Abstract
Patellofemoral pain (PFP) is a frequent cause of anterior knee pain in athletes, which affects patients with and without structural patellofemoral joint (PFJ) damage. Most younger patients do not have any structural changes to the PFJ, such as an increased Q angle and a cartilage damage. This clinical entity is known as patellofemoral pain syndrome (PFPS). Older patients usually present with signs of patellofemoral osteoarthritis (PFOA). A key factor in PFPS development is dynamic valgus of the lower extremity, which leads to lateral patellar maltracking. Causes of dynamic valgus include weak hip muscles and rearfoot eversion with pes pronatus valgus. These factors can also be observed in patients with PFOA. The available evidence suggests that patients with PFP are best managed with a tailored, multimodal, nonoperative treatment program that includes short-term pain relief with nonsteroidal anti-inflammatory drugs (NSAIDs), passive correction of patellar maltracking with medially directed tape or braces, correction of the dynamic valgus with exercise programs that target the muscles of the lower extremity, hip, and trunk, and the use of foot orthoses in patients with additional foot abnormalities.
Introduction
Patellofemoral pain (PFP) is the accepted term for localized pain of the anterior aspect of the knee.Citation1,Citation2 The prevalence of PFP is high;Citation1,Citation2 it affects 11–17% of patients who present to general practitioners.Citation1,Citation2 PFP is typically associated with activities that load the patella, such as ascending or descending stairs, jumping, running, and squatting.Citation1–Citation4 Other symptoms often associated with PFP are crepitus and mild/moderate joint effusion.Citation1
It was recently reported that ~25% of recreational athletes diagnosed with PFP will stop participating in sports because of knee pain.Citation5 PFP frequently affects running and jumping athletes.Citation6 In an observational study of 810 adolescent basketball players, the overall prevalence of PFP was 25%, with ~26% of female and 18% of male players affected.Citation6 Functional patellofemoral pain syndrome (PFPS), a synonym for nonspecific PFP,Citation7 was the most common diagnosis with an overall prevalence of 6.4%.Citation6 Other less common diagnoses included Sinding-Larsen-Johansson disease (4.8%), Osgood-Schlatter disease (2.5%), and plica syndrome (2.3%).Citation6 These observations show that PFP can affect patients with and without any structural damage to the patellofemoral joint (PFJ).Citation7 Structural damage that is sometimes associated with PFP includes chondral and osteochondral damage, osteoarthritis (OA), overuse injuries of the extensor apparatus (tendonitis and insertional tendinosis), and patellar instability.Citation9 It has been recommended that patients with a history of dislocations or subluxations should be considered separately from other patients with PFP because this subgroup of patients frequently have biomechanical risk factors that require different treatment approaches.Citation1 The same is true for those with overuse injuries of the extensor apparatus or cartilage damage.
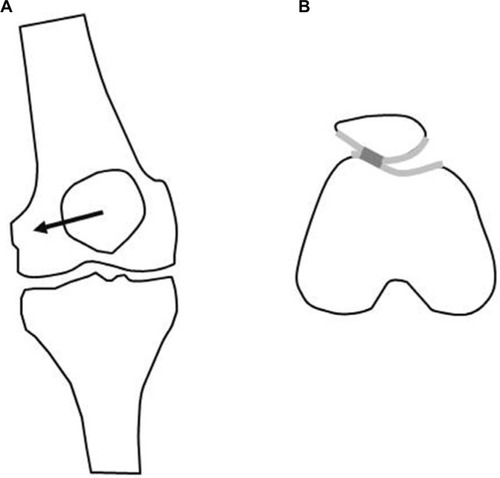
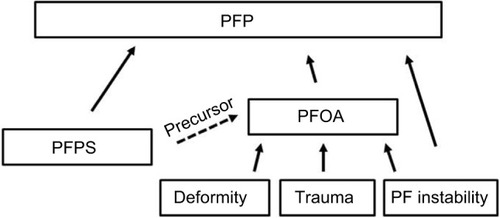
Nonspecific PFP is a common cause of “anterior knee pain” and mainly affects young athletes without any structural abnormalities.Citation7 Patellofemoral osteoarthritis (PFOA) predominantly affects older athletes with cartilage damage and bone marrow lesions.Citation7 Well-known causes of PFOA are trauma, deformity, and instability (). PFP and PFOA are two separate clinical entities. However, a recent systematic review suggested that nonspecific PFP in young patients could be a precursor to subsequent PFOA.Citation8
Figure 1 Schematic drawing showing the relationship of PFP, PFPS, and PFOA.
The purpose of this article is to summarize the evidence regarding the pathophysiology of nonspecific PFP and PFOA and to review the treatment of athletes with these conditions.
PFP pathophysiology or pathomechanics
Patella maltracking and PFP
A recent study using 3 T magnetic resonance imaging (MRI) demonstrated that structural abnormalities of the patellofemoral cartilage are not associated with PFP.Citation9 In this study, minor patellar cartilage defects or patellar bone marrow lesions were frequently seen in both PFP patients and subjects without PFP. These observations are in accordance with the findings of arthroscopic studies.Citation9
A recent systematic review examined the association of other PFJ imaging features, such as bisect offset, congruence angle, and patellar tilt, with PFP.Citation10 In this study, an increased MRI bisect offset, increased patellar tilt, and increased congruence angle under load and without load were associated with PFP.Citation10 All of these imaging parameters are indices of patellar maltracking.Citation7 This provides strong scientific evidence that PFP is associated with patellar maltracking.Citation10 Interestingly, both patellar tilt and bisect offset were increased when MRI was performed under load.Citation10 Wilson et alCitation11 used skin markers and an optoelectronic motion capture system to examine patellar glide in young patients with PFPS while in a standing position and while squatting. They found that the patellae of patients with PFPS had significantly increased lateral translation (maltracking), lateral patellar spin, and a tendency toward increased lateral tilt compared with the patellae of healthy subjects.Citation11 The observation that patellar maltracking is most severe in the upright or weight-bearing (squat) positions indicates that muscular activity is the primary determinant of patellar position in PFP patients.
Other studies have also investigated the association between patellar maltracking and PFP. The Health ABC study examined the relationship between patellar tracking and PFOA in a cohort of 3075 men and women aged between 70 and 79 years.Citation12 In this population, patellar maltracking was associated with PFOA progression.Citation12 Lateral displacement and patellar tilt predisposed to lateral PFOA progression, while medial displacement was predictive of medial PFOA progression.Citation12 Greater patellar tilt was associated with more severe pain.Citation12 In the Multicenter Osteoarthritis (MOST) and Framingham Osteoarthritis (FOA) studies, PFP was associated with lateral patellofemoral cartilage damage and concomitant bone marrow lesions but not with medial cartilage damage.Citation13 Similarly, a recent review concluded that there is strong evidence that PFOA is also associated with signs of patellofemoral instability, such as trochlear dysplasia and frontal plane knee alignment.Citation1
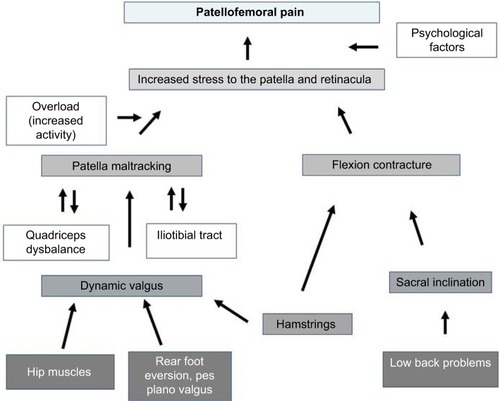
In conclusion, patellar maltracking plays a key role in patients with PFP related to PFPS or PFOA ().
Dynamic valgus
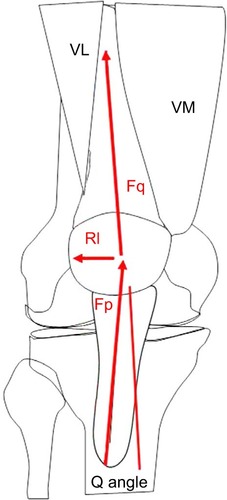
It is well known that the direction of the force generated by the quadriceps influences patellar tracking because the quadriceps force vector is lateral to the center of the joint line.Citation7,Citation14–Citation16 The quadriceps angle (Q angle) is a static measure of the quadriceps force vector.Citation7,Citation14 The Q angle is formed by a line from the anterior superior iliac spine to the midpoint of the patella and a line from the midpoint of the patella to the tibial tubercle ().Citation14 The normal value for this angle is 13.5 ± 4.5° (in healthy subjects between 18 and 35 years old).Citation14,Citation16 An increase in the Q angle increases the lateral force on the patella.Citation7,Citation14,Citation16 It has been shown that larger Q angles are associated with femoropatellar instability and with PFOA.Citation14,Citation15 However, the use of the Q angle to predict PFP is controversial. A recent systematic review reported that greater Q angles were associated with PFP,Citation17 but other studies have not found correlations between Q angle and PFP in young patients.Citation18–Citation21 This suggests that there may be a subgroup of patients in whom PFP is not the result of a structural fault.Citation7 This hypothesis is supported by Dierks et alCitation22 who showed that among runners with PFP, there was a subgroup of patients with functional knee valgus. The search for an explanation for this seeming contradiction (patellar maltracking without increased Q angle) led to the concept of a dynamic, or functional, valgus malalignment.Citation7
Figure 3 Schematic drawing showing the Q angle.
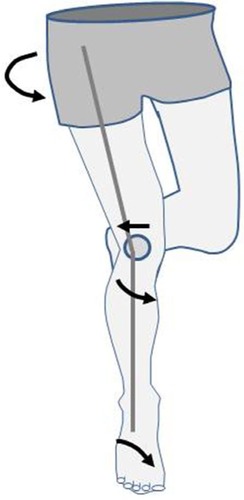
Myer et alCitation23 examined dynamic lower limb alignment in female middle- and high-school basketball players and found that the athletes who developed new PFP had increased knee abduction moments of the symptomatic limb. Nakagawa et alCitation24 found increased hip adduction and knee abduction in patients with PFPS. Souza and PowersCitation25 showed that females with PFPS demonstrated greater peak hip internal rotation compared with controls. These results highlight the existence of a subgroup of patients with PFP who do not have a structural valgus deformity but instead have a dynamic valgus malalignment caused by internal rotation of the femur and tibia ().Citation7 Several studies have shown that dynamic valgus malalignment is more frequently observed in female athletes than in male athletes;Citation6,Citation26,Citation27 this may explain the higher prevalence of PFP in young female athletes.Citation28
Figure 4 Drawing showing the dynamic valgus.
Dynamic valgus malalignment influences patellar tracking because the lateralized quadriceps force vector subsequently leads to lateralization of the patella.Citation29 Souza et alCitation29 measured femoral and patellar rotation in PFPS patients using open MRI and found that lateral rotation of the patella in females with PFPS was associated with excessive internal rotation, not torsion, of the femur. One-legged squats are a clinical test used to visualize dynamic valgus.Citation30 The one-legged squat task is a qualitative clinical assessment tool that is capable of identifying people with poor hip muscle function.Citation30 For this clinical test, participants are instructed to fold their arms across their chest and to squat down as far as possible five times consecutively, in a slow, controlled manner.Citation30 Based on five functional criteria (balance, trunk posture, pelvis posture, hip adduction, and knee valgus), the performance on the single leg squat is rated as good, fair, or poor.Citation30 Crossley et alCitation30 showed that the good performers exhibited greater hip abduction torque. Therefore, the one-legged squat can be clinically used to evaluate hip muscle function in patients with PFP.
Muscular dysfunction in PFP patients
There is strong evidence that muscular imbalances play a key role in the pathogenesis of PFP.Citation1 Many previous studies have focused on dysfunction of vastus medialis muscle and vastus lateralis muscle in PFP patients because these muscles attach directly to the patella.Citation31–Citation33 These studies have shown that an imbalance in the activation of m. vastus medialis obliquus and m. vastus lateralis correlates with lateral patellar tracking in PFP patients.Citation31–Citation33
Quadriceps dysfunction is also an important factor in PFOA.Citation1 Several studies have shown that quadriceps muscle size, strength, and force are impaired in patients with POA,Citation34–Citation37 and quadriceps weakness is considered a risk factor for PFOA.Citation1,Citation38 However, despite these results, it remains unclear whether quadriceps dysfunction is the primary cause of patellar maltracking.Citation7
There is some evidence in the literature for the involvement of additional muscular imbalances in PFP development.Citation7 Several studies have focused on hip muscle dysfunction because of the external rotators of the hip control femoral rotation.Citation39–Citation42 These studies have shown that dynamic valgus malalignment does not arise in the knee joint but rather through internal rotation of the femur owing to weakness of hip external rotators and abductors (m. gluteus medius and minimus).Citation39–Citation42 A systematic review demonstrated strong evidence that females with PFP have decreased hip abduction, external rotation, and extension strength compared with healthy controls.Citation42 Padua et alCitation43 showed that decreased strength of the hip abductors and external rotators is related to knee valgus after landing a drop jump. These results show that hip muscle dysfunction is probably an important factor in the pathogenesis of functional valgus malalignment in young patients with PFPS.
Some authors have also detected hip muscle dysfunction in patients with PFOA.Citation44,Citation45 Studies have demonstrated lower gluteus minimus and medius peak muscle forces and lower hip abductor strength compared with that of healthy controls.Citation44,Citation45 Other muscular abnormalities detected in PFP patients affect the iliotibial tract (m. tensor fascia latae) and the hamstrings.Citation7 The influence of the iliotibial tract on patellar trackingCitation46 may be anatomically explained by Kaplan’s fibers, which connect the iliotibial tract to the patella.Citation7
There is also some evidence in the literature that frontal plane knee alignment is not the only kinematic abnormality in patients with PFP. White et alCitation47 found significant hamstring tightness in patients relative to the control group. Patil et alCitation48 showed by electromyography that the lateral hamstrings of PFP patients contracted earlier than their medial hamstrings during isometric exercises. Besier et alCitation49 demonstrated that patients with PFPS have greater cocontraction of the quadriceps and hamstrings than do controls without symptoms of PFPS. By this mechanism, PFP patients might experience greater joint contact forces and joint stresses than healthy subjects. In addition, Tsuji et al found that elderly patients with PFP have less sacral inclination than healthy controls and referred this condition as “knee-spine syndrome”.Citation50 In a study by Teng et al, a higher knee flexion moment during the second half of the stance phase of gait was associated with PFOA progression.Citation51 However, although the studies reviewed here report several muscular imbalances that have been observed in patients with PFP, altered hip muscle function is considered to be the main cause of dynamic valgus malalignment in PFP patients.Citation7
Foot disorders
Hip muscle dysfunction is likely not the only factor contributing to dynamic valgus. There is strong evidence that, in some patients, foot disorders or deformities such as increased rear-foot eversion or pes pronatus valgus contribute to functional valgus.Citation52–Citation56 This deformity can cause internal rotation of the tibia in patients with PFPS.Citation34
A systematic review described the kinematic gait characteristics of patients with PFPS.Citation54 These gait characteristics included increased rearfoot eversion at heel strike, delayed timing of peak rearfoot eversion, and reduced rearfoot eversion range relative to controls.Citation52 Other studies have examined midfoot and forefoot abnormalities in patient with PFP.Citation53,Citation55 Mølsgaard et al also found increased navicular drop, navicular drift, and dorsiflexion in high-school students with PFP relative to unaffected students.Citation54 Barton et alCitation53 demonstrated that PFP patients had greater forefoot abduction than a healthy control group.
In conclusion, the literature provides evidence that in a subgroup of PFP patients, rearfoot and forefoot abnormalities contribute to the pathogenesis of dynamic valgus.
Psychological factors
Several studies have shown that pain and knee function can be associated with psychological factors in some patients with PFP.Citation57–Citation61 For example, Thomeé et alCitation61 found that the pain experience and pain coping in PFP patients were similar to those in other groups of patients with chronic pain. However, patients suffering from PFP had higher scores on the pain catastrophizing scale compared with other chronic pain patients. Similarly, Jensen et alCitation57 reported that patients with PFPS have greater levels of mental distress and worse self-perceived health than healthy subjects. Two studies have identified fear-avoidance beliefs about physical activity as a psychological predictor of pain and dysfunction in PFP patients.Citation60
In conclusion, there is evidence that psychological factors could modify the severity of PFP.
Neurophysiological sources of pain in patients with PFP
The exact source of the pain experienced by patients with PFP is unclear. Most likely the pain develops in the insertions of the extensor muscles or within the subchondral bone.Citation7 In an experimental arthroscopy performed using local skin anesthesia, a patient experienced strong pain when the probe touched their retinacula, Hoffas fat pad, or peripatellar synovium.Citation62 Several neurotransmitters, including substance P, neurofilament protein, S-100 protein, and neural growth factor, have been found within these structures.Citation63,Citation64 These findings suggest that retinacular innervation may play a key role in the development of anterior knee pain. However, there is also evidence that the pain may also originate in the subchondral bone; a PET CT study demonstrated increased metabolic bone activity in patients with PFP.Citation65
Therapy
Surgical treatment options for PFP
Nonsurgical therapy is the treatment of choice for PFPS in young patients.Citation7 Kettunen et alCitation64 performed a prospective, randomized trial to compare the outcome of arthroscopy combined with a home exercise program versus a home exercise program alone in patients with PFPS. Patients included in their study were between 18 and 40 years old and had persistent (>6 months) symptoms of PFP during jumping, running, squatting, or while going up or downstairs.Citation64 Exclusion criteria were OA, patellar instability, osteochondritis dissecans, and jumper’s knee.Citation64 The following procedures were performed arthroscopically: resection of the medial plicae, debridement of chondral lesions, partial synovectomy, and lateral release.Citation64 Fifty-six patients were included in the study and were randomized either to the arthroscopy plus exercise or to the exercise-only group.Citation64 The mean postintervention improvements in the Kujala knee score and VAS scale score for ascending and descending stairs were greater in the arthroscopy group than in the exercise-only group;Citation64 however, these differences were not statistically significant.Citation64 The health care costs for patients in the arthroscopy group were significantly higher than the costs for patients in the control group. The results of this study must be considered with caution because only 56 patients were included and thus the study might be underpowered.Citation64 With a larger patient population, the observed differences in the clinical scores probably would have been significant.Citation64 More criticism of this study includes the heterogeneity of the arthroscopic procedures that were actually performed (11 patients had no arthroscopic treatment, 11 patients underwent cartilage shaving, 5 patients underwent plica resection, 1 lateral release, and 2 partial meniscectomies). Only one patient had a grade IV cartilage defect, and all grade III cartilage defects were treated with debridement; thus, the results of this study are not valid for patients with severe cartilage defects. Severe cartilage defects may indicate that cartilage resurfacing procedures such as matrix-augmented chondrogenesis (AMIC) or autologous chondrocyte implantation (ACI) are required. The results of this prospective, randomized trial suggest that arthroscopy might not be the best first-line treatment for patients with PFPS. However, it is likely that a subgroup of patients exists who would benefit from arthroscopic surgery. This subgroup could include patients with structural joint damage such as grade III or IV cartilage defects or with lateral subluxation of the patella. In a previous study, Kettunen et alCitation65 showed that among patients with PFPS, those with severe lesions of the patellar cartilage or femoral trochlea subjectively reported more symptoms and functional limitations at followup than those with no lesions or with small cartilage lesions of the patella or femoral trochlea.
In patients with focal III and IV degrees chondral defects, two studies have reported good clinical results after ACI.Citation66,Citation67 In both of these studies, a tibial tubercle transfer and lateral release was used to treat patients with patellofemoral malalignment.Citation66,Citation67 In a long-term follow-up study, ACI in combination with anteromedialization of the tibial tuberosity resulted in significant amelioration of symptoms and improvement in function with a low incidence of adverse events in patients with isolated, symptomatic, patellar chondral defects after a mean follow-up period of more than 7 years.Citation68 When cartilage damage is associated with patellar instability, the PFJ should be stabilized by either MPFL reconstruction, tibial tuberosity transfer, or rotational osteotomy.Citation69
Surgical treatment options for PFOA
There is consensus that PFOA should be treated primarily non-operatively.Citation2,Citation70 Non-surgical treatment options for PFOA include exercise, knee realignment braces, patellofemoral taping, foot orthoses, and intra-articular injections of hyaluronic acid or platelet-rich plasma.Citation2,Citation70–Citation72 Surgical treatment is indicated if adequate pain relief cannot be achieved with non-surgical management. Surgical options for PFOA are anteromedial tibial tuberosity transfer or patellofemoral resurfacing.Citation73
Nonsurgical treatment options for PFP
Two recently published articles describe the guidelines for conservative management of PFP: These publications, the “2016 Patellofemoral Pain Consensus Statement” and the “Best Practice Guidelines”,Citation2,Citation74 both recommended interventions that include exercise, taping, bracing, foot orthoses, and combined therapies.Citation2,Citation74 In addition, the “Best Practice Guidelines” recommend acupuncture and patient education. In both publications, these interventions are recommended for young patients with PFPS and for patients with PFOA.Citation2 However, PFP treatment should be individualized for each patient; not all patients will require all treatments but scientific evidence to guide the tailoring of interventions is very limited.Citation2,Citation74
Exercise
Most authors agree that exercise therapy is the treatment of choice for patients with PFP.Citation2,Citation74 Exercise has been the most well-studied form of PFPS therapy and should aim to correct the dynamic valgus malalignment that occurs in many patients.Citation7 Five recently published systematic reviews concluded that exercise had a positive effect on pain and function in patients with PFP.Citation75–Citation79 The most effective intervention programs included exercises targeting the hip external rotator and abductor muscles and knee extensor muscles. However, positive results have also been described for exercises that target only muscles acting on the knee and hip.Citation75–Citation79 One study showed a positive effect of trunk stabilization exercises, which targeted core muscles such as the rectus abdominis. The results of previous studies suggest that, if knee and hip exercises are recommended, then the patient should begin with the more proximal exercises because they have greater benefit and may cause fewer adverse effects.Citation2,Citation74
A positive clinical effect has been described for active stretching exercises, ergometer exercise, squats, static quadriceps exercises, leg presses, active leg raises and lowers, and climbing exercises.Citation7,Citation75–Citation79 Open- and closed-chain, balance, and neuromuscular training programs have been described.Citation7,Citation75–Citation79 The most frequent duration of the exercise programs was 6 weeks, and the exercises were generally conducted two to four times daily with 10 repetitions per exercise session.Citation7,Citation75–Citation79 Both supervised and home-based exercise programs have been described.Citation7,Citation75–Citation79 In several studies, additional interventions such as restriction of symptom-inducing activities, tape, braces, and nonsteroidal anti-inflammatory drugs (NSAIDs) were allowed.Citation7
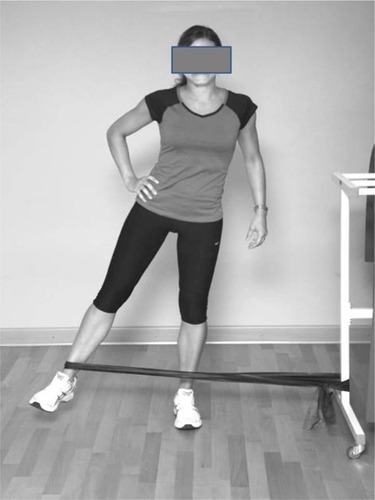
In summary, there is strong evidence that a targeted exercise program is an effective treatment for PFP.Citation7 Exercises to treat PFP should target the muscles of the hip, knee (quadriceps and hamstrings), trunk, and the iliotibial tract ().
Pharmacological therapy
The “Best Practice Guidelines” recommend that immediate pain relief should be a priority to gain patient trust.Citation74 A Cochrane review from 2004 concluded that there was limited evidence that NSAIDs effectively reduced acute anterior knee pain in PFPS patients.Citation7,Citation80 More recent systematic reviews of pharmacological treatments for PFP are lacking. The OARSI guideline for the nonoperative treatment of knee OA recommend the use of selective or nonselective NSAIDs for patients without comorbidities.Citation70 Thus, despite the limited evidence supporting their use, NSAIDs may be appropriate in patients with PFOA.
Correction of patellar maltracking by taping
Taping is a popular treatment for athletes with PFPS,Citation81–Citation83 in part because the tape strips do not hinder sporting activity. Classical taping technique is different from Kinesio taping.Citation84
The most popular classical taping technique for PFPS treatment was described by McConnellCitation85 (). The aim of McConnell taping is to correct lateral patellar maltracking and patellar tilt by applying adhesive strips to the skin.Citation85 This technique has been recommended for athletes with PFPS for use during training and competition.Citation81
Figure 6 Tape applications for patients with PFP.
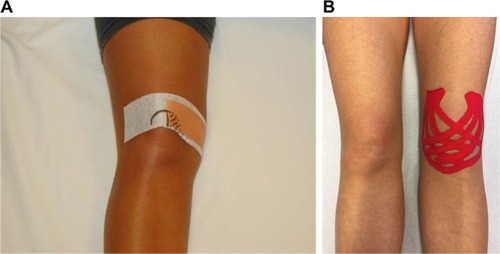
A recent systematic review concluded that there is moderate evidence that customized classical taping provides pain reduction that is superior to that provided by untailored tape application, and there is limited evidence that tailored taping provides better pain relief than exercise alone after 4 weeks of each intervention.Citation83 There was also evidence that tailored taping stimulated earlier m. vastus medialis activation relative to m. vastus lateralis activation.Citation83 These findings suggest that in addition to its biomechanical effects, taping may also have neuromotor effects.Citation83 However, the finding that even sham tape application produces a clinically meaningful reduction in knee pain in patients with PFPS suggests that placebo or sensory skin effects may contribute to the benefits of taping.Citation86 It should be noted that the effects of tape on pain reduction have only been investigated in short-term studies (12-week follow-up).Citation7,Citation83 The long-term effects of tape on anterior knee pain have not been established. Therefore, current evidence supports the use of tape for temporary pain relief in the treatment of anterior knee pain in PFPS patients,Citation83 but the benefits of long-term taping have not been established. According to the “2016 Patellofemoral Pain Consensus Statement” and the “Best Practice Guidelines”, tailored classical tape application can be recommended in combination with other treatments, such as exercise.Citation2,Citation74
During the past few years, the use of Kinesio tape has become increasingly popular (). Kinesio taping uses a different approach than classical taping; in Kinesio taping, the elastic tape strips are used to increase the space between muscle and fascia. In this way, Kinesio taping can stimulate cutaneous mechanoreceptors and improve knee proprioception.Citation81 The tape can either stimulate muscle activity or prevent muscle overuse, depending on how it is applied.Citation87
A recently published systematic review compared studies that used Kinesio taping with studies that used the classic McConnell taping technique.Citation81 This review reported that both taping techniques had a positive effect on pain and quality of life, while meta-analysis showed that Kinesio taping provided more effective pain relief than McConnell taping.Citation81 However, both methods work in different ways. Kinesio taping increases muscle flexibility, improves motor function, and has a moderate effect on muscle activity in PFPS patients compared with controls.Citation81 Meta-analysis has shown a small effect on pain reduction and motor function improvement and a moderate effect on muscle activity, in PFPS patients treated with Kinesio taping.Citation81 The positive effects of McConnell taping have been attributed to correction of patellar maltracking.Citation81 The authors of this systematic review concluded that both patellar taping techniques can be useful in the treatment of PFPS patients.Citation81
Patellar braces
A disadvantage of taping is that its effects decrease over time. Patellar braces are an alternative option; these apply an external, medially directed force that may counteract lateral patella maltracking ().Citation7 Biomechanical studies have shown that patellar braces can alter patellar tracking. Draper et alCitation88 demonstrated using real-time MRI that a knee brace could reduce patellar lateralization and tilt in women with PFPS. Becher et alCitation89 demonstrated that a dynamic realignment brace significantly affected the reduction in the three patellar height ratios, patellar tilt angle, and bisect offset, as well as TT–TG distance. This dynamic realignment brace (Agilium Patella pro; Otto Bock, Duderstadt, Germany) applies a medially directed force only when the knee is flexed to between 0 and 30°, which is when the patella is not stabilized by the trochlea. Callaghan et alCitation90 have shown that use of a patellar brace alters position and increases contact area between the patella and the femoral trochlea in patients with patellofemoral OA.
Figure 7 Example of a patella realignment brace (Agillium Patella pro; Otto Bock, Duderstdt, Germany).

A 2015 meta-analysis found insufficient evidence to recommend the use of knee braces in the treatment of patients with PFPS.Citation91 However, two recently published, prospective, randomized studies did demonstrate a positive effect of knee braces in patients with PFPS and PFOA. Callaghan et alCitation92 demonstrated that a patellar brace (Bioskin Patellar Tracking Q Brace; Ossur UK, Manchester, England) relieved knee pain in patients with PFOA. This was attributed to a reduction in the volume of bone marrow lesions in the targeted compartment of the knee. Petersen et alCitation93 examined the effect of a dynamic realignment brace (Patella pro) in patients with PFPS. After 6 and 12 weeks of treatment, they found that use of the brace led to better outcomes in patients with PFPS than exercise alone.Citation93 However, 1 year later, this positive effect had diminished.Citation93 The results of both of these randomized trials suggest that the use of realignment braces in patients with PFP is justified.
Foot orthotics
Foot abnormalities such as increased rearfoot eversion and pes pronatus can favor internal rotation of the tibia and create a functional malalignment of the leg.Citation7 Therefore, insoles or foot orthotics may be a treatment option for patients with PFP.Citation7 A systematic review published in 2010 found limited evidence that prefabricated foot orthoses reduce the range of transverse plane knee rotation, which has been associated with short-term improvements in individuals with PFP.Citation94 A recently published systematic review of 11 clinical studies demonstrated that the use of foot orthotics had significant effects on pain and function in patients with PFP.Citation95 This review also identified a slight effect of foot orthoses on lower limb kinematics and muscle activation.Citation95 However, other studies have not found any effects of foot orthoses on clinical outcome in patients with PFP.Citation96 This heterogeneity in study results demonstrates that there may be substantial variations in individual responses to this treatment and that foot orthoses may not be beneficial for all patients with PFP.Citation2 Patients with foot abnormalities, such as those with increased rearfoot eversion or pes pronatus, may benefit the most from foot orthotics. Therefore, foot orthoses might be a treatment option for patients with the combination of disorders of foot posture and PFPS.Citation7
Conclusion
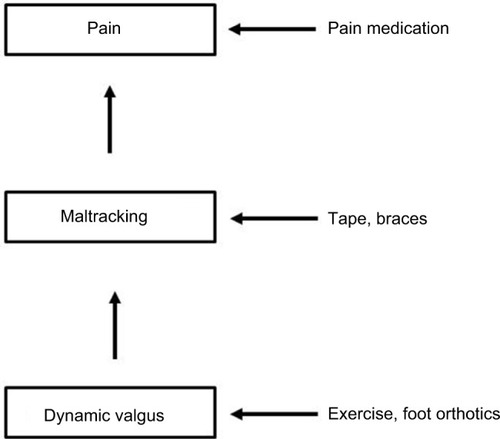
The existing evidence regarding the pathogenesis of PFP can be summarized in an algorithm shown in . Patellar maltracking owing to a functional malalignment or dynamic valgus may be an underlying cause of PFP. Possible causes of functional valgus may be decreased hip muscle strength or foot abnormalities. Secondary consequences include quadriceps imbalance, hamstring tightness, or iliotibial tract tightness (). The clinical significance of these findings is that an individually tailored, multimodal treatment plan for each patient based on their underlying pathology is necessary. Options for this treatment plan include exercise programs that target the muscles of the lower extremity, hip, and trunk, patellar taping or bracing, foot orthoses, and the short-term use of NSAIDs (). The greatest evidence exists for exercises. If the clinical examination shows signs of hip muscle weakness, these muscles should be addressed. Foot orthoses might be a treatment option for patients with the combination of disorders of foot posture and PFPS. Bracing and taping can support patella tracking. NSAIDs should be used for acute episode of pain.
Figure 8 Algorithm for the pathogenesis of PFPS.
Abbreviation: PFPS, patellofemoral pain syndrome.
Disclosure
Wolf Petersen, Ingo Rembitzki, and Christian Liebau receive consultant fees from Otto Bock Health Care (Duderstadt, Germany). The authors report no other conflicts of interest in this work.
References
- CrossleyKMStefanikJJSelfeJPatellofemoral pain consensus statement from the 4th International Patellofemoral Pain Research Retreat, Manchester. Part 1: terminology, definitions, clinical examination, natural history, patellofemoral osteoarthritis and patient-reported outcome measuresBr J Sports Med2016501483984327343241
- CrossleyKMvan MiddelkoopMCallaghanMJPatellofemoral pain consensus statement from the 4th International Patellofemoral Pain Research Retreat, Manchester. Part 2: recommended physical interventions (exercise, taping, bracing, foot orthoses and combined interventions)Br J Sports Med2016501484485227247098
- ClementDBTautonJESmartGWMcNicolKLA survey of overuse running injuriesPhys Sportsmed198191475827453020
- DierksTAManalKTHamillJDavisILower extremity kinematics in runners with patellofemoral pain during a prolonged runMed Sci Sports Exerc201143469370020798656
- RathleffMSRasmussenSOlesenJLUnsatisfactory long-term prognosis of conservative treatment of patellofemoral pain syndromeUgeskr Laeger2012174151008101322487407
- FossKDMyerGDMagnussenRAHewettTEDiagnostic differences for anterior knee pain between sexes in adolescent basketball playersJ Athl Enhanc2014311814182025362859
- PetersenWEllermannAGösele-KoppenburgAPatellofemoral pain syndromeKnee Surg Sports Traumatol Arthrosc201422102264227424221245
- ThomasMJWoodLSelfeJPeatGAnterior knee pain in younger adults as a precursor to subsequent patellofemoral osteoarthritis: a systematic reviewBMC Musculoskelet Disord20101120121020828401
- van der HeijdenRAde KanterJLBierma-ZeinstraSMStructural abnormalities on magnetic resonance imaging in patients with patellofemoral pain: a cross-sectional case-control studyAm J Sports Med20164492339234627206691
- DrewBTRedmondACSmithTOPennyFConaghanPGWhich patellofemoral joint imaging features are associated with patellofemoral pain? Systematic review and meta-analysisOsteoarthritis Cartilage201624222423626471209
- WilsonNAPressJMKohJLHendrixRWZhangLQIn vivo noninvasive evaluation of abnormal patellar tracking during squatting in patients with patellofemoral painJ Bone Joint Surg Am200991355856619255215
- HunterDJZhangYQNiuJBPatella malalignment, pain and patellofemoral progression: the Health ABC StudyOsteoarthritis Cartilage200715101120112717502158
- StefanikJJGrossKDGuermaziAThe relation of MRI-detected structural damage in the medial and lateral patellofemoral joint to knee pain: the Multicenter and Framingham Osteoarthritis StudiesOsteoarthritis Cartilage201523456557025575967
- SheehanFTDerasariAFineKMBrindleTJAlterKEQ-angle and J-sign: indicative of maltracking subgroups in patellofemoral painClin Orthop Relat Res2010468126627519430854
- MacriEMStefanikJJKhanKMIs tibiofemoral or patellofemoral alignment or trochlear morphology associated with patellofemoral osteoarthritis? A systematic reviewArthritis Care Res (Hoboken)201668101453147026814979
- HortonMGHallTLQuadriceps femoris muscle angle:normal values and relationships with gender and selected skeletal measuresPhys Ther198969111721
- LankhorstNEBierma-ZeinstraSMvan MiddelkoopMFactors associated with patellofemoral pain syndrome: a systematic reviewBr J Sports Med201347419320622815424
- ParkSKStefanyshynDJGreater Q angle may not be a risk factor of patellofemoral pain syndromeClin Biomech (Bristol, Avon)2011264392396
- AlmeidaGPSilvaAPFrançaFJMagalhãesMOBurkeTNMarquesAPmQ-angle in patellofemoral pain: relationship with dynamic knee valgus, hip abductor torque, pain and functionRev Bras Orthop2016512181186
- KwonOYunMLeeWCorrelation between intrinsic patellofemoral pain syndrome in young adults and lower extremity biomechanicsJ Phys Ther Sci201426796196425140074
- PappasEWong-TomWMProspective predictors of patellofemoral pain syndrome: a systematic review with meta-analysisSports Health20124211512023016077
- DierksTAManalKTHamillJDavisILower extremity kinematics in runners with patellofemoral pain during a prolonged runMed Sci Sports Exerc201143469370020798656
- MyerGDFordKRBarber FossKDThe incidence and potential pathomechanics of patellofemoral pain in female athletesClin Biomech (Bristol, Avon)2010257700707
- NakagawaTHMoriyaETMacielCDSerrãoFVTrunk, pelvis, hip, and knee kinematics, hip strength, and gluteal muscle activation during a single-leg squat in males and females with and without patellofemoral pain syndromeJ Orthop Sports Phys Ther201242649150122402604
- SouzaRBPowersCMDifferences in hip kinematics, muscle strength, and muscle activation between subjects with and without patellofemoral painJ Orthop Sports Phys Ther2009391121919131677
- FordKRMyerGDHewettTEValgus knee motion during landing in high school female and male basketball playersMed Sci Sports Exerc200335101745175014523314
- FordKRMyerGDTomsHEHewettTEGender differences in the kinematics of unanticipated cutting in young athletesMed Sci Sports Exerc200537112412915632678
- FulkersonJPThe etiology of patellofemoral pain in young, active patients: a prospective studyClin Orthop Relat Res1983179129133
- SouzaRBDraperCEFredericsonMPowersCMFemur rotation and patellofemoral joint kinematics: a weight-bearing magnetic resonance imaging analysisJ Orthop Sports Phys Ther201040527722785
- CrossleyKMZhangWJSchacheAGBryantACowanSMPerformance on the single-leg squat task indicates hip abductor muscle functionAm J Sports Med201139486687321335344
- CavazzutiLMerloAOrlandiFCampaniniIDelayed onset of electromyographic activity of vastus medialis obliquus relative to vastus lateralis in subjects with patellofemoral pain syndromeGait Posture201032329029520727760
- ChenHYChienCCWuSKLiauJJJanMHElectromechanical delay of the vastus medialis obliquus and vastus lateralis in individuals with patellofemoral pain syndromeJ Orthop Sports Phys Ther201242979179622951377
- CowanSMBennellKLHodgesPWCrossleyKMMcConnellJDelayed onset of electromyographic activity of vastus medialis obliquus relative to vastus lateralis in subjects with patellofemoral pain syndromeArch Phys Med Rehabil200182218318911239308
- HartHFAcklandDCPandyMGCrossleyKMQuadriceps volumes are reduced in people with patellofemoral joint osteoarthritisOsteoarthritis Cartilage201220886386822525223
- PeatGDuncanRCWoodLRJClinical features of symptomatic patellofemoral joint osteoarthritisArthritis Res Ther20121426369
- FarrokhiSPivaSRGilABOddisCVBrooksMMFitzgeraldGKAssociation of severity of coexisting patellofemoral disease with increased impairments and functional limitations in patients with knee osteoarthritisArthritis Care Res (Hoboken)201365454455123045243
- FokLASchacheAGCrossleyKMLinYCPandyMGPatellofemoral joint loading during stair ambulation in people with patellofemoral osteoarthritisArthritis Rheum20136582059206923740512
- AminSBakerKNiuJQuadriceps strength and the risk of cartilage loss and symptom progression in knee osteoarthritisArthritis Rheum200960118919819116936
- Baldon RdeMNakagawaTHMunizTBAmorimCFMacielCDSerrãoFVEccentric hip muscle function in females with and without patellofemoral pain syndromeJ Athl Train200944549049619771287
- BolglaLAMaloneTRUmbergerBRUhlTLHip strength and hip and knee kinematics during stair descent in females with and without patellofemoral pain syndromeJ Orthop Sports Phys Ther2008381121618349475
- BrentJLMyerGDFordKRHewettTEA longitudinal examination of hip abduction strength in adolescent males and femalesMed Sci Sports Exerc2008393445
- PrinsMRvan der WurffPFemales with patellofemoral pain syndrome have weak hip muscles: a systematic reviewAust J Physiother200955191519226237
- PaduaDAMarshallSWBeutlerAIPredictors of knee valgus angle during a jump-landing taskMed Sci Sports Exerc200537398404
- CrossleyKMDornTWOzturkHvan den NoortJSchacheAGPandyMGAltered hip muscle forces during gait in people with patellofemoral osteoarthritisOsteoarthritis Cartilage201220111243124922885566
- PohlMBPatelCWileyJPFerberRGait biomechanics and hip muscular strength in patients with patellofemoral osteoarthritisGait Posture201337344044423047017
- WuCCShihCHThe influence of iliotibial tract on patellar trackingOrthopedics200427219920314992387
- WhiteLCDolphinPDixonJHamstring length in patellofemoral pain syndromePhysiotherapy2009951242819627682
- PatilSDixonJWhiteLCJonesAPHuiACAn electromyographic exploratory study comparing the difference in the onset of hamstring and quadriceps contraction in patients with anterior knee painKnee201118532933220724165
- BesierTFFredericsonMGoldGEBeaupréGSDelpSLKnee muscle forces during walking and running in patellofemoral pain patients and pain-free controlsJ Biomech200942789890519268945
- BartonCJLevingerPMenzHBWebsterKEKinematic gait characteristics associated with patellofemoral pain syndrome: a systematic reviewGait Posture200930440541619651515
- BartonCJLevingerPWebsterKEMenzHBWalking kinematics in individuals with patellofemoral pain syndrome: a case-control studyGait Posture201133228628921194952
- BartonCJLevingerPCrossleyKMWebsterKEMenzHBThe relationship between rearfoot, tibial and hip kinematics in individuals with patellofemoral pain syndromeClin Biomech (Bristol, Avon)2012277702705
- BartonCJBonannoDLevingerPMenzHBFoot and ankle characteristics in patellofemoral pain syndrome: a case control and reliability studyJ Orthop Sports Phys Ther201040528629620436240
- MølgaardMRathleffMSSimonsenOPatellofemoral pain syndrome and its association with hip, ankle, and foot function in 16- to 18-year-old high school students: a single-blind case-control studyJ Am Podiatr Med Assoc2011101321522221622633
- JensenRHystadTBaerheimAKnee function and pain related to psychological variables in patients with long-term patellofemoral pain syndromeJ Orthop Sports Phys Ther200535959460016268247
- JensenRHystadTKvaleABaerheimAQuantitative sensory testing of patients with long lasting patellofemoral pain syndromeEur J Pain200711666567617204440
- PivaSRFitzgeraldGKWisniewskiSDelittoAPredictors of pain and function outcome after rehabilitation in patients with patellofemoral pain syndromeJ Rehabil Med200941860461219565153
- PivaSRFitzgeraldGKIrrgangJJAssociates of physical function and pain in patients with patellofemoral pain syndromeArch Phys Med Rehabil200990228529519236982
- ThomeéPThomeéRKarlssonJPatellofemoral pain syndrome: pain, coping strategies and degree of well-beingScand J Med Sci Sports200212527628112383072
- DyeSFThe pathophysiology of patellofemoral pain: a tissue homeostasis perspectiveClin Orthop Relat Res2005436100110
- Sanchis-AlfonsoVRoselló-SastreEImmunohistochemical analysis for neural markers of the lateral retinaculum in patients with isolated symptomatic patellofemoral malalignment. A neuroanatomic basis for anterior knee pain in the active young patientAm J Sports Med2000285725731
- WojtysEMBeamanDNGloverRAJandaDInnervation of the human knee joint by substance-P fibersArthroscopy1990642542631702291
- DraperCEFredericsonMGoldGEPatients with patellofemoral pain exhibit elevated bone metabolic activity at the patellofemoral jointJ Orthop Res201230220921321812024
- KettunenJAHarilainenASandelinJKnee arthroscopy and exercise versus exercise only for chronic patellofemoral pain syndrome: a randomized controlled trialBMC Med20075384518078506
- KettunenJAVisuriTHarilainenASandelinJKujalaUMPrimary cartilage lesions and outcome among subjects with patellofemoral pain syndromeKnee Surg Sports Traumatol Arthrosc20051323134
- EbertJRFallonMSmithAJanesGCWoodDJProspective clinical and radiologic evaluation of patellofemoral matrix-induced autologous chondrocyte implantationAm J Sports Med20154361362137225784629
- MeyerkortDEbertJRAcklandTRMatrix-induced autologous chondrocyte implantation (MACI) for chondral defects in the patellofemoral jointKnee Surg Sports Traumatol Arthrosc201422102522252324817164
- GilloglySDArnoldRMAutologous chondrocyte implantation and anteromedialization for isolated patellar articular cartilage lesions: 5- to 11-year follow-upAm J Sports Med201442491292024519181
- PetersenWForkelPAchtnichAChronic patellofemoral instabilityUnfallchirurg2012115539740922588526
- McAlindonTEBannuruRRSullivanMCOARSI guidelines for the non-surgical management of knee osteoarthritisOsteoarthritis Cartilage201422336338824462672
- CampbellKAEricksonBJSaltzmanBMIs local viscosupple-mentation injection clinically superior to other therapies in the treatment of osteoarthritis of the knee: a systematic review of overlapping meta-analysesArthroscopy201531102036204525998016
- MeheuxCJMcCullochPCLintnerDMVarnerKEHarrisJDEfficacy of intra-articular platelet-rich plasma injections in knee osteoarthritis: a systematic reviewArthroscopy201632349550526432430
- MosierBAArendtEADahmDLDejourDGomollAHManagement of patellofemoral arthritis: from cartilage restoration to arthroplastyJ Am Acad Orthop Surg20162411163173
- BartonCJLackSHemmingsSTufailSMorrisseyDThe ‘Best Practice Guide to Conservative Management of Patellofemoral Pain’: incorporating level 1 evidence with expert clinical reasoningBr J Sports Med2015491492392325716151
- HarvieDO’LearyTKumarSA systematic review of randomized controlled trials on exercise parameters in the treatment of patellofemoral pain: what works?J Multidiscip Healthc2011438339222135495
- Alba-MartínPGallego-IzquierdoTPlaza-ManzanoGRomero-FrancoNNúñez-NagySPecos-MartínDEffectiveness of therapeutic physical exercise in the treatment of patellofemoral pain syndrome: a systematic reviewJ Phys Ther Sci20152772387239026311988
- PetersJSTysonNLProximal exercises are effective in treating patellofemoral pain syndrome: a systematic reviewInt J Sports Phys Ther20138568970024175148
- ThomsonCKrouwelOKuismaRHebronCThe outcome of hip exercise in patellofemoral pain: a systematic reviewMan Ther20162613027428378
- van der HeijdenRALankhorstNEvan LinschotenRBierma-ZeinstraSMvan MiddelkoopMExercise for treating patellofemoral pain syndromeCochrane Database Syst Rev20151CD01038725603546
- HeintjesEBergerMYBierma-ZeinstraSMBernsenRMVerhaarJAKoesBWPharmacotherapy for patellofemoral pain syndromeCochrane Database Syst Rev20043CD003470
- ChangWDChenFCLeeCLLinHYLaiPTEffects of Kinesio Taping versus McConnell Taping for patellofemoral pain syndrome: a systematic review and meta-analysisEvid Based Complement Alternat Med2015201547120826185517
- WardenSJHinmanRSWatsonMAJrAvinKGBialocerkowskiAECrossleyKMPatellar taping and bracing for the treatment of chronic knee pain: a systematic review and meta-analysisArthritis Rheum2008591737818163413
- BartonCBalachandarVLackSMorrisseyDPatellar taping for patellofemoral pain: a systematic review and meta-analysis to evaluate clinical outcomes and biomechanical mechanismsBr J Sports Med201448641742424311602
- CampoloMBabuJDmochowskaKScariahSVarugheseJA comparison of two taping techniques (Kinesio and McConnell) and their effect on anterior knee pain during functional activitiesInt J Sports Phys Ther20138210511023593548
- CallaghanMJSelfeJPatellar taping for patellofemoral pain syndrome in adultsCochrane Database Syst Rev20124CD006717
- McConnellJA novel approach to pain relief pre-therapeutic exerciseJ Sci Med Sport20003332533411101271
- OsorioJAVairoGLRozeaDGThe effects of two therapeutic patellofemoral taping techniques on strength, endurance, and pain responsesPhys Ther Sport201314419920623557728
- DraperCEBesierTFSantosJMUsing real-time MRI to quantify altered joint kinematics in subjects with patellofemoral pain and to evaluate the effects of a patellar brace or sleeve on joint motionJ Orthop Res200927557157718985690
- BecherCSchumacherTFleischerBEttingerMSmithTOstermeierSThe effects of a dynamic patellar realignment brace on disease determinants for patellofemoral instability in the upright weight-bearing conditionJ Orthop Surg Res20151012626282268
- CallaghanMJGuneyHReevesNDA knee brace alters patella position in patellofemoral osteoarthritis: a study using weight bearing magnetic resonance imagingOsteoarthritis Cartilage201624122055206027432215
- SmithTODrewBTMeekTHClarkABKnee orthoses for treating patellofemoral pain syndromeCochrane Database Syst Rev201512CD010513
- CallaghanMJParkesMJHutchinsonCEA randomised trial of a brace for patellofemoral osteoarthritis targeting knee pain and bone marrow lesionsAnn Rheum Dis20157461164117025596158
- PetersenWEllermannARembitzkiIVEvaluating the potential synergistic benefit of a realignment brace on patients receiving exercise therapy for patellofemoral pain syndrome: a randomized clinical trialArch Orthop Trauma Surg2016136797598227146819
- BartonCJMunteanuSEMenzHBCrossleyKMThe efficacy of foot orthoses in the treatment of individuals with patellofemoral pain syndrome: a systematic reviewSports Med201040537739520433211
- AhlhelmAAlfuthMThe influence of foot orthoses on patellofemoral pain syndrome: a systematic analysis of the literatureSportverletz Sportschaden201529210711725675398
- HossainMAlexanderPBurlsAJobanputraPFoot orthoses for patellofemoral pain in adultsCochrane Database Syst Rev20111CD008402