Abstract
Introduction
The study examines the feasibility, quality of counseling, and knowledge after a virtual Group Contraception Counseling (GCC) session.
Methods
At an urban academic hospital, we recruited English-speaking pregnant women aged 15–49 who had access to a video-enabled electronic device. Participants engaged in a standardized 45-minute educational session about contraceptive methods in groups of two to five persons conducted over a video conferencing platform. The primary outcome was participant perceived quality of contraception counseling measured by the Person-Centered Contraception Counseling (PCCC) scale. The secondary outcomes were knowledge change before and after counseling, and postpartum contraception uptake. We used an adjusted multivariable linear regression model to analyze knowledge scores.
Results
Twenty-two participants completed the study. Participants identified primarily as Black or Hispanic/Latinx (78%), in a partnership (50%), having completed college (59%), and having an annual income of less than $50,000 (78%). A total of 77% of participants recorded a perfect score for quality of counseling using the Person-Centered Contraceptive Counseling (PCCC) scale. There was an increase in knowledge after counseling (Mean difference (M)=0.07, p<0.01). Notably, certain subsets of participants had decrease in knowledge scores after counseling. Participants who used postpartum contraception were more likely to have increase in knowledge after counseling compared to those who did not (Mean difference (M)=0.09, p<0.01).
Conclusion
Our findings suggest virtual group contraception counseling is feasible for providing high-quality counseling and can possibly increase contraceptive knowledge.
Introduction
Traditionally, contraception counseling has been a part of routine prenatal and postpartum care and performed on an individualized basis. Both antepartum and postpartum contraceptive counseling significantly increase postpartum contraceptive uptake compared to no counseling.Citation1–6 Additionally, the availability of Long-Acting Reversible Contraception (LARC) contraceptive devices in the immediate postpartum period can increase LARC usage in postpartum adolescent mothers.Citation7
Individualized contraception counseling is the most common in the antenatal setting; however, different methods of contraception counseling have been researched. Contraceptive counseling using written materials and pre-recorded video contraceptive informatics for contraceptive counseling have shown increased contraceptive adherence, contraceptive decision-making, and contraceptive knowledge.Citation8–12 Research on patient desires around contraception counseling has shown that developing rapport, personalizing discussions, setting goals, developing action plans and using shared decision-making improve reproductive health outcomes.Citation2
Group contraceptive counseling (GCC) is an approach to antenatal contraception counseling that brings together small groups of people to discuss contraception options. Centering pregnancies, in which a cohort of women receive routine antenatal care together in a group setting, which includes GCC, has been shown to increase LARC and modern contraception uptake, increase patient satisfaction with care received, increase utilization of family planning services, decrease risk of unintended pregnancy and increase overall postpartum contraception usage.Citation13–18 GCC as a separate entity outside of centering pregnancies has limited research on its use and effectiveness. A small randomized pilot study found that GCC of resettled African refugee women increased knowledge acquisition but did not have a significant effect on contraception usage.Citation19 GCC can signify a potential for improved patient centered, contraception education during the antepartum period. We sought to explore this potential option for patient education while simultaneously prioritizing ease of access by implementing a feasibility study of GCC in the antepartum period. This study explores the participant perceived quality of GCC and change in contraceptive knowledge after counseling in the antepartum period.
Materials and Methods
This study was approved by the University of Illinois at Chicago Institutional Review Board (Protocol # 2020–1626) and was conducted at a large urban, academic hospital center. Participants were informed of the purpose of this study and the study complies with the Declaration of Helsinki. We recruited participants between August 2021 and September 2022. We included participants who received prenatal care at the hospital center, aged greater than 16 years of age, were fluent in English and had access to a video device. Participants were recruited with flyers posted in the Obstetrics and Gynecology outpatient office. Participants were consented by a member of the study team. After enrollment, prior to their GCC session, all participants completed an online survey consisting of demographics and baseline contraceptive knowledge questions. The knowledge survey was adapted from the Fog Zone StudyCitation20 and consisted of 22 true or false questions on contraception. The Fog Zone study was a national survey conducted in the United States on the perceptions and knowledge of contraception for unmarried young adults. The survey questions were adjusted for relevance to contraception methods being discussed during the counseling session and a small internal peer review with six reviewers was conducted prior to survey use. After completion of the surveys, participants were placed into groups of 2–4 persons for GCC.
GCC sessions took place on a HIPPA compliant web-based video communication system. Counseling sessions lasted approximately one hour and were recorded. All sessions were recorded and led by a singular Obstetrician and Gynecology resident. The counseling sessions consisted of a PowerPoint reviewing postpartum birth control options including hormonal and non-hormonal intrauterine devices, subdermal implants, female and male sterilizations, injectable contraception, oral contraceptives, contraception patch, the vaginal ring, barrier methods, coitus-related methods, abstinence, lactational amenorrhea and fertility awareness. The benefits and adverse outcomes of all options were discussed, including potential effects on breastfeeding. At the conclusion of the informational presentation, the forum was opened to a generalized discussion of questions and comments.
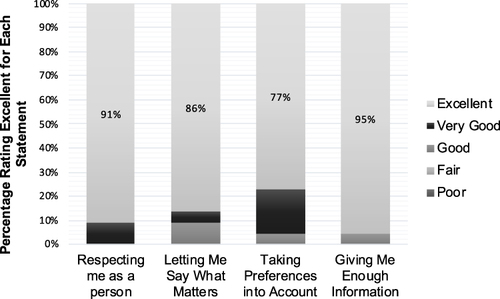
Upon completion of the counseling session, participants were asked to retake the knowledge survey to assess knowledge acquisition. Participants also completed the Person-Centered Contraceptive Counseling (PCCC) survey to assess the quality of contraception counseling.Citation21 The PCCC is a validated quality improvement tool developed to assess the quality of clinician contraceptive counseling by measuring patient satisfaction after contraceptive counseling.Citation21 The tool was created with patient input and prioritizes interpersonal connection, adequate information and decision support in contraception counseling.Citation22 The PCCC is a Likert scale survey with four statements examining contraception counseling quality by asking about respect, prioritization of preferences, adequate information and valuing of patient input.Citation21 Participants who completed these steps were given a $20 Target gift card. A final survey was then emailed to participants at 6 weeks postpartum to identify the contraception option chosen. If the survey was completed, participants received an additional $20 Target gift card. All participants received prenatal care at the study hospital center and had the ability to obtain contraception immediately postpartum or at their 2- or 6-week postpartum visits at the hospital center. Contraception options, including sterilization, and LARC were covered by public and private insurance in the postpartum period, with few exceptions.
The primary outcome was patient perceived quality of GCC, measured with the PCCC scale. Secondary outcomes were knowledge acquisition, measured by score change on the knowledge survey, postpartum contraception uptake and acquisition of desired contraceptive method. The PCC survey was analyzed by calculating the total sum of scores out of a total of 20 possible points. Knowledge survey scores were converted to percentages. The mean change in knowledge score before and after counseling was calculated. A multivariable regression using a generalized estimating equation that predicted score from pre or post counseling was performed, and adjusted for race (Black versus other), marital status (single versus other), employment (part-time and unemployed versus full-time employment as reference), education (college versus high school as reference), household income (more or less than $50,000 per year), and if they received contraception following counseling or not. A t-test was performed to compare a patient's perceived quality of contraception score with mean change in knowledge score.
Results
A total of 22 participants in eight groups completed the study. A majority of participants were Black and Latino (78%) and the mean age was 29 years (). Most participants were employed (64%), college educated (59%) with annual household income of less than $50,000 (78%). A majority of participants, 77%, rated the quality of counseling as 20 out of 20 (). There was no significant difference in rating of the quality of contraception counseling based on change in knowledge score after counseling (p=0.218).
Table 1 Participant Demographics (2021–2022)
The mean pre-counseling knowledge score was 78%, and the mean post-counseling score was 85%. Using the multivariable regression, we found that even after adjusting for race, employment, education, marital status, and contraception uptake, scores were higher following counseling (Mean Score Difference (M)=0.07, 95% CI 0.02–0.12, SE=0.02, p<0.01) (). However, certain groups were noted to have significantly lower increases or decreases in score. Black participants were more likely to see a decrease in knowledge score after counseling compared to non-Black participants (M= −0.12, p<0.01). Participants who were employed part-time (M= −0.12, p<0.01) and unemployed participants (M= −0.08, p<0.001) compared to those who were employed full time were significantly more likely to have a decrease in knowledge score after counseling. Finally, participants who received any form of postpartum contraception were significantly more likely to have a larger increase in knowledge score after counseling (M=0.09, p<0.01) compared to those who did not receive contraception.
Table 2 Multivariable Linear Regression Analysis of Participant Characteristics and Mean Change in Knowledge Score After Virtual GCC (2021–2022)
A majority of participants (77%) completed postpartum contraception uptake surveys. Of the participants who completed the postpartum survey, 82% received some type of contraception. However, only 88% of participants who completed the postpartum survey received their preferred choice of contraception. Close to half, 47%, of participants chose a LARC device.
Discussion
This study demonstrates that virtual GCC is feasible, high quality, and can increase knowledge of postpartum contraceptive options. Virtual group contraception counseling can be an additional option for antepartum patients seeking postpartum contraception options. Contraception counseling that focuses on patient preferences and shared-decision making can empower women and reduce the risk of unintended pregnancy.Citation22
Our study also demonstrated an association between increased knowledge score and increased postpartum contraception uptake. A randomized control trial in Ghana found that GCC was non-inferior to individual counseling and noted increased contraceptive knowledge.Citation23 Other smaller studies have also demonstrated improved knowledge acquisition with group contraception counseling but limited effect on contraception uptake.Citation19 Our study aligns with prior research showing a modest increase in knowledge score after counseling. These results are not generalizable; however, virtual GCC may prove to be a valuable resource for contraception counseling options. Telehealth services have increased since the COVID-19 pandemic and increased health care access, especially for underserved population and those in rural communities.Citation24 Virtual GCC may provide an option for increasing health equity around contraception counseling while providing the same educational uptake as individual counseling. Several factors that are important in contraception counseling include information, respect, privacy, confidentiality, reliability, cost, and informed choice.Citation25–27 This diversity in contraception needs and desires suggests that multiple contraception counseling options and choices are needed to provide people with the counseling method they prefer. Virtual GCC is not a private setting, but participants may find comfort in having these discussions in a chosen, comfortable place. Virtual GCC should be included as a viable option for contraception counseling, especially for communities that would benefit from increased access through telehealth services. Virtual GCC could be integrated into clinical practice, for example, through monthly meetings offered at a clinic or hospital practice as part of their standard prenatal care. The variety of values and desires around contraception counseling also encourage the use of a scale like the PCCC for counseling assessment, which is adaptable to any mode of contraception counseling.
While our study demonstrated an overall increase in knowledge, certain groups were less likely to see this benefit, namely participants who identified as African American or those who were not employed full time. A multitude of factors could have contributed to this. We hypothesize that the knowledge survey used in this study may not be the ideal test to ascertain contraceptive knowledge, particularly for certain groups.
This study was limited in its small number of participants and lack of a comparison group. The Fog Zone study is not a verified measure of knowledge for this particular participant group and the results for this study establish a trend and not necessarily direct knowledge acquisition. The authors also acknowledge that, although there is an increase in knowledge demonstrated, the increase is notably small. Additional research is needed with validated tools to assess contraceptive knowledge. A notable strength of this study is the use of telehealth for contraception counseling and centering of patient preferences as a measurement of successful contraception counseling. This study does provide valid and useful insights into contraceptive counseling methods and patient perceived quality of such methods.
Conclusion
Using the PCCC scale as a tool can give objective data on patient’s perceived quality of contraceptive counseling. This is an important step away from using LARC as a marker of contraceptive counseling success.Citation28 By focusing on patient rating of counseling quality, it is possible to systematically rework the way we counsel patients on contraception and place the focus on how the patient feels about their contraception counseling and their reproductive needs. Virtual GCC may be one potential avenue to improve the way we counsel patients on contraception to ensure understanding of the subject and usage of desired contraceptive options.
Disclosure
The authors report no conflicts of interest in this work.
Additional information
Funding
References
- Hernandez LE, Sappenfield WM, Goodman D, Pooler J. Is effective contraceptive use conceived prenatally in Florida? The association between prenatal contraceptive counseling and postpartum contraceptive use. Maternal Child Health J. 2011;16(2):423–429. doi:10.1007/s10995-010-0738-9
- Zapata L, Pazol K, Dehlendorf C, Curtis K, Malcolm N, Rosmarim R. Contraceptive counseling in clinical settings: an updated systematic review. Am J Prev Med. 2018;55(5):677–690. doi:10.1016/j.amepre.2018.07.006.
- Zapata LB, Murtaza S, Whiteman MK, et al. Contraceptive counseling and postpartum contraceptive use. Am J Clin Exp Obstet Gynecol. 2015;212(2):171.e1–8. doi:10.1016/j.ajog.2014.07.059
- Rutledge RI, Domino ME, Hillemeier MM, Wells R. The effect of maternity care coordination services on utilization of postpartum contraceptive services. Contraception. 2016;94(5):541–547. doi:10.1016/j.contraception.2016.06.007
- Achwoka D, Pintye J, McGrath CJ, et al. Uptake and correlates of contraception among postpartum women in Kenya: results from a national cross-sectional survey. Contraception. 2018;97(3):227–235. doi:10.1016/j.contraception.2017.10.001
- Lopez LM, Hiller JE, Grimes DA, Chen M. Education for contraceptive use by women after childbirth. Cochrane Database Syst Rev. 2012;8(8):CD001863.
- Frarey A, Gurney EP, Sober S, Whittaker PG, Schreiber CA. Postpartum contraceptive counseling for first-time adolescent mothers: a randomized controlled trial. Arch Gynecol Obstetrics. 2019;299(2):361–369. doi:10.1007/s00404-018-4969-0.
- Garbers S, Meserve A, Kottke M, Hatcher R, Chiasson MA. Tailored health messaging improves contraceptive continuation and adherence: results from a randomized controlled trial. Contraception. 2012;86(5):536–542. doi:10.1016/j.contraception.2012.02.005.
- Hersh AR, Muñoz LF, Rincón M, et al. Video compared to conversational contraceptive counseling during labor and maternity hospitalization in Colombia: a randomized trial. Contraception. 2018;98(3):210–214. doi:10.1016/j.contraception.2018.05.004
- Johnson LK, Edelman A, Jensen J. Patient satisfaction and the impact of written material about postpartum contraceptive decisions. Am J Clin Exp Obstet Gynecol. 2003;188(5):1202–1204. doi:10.1067/mob.2003.308
- Pazol K, Zapata LB, Dehlendorf C, Malcolm NM, Rosmarin RB, Frederiksen BN. Impact of contraceptive education on knowledge and decision making: an updated systematic review. Am J Prev Med. 2018;55(5):703–715. doi:10.1016/j.amepre.2018.07.012
- Staley S, Charm S, Slough L, Zerden M, Morse J. Prenatal contraceptive counseling by video. South Med J. 2019;112(1):8–13. doi:10.14423/SMJ.0000000000000913.
- Trotman G, Chhatre G, Darolia R, Tefera E, Damle L, Gomez-Lobo V. The effect of centering pregnancy versus traditional prenatal care models on improved adolescent health behaviors in the perinatal period. J Pediatr Adolesc Gynecol. 2015;28(5):395–401. doi:10.1016/j.jpag.2014.12.003.
- Tandon SD, Cluxton-Keller F, Colon L, Vega P, Alonso A. Improved adequacy of prenatal care and healthcare utilization among low-income latinas receiving group prenatal care. J Women’s Health. 2013;22(12):1056–1061. doi:10.1089/jwh.2013.4352.
- Smith E. Centering contraception: postpartum contraceptive choices of women enrolled in group versus traditional prenatal care. Contraception. 2015;94(4):404. doi:10.1016/j.contraception.2016.07.082.
- Lori JR, Chuey M, Munro-Kramer ML, Ofosu-Darkwah H, Adanu RMK. Increasing postpartum family planning uptake through group antenatal care: a longitudinal prospective cohort design. Reproductive Health. 2018;15(1):208. doi:10.1186/s12978-018-0644-y.
- Halpern V, Lopez LM, Grimes DA, Stockton LL, Gallo MF. Strategies to improve adherence and acceptability of hormonal methods of contraception. Cochrane Database Syst Rev. 2013;(10):CD004317. doi:10.1002/14651858.CD004317.pub4
- Hale N, Picklesimer AH, Billings DL, Covington-Kolb S. The impact of centering pregnancy group prenatal care on postpartum family planning. Am J Clin Exp Obstet Gynecol. 2014;210(1):50.e1–50.e7. doi:10.1016/j.ajog.2013.09.001.
- Royer P, Jenkins A, Weber L, Jackson B, Sanders J, Turok D. Group versus individual contraceptive counseling for resettled African refugee women: a pilot randomized controlled trial. Contraception. 2015;94(4):419. doi:10.1016/j.contraception.2016.07.133.
- Kaye K, Suellentrop K, Sloup C. How misperceptions, magical thinking, and ambivalence put young adults at risk for unplanned pregnancy the fog zone the fog zone; 2009. Available from: https://powertodecide.org/sites/default/files/resources/primary-download/fog-zone-full.pdf. Accessed June 26, 2024.
- Dehlendorf C, Henderson JT, Vittinghoff E, Steinauer J, Hessler D. Development of a patient-reported measure of the interpersonal quality of family planning care. Contraception. 2018;97(1):34–40. doi:10.1016/j.contraception.2017.09.005
- Dehlendorf C, Levy K, Kelley A, Grumbach K, Steinauer J. Women’s preferences for contraceptive counseling and decision making. Contraception. 2013;88(2):250–256. doi:10.1016/j.contraception.2012.10.012
- Schwandt HM, Creanga AA, Danso KA, Adanu RM, Agbenyega T, Hindin MJ. Group versus individual family planning counseling in Ghana: a randomized, noninferiority trial. Contraception. 2013;88(2):281–288. doi:10.1016/j.contraception.2013.03.008
- Gajarawala SN, Pelkowski JN. Telehealth benefits and barriers. J Nurse Pract. 2021;17(2):218–221. doi:10.1016/j.nurpra.2020.09.013
- Holt K, Zavala I, Quintero X, et al. Women’s preferences for contraceptive counseling in Mexico: results from a focus group study. Reprod Health. 2018;15(128). doi:10.1186/s12978-018-0569-5
- Yeh PT, Kautsar H, Kennedy CE, Gaffield ME. Values and preferences for contraception: a global systematic review. Contraception. 2022;111:3–21. doi:10.1016/j.contraception.2022.04.011
- Holt K, Uttekar BV, Reed R, et al. Understanding quality of contraceptive services from women’s perspectives in Gujarat, India: a focus group study. BMJ Open. 2021;11(10):e049260. doi:10.1136/bmjopen-2021-049260
- Eeckhaut MC, Hara Y. Reproductive oppression enters the twenty-first century: pressure to use long-acting reversible contraception (Larc) in the context of “Larc first. Socius: Sociological Research for a Dynamic World. 2023;9. doi:10.1177/23780231231180378
- Dehlendorf C, Krajewski C, Borrero S. Contraceptive Counseling. Clin Obstet Gynecol. 2014;57(4):659–673. doi:10.1097/GRF.0000000000000059