected health service facilities: the first being a private hospital named Somali Sudanese Hospital, and the second a public hospital known as Benadir Mother & Child Hospital. These hospitals are in Hodan and Wadajir Districts, Mogadishu, respectively.
Study Population
The target populations for this study comprised all married women of reproductive age (15–49 years) who were using hormonal contraceptive methods and seeking health services at the selected hospitals in Mogadishu, Somalia.
Inclusion Criteria and Exclusion Criteria
For inclusion criteria, we included married women using hormonal contraceptives and seeking care at the selected hospitals in Mogadishu, Somalia. However, married women who refused to participate in the study and those who had been diagnosed with common mental illnesses, such as schizophrenia and pregnant women, were excluded from the study. We did not exclude women with gynecological co-morbidities. Also, non-married women were excluded because, the selected hospital only provided hormonal contraceptives to married women.
Sample Size and Sampling Technique
To collect data from the participants, a simple random sampling approach was employed. A sample frame was created, listing women who used hormonal contraceptives from each hospital. For a 10% non-response rate, 23 participants were added to the calculated sample size: 204 + 23 = 227. Therefore, the final sample size for this study was determined to be 227 participants. A single proportional-to-size allocation methodCitation27 was used to select a representative sample from each sector, resulting in a total of 227 reproductive-age women who were not pregnant and were using hormonal contraception for the study.
Since the exact number of study population was unknown, we considered the appropriate formula for sample size determination was Cochran’s single population proportion formula which is calculated as:
n= 204 that is the sample size. We added 10% of non-responses rate which was equal 23.
So, the last sample size was 227.
n= the desired sample size.
Z2= is the squared critical value of the desired confidence level.
P= is the estimated attribute proportion which is present in the population under study based on previous or pilot studies. q= is the estimated attribute proportion which is not present in the population under study based on previous or pilot studies, calculated as (1-p).
e2 = is the squared value of the desired level of precision error, also known as margin of error.
In this study, as we know from the Somali demography and health survey of 2020, showed that only 7% of married reproductive aged women in Somalia use pregnancy spacing services.Citation28 So, we have 7% (0.07) as P, while q= 1-p (1–0.07) = 0.93 (93%). Z2= the standard squared critical value usually set at 1.96 which correspondents to 95% confidence level.
Data Collection and Procedures
Semi-structured questionnaires were administered using English and Somali versions to the study participants from the women of two hospitals who use hormonal contraceptive methods in Mogadishu-Somalia. A standard questionnaire was used to collect the data, which included Patient Health Questionnaire-9 (PHQ-9). For the previous two weeks, patient depression was assessed using the PHQ-9 with a 3-point severity scale. Based on the standard PHQ-9 instrumentCitation29 interpretation of total scores ranging from 0 to 4 Non-depression (Minimal depression), 5–9 Mild depression, 10–14 moderate depression, 15–19 moderately severe depression, and severe depression score (≥16 scores were considered significant for meeting the symptoms of depression). Major depression was diagnosed when a study participant experienced five or more of the nine depressive symptoms on most days over the past two weeks. Other forms of depression were assessed when respondents exhibited symptoms related to the primary symptoms of depression (symptoms one, two, three, and four) in addition to other symptoms.Citation29 The questionnaire also gathered socio-demographic information, including age, occupation, degree of education, monthly income, number of children, duration of contraceptive use, and self-reported health status. The primary outcome was the prevalence of depression among women using hormonal contraceptives. Secondary outcome was associated factors with hormonal contraceptive use and depression among Somali married women in selected hospitals, Mogadishu, Somalia. The data was collected between July and September 2022.
Data Management Plan and Analysis
A well-designed data collection tool was meticulously developed to ensure data quality in this study. The lead investigator conducted a thorough review of the collected data each day. Any issues or challenges encountered during the data collection process were promptly addressed, with corrective actions implemented as needed. The data collectors were given guidance to ensure the accuracy of the responses provided by participants. Additionally, a field supervisor carried out a double-check of the completed questionnaires immediately after each field interview and during the submission process. This rigorous quality control process ensured that the data collected was accurate, complete, and consistent on a daily basis. Following the data collection phase, the collected data, including samples and completed questionnaires, underwent thorough cleaning to eliminate any inconsistencies or errors. Subsequently, the data was subjected to analysis using the Statistical Package for Social Sciences (SPSS) version 25. Descriptive statistics were employed to present the data, which was summarized using frequency and percentage distributions. This approach allows readers to easily discern trends in the data distribution. For statistical significance, a p-value equal to or less than 0.05 was considered as the threshold. Multivariate analysis was conducted, with all variables adjusted to assess potential confounding factors.
Ethical Consideration
The study was approved by the ethics committee of the Postgraduate Ethical Review Committee of the School of Public Health and Research (SPHR) of the Somali National University and the selected hospitals. This study followed the ethics stated in the Declaration of Helsinki. Additionally, verbal informed consent was obtained from all the participants or their parents/legal guardians, which the Ethical Review Committee of the SPHR also approved.
Results
Socio-Demographic Characteristics of the Study Participants (n=227)
In the study, a total of 227 female participants were included, with a 100% response rate. More than half of the women, 54.2%, were in the age range of 25 to 34 years old. The majority of women were housewives, accounting for 68.7% of the respondents and 37% had completed a secondary-level education. Regarding income, 87.7% of participants reported a monthly income of less than 500 dollars. Approximately 31.3% of the respondents were employed, as shown in .
Table 1 Socio-Demographic Information of the Study Participants (n=227)
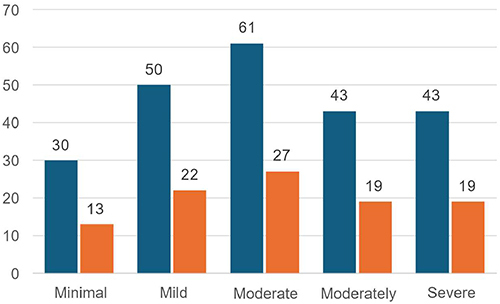
The prevalence of depression was calculated using the Patient Health Questionnaire-(PHQ-9). The respondents who answered yes to more than 16 questions were classified as having depression, while those who answered no to less than 16 questions were considered as not experiencing regular depression. illustrates the distribution of depression levels among the participants, categorized into five groups. The majority of the respondents, 27%, had moderate depression based on the PHQ-9 scale, while 22% had mild depression. Moreover, 19% of the participants experienced moderately severe and severe depression respectively and the lowest rate of depression was observed in 13.1% of the participants.
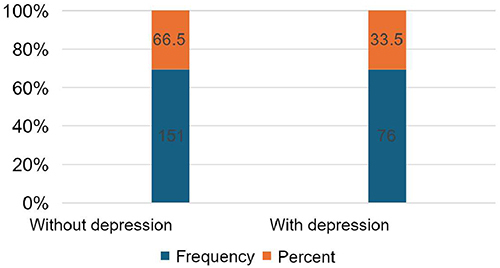
shows the prevalence of depression among study participants was 33.5% and respondents without depression was 66.5%.
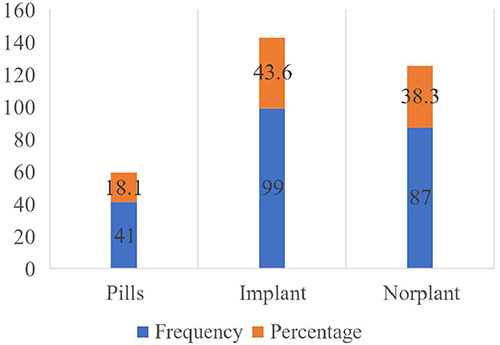
The types of contraceptives, 44% of respondents used the implant method inserted in the upper arm for approximately three years, 38.3% used Norplant, and 18.1% used oral contraceptive pills for child spacing as shown in .
Hormonal Contraceptive Uses Characteristics
shows the characteristics of the participants using hormonal contraceptive methods. The number of children per family, 50.2% had less than three children, but 33.9% of the mothers had 4–7 children, while 15.9% had eight children. Additionally, 44.1% of participants had been using hormonal contraceptives for family planning for over one year, while 53.9% had used them for less than six months. Approximately 39.6% of the participants had taken depression therapy in the past six months. A significant proportion, 78.9%, reported good self-related health status.
Table 2 Hormonal Contraceptive Uses Characteristics of Participants (N= 227)
Logistic Regression Bivariate and Multivariate Analysis Model
In our study, we conducted a multivariate logistic regression analysis to account for potential confounding factors. This analysis was performed on the predictors that had shown significant associations at the bivariate analysis level. In the multivariate analyses, several variables including occupation, income level, types of hormonal contraceptives, and duration of contraceptive use exhibited statistically significant associations with depression among women who used hormonal contraceptives.
In , those who identified as housewives had a 1.91-fold increased likelihood of experiencing depressive illness compared to those who were employed (95% CI=1.10–3.34), with a statistically significant p-value of 0.022. Despite the occupational status, housewives had a 1.91 times higher risk of depressive disorder than those who worked (95% CI=1.10–3.34) with a p-value of 0.022. That means housewives are more susceptible to develop depression once they use hormonal contraceptive methods compared those who are employed. Family income was statistically associated with depression, particularly those earning less than $500 with AOR 0.45 (95% CI=0.26–0.80) per month with a p-value of 0.007, compared to families with more than $600.
Table 3 Logistic Regression Bivariate and Multivariate Analysis Model (N= 227)
On the other hand, the type of hormonal methods was adjusted and statistically reported significance for both oral contraceptive pills with AOR 2.25 (95% CI=1.18–4.32) and implant methods performed AOR 2.26 (95% CI=1.11, 4.63). The oral contraceptive pills p-value was recorded as 0.014. Similarly, implant methods ranged in a p-value less than 0.024.
Therefore, duration was confirmed to be significantly strongly associated with depression of mothers who used hormonal contraceptives for child spacing. In fact, less than three months duration of performed hormonal contraceptives was a high risk of developing depression AOR 0.35 (95% CI=0.19–0.64) with a p-value of 0.001, and six-month duration was AOR 0.30 (95% CI= 0.15–0.60) presented p-value for 0.001.
Discussion
This study revealed that the prevalence of depression among women who used hormonal contraceptives was 33.5%. Another study with a prevalence of depression among hormonal contraceptives conducted in South AfricaCitation30 was reported a similar result, 33.5%. Additionally, a cross-sectional study conducted in EthiopiaCitation1 was roughly 34.1%, and other studies conducted in Jeddah, Saudi ArabiaCitation22, was about 34.6%.
Therefore, a high prevalence of depression was reported in a cross-sectional study conducted in Jazan province, Saudi Arabia, which was higher than the Jeddah study 43.3%.Citation4 Moreover, similar studies on hormonal contraceptives in Iran was reported 37.7%Citation8 and 47.8%Citation3 respectively. For instance, a low prevalence of depression disorders was reported in studies in ThailandCitation31 and the Gambia.Citation32 The findings of this study indicate that those with a higher income level have a decreased likelihood of developing depression in comparison to those with a lower income level (Adjusted Odds Ratio [AOR] = 0.45, 95% Confidence Interval [CI] = 0.26–0.80). Nevertheless, the research findings conducted in EthiopiaCitation1 supported our study results.
Furthermore, the findings of this research shows that there is a higher likelihood of women experiencing depression when utilizing the implant technique or oral pills compared to those who use Norplant. The adjusted odds ratio (AOR) for the implant method is 2.26 (95% CI=1.11–4.63), while the AOR for oral pills is 2.25 (95% CI=1.18–4.32). Despite this study identified mothers who use hormonal contraceptives for one year or more had less chance of getting depression compared with those who use hormonal contraceptives for approximately three months or six months, with AOR 0.3 (95% CI=0.15–0.60), and AOR 0.30 (95% CI=0.15–0.60). Other researchers from Saudi ArabiaCitation4 and IranCitation3 presented similar findings regarding the duration of hormonal contraceptives. While other studies have suggested a potential link between hormonal contraceptives and depression in women, others have not found a significant association. The decision to use hormonal contraceptives should be made individually in consultation with a healthcare provider, considering the potential benefits and risks. Due to the evidence not being convincing, it is clear that depression is a severe health concern for women, and healthcare providers must be aware of the risks associated with hormonal contraceptive use. It is recommended that women who utilize hormonal contraceptives and exhibit symptoms of depression or other mood disorders should promptly consult their healthcare providers in order to determine the most effective course of treatment.
This study has limitations. Firstly, this study is a cross-sectional study which does not allow for determining causation. Secondly the data collected from the questionnaire were self-reported which could subject to recall bias. Despite these limitations, the study determined the prevalence of depression among married women who use hormonal contraceptives in selected hospitals in Mogadishu, Somalia.
Further studies need to be conducted and patients with gynecological comorbidities using hormonal contraceptive use can be explored.
Conclusion and Recommendations
The study conducted at selected hospitals in Mogadishu, Somalia, revealed a significant frequency of depression among married women who use hormonal contraceptives. This study identified a correlation between depression and the use of hormonal contraceptive methods. The significant variables were included occupational, particularly housewives, low income, type of hormonal contraceptive, and first six months of using hormonal contraceptives. Also, this study presented the statistical significance of oral contraceptive pills and the usage of implant methods.
Finally, we recommend that women be aware of hormonal contraceptive side effects before beginning contraception; customized, patient-centered decisions that consider the individual’s history and predispositions are advised. For this study, depression is one of the leading public health issues affecting women during childbearing, and therefore, starting mental health care support innovations in childbearing-age women and awareness raising is crucial. In this regard, we advised conducting a comparable study in Somalia to reduce the prevalence of depression of hormonal contraceptives to fill the research gap.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgment
We would like to acknowledge Dr. Kamaludin Sh. Ahmed for his technical advice during this research and we also acknowledge, School of Public Health and Research, Somali National University. Additionally, we would like to extend our appreciation to Dr. Ismail Mohamed Sh. Abukar and Said Mohamed Yusuf for their continuous support during the study.
References
- Lenjisa G. Addis Ababa University School of Public Health Department of Preventive Medicine Contraceptive Use and Depression Among Female Employees in Governmental Institution in Sebeta Town. Ethiopia: Oromia Regional State; 2016.
- illustrated Guide A. Doing what matters in times of stress: An illustrated guide.
- AAKGR ES. The association of contraceptive methods and depression. Iran J Nurs Midwifery Res. 2012.
- Alfaifi M, Najmi A, Swadi K, Almushtawi A, Jaddoh S. Prevalence of contraceptive use and its association with depression among women in the Jazan province of Saudi Arabia. J Family Med Prim Care. 2021;10(7):2503. doi:10.4103/jfmpc.jfmpc_1308_20
- Sopian MM, Abbas S, Teoh SH, Khan E, Hami R, Din SAT. Mental health and obesity: A narrative review. Pak J Med Health Sci. 2021;15(5):1468–1473. doi:10.53350/pjmhs211551468
- Gregory AM, Van Der Ende J, Willis TA, Verhulst FC Parent-reported sleep problems during development and self-reported anxiety/depression, attention problems, and aggressive behavior later in life; 2008. Available from: http://archpedi.jamanetwork.com/. Accessed June 4, 2024.
- McKetta S, Keyes KM. Oral contraceptive use and depression among adolescents. Ann Epidemiol. 2019;29:46–51. doi:10.1016/j.annepidem.2018.10.002
- Shakerinejad G, Hidarnia A, Motlagh ME, Karami K, Niknami S, Montazeri A. Factors predicting mood changes in oral contraceptive pill users. Reprod Health. 2013;10(1). doi:10.1186/1742-4755-10-45
- Jensen MCH, Jørgensen L, Gemzell-Danielsson K, Sundström Poromaa I, Schroll JB. Hormonal contraceptive use and depression. CochrDat Syst Rev. 2021;2021(1). doi:10.1002/14651858.CD013838
- Teal S, Edelman A. Contraception selection, effectiveness, and adverse effects: a review. JAMA. 2021;326(24):2507–2518. doi:10.1001/jama.2021.21392
- Klipping C, Duijkers I, Parke S, Mellinger U, Serrani M, Junge W. Hemostatic effects of a novel estradiol-based oral contraceptive an open-label, randomized, crossover study of estradiol valerate/dienogest versus Ethinylestradiol/Levonorgestrel. Drugs. 2011;11.
- Hugon-Rodin J, Gompel A, Plu-Bureau G. Mechanisms in endocrinology: Epidemiology of hormonal contraceptives-related venous thromboembolism. Eur J Endocrinol. 2014;171(6):R221–R230. doi:10.1530/EJE-14-0527
- Hormonal contraception, mood and sexual function CECILIA LUNDIN; 2020. Avaiable from: http://urn.kb.se/resolve?urn=urn:nbn:se:uu:diva-420736. Accessed June 4, 2024.
- Hajek A, König HH. Prevalence and correlates of individuals screening positive for depression and anxiety on the phq-4 in the German general population: findings from the nationally representative German socio-economic panel (GSOEP). Int J Environ Res Public Health. 2020;17(21):1–11. doi:10.3390/ijerph17217865
- Faizi N, Kazmi S. Universal health coverage - There is more to it than meets the eye. J Family Med Prim Care. 2017;6(1):169. doi:10.4103/jfmpc.jfmpc_13_17
- Kessler RC, Berglund P, Olga Demler M, et al. Avaiable from: http://stats.bls.gov/cps/cpstn1.htm. The Epidemiology of Major Depressive Disorder Results From the National Comorbidity Survey Replication (NCS-R).
- Andersen MN, Bech P, Csillag C. Development and remission of depressive symptoms and treatment with hormonal contraceptives. Oxf Med Case Reports. 2014;2014(3):63–64. doi:10.1093/omcr/omu025
- Williams L, Jacka F, Pasco J, et al. The prevalence of mood and anxiety disorders in Australian women. Australas Psych. 2010;18(3):250–255. doi:10.3109/10398561003731155
- Segebladh B, Borgström A, Odlind V, Bixo M, Sundström-Poromaa I. Prevalence of psychiatric disorders and premenstrual dysphoric symptoms in patients with experience of adverse mood during treatment with combined oral contraceptives. Contraception. 2009;79(1):50–55. doi:10.1016/j.contraception.2008.08.001
- Mekonnen BD, Wubneh CA. Prevalence and associated factors of contraceptive discontinuation among reproductive-age women in Ethiopia: using 2016 Nationwide Survey Data. Reprod Health. 2020;17(1). doi:10.1186/s12978-020-01032-4
- Kungu W, Agwanda A, Khasakhala A. Prevalence of and factors associated with contraceptive discontinuation in Kenya. Afr J Prim Health Care Fam Med. 2022;14(1). doi:10.4102/phcfm.v14i1.2992
- Alhusain F, Alkaabba F, Alhassan N, et al. Patterns and knowledge of contraceptive methods use among women living in Jeddah, Saudi Arabia. Saudi J Health Sci. 2018;7(2):121. doi:10.4103/sjhs.sjhs_8_18
- Chebet JJ, McMahon SA, Greenspan JA, et al. “Every method seems to have its problems”- Perspectives on side effects of hormonal contraceptives in Morogoro Region, Tanzania. BMC Women's Health. 2015;15(1). doi:10.1186/s12905-015-0255-5
- Durowade KA, Omokanye LO, Elegbede OE, et al. Barriers to contraceptive uptake among women of reproductive age in a semi-Urban community of Ekiti State, Southwest Nigeria. Ethiop J Health Sci. 2017;27(2):121–128. doi:10.4314/ejhs.v27i2.4
- Gele AA, Musse FK, Qureshi S, Bartels S. Unmet needs for contraception: a comparative study among Somali immigrant women in Oslo and their original population in Mogadishu, Somalia. PLoS One. 2019;14(8):e0220783. doi:10.1371/journal.pone.0220783
- Abdulahi M, Kakaire O, Namusoke F. Determinants of modern contraceptive use among married Somali women living in Kampala; A cross sectional survey. Reprod Health. 2020;17(1). doi:10.1186/s12978-020-00922-x
- Naing L, Naing L, Winn T, Rusli BN. Practical Issues in Calculating the Sample Size for Prevalence Studies Practical Issues in Calculating the Sample Size for Prevalence Studies; 2006. Avaiable from: https://www.researchgate.net/publication/45459002. Accessed June 4, 2024.
- The Federal Republic Of Somalia. Avaiable from: www.nbs.gov.so. Accessed June 4, 2024.
- Kroenke K, Spitzer RL, Williams JBW. The PHQ-9 Validity of a Brief Depression Severity Measure. J Gen Intern Med. 2001;16(9):606–613. doi:10.1093/omcr/omu025
- Singata-Madliki M, Hellencourt F, Lawrie TA, Balakrishna Y, Hofmeyr GJ. Effects of three contraceptive methods on depression and sexual function: an ancillary study of the ECHO randomized trial. Int J Gynecol Obstet. 2021;154(2):256–262. doi:10.1002/ijgo.13594
- Charoenpaitoon S, Jirapongsuwan Phd A, Sangon Phd S, Sativipawee Phd P, Kalampakorn Phd S. Factors associated with depression among Thai female workers in the electronics industry. J Med Assoc Thailand. 2012;Vol 95.
- Coleman R, Morison L, Paine K, Powell RA, Walraven G. Women’s reproductive health and depression: a community survey in the Gambia, West Africa. Soc Psycht Epid. 2006;41(9):720–727. doi:10.1007/s00127-006-0085-8