Abstract
Introduction
Stenosing tenosynovitis that is characterized by the inability to flex the digit smoothly, usually leads to prolonged rehabilitation or surgery.
Study design
This case series is a retrospective cohort study.
Purpose
The aim of this case series was to evaluate the effectiveness of radial extracorporeal shockwave therapy (rESWT) for the treatment of stenosing tenosynovitis of the digital flexor tendon (trigger digit).
Methods
A retrospective analysis of 44 patients (49 fingers) treated with an individually adapted rESWT protocol was conducted. Trigger digit pain and function were evaluated at baseline and 1-, 3-, and 12-months posttreatment. Recurrence and pretreatment symptom duration were analyzed.
Results
Significant reductions in pain scores and functional improvement were found between baseline and all follow-up assessments (P<0.001). Pretreatment symptom duration was significantly correlated with the number of rESWT sessions required (r=0.776, P<0.001) and 1-year posttreatment pain score (r=0.335, P=0.019).
Conclusion
This study provides initial evidence that rESWT is an effective treatment for trigger digit, but randomised controlled trials are required to provide further evidence of this effect.
Introduction
Trigger digit, also known as stenosing tenosynovitis, is characterized by an inability to flex or extend the digit smoothly, often with pain over the palmar aspect of the metacarpophalangeal joint.Citation1–Citation3 This condition develops when thickening of the tendon sheath at the first annular ligament’s pulley and subsequent constriction of the tendon prevents it from gliding through. Pinching of the tendon often causes nodule formation,Citation1,Citation3,Citation4 and patients typically present with a locking, popping sensation as the nodule catches at the constriction.Citation1,Citation2,Citation4 In some cases, it resolves spontaneously; however, if left untreated, trigger digit may gradually progress until the affected finger or thumb is permanently locked in flexion.Citation1 Histologically, the A1 pulley exhibits fibrocartilaginous metaplasia, and in the tendon tissue, areas of hyalinosis, mucoid degeneration, and chondral metaplasia are found.Citation5 It is the most common flexor tendinopathy,Citation2 with highest incidence in women (75%) and in those aged between 52 and 62 years,Citation6 with the fourth digit (ring finger) and thumb most often affected.Citation3
Trigger digits are usually idiopathic; however, some authors argue that there is a possible correlation with excessive use of the hand.Citation7,Citation8 Other potential risk factors include rheumatoid arthritis, diabetes mellitus, carpal tunnel syndrome, Dupuytren’s disease, amyloidosis, hypothyroidism, mucopolysaccharide storage disorders, congestive heart failure, and genetic predisposition.Citation4,Citation9,Citation10
Treatment aims to eliminate pain and stop triggering. Currently accepted conservative treatments include pain medication, orthoses, physiotherapy, and corticosteroid injections.Citation3 Corticosteroid injection has the greatest success rate;Citation11 however, it is still reported to be effective only in 57% of the patients.Citation6 Moreover, multiple injections may cause tendon rupture, a course of more than two injections is reported to almost never be successful, and repeated injections before surgery are not cost-effective. Thus, for many patients, corticosteroid injection is not a long-term treatment option.Citation2,Citation12,Citation13
Surgical treatment involves percutaneous and open release of the A1 pulley.Citation2,Citation3 Both are reported to be similarly effective and superior to corticosteroid injection,Citation14 with remission of symptoms achieved in 97%–100% of cases.Citation14–Citation17 However, it is associated with longer recovery times and more complications including tendon bowstringing, digital ulnar drift, and nerve injuries.Citation3 Due to these possible complications and as guidelines by the American College of Occupational and Environmental MedicineCitation18 recommend surgery only when conservative treatments have failed, radial extracorporeal shock wave therapy (rESWT) could play a role as a noninvasive alternative.
rESWT is a noninvasive and safe therapy and has been used in the management of tendon pathologies since the early 1990s in order to alleviate pain and improve function. A radial shockwave is a low-energy wave that is generated when a projectile in the hand piece of the rESWT device is accelerated by a compressed air source and hits a metal applicator. The pressure wave is transmitted to the patient’s skin through ultrasound gel and spreads as a spherical (radial) wave into the tissue. The energy is highest at the tip of the applicator and decreases peripherally by the square of the distance.Citation19–Citation21 The biological mechanisms by which rESWT induces therapeutic effects on pathological tendon tissue are not completely elucidated, although it is suggested that shockwaves may facilitate the healing process through the disruption of avascular, damaged tissues, stimulation of growth factor release, stem cell recruitment, and neovascularisation.Citation22–Citation25
rESWT has been used to treat numerous other tendinopathies, such as epicondylitis,Citation22,Citation26 plantar fasciitis,Citation26–Citation28 patellar tendinopathy,Citation21,Citation26,Citation29 shoulder calcific tendinitis,Citation19,Citation30,Citation31 proximal hamstring tendinopathy,Citation32 and medial tibial stress syndrome.Citation20,Citation33 However, to the authors’ knowledge, to date, no studies on rESWT and trigger digit have been conducted.
Acknowledging the poor efficacy and the prolonged rehabilitation of traditional conservative treatments, possible complications associated with surgery, and the evidence that rESWT (with the additional advantage that it is noninvasive) is effective in the treatment of other tendinopathies, the aim of this study was to determine whether rESWT is a safe and effective treatment for trigger digit. Therefore, the functional improvement and mean pain reduction over a 1-year follow-up period were assessed. In addition, the individualised treatment protocol was retrospectively analysed to look for correlations between pre-treatment symptom duration, the number of rESWT sessions required until recovery, and the 1-year post-treatment visual analog scale score.
Materials and methods
Study subjects
Ethical approval for this retrospective, uncontrolled cohort study was granted by the Thessaloniki Clinic Institutional Review Board (ART No 2012-03). All participants provided written informed consent. The study included 44 adults (49 fingers/thumbs; 39 adults with single-digit pathology and five with two-digit pathology) who were sequentially diagnosed with trigger digit by a consultant in Sport and Exercise Medicine outpatient clinic between 2009 and 2013 (). The diagnosis was based on clinical history and examination. Patients underwent ultrasound imaging to assess thickening of the A1 pulley.
Table 1 Characteristics of patients and trigger digits receiving radial extracorporeal shockwave therapy
The mean age of the study participants was 49±10 years (ranging from 32 to 71 years). Of the total participants, 33 participants (67.3%) were women and 16 (32.7%) were men. The average pretreatment symptom duration was 5±5.7 months (ranging from 1 to 24 months); 19 fingers/thumbs (38.8%) had symptoms for <3 months, 19 fingers/thumbs (38.8%) from 3 to 6 months, 4 fingers/thumbs (8.2%) from 6 to 12 months, and 7 (14.3%) fingers/thumbs from 12 to 24 months.
Inclusion criteria
Patients with Grade 2 and Grade 3 trigger digit according to Quinnell’s classification (Grade 0: normal finger movements, Grade 1: uneven finger movements, Grade 2: actively correctable triggering, Grade 3: passively correctable triggering, and Grade 4: locked digit) were included.Citation34
Exclusion criteria
Patients with Quinnell’s Grade 1 and Grade 4 trigger digit were excluded from the study, and Grade 4 was referred for surgery. The exclusion criteria were as follows: traumatic trigger digit, age <18 years, rheumatoid arthritis, generalized polyarthritis, local infection, and history of malignancy, cervical pain, or previous surgery for trigger digit. Possible differential diagnoses such as infective tenosynovitis, metacarpophalangeal articular pathology, gamekeeper’s thumb, and Dupuytren’s contracture were excluded by clinical examination and ultrasound imaging.
Procedure and equipment
Treatment was administered by using the Storz Medical Masterplus® MP200 (Storz Medical, Tägerwilen, Switzerland) rESWT device. At each session, 2,000 impulses were applied to the painful area overlying the pathological flexor tendon at a frequency of 5–6 Hz. The device pressure varied from 1 to 3 bars depending on the patient’s individual pain tolerance; it was kept low enough to ensure that pain was tolerable, but high enough to have a therapeutic effect. Treatment sessions took place weekly until symptoms subsided, and thus, the total number of treatment sessions for each patient were based on the individual response to treatment.
Ultrasound gel was used for the transmission of shock-waves to the patient’s skin. No local anesthesia was administered as it is known to reduce the efficacy of ESWT.Citation27,Citation28,Citation35,Citation36 The painful area was covered in a longitudinal pattern starting at the point of maximum pain determined by patient’s feedback. At the end of each session, the patients were advised to use the finger normally, and they underwent no other treatments during the follow-up period of the study. All the patients were free to seek additional care (surgical consultation) if unsatisfied with improvement.
Outcome measures and follow-up
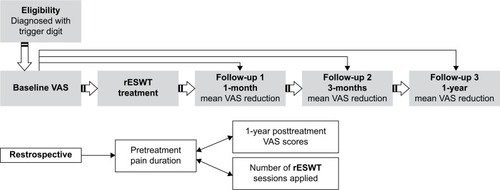
Patients were assessed at baseline (pretreatment) and at 1-, 3-, and 12-months follow-up appointments (posttreatment) when a full clinical examination was performed (). All patients were present during the follow-up period. The Roles and Maudsley score was used to assess functional outcome after rESWT treatment. This is a 4-point scale where 1 indicates an “excellent” result, 2 a “good” result, 3 a “fair” result, and 4 a “poor” posttreatment result. “Excellent” and “good” results were considered a success, meaning that the patients had full movement of the affected finger and activity was not restricted. “Fair” and “poor” results were considered a failure, bearing identical or even worse symptoms after rESWT treatment. These cases experienced some discomfort after prolonged activity or pain-limited activities.Citation37
Figure 1 Research study design and stages.
Abbreviations: rESWT, radial extracorporeal shockwave therapy; VAS, visual analog scale.
Pain severity was measured using the standard VAS. A score of 10 indicated maximum pain and 0 the minimum. Primary outcome measures were functional improvement and mean VAS reductions at 1-, 3-, and 12-months posttreatment compared with baseline. A VAS reduction of 60% was considered a clinically positive result. Recurrence of symptoms was defined as a 1-year follow-up VAS score of ≥2.
The individualized protocols were also retrospectively analyzed in terms of the number of sessions required and the pressure used (bars). To do this, additional outcome measures were used to assess correlations, first, between pretreatment symptom duration and the number of rESWT sessions required until recovery and, second, between pretreatment symptom duration and the 1-year posttreatment VAS score.
Statistics
Descriptive analysis was conducted, aiming at a comprehensive presentation of the patients’ demographics (such as age and sex) and the distribution of the affected hands and fingers. Total number of rESWT sessions required, shockwave impulses, and pressure and frequency used were retrospectively analyzed as means. Mean VAS scores were calculated at each follow-up interval, and mean VAS reductions were assessed from the percentage decrease in mean pain level from the pretreatment (baseline) VAS. Significant differences between baseline VAS and follow-up VAS scores were assessed by using Wilcoxon signed rank test, and Monte Carlo simulation was used to test statistical significance. Quartile statistics were also used to describe VAS variables as a nonparametric test was used.
In order to assess the relationship between pretreatment pain duration (in months), the number of rESWT sessions required, and the 1-year follow-up VAS score posttreatment, Spearman’s rank correlation coefficient was used.
A combination of Statistical Package for the Social Sciences Version 20 (IBM Corporation, Armonk, NY, USA) and Microsoft Excel (Microsoft Corporation, Redmond, WA, USA) was used to conduct all statistical analyses, and the confidence level was predefined at 95% (α =0.05) for all statistical analyses.Citation38,Citation39
Results
The average number of rESWT sessions required was 6±1.3 (ranging from 3 to 8). All the 44 subjects (49 digits) were treated with 2,000 impulses of shockwave per session at a mean pressure of 1.4±0.3 bar (ranging from 1 to 3) and a mean frequency of 5±0.4 Hz (ranging from 5 to 6; ).
Figure 2 Radial extracorporeal shockwave therapy mean impulses, mean pressure, mean frequency per session, and number of digits (fingers or thumbs) contributing to each successive session.
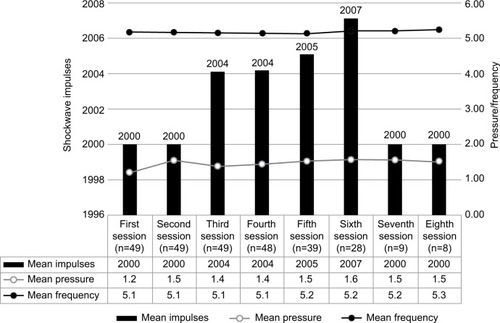
From the total of 49 digits, one (2%) received three sessions, nine (18.4%) received four sessions, 12 (24.5%) received five sessions, 20 (40.8%) received six sessions, and 7 (14.3%) received eight sessions.
According to the Roles and Maudsley score, 73.5% (36) of the patients stated their functional post-rESWT treatment condition as “excellent” and 20.4% (10) as “good” (). A “fair” functional post-rESWT treatment condition was stated in three cases (6.1%).
Table 2 Roles and Maudsley score functional radial extracorporeal shockwave therapy treatment results
A statistically significant reduction in VAS scores was found between baseline and 1-month follow-up (z=−6.212, P<0.001), between baseline and 3-month follow-up (z=−6.220, P<0.001), and between baseline and 1-year follow-up (z=−6.209, P<0.001). All the 49 cases had negative ranks with a mean rank of 25.00 in all cases. Pain score rating was 8.0 at baseline, 3.0 at 1-month posttreatment, and 1.0 both at 3-month and 1-year follow-up ( and ).
Figure 3 Radial extracorporeal shockwave therapy mean VAS reduction and average pain level at follow-up time intervals.
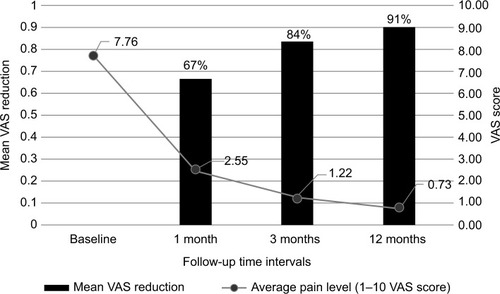
Table 3 Visual analog scale (VAS) scores means, standard deviation, and variance at baseline and follow-up
Three patients had recurrent symptoms at 1-year follow-up with the recurrence rate estimated at 6.1%; 34.7% (17 digits) had a VAS score of 0 (asymptomatic), 59.2% (29 digits) had a VAS score of 1.0, and 4.1% (two digits) had a VAS score of 2.0. In addition, no complications were reported in the subjects.
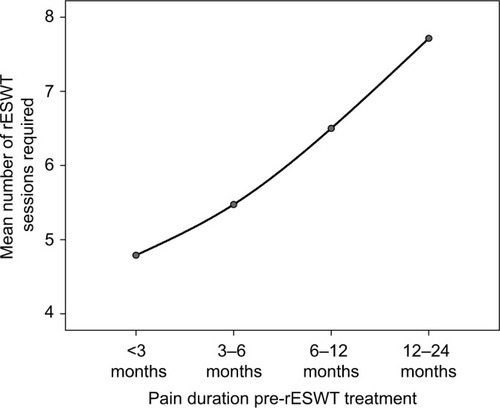
A strong positive Spearman’s ρ correlation was found between pre-rESWT treatment symptoms duration and the number of sessions required (r=0.776, P<0.001; ). Significant, positive, but weak correlation was also found to 1-year VAS with pretreatment symptoms duration (r=0.335, P=0.019).
Discussion
Trigger digit caused by fibrocartilaginous metaplasia of the tendon sheath can be a chronic and progressive condition.Citation1–Citation3 In the literature spontaneous recovery has been reported in 20%–29% of cases; however, in some untreated patients, the initial symptoms of intermittent pain, snapping or triggering progress over time, and long-standing cases may present with the affected finger or thumb locked in flexion.Citation1
According to the authors’ knowledge, this is the first study conducted to assess the effectiveness of rESWT for trigger digit. Evidence from previous studies has found that rESWT is effective in the treatment of multiple other tendinopathies.Citation19–Citation33,Citation40,Citation41 However, the specific biological mechanisms by which it induces therapeutic effects on pathological tendon tissue are not completely elucidated. Evidence from a recent study of human tendons suggested that the mechanical stimulus of ESWT aids tendon remodeling by promoting inflammatory and catabolic processes that are associated with the removal of damaged matrix constituents.Citation42 In vitro studies have further suggested that ESWT increases tendon healing through the stimulation of cell proliferation and motility, neovascularization, and expression of critical differentiation genes.Citation43 However, these in vitro findings cannot be automatically generalized to the in vivo conditions in human tendinopathies.
In the present study, statistically significant pain reductions (P<0.001) and functional improvements were found through all midpoints during the 1-year follow-up in 93.1% of cases, whereas only three patients had recurrent symptoms at 1-year posttreatment assessment. According to this initial evidence, rESWT was proven to be a suitable treatment for trigger digit. The analysis of the individualized treatment protocols demonstrated that longer pretreatment symptom duration was positively correlated with more sessions required until recovery (P<0.001) and a higher VAS score at 1-year posttreatment (P<0.05).
rESWT compared with traditional treatments for trigger digit
Of the currently accepted conservative treatments, including pain medications, orthoses, physiotherapy, and corticosteroid injection, corticosteroid injection is the most effective treatment. However, corticosteroid injection is effective in only 57% of the patients.Citation6 Moreover, symptom recurrence at 1 year after injection is reported to be 33%–56%,Citation14,Citation44,Citation45 and thus, surgery is often still required. The success rate is further decreased in certain patient groups, such as diabetics.Citation3,Citation44,Citation46 The present study, with a recurrence rate of only 6.1% at 1-year posttreatment, would indicate a better outcome with rESWT than corticosteroid injection and all other conservative methods.
Surgery is widely accepted as the definitive treatment for trigger digit, with remission of symptoms reported to be achieved in 97%–100% of cases.Citation14–Citation17 Consequently, in the present study, rESWT was offered only to the patients with Quinnell’sCitation34 Grade 2 or 3 trigger digit, and patients with Grade 4 were referred for surgery. Therefore, only the effectiveness of rESWT in the treatment of Grade 2 and 3 conditions was commented in the present study. For these cases of trigger digit, which are not yet a fixed deformity, the recurrence rate of only 6.1% at 1-year post-rESWT was reported. This suggests that rESWT is a promising, noninvasive alternative for the treatment of trigger digits before they become a fixed deformity (locked digit). rESWT is a conservative treatment modality without the longer recovery time and risk of complications such as nerve damage, infections, and painful scarring that are associated with surgery.Citation16,Citation17 Often quoted, minor complications of rESWT include bruising and redness. However, in the present study, no complications were reported, perhaps because a high pressure and high total energy flux density were not used.
Notably, in the present study, pain reductions continuously increased over the entire 1-year follow-up period. At 1-month posttreatment, the mean VAS score had reduced by 67% from baseline and at 12 months, it had reduced by 91%, providing excellent long-term efficacy of rESWT. Previous studies investigating shockwave therapy for various other tendinopathies have likewise demonstrated an increasing improvement in symptoms over the entire 1-year follow-up.Citation22,Citation27
Treatment protocol
Although multiple, high-quality studies have demonstrated that rESWT is safe and effective in the treatment of various tendinopathies,Citation19,Citation20,Citation22,Citation27–Citation31 controversy exists over the optimum treatment protocol that should be used in terms of shockwave generation (focused or radial), energy density, the number and frequency of treatments, method of localization (using anatomical landmarks, clinical focusing, or image-guided focusing), and the use of concomitant anaesthesia.Citation27,Citation29
In the present study, radial shockwaves were used because they allow the treatment of a larger tissue volume.Citation21,Citation26,Citation27,Citation30,Citation47 The pathologically changed painful area of tendon is relatively large in trigger digit compared to insertional tendinopathies. Thus, radial waves are advantageous as the pathologic tissue is included in the wave propagation area. Moreover, ultrasound or fluoroscopy guidance is not required with rESWT, making the application easier.Citation19,Citation26,Citation48 rESWT is also less painful than focused ESWT. This makes local anesthetic unnecessary and potentially improves treatment outcome as concomitant local anesthesia has been demonstrated to reduce ESWT efficacy.Citation27,Citation28,Citation35,Citation36
With regard to pressure and the number of sessions prescribed, the protocol used in the present study was individualized to each patient. It has been demonstrated that when rESWT is used for the treatment of tendinopathy, there must be a balance between pressure and the number of sessions required. The higher the pressure, the greater the treatment effects; thus, less sessions are required, but pain during the treatment increases. The lower the pressure, the more sessions are required to have a therapeutic effect.Citation49 Therefore, in the present study, pressure was set between 1.0 and 1.7 bars depending on each patient’s individual pain tolerance. The pressure was kept low enough to ensure that the pain was tolerable, but high enough to have a therapeutic effect.
The total number of sessions prescribed was determined when symptoms resolved and ranged from 3 to 8, depending on the patient’s individual response to treatment. Currently, there are no standardized guidelines for the number of rESWT sessions required when treating soft tissue conditions,Citation50 although studies have suggested that multiple applications provide superior long-term results compared with a single application.Citation51 Compared to other tendinopathies treated with rESWT, the finger is a rather painful area to treat. This might explain why comparatively low pressures have to be used.
Strengths of the study
This is the first retrospective cohort study to evaluate the effectiveness of rESWT for the treatment of stenosing tenosynovitis of the digital flexor tendon (trigger digit). All patients completed the 1-year follow-up. Individualization of the protocol might be a further strength and provides a possible explanation for the high efficacy of rESWT demonstrated in the present study compared to that reported by most previous studies on rESWT for tendinopathy. To the authors’ knowledge, all previous studies have applied a standardized number of treatments to the patients.
Limitations of the study
Patients with a prior symptom duration ranging from 1 to 24 months were included, whereas most previous studies on rESWT have only investigated its effectiveness for more chronic tendinopathies (such as those with a prior symptomatic period of at least 6 months).Citation20,Citation21,Citation27 As this study is a retrospective cohort study, it also has some inherent limitations that require consideration. There was no randomization, and there was no control group in this investigation. Furthermore, the number of subjects was relatively small in order to provide external validity to the present study. A comparative study with a control series will be more demonstrative.
Recommendations for the treatment of trigger digit with rESWT
The results demonstrate that there is no standard pressure or number of sessions that is suitable for everyone: some patients tolerate a higher pressure, and some require more treatments until recovery. With the individualized protocol, significant pain reductions were found and all patients found improvement. It was also found that pretreatment symptom duration is one of other possible factors that influence the number of sessions required by a patient. Shorter-term cases required fewer sessions and also had a lower VAS score at 1-year follow-up. Thus, the patients presenting with a longer history of symptoms need more rESWT sessions. According to the present study, varying the protocol according to each patient’s tolerance and response to treatment is the best way to treat tendinopathies with rESWT.
Conclusion
The present study provides initial evidence for the effectiveness of rESWT for the treatment of trigger digit. Randomized controlled trials are required to prove well the evidence of the rESWT effect.
Author contributions
Malliaropoulos N planned the study, performed the clinical work, and contributed to writing the manuscript. Jury R collected data, performed the literature review, and contributed to writing and editing the manuscript. Pyne D, Padhiar N, and Turner J contributed to writing the manuscript. Korakakis V and Lohrer H contributed to writing and editing the manuscript. Meke M conducted the statistical analysis and contributed to writing and editing the manuscript. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
The authors are grateful to Storz Medical, Lohstampfestrasse 8, 8274 Tägerwilen, Switzerland, for funding the open access publication article-processing charge. The abstract of this paper was presented at the 4th Annual Podiatric Sports Medicine Conference in Association with European College of Sports & Exercise Physicians, June 19–20, 2015, in London, UK. This paper received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. The authors affirm that this manuscript is an honest, accurate, and transparent account of the study being reported, that no important aspects of the study have been omitted, and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Disclosure
Lohrer H received research support and was a paid speaker from Storz Medical. The other authors report no conflicts of interest in this work.
References
- MooreJSFlexor tendon entrapment of the digits (trigger finger and trigger thumb)J Occup Environ Med200042552654510824306
- FarneboSChangJPractical management of tendon disorders in the handPlast Reconstr Surg20131325841e853e
- RyzewiczMWolfJMTrigger digits: principles, management, and complicationsJ Hand Surg Am200631113514616443118
- BlythMJRossDJDiabetes and trigger fingerJ Hand Surg Br19962122442458732409
- LaszloGJozsaPKHuman Tendons: Anatomy, Physiology and PathologyChampaign (IL)Human Kinetics Publishers1997
- FleischSBSpindlerKPLeeDHCorticosteroid injections in the treatment of trigger finger: a level I and II systematic reviewJ Am Acad Orthop Surg200715316617117341673
- GorscheRWileyJPRengerRBrantRGemerTYSasyniukTMPrevalence and incidence of stenosing flexor tenosynovitis (trigger finger) in a meat-packing plantJ Occup Environ Med19984065565609636936
- TreziesAJLyonsARFieldingKDavisTRIs occupation an aetiological factor in the development of trigger finger?J Hand Surg Br19982345395409726564
- ChammasMBousquetPRenardEPoirierJLJaffiolCAllieuYDupuytren’s disease, carpal tunnel syndrome, trigger finger, and diabetes mellitusJ Hand Surg Am19952011091147722249
- ChambersRGJrCorticosteroid injections for trigger fingerAm Fam Physician200980545419725485
- SalimNAbdullahSSapuanJHaflahNHOutcome of corticosteroid injection versus physiotherapy in the treatment of mild trigger fingersJ Hand Surg Eur Vol2012371273421816888
- BensonLSPtaszekAJInjection versus surgery in the treatment of trigger fingerJ Hand Surg Am19972211381449018627
- KerriganCLStanwixMGUsing evidence to minimize the cost of trigger finger careJ Hand Surg Am2009346997100519643287
- WangJZhaoJGLiangCCPercutaneous release, open surgery, or corticosteroid injection, which is the best treatment method for trigger digits?Clin Orthop Relat Res201347161879188623208122
- GilbertsECBeekmanWHStevensHJWereldsmaJCProspective randomized trial of open versus percutaneous surgery for trigger digitsJ Hand Surg Am200126349750011418913
- SatoESGomes Dos SantosJBBellotiJCAlbertoniWMFaloppaFTreatment of trigger finger: randomized clinical trial comparing the methods of corticosteroid injection, percutaneous release and open surgeryRheumatology2012511939922039269
- TurowskiGAZdankiewiczPDThomsonJGThe results of surgical treatment of trigger fingerJ Hand Surg Am19972211451499018628
- National Guideline CHand, wrist, and forearm disorders, not including carpal tunnel syndrome Available from: http://www.guideline.gov/content.aspx?id=34435Accessed March 23, 2015
- CacchioAPaoloniMBarileAEffectiveness of radial shock-wave therapy for calcific tendinitis of the shoulder: single-blind, randomized clinical studyPhys Ther200686567268216649891
- RompeJDCacchioAFuriaJPMaffulliNLow-energy extracorporeal shock wave therapy as a treatment for medial tibial stress syndromeAm J Sports Med201038112513219776340
- LohrerHSchollJArentzSAchillodynie und Patellaspitzensyndrom – Ergebnisse der Behandlung austherapierter, chronischer Fälle mit radialen Stoßwellen. [Achilles tendinopathy and patellar tendinopathy. Results of radial shockwave therapy in patients with unsuccessfully treated tendinoses]Sportverletz Sportschaden2002163108114 German12382183
- PettroneFAMcCallBRExtracorporeal shock wave therapy without local anesthesia for chronic lateral epicondylitisJ Bone Joint Surg Am20058761297130415930540
- ThielMApplication of shock waves in medicineClin Orthop Relat Res20013871821
- RompeJDKirkpatrickCJKullmerKSchwitalleMKrischekODose-related effects of shock waves on rabbit tendo Achillis. A sonographic and histological studyJ Bone Joint Surg Br19988035465529619954
- EngebretsenKGrotleMBautz-HolterEEkebergOMJuelNGBroxJISupervised exercises compared with radial extracorporeal shock-wave therapy for subacromial shoulder pain: 1-year results of a single-blind randomized controlled trialPhys Ther2011911374721088117
- GerdesmeyerLGollwitzerHDiehlPWagnerKRadial extracorporeal shockwave therapy (rESWT) in orthopaedicsJ Miner Stoffwechs2004113639
- GerdesmeyerLFreyCVesterJRadial extracorporeal shock wave therapy is safe and effective in the treatment of chronic recalcitrant plantar fasciitis: results of a confirmatory randomized placebo-controlled multicenter studyAm J Sports Med200836112100210918832341
- LohrerHNauckTDorn-LangeNVSchollJVesterJCComparison of radial versus focused extracorporeal shock waves in plantar fasciitis using functional measuresFoot Ankle Int20103111920067715
- van LeeuwenMTZwerverJvan den Akker-ScheekIExtracorporeal shockwave therapy for patellar tendinopathy: a review of the literatureBr J Sports Med200943316316818718975
- MagoschPLichtenbergSHabermeyerPRadiale Stoßwellentherapie der Tendinosis calcarea der Rotatorenmanschette – Eine prospektive Studie. [Radial shock wave therapy in calcifying tendinitis of the rotator cuff–a prospective study]Z Orthop Ihre Grenzgeb20031416629636 German14679427
- Avancini-DobrovicVFrlan-VrgocLStamenkovicDPavlovicIVrbanicTSRadial extracorporeal shock wave therapy in the treatment of shoulder calcific tendinitisColl Antropol201135Suppl 222122522220440
- CacchioARompeJDFuriaJPSusiPSantilliVDe PaulisFShock-wave therapy for the treatment of chronic proximal hamstring tendinopathy in professional athletesAm J Sports Med201139114615320855554
- MoenMHRayerSSchipperMSchmikliSWeirATolJLBackxFJShockwave treatment for medial tibial stress syndrome in athletes; a prospective controlled studyBr J Sports Med201246425325721393260
- QuinnellRCConservative management of trigger fingerPractitioner198022413401871907367373
- RompeJDMeurerANafeBHofmannAGerdesmeyerLRepetitive low-energy shock wave application without local anesthesia is more efficient than repetitive low-energy shock wave application with local anesthesia in the treatment of chronic plantar fasciitisJ Orthop Res200523493194116023010
- LabekGAuerspergVZiernholdMPouliosNBohlerNEinfluss von Lokalanästhesie und Energieflussdichte bei niederenergetischer Extrakorporaler Stoßwellentherapie der chronischen Plantaren Fasziitis. [Influence of local anesthesia and energy level on the clinical outcome of extracorporeal shock wave-treatment of chronic plantar fasciitis]Z Orthop Ihre Grenzgeb20051432240246 German15849646
- RolesNCMaudsleyRHRadial tunnel syndrome: resistant tennis elbow as a nerve entrapmentJ Bone Joint Surg Br19725434995084340924
- CohenJStatistical Power Analysis for the Behavioral Sciences2nd edNew JerseyLawrence Erlbaum Associates1988
- FaulFErdfelderELangAGBuchnerAG*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciencesBehav Res Methods200739217519117695343
- HarnimanECaretteSKennedyCBeatonDExtracorporeal shock wave therapy for calcific and noncalcific tendonitis of the rotator cuff: a systematic reviewJ Hand Ther200417213215115162101
- GerdesmeyerLWagenpfeilSHaakeMExtracorporeal shock wave therapy for the treatment of chronic calcifying tendonitis of the rotator cuff: a randomized controlled trialJama2003290192573258014625334
- WaughCMMorrisseyDJonesERileyGPLangbergHScreenHRIn vivo biological response to extracorporeal shockwave therapy in human tendinopathyEur Cell Mater201529268280 discussion 28025978115
- ViscoVVulpianiMCTorrisiMRFerrettiAPavanAVetranoMExperimental studies on the biological effects of extracorporeal shock wave therapy on tendon models. A review of the literatureMuscles Ligaments Tendons J20144335736125489555
- RozentalTDZurakowskiDBlazarPETrigger finger: prognostic indicators of recurrence following corticosteroid injectionJ Bone Joint Surg Am20089081665167218676896
- AndersonBKayeSTreatment of flexor tenosynovitis of the hand (‘trigger finge’) with corticosteroids. A prospective study of the response to local injectionArch Intern Med199115111531561985590
- BaumgartenKMGerlachDBoyerMICorticosteroid injection in diabetic patients with trigger finger. A prospective, randomized, controlled double-blinded studyJ Bone Joint Surg Am200789122604261118056491
- GerdesmeyerLMaierMHaakeMSchmitzCPhysikalisch-technische Grundlagen der extrakorporalen Stoßwellentherapie (ESWT). [Physical-technical principles of extracorporeal shockwave therapy (ESWT)]Orthopade2002317610617 German12219657
- KolkAYangKGTammingaRvan der HoevenHRadial extracorporeal shock-wave therapy in patients with chronic rotator cuff tendinitis: a prospective randomised double-blind placebo-controlled multicentre trialBone Joint J201395-B111521152624151273
- LeeSJKangJHKimJYKimJHYoonSRJungKIDose-related effect of extracorporeal shock wave therapy for plantar fasciitisAnn Rehabil Med201337337938823869336
- SpeedCAExtracorporeal shock-wave therapy in the management of chronic soft-tissue conditionsJ Bone Joint Surg Br200486216517115046427
- TakahashiNOhtoriSSaisuTMoriyaHWadaYSecond application of low-energy shock waves has a cumulative effect on free nerve endingsClin Orthop Relat Res200644331531916462457