 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background: Hypertension is the leading risk factor for global mortality. Isometric resistance exercise training reduces blood pressure (BP). However, the protocols used are often limited by cost/immobility and the use of rigid exercise modalities. In response, a novel more versatile, isometric exercise (IE) device, the IsoBall (IB) was created.
Purpose: The aim of this study was to test the BP-lowering effectiveness of this prototype.
Methods: Twenty-three healthy participants (29.10±2.19 years old, 173.95±3.83 cm, 75.43±5.06 kg, SBP 127.10±10.37 mmHg, DBP 70.40±6.77 mmHg) were randomly allocated to either a control group (CON) or 2 isometric handgrip (IHG) training groups that used the Zona plus (ZON) and IB devices. The intervention groups completed 3 sessions each week of 4, 2 min IHG at 30% maximal voluntary contraction, with a 1-min rest, for 4 weeks. Resting BP, heart rate (HR) and IHG strength were measured in all groups at baseline and postintervention.
Results: Postintervention systolic BP (SBP) was significantly lower in both ZON (114.5±8.2 mmHg, p = 0.000) and IB (119.9±7.0 mmHg, p = 0.000) compared to control (131.0±12.4 mmHg). Postintervention diastolic BP (DBP) was reduced in both intervention groups (ZON 66.6±7.4 mmHg, p = 0.004; IB 65.7±10.0 mmHg, p = 0.012) compared to CON (71.1±8.8 mmHg). Mean arterial pressure (MAP) was reduced in both groups (ZON 82.6±6.8 mmHg, p = 0.000; IB 84.3±9.1 mmHg, p = 0.000) compared to control (91.0±9.7 mmHg). No significant changes were seen in HR or strength (p > 0.05).
Conclusion: The results of this study indicate that both the ZON and IB devices elicit significant SBP, DBP and MAP reductions. Despite the ZON group having larger reductions in BP, no significant differences were found between the two devices. Thus, this study indicates the IB device to be an effective alternative to the ZON that can also be used to perform other IE modalities.
Introduction
Globally, hypertension is estimated to affect ~30% populationCitation1 and is the leading risk factor for global mortality causing an estimated 9.4 million deaths a year.Citation2 Hypertension is a major risk factor in the development of cardiovascular disease (CVD) and coronary heart disease (CHD).Citation3,Citation4 A reduction in blood pressure (BP) is associated with a reduced risk of developing CVD.Citation5,Citation6 The significant public health burden that hypertension represents highlights the importance of effective antihypertensive treatments.
Despite the proven efficacy of pharmacological antihypertensive treatments,Citation7 less than 50% of medicated hypertensives adhere to treatment for numerous reasons, including deleterious side effects, and many often fail to achieve clinical targets.Citation8–Citation10 These, together with the high cost of hypertension to the national health service (NHS), make lifestyle modification treatments essential. Lifestyle modification treatments are a widely recommended approach to reduce BP.Citation11 These interventions include weight reduction, dietary alterations including sodium and alcohol restriction, and increased physical activity.Citation12 These treatments have no deleterious side effects and are comparatively low in cost.Citation13
As noted above, increased physical activity is a cornerstone lifestyle modification for hypertension management, with guidelines around the world overwhelmingly recommending aerobic exercise training with dynamic resistance training as an adjuvant intervention.Citation14–Citation18 Recently, isometric handgrip (IHG) training (a form of isometric resistance exercise training (IET)) has been introduced into formal guidelines, most notably by the American College of Cardiology and the American Heart Association in their 2017 Guidelines.Citation14 To date, IET interventions have consisted of a limited number of exercises, with the most studied being IHG interventions.Citation19–Citation27 IET generally consists of four, 2-minutes (min) isometric contractions, separated by brief rest periods.Citation28 IHG training is most often performed at 30% of maximal voluntary contraction (MVC), three times per week,Citation14,Citation28 over a period of 8–10 weeks;Citation28 however, several studies have reported significant BP reductions using shorter, 4-week, intervention.Citation23,Citation24,Citation27,Citation29,Citation30–Citation32 Other protocols, such as double and single leg extensions,Citation27,Citation29,Citation33–Citation35 isometric wall squatCitation30 and the maximal intermittent (MINT) handgrip protocolCitation36 have also been found to reduce BP.
Numerous randomized control trials and meta-analyses have found IET to elicit significant reductions in resting blood pressure (RBP) in those with and without hypertension.Citation19–Citation21,Citation27,Citation29,Citation30,Citation37,Citation38 Early evidence suggests that IET also reduces 24-hours (hrs) ambulatory BP.Citation39
As with many BP-lowering treatments, and for reasons not yet entirely understood, not everyone responds to IET similarly. Inherent participant characteristics together with training intensity may all play a role in response efficacy. For example, individuals with higher pre-training RBP, older individuals and individuals who have a high pre-training BP reactivity response appear most responsive to IET.Citation19,Citation27,Citation40–Citation42 IET appears ineffective in well-controlled medicated hypertensivesCitation25 and the role of gender is unclear;Citation19,Citation39,Citation41 however, there is evidence to suggest that older women may be more responsive.Citation43 With respect to the latter, the equivocal nature of the findings to date may reflect the higher initial gender-specific baseline pressures and/or the small number of women collectively studied to date in IET trials. Finally, there is evidence to suggest that low-intensity short duration IET (isometric leg) interventions may be insufficient to cause RBP reduction.Citation33,Citation44
Regarding IET’s efficacy compared to other exercise interventions, Cornelissen et alCitation45 noted reductions of 13.5 mmHg systolic pressure and 6.1 mmHg diastolic pressure following IET, with post-training reductions of ~5/4 mmHg cited in the most recent meta-analysis.Citation19 These reductions are similar to those seen in traditional dynamic exercise interventions, both aerobic and resistance, despite the lower time to perform the exercise bouts.Citation37 The lower time commitment (as little as 12 min) coupled with the simplicity of the intervention, and the lower cost, may contribute to increased adoption of and adherence to the intervention.Citation37 Making IET interventions, particularly IHG training, more applicable for those individuals with mobility issues. It should also be noted that IET interventions have been found to yield beneficial results when performed unsupervised in the participants home,Citation30 which may further contribute to increased adherence rates.
Each IET program utilizes equipment and protocols designed specifically for that exercise (eg, handgrip dynamometers), or immobile equipment (isokinetic dynamometers) that are expensive and/or not available outside medical/academic institutions. These factors may restrict accessibility to IET and those with mobility limitations may not be able to perform specific IET exercises or travel to a location with specialized equipment. In response, a multidisciplinary research team at the University of Greenwich has developed a versatile isometric device that can be used to perform any number of isometric exercises (IE). This work has resulted in the development of a prototype novel IE device designated the IsoBall (IB). The IB device was developed using several criteria, including low cost, high versatility and ease of transport/mobility. These criteria were used in order to increase the applicability, accessibility, adherence and initiation rates.Citation46–Citation48
The aim of the current study was to investigate the concept and efficacy of this device using the most widely studied and efficacious IET protocol (IHG training, four, 2-min contractions separated by a 1-min rest at 30% MVC, 3 times a weekCitation14,Citation28), and the one included in the ACC/AHA 2017 Guidelines.Citation14 It was hypothesized that the IB device would elicit similar significant BP reductions when compared to a traditional computerized handgrip dynamometer following a 4-week intervention.
Method
Twenty-three healthy participants were recruited via poster and email advertisements (). Sample size was calculated using G*power (version 3.1.9.2, Germany). Effect size data, relating to SBP, form several meta-analysis was used to estimate sample size.Citation19,Citation37,Citation45 The results of this analysis indicate the need for n=26, to achieve a β≥0.95 and α≤0.05. Participants reported not taking any medications known to effect cardiovascular function during the study. All female participants reported using oral contraception. Ethical approval was granted by the University Research Ethics Committee (UREC/16.2.5.14) at the University of Greenwich.
Table 1 Participants’ baseline characteristics
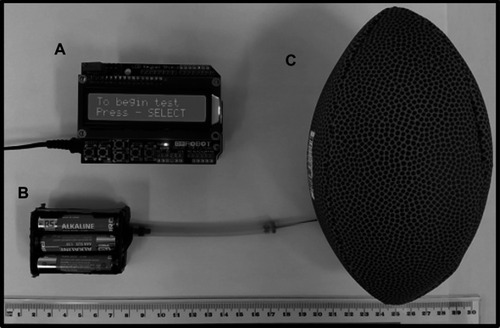
After providing written informed consent, participants were randomly allocated to one of three groups, using a counterbalanced simple randomization method by a third-party researcher. These groups were the control (CON) group, the ZON group that completed the intervention using the Zona plus (Zona plus Series 3, Zona Health Inc, USA) device and the IB group that used the novel ball device () attached to a mini size Rugby ball (British & Irish Lions replica, Rhino, UK) to complete the intervention. Intervention groups’ familiarization sessions consisted of RBP measurements, handgrip strength tests (Str) and 1 bout of IHG exercise (four, 2-min IHG contractions performed at 30% MVC using alternating hands, with each IHG contraction separated by a 1-min rest period). Participants completed the familiarization sessions using either the IB or the ZON depending upon group allocation. Control group familiarization sessions consisted of only RBP measures, as the use of IET has been found to effect BP after one session.Citation49 Two familiarization sessions were used to ensure participants were completely comfortable with all protocols and with having their BP measured, these sessions were separated by ≥24 hrs. Participant’s stature (Seca 213 stadiometer, Seca GmBH, Germany) and mass (Seca 861 weight scales, Seca GmBH, Germany) were measured during the first familiarization session. At least 24 hrs after the last familiarization session, baseline testing occurred to assess RBP, heart rate (HR) and Str. After baseline testing, participants in the intervention groups (ZON; IB) were required to train 3 times per week for 4 weeks. All training sessions were completed within the University of Greenwich’s laboratory, under supervision. Each training session involved four, 2-min IHG contractions at 30% MVC separated by 1 min, each 2-min IHG contraction was performed in alternate hands. Post-training assessments of RBP, HR and Str were performed ≥24 hrs following the last training session. Participants randomized to the CON group performed no IHG training and returned to the laboratory for post-testing 4 weeks following their pre-testing session. Each of the training and assessment sessions was separated by ≥24 hrs, and sessions were conducted at the same time of day to avoid circadian rhythm effects.
Figure 1 (A) IB visual display and processing unit. (B) IB pressure sensor unit with needle valve adaptor. (C) Mini size rugby ball.
Participants were instructed to abstain from caffeine and nicotine for >2 hrs prior to testing and from alcohol >24 hrs prior to testing. Participants were asked to maintain their habitual diet and exercise habits throughout the study period, and this was confirmed verbally prior to the initiation of each testing session. Participants were tested at the same of time of day, with the temperature controlled between 19°C and 23°C, and ambient noise kept to a minimum.
Equipment
Briefly, the IB device works by sensing the pressure exerted on the ball attached to the pressure sensor via the needle valve adaptor (). This data is sent via Bluetooth to the visual display and processing unit (), which displays visual feedback to participants, informing them to either apply more or less pressure. Upon initial start-up of the device, an automatic MVC protocol is completed, consisting of a single 5-second (s) maximal contraction. The MVC data is used by the device to calculate the intensity (30% MVC). Preliminary testing found the device to be highly correlated with calculated values (y=0.3277x+1.0199 R2=0.9814), indicating it to be an accurate method of controlling IE intensity.
Measurement procedures
Resting blood pressure and heart rate
RBP (systolic BP (SBP); diastolic BP (DBP)) and HR measurements were recorded from the participant’s non-dominant arm (Intellisense M3, Omron Healthcare Co, Japan), in a supine position. BP was collected supine, as this allowed for more comfortable and controllable positioning of the participants. The positioning was selected based on previous research.Citation50,Citation51 Briefly, Vischer and BurkardCitation50 and Pickering et alCitation51 describe how BP changes based upon body position, and note that whichever position (seated or supine) selected should be adhered to throughout all subsequent readings. Thus, the methods used for BP measurements were based upon these studiesCitation50,Citation51 and collected as follows. Participants’ supine with the BP cuff placed directly onto the skin so that the bottom of the cuff was 2–3 cm above the antecubital fossa area of the nondominant arm. The arm was supported so that it rested at the midpoint between the bed and the sternum to align with the right atrium. The participant was relaxed throughout with their legs uncrossed. All data was acquired following bladder voiding and a 10-min quiet rest period. Readings were taken in triplicate with a 60-s period between each reading and the average of the three readings were calculated for data analysis. Mean arterial pressure (MAP) was calculated using the following equation:
Handgrip strength
IHG strength was measured using a digital hand grip dynamometer (Grip-D, T.K.K 5401, Takei, Japan) as per published protocol.Citation52 Instantaneous MVC for each hand (right-handgrip strength (StrR) and left-handgrip strength (StrL)) were obtained in triplicate, alternating hand after each test. A 60-s rest period separated each reading.
Statistical analysis
All statistical analyses were performed using Excel (Excel 2013, Microsoft office professional plus 2013, Microsoft corp, USA) and the Statistical Package for the Social Sciences (SPSS version 24, IBM corp, USA), with α set at p ≤ 0.05. Shapiro–Wilk analysis was performed to establish data distribution. An ANCOVA test was performed to ascertain if there was a significant difference in the amount each group changed over the course of the intervention when controlling for baseline measures. Post-hoc Bonferroni tests were performed to establish between group differences. Individual response data is reported using the methods described in HopkinsCitation53; these data are reported in standardized units to 95% CIs.
Results
All participants in the intervention groups completed 12 IET sessions with a 100% adherence rate. No changes in diet or exercise were indicated. All outcome data were found to be normally distributed (p ≥ 0.05).
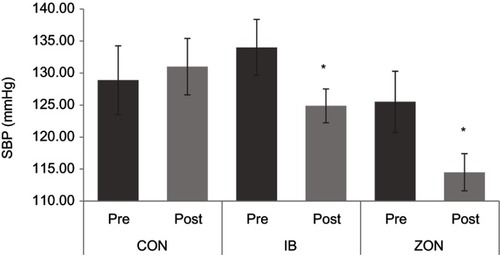
An ANCOVA test revealed that baseline SBP levels were significantly related to postintervention SBP levels (F (1, 23) = 79.63, p = 0.000, r = 0.95). After controlling for the covariate (baseline SBP) a significant effect was found (F (2, 23) = 24.14, p = 0.000, ηp2 = 0.71). The post-hoc Bonferroni test indicates the significant difference to be between the intervention groups (IB, 119.9±7.0 mmHg, p = 0.000; ZON, 114.5±8.2 mmHg, p = 0.000) and the control group (131.0±12.4 mmHg). No significant difference was apparent between the IB and ZON groups (p = 0.620, see . Individual standardized SBP response data indicate the IB (0.62±0.66) to have experienced a trivial to very large change and the ZON (0.72±0.28) group experienced moderate to very large change.
Figure 2 Pre- to post-systolic blood pressure (SBP) mean ± standard error.
Abbreviations: CON, control; IB, IsoBall; ZON, Zona.
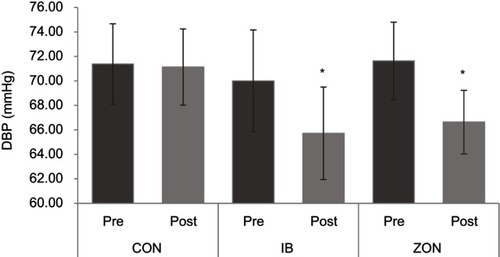
Postintervention, DBP data was also found to be significantly related to baseline measures (F (1, 23) = 229.259, p = 0.000, r = 0.70). After controlling for baseline DBP levels, a significant effect was found (F (2, 23) = 8.624, p = 0.000, ηp2 = 0.47). The post-hoc test revealed a significant difference (p = 0.012) between postintervention IB (65.7±10.0 mmHg) and CON (71.1±8.8 mmHg); there was also a significant difference between CON and ZON (66.6±7.4 mmHg, p = 0.004). No significant difference was found between the two intervention groups (IB and ZON, p = 1.000, see . Individual DBP response was trivial to large in the IB group (0.46±0.43) and small to large responses in the ZON group (0.56±0.34).
Figure 3 Pre- to post-diastolic blood pressure (DBP) mean ± standard error.
Abbreviations: CON, control; IB, IsoBall; ZON, Zona.
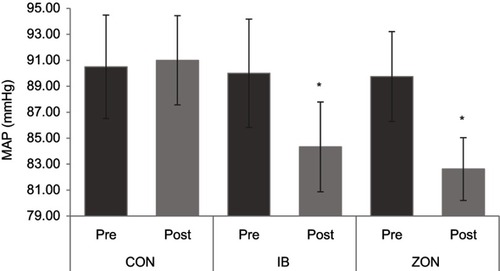
Postintervention MAP data was also found to be significantly related to preintervention MAP results (F (1, 23) = 227.662, p = 0.000, r = 0.85). After controlling for this, a significant intervention effect was found (F (2, 23) = 22.374, p = 0.000, ηp2 = 0.70). The post-hoc tests revealed a significant difference between each intervention group (IB 84.3±9.1 mmHg, p = 0.000; ZON 82.6±6.8 mmHg, p = 0.000) and control (91.0±9.7 mmHg). No significant difference was found between the intervention groups (p = 0.750). . MAP individual responses indicate the IB to cause trivial to large (0.50±0.43) responses, with small to very large responses seen in the ZON group (0.63±0.54).
Figure 4 Pre- to post-mean artierial pressure (MAP) mean ± standard error.
Abbreviations: CON, control; IB, IsoBall; ZON, Zona.
No significant differences (p > 0.05) were observed in any other parameters measured. Data values for all parameters collected over the 4-weeks of IET intervention are summarized in .
Table 2 Mean and SD values for all parameters measured, for each group, preintervention and postintervention
Discussion
The primary aim of this study was to evaluate the concept and efficacy of the prototype IB using the widely studied IHG training protocol against a commercially available equivalent (ZON). Despite the ZON eliciting larger BP reductions in all parameters, the non-significant differences between the two devices confirm the hypothesis that both devices would elicit similar significant BP reductions compared to control. The BP results presented in this study are in line with previous IHG studies conducted over similar durations of 4-weeks,Citation24,Citation27 5-weeks,Citation24,Citation54 and 6-weeks.Citation21,Citation55,Citation56 It is difficult to say whether the increase in control group SBP values contributed to the statistical significance of the reductions after isometric training. The reductions in both of the isomeric training groups were of a magnitude that was similar (if not greater) than many of the previous intervention studies, which average approximately 5.99 mmHg SBP and 3.94 mmHg DBP reduction.Citation19,Citation37
It should be noted that BP reductions following IHG appear not to be associated with age or gender in young, healthy adults.Citation40 This can be seen in studies that have directly compared male and female participants and deduced no gender difference. Somani et alCitation39 and Hanik et alCitation57 noted no difference in the magnitude of BP reduction following IHG between male and female participants, indicating IET to be equally effective in both genders. However, these studies were performed using young (mid-twenties) participants. In older postmenopausal women, greater BP reductions have been found than those seen in age-matched men.Citation41,Citation43,Citation58 These findings are in agreement with previous research showing that the amount to which BP is reduced by IET is dictated by initial BP.Citation19,Citation40 That is to say, participants with higher initial BP experience greater reductions post-IET. Thus, it could be concluded that hypertensives will experience greater reductions in BP than normotensives. Due to the small sample size and baseline differences apparent between the male and female participants within this study, no investigations or conclusions can be conducted or drawn from the current data.
Regarding HR and handgrip strength, the results of the present study are consistent with the majority of previous IHG research in normotensive and hypertensive populations in finding no significant change in HR or strength.Citation22–Citation27,Citation41,Citation59 These results may be due to the intensity used not causing a great enough stimulus to elicit strength gains. Indeed, the current study and those that have previously reported no change in handgrip strength have all utilized similar IHG protocols.Citation22–Citation27,Citation41,Citation59 This is however, a speculative comment and studies investigating this phenomenon are warranted.
As well as statistical significance, it is also important to consider clinical importance, in order to convey further clinical insight.Citation60,Citation61 Clinical importance is established using Minimal Clinically Important Difference (MCID).Citation60 MCID is considered the smallest effect required to produce clinically important results.Citation62 Limited data is available on MCID in regard to BP; however, several papers have found reductions of ≥2 mmHg SBP and DBP could reduce CHD and stroke risk.Citation63,Citation64 Neaton et al. 1995 cited inCitation65 Indeed, Cook et alCitation64 noted a 2 mmHg DBP reduction would result in a 17% reduced risk of hypertension, 6% reduction in CHD risk and a 15% reduction in stroke risk. Neaton et al (1995 cited inCitation65) estimated this same reduction (−2 mmHg SBP) would reduce cardiovascular disease risk by 5% and all-cause mortality by 3%. These potential effects were also estimated in Stamler et alCitation65 noting a 2 mmHg SBP reduction leading to −4% risk of CHD, −6% risk of stroke and −3% risk of all-cause mortality. Using ≥2 mmHg as the MCID for both SBP and DBP, the results of the present study show that 93.33% of the participants in the intervention groups achieved the ≥2 mmHg SBP goal (87.50% ZON and 100% IB). A 86.66% experienced a ≥2 mmHg DBP in both intervention groups (87.50% ZON and 85.71% IB). These findings are in line with previous literature that noted MCID rates of 60–96% in unmedicated individuals.Citation37 Despite these MCID data, individual response data indicate there to be a small to very large effect on SBP when IHG is performed with either the IB or the ZON devices. Small to very large effect on ZON DBP and MAP data, with trivial to large DBP and MAP changes, is seen in the IB group data. These large variations in the individual response data are likely due to the small sample size.
One aspect of the IB that differentiates it from other IE devices is its versatility. The IB device can be attached to any ball via a needle valve adaptor; this enables the shape and size of the ball to be changed allowing for a wide variety of possible exercises to be performed. Such versatility may have adherence implications. Previous exercise adherence research has noted several factors that may dissuade individuals from initiating and maintaining physical activity programs. Factors include lack of time, boredom, location and difficulty of the exercise.Citation46,Citation47,Citation48 All of these factors are overcome with IE as the interventions used require a short time commitment, at a low intensity and can be performed virtually anywhere. The final aspect, variety of exercise, is yet to be tested. Despite this, numerous IE modalities have been used to elicit BP reductions. Most common among these exercises is IHGCitation20–Citation27,Citation39,Citation41,Citation66; however, both single leg and double leg extension have also been used to significantly reduce BP,Citation33–Citation35,Citation44,Citation67,Citation68 with other, more novel, exercises also appearing in the literature, for instance, Howden et alCitation68 found isometric arm curls efficacious at reducing BP, Bentley et alCitation36,Citation69 noting significant BP reductions with a high-intensity handgrip and MINT protocols and Wiles et alCitation30 noting significant reductions following an isometric wall squat intervention. This variety of IE used in the previous research alludes to the plausibility that a multiexercise isometric program may be efficacious at reducing BP as well as having a positive influence on adherence rates. This remains to be tested; however, the IB device offers a method of controlling isometric intensity throughout a variety of exercise protocols, thus offering a low-cost and mobile method of conducting/prescribing such an intervention.
As the IB device was developed as an alternative to the currently available isometric intensity controlling devices, it is worth briefly comparing the IB to other devices. The IB prototype was developed at a build cost of approximately £150 which is substantially less than the Zona plus series 3 device (used in this study) that is priced at £549.00.Citation70 Currently, the Zona device is similar in size to the IB and thus is as mobile. The Zona is, however, limited as only one type of IE (IHG) can be performed with the device, thus limiting its use by individuals with hand mobility issues such as arthritis. Low-cost grip dynamometers can be purchased for ~£20 and IHG can be performed with these devices; yet, they are limited to one type of IE and can be cumbersome. More versatile devices such as isokinetic dynamometers are viable options for performing a variety of IE; however, these devices are also limited by both cost and immobility limiting their applicability. Other more novel devices such as the bend and squat deviceCitation30 are interesting options; however, again, this device is limited to one specific type of IE.
The next stage of the development of the IB is to link it to a smartphone application via a Bluetooth link. This has the potential to decrease the cost of a production version, allowing greater flexibility in the display, tracking of performance and increasing patient compliance with engagement through games.
The main limitation of the study was our slightly smaller than target sample size. Despite failing to recruit the estimated sample size by three participants (n=23 vs 26), the study proceeded as a proof of concept/pilot study. Importantly, a post-hoc power analysis using SBP as the primary measure indicated a power of 0.99 with the achieved sample size of n=23. Another limiting factor of the study is the lack of menstrual cycle control. Generally, BP fluctuates with the phases of the menstrual cycle, with higher BP occurring during the follicular phase (0- to 14-day postmenstruation) and lower BP during the luteal phase (−14 to −1 days prior to menstruation).Citation71 In normotensive participants, fluctuations of ±5.2 mmHg SBP and ±2.1 mmHg DBP have been found,Citation72 with other studies finding smaller ranges of ±1.45 mmHg SBP and ±0.55 mmHg DBP.Citation71 It is likely that this factor influenced the results of this study; however, as the participant population consisted of both men and women, research has shown that this effect is smaller than the BP reduction found in this study. Given that numerous other IHG studies, conducted using both male and female participants, have found similar effects to those presented in this study,Citation20,Citation22,Citation23,Citation27,Citation57 it is unlikely that the results presented here are entirely due to this factor. Finally, the inclusion of a placebo/sham intervention group would have strengthened the results of this study. However, due to the use of a proven device (ZON), it was concluded that this would be unnecessary. It should be noted that this is a common issue to IE research with very few studies including a sham/placebo group.
Further studies should be conducted using the IB device, and these studies should aim to increase the evidence for the efficacy of the IB device and utilize the adaptability of the device to create a variety of effective IE programs. Studies should also aim to investigate the efficacy of a multiexercise isometric program. Further studies should also continue to investigate the efficacy of home-based interventions as these data remain scarce.
Conclusion
In conclusion, despite the ZON eliciting greater reductions in BP, the novel IE device (IB) also elicited significant reductions in all resting BP parameters similarly to the ZON with no significant differences between the two devices. Therefore, the IB device should be further tested and used in future studies as a diverse, low-cost and portable method for controlling IE intensity aimed at reducing BP.
Disclosure
The authors report no conflicts of interest in this work.
References
- World Health Organization.World Health Statistics: a snapshot of global health. WHO press 2012; 27(2):1–180 doi:10.2307/3348165
- Chan M. A Global Brief on Hypertension - Silent Killer, Global Public Health Crisis. World health organ. 2013; 1(1):1–40. doi:10.1136/bmj.1.4815.882-a
- NHSDigital. Cardiovascular Disease. NHS website. https://www.nhs.uk/conditions/cardiovascular-disease/. Published 2015. Accessed February 11, 2016.
- NHS Digital. Coronary Heart Disease. NHS website. https://www.nhs.uk/conditions/coronary-heart-disease/. Published 2015. Accessed February 11, 2016.
- Leary SD, Ness AR, Smith GD, et al. Physical activity and blood pressure in childhood: findings from a population-based study. Hypertension. 2008;51(1):92–98. doi:10.1161/HYPERTENSIONAHA.107.09905118071055
- Rosendorff C, Lackland DT, Allison M, et al. Treatment of Hypertension in Patients with Coronary Artery Disease: A Scientific Statement from the American Heart Association, American College of Cardiology, and American Society of Hypertension. J Hypertens. 2015; 65(6):1372–1407. doi:10.1161/HYP.0000000000000018
- Turnbull F. Effects of different blood- pressure- lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet. 2003;362(9395):1527–1535. doi:10.1017/CBO9781107415324.00414615107
- Brown MJ. Science, medicine, and the future. Hypertension. Br Med J. 1997;314(7089):1258–1261. doi:10.1017/CBO9781107415324.0049154032
- Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. J Chem Inf Model. 2003;290(2):199–206. doi:10.1017/CBO9781107415324.004
- Rajpura J, Nayak R. Medication adherence in a sample of elderly suffering from hypertension: evaluating the influence of illness perceptions, treatment beliefs, and illness burden. J Manag Care Pharm. 2014;20(1):58–65. doi:10.18553/jmcp.2014.20.1.5824511766
- National institute for health and clinical excellence guidelines for the clinical management of primary hypertension in adults (update). London Natl Inst Clin Excell. 2011;127:1–94. PMID:22855971.
- Williams B, Poulter NR, Brown MJ, et al. Guidelines for management of hypertension: report of the fourth working party of the British Hypertension Society, 2004 — BHS IV. J Hum Hypertens. 2004;18:139–185. doi:10.1038/sj.jhh.100168314973512
- Pescatello LS, Franklin BA, Fagard R, Farquhar WB, Kelley GA, Ray CA. American College of Sports Medicine position stand. Exercise and hypertension. Med Sci Sports Exerc. 2004;36(3):533–553. doi:10.1017/CBO9781107415324.00415076798
- Whelton PK, Carey RM, Aronow WS, et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. J Am Coll Cardiol. 2017;2017:1–193. doi:10.1016/j.jacc.2017.11.006
- Leung AA, Nerenberg K, Daskalopoulou SS, et al. Hypertension Canada’s 2016 Canadian Hypertension Education Program Guidelines for Blood pressure measurement, diagnosis, assessment of risk, prevention, and treatment of hypertension. Can J Cardiol. 2016;32(5):569–588. doi:10.1016/j.cjca.2016.02.06627118291
- Mancia G, Fagard R, Narkiewicz K, et al. ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013;34(28):2159–2219. doi:10.1093/eurheartj/eht15123771844
- Weber MA, Schiffrin EL, White WB, et al. Clinical practice guidelines for the management of hypertension in the community a statement by the American Society of Hypertension and the International Society of Hypertension. J Clin Hypertens. 2014;16(1):14–26. doi:10.1111/jch.12237
- Pescatello LS, MacDonald HV, Lamberti L, Johnson BT. Exercise for hypertension: a prescription update integrating existing recommendations with emerging research. Curr Hypertens Rep. 2015;17(87):1–10. doi:10.1007/s11906-015-0600-y
- Inder JD, Carlson DJ, Dieberg G, Mcfarlane JR, Hess NCL, Smart NA. Isometric exercise training for blood pressure management: a systematic review and meta-analysis to optimize benefit. Hypertens Res. 2016;39(2):89–94. doi:10.1038/hr.2015.111
- Carlson DJ, Inder J, Palanisamy SKA, McFarlane JR, Dieberg G, Smart NA. The efficacy of isometric resistance training utilizing handgrip exercise for blood pressure management: a randomized trial. Medicine (Baltimore). 2016;95(52):e5791. doi:10.1097/MD.000000000000579128033302
- Baross AW, Hodgson DA, Padfield SL, Swaine IL. Reductions in resting blood pressure in young adults when isometric exercise is performed whilst walking. J Sports Med. 2017;2017:1–6. doi:10.1155/2017/7123834
- Garg R, Malhotra V, Kumar A, Dhar U, Tripathi Y. Effect of isometric handgrip exercise training on resting blood pressure in normal healthy adults. J Clin Diagnostic Res. 2014;8(9):BC08–BC10. doi:10.7860/JCDR/2014/8908.4850
- Taylor AC, McCartney N, Kamath MV, Wiley RL. Isometric training lowers resting blood pressure and modulates autonomic control. Med Sci Sports Exerc. 2003;35(2):251–256. doi:10.1249/01.MSS.0000048725.15026.B512569213
- Wiley RL, Dunn CL, Cox RH, Hueppchen NA, Scott MS. Isometric exercise training lowers resting blood pressure. Med Sci Sports Exerc. 1992;24(7):749–754.1501558
- Stiller-Moldovan C, Kenno K, McGowan CL. Effects of isometric handgrip training on blood pressure (resting and 24 h ambulatory) and heart rate variability in medicated hypertensive patients. Blood Press Monit. 2012;17(2):55–61. doi:10.1097/MBP.0b013e32835136fa22322195
- Ray CA, Carrasco DI. Isometric handgrip training reduces arterial pressure at rest without changes in sympathetic nerve activity. Am J Physiol Hear Circ Physiol. 2000;279:245–249. doi:10.1152/ajpheart.2000.279.1.H245
- Badrov MB, Bartol CL, Dibartolomeo MA, Millar PJ, McNevin NH, McGowan CL. Effects of isometric handgrip training dose on resting blood pressure and resistance vessel endothelial function in normotensive women. Eur J Appl Physiol. 2013;113(8):2091–2100. doi:10.1007/s00421-013-2644-523588257
- McGowan CL, Proctor DN, Swaine IL, Brook RD, Jackson EA, Levy PD. Isometric handgrip as an adjunct for blood pressure control: a primer for clinicians. Curr Hypertens Rep. 2017;19(51):1–8. doi:10.1007/s11906-017-0748-828083801
- Devereux GR, Wiles JD, Swaine IL. Reductions in resting blood pressure after 4 weeks of isometric exercise training. Eur J Appl Physiol. 2010;109(4):601–606. doi:10.1007/s00421-010-1394-x20186425
- Wiles JD, Goldring N, Coleman D. Home-based isometric exercise training induced reductions resting blood pressure. Eur J Appl Physiol. 2017;117(1):83–93. doi:10.1007/s00421-016-3501-027853886
- Devereux GR, Wiles JD, Howden R. Immediate post-isometric exercise cardiovascular responses are associated with training-induced resting systolic blood pressure reductions. Eur J Appl Physiol. 2015;115(2):327–333. doi:10.1007/s00421-014-3021-825308878
- Taylor K, Wiles J, Coleman D, Leeson P, Sharma R, O’Driscoll J. Neurohumoral and ambulatory haemodynamic adaptations following isometric exercise training in unmedicated hypertensive patients. J Hypertens. 2018; Epub ahead of print. doi:10.1097/HJH.0000000000001922.Epub
- Gill KF, Arthur ST, Swaine I, et al. Intensity-dependent reductions in resting blood pressure following short-term isometric exercise training. J Sports Sci. 2015;33(6):616–621. doi:10.1080/02640414.2014.95397925277169
- Wiles JD, Coleman DA, Swaine IL. The effects of performing isometric training at two exercise intensities in healthy young males. Eur J Appl Physiol. 2010;108(3):419–428. doi:10.1007/s00421-009-1025-619280213
- Baross AW, Wiles JD, Swaine IL. Double-leg isometric exercise training in older men. Open Access J Sport Med. 2013;4:33–40. doi:10.2147/OAJSM.S39375
- Bentley DC, Thomas S. Maximal Intermittent Handgrip Strategy : Design and Evaluation of an Exercise Protocol and a Grip Tool. Clin Interv Aging. 2016;11(1):589–601.
- Carlson DJ, Dieberg G, Hess NC, Millar PJ, Smart NA. Isometric exercise training for blood pressure management: a systematic review and meta-analysis. Mayo Clin Proc. 2014;89(3):327–334. doi:10.1016/j.mayocp.2013.10.03024582191
- Owen A, Wiles J, Swaine I. Effect of isometric exercise on resting blood pressure: a meta analysis. J Hum Hypertens. 2010;24(12):796–800. doi:10.1038/jhh.2010.1320182455
- Somani Y, Baross A, Levy P, et al. Reductions in ambulatory blood pressure in young normotensive men and women after isometric resistance training and its relationship with cardiovascular reactivity. Blood Press Monit. 2017;22(1):1–7. doi:10.1097/MBP.000000000000022227824678
- Millar PJ, Bray SR, McGowan CL, MacDonald MJ, McCartney N. Effects of isometric handgrip training among people medicated for hypertension: a multilevel analysis. Blood Press Monit. 2007;12(5):307–314. doi:10.1097/MBP.0b013e3282cb05db17890969
- Millar PJ, Bray SR, MacDonald MJ, McCartney N. The hypotensive effects of isometric handgrip training using an inexpensive spring handgrip training device. J Cardiopulm Rehabil Prev. 2008;28(3):203–207. doi:10.1097/01.HCR.0000320073.66223.a718496321
- Millar P, Paashuis A, McCartney N. Isometric handgrip effects on hypertension. Curr Hypertens Rev. 2009;5(1):54–60. doi:10.2174/157340209787314351
- Bentley DC, Nguyen CH, Thomas SG. Resting blood pressure reductions following handgrip exercise training and the impact of age and sex: a systematic review and narrative synthesis. Syst Rev 2018;7(29):1–17.
- Baross AW, Wiles JD, Swaine IL. Effects of the intensity of leg isometric training on the vasculature of trained and untrained limbs and resting blood pressure in middle-aged men. Int J Vasc Med. 2012;1–8. doi:10.1155/2012/964697
- Cornelissen VA, Smart NA. Exercise training for blood pressure: a systematic review and meta-analysis. J Am Heart Assoc. 2013;1–68. doi:10.1161/JAHA.112.004473
- Perri MG, Anton SD, Durning PE, et al. Adherence to exercise prescriptions : effects of prescribing moderate versus higher levels of intensity and frequency. Heal Psychol. 2002;21(5):452–458. doi:10.1037//0278-6133.21.5.452
- King AC, Castro C, Wilcox S, Eyler AA, Sallis JF, Brownson RC. Personal and environmental factors associated with physical inactivity among different racial-ethnic groups of U.S. middle-aged and older-aged women. Heal Psychol. 2000;19(4):354–364. doi:10.1037/AB78
- Barbour KA, Miller NH. Adherence to exercise training in heart failure : a review. Hear Fail Rev. 2008;13:81–89. doi:10.1007/s10741-007-9054-x
- Van Assche T, Buys R, De Jaeger M, Coeckelberghs E, Cornelissen V. One single bout of low intensity isometric handgrip exercise reduces blood pressure during daily activities in healthy pre- and hypertensive individuals. J Sports Med Phys Fitness. 2017;57(4):469–475. doi:10.23736/S0022-4707.16.06239-327029960
- Vischer AS, Burkard T. Principles of blood pressure measurement – current techniques, office vs ambulatory blood pressure measurement. Adv Exp Med Biol. 2016. doi:10.1007/5584
- Pickering TG, Hall JE, Appel LJ, et al. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans - A statement for professionals from the subcommittee of professional and public education of the American Heart Association Co. Circulation. 2005;111(5):697–716. doi:10.1161/01.CIR.0000154900.76284.F615699287
- Roberts HC, Dnison HJ, Martin HJ, et al. A review of the measurement of grip strength in clinical and epidemiological studies: towards a standardised approach. Age Ageing. 2011;(40):423–429. doi:10.1093/ageing/afr05121624928
- Hopkins WG. Individual responses made easy. J Appl Physiol. 2015;(118):1444–1446. doi:10.1152/japplphysiol.00098.201525678695
- Ray CA, Carrasco DI. Isometric handgrip training reduces arterial pressure at rest without changes in sympathetic nerve activity. Am J Physiol Heart Circ Physiol. 2000;279(1):H245–H249. doi:10.1152/ajpheart.2000.279.1.H24510899063
- Peters PG, Alessio HM, Hagerman AE, Ashton T, Nagy S, Wiley RL. Short-term isometric exercise reduces systolic blood pressure in hypertensive adults: possible role of reactive oxygen species. Int J Cardiol. 2006;110(2):199–205. doi:10.1016/j.ijcard.2005.07.03516239039
- Hess NCL, Carlson DJ, Inder JD, Jesulola E, Mcfarlane JR, Smart NA. Clinically meaningful blood pressure reductions with low intensity isometric handgrip exercise. A randomized trial. Physiol Res. 2016;65(3):461–468. doi:10.1017/CBO9781107415324.00427070747
- Hanik SE, Badrov MB, Stiller-Moldovan C, et al. 084 isometric handgrip training induces equal blood pressure reductions in normotensive males and females without influencing heart rate variability. Can J Cardiol. 2012;28(5):S118–S119. doi:10.1016/j.cjca.2012.07.094
- Bentley DC, Nguyen CH, Thomas SG. Resting blood pressure reductions following isometric handgrip exercise training and the impact of age and sex: protocol for a systematic review. Syst Rev. 2015;4(1):2–7. doi:10.1186/s13643-015-0164-625563983
- Badrov MB, Horton S, Millar PJ, Mcgowan CL. Cardiovascular stress reactivity tasks successfully predict the hypotensive response of isometric handgrip training in hypertensives. Psychophysiology. 2013;50(4):407–414. doi:10.1111/psyp.1203123418955
- Page P. Clinical commentary beyond statistical significance: clinical interpretation of rehabilitation research corresponding author. Int J Sports Phys Ther. 2014;9(5):726–736.25328834
- Brignardello-Petersen R, Carrasco-Labra A, Shah P, Azarpazhooh A. A practitioner’s guide to developing critical appraisal skills: what is the difference between clinical and statistical significance? J Am Dent Assoc. 2014;144(7):780–786. doi:10.14219/jada.archive.2013.0187
- Copay AG, Subach BR, Glassman SD, Polly DW, Schuler TC. Understanding the minimum clinically important difference: a review of concepts and methods. Spine J. 2007;7:541–546. doi:10.1016/j.spinee.2007.01.00817448732
- Stamler J, Rose G, Stamler R, Elliott P, Dyer A, Marmot M. Special feature INTERSALT study findings. Hypertension. 1989;14(5):570–577. doi:10.1161/01.HYP.14.5.5702807518
- Cook NR, Cohen J, Patricia HR, Taylor JO, Hennekens CH. Implications of small reductions in diastolic blood pressure for primary prevention. Arch Intern Med. 1995;155:701–709.7695458
- Stamler J. The INTERSALT study: background, methods, findings, and implications. Am J Clin Nutr. 1997;65:626–642. doi:10.1093/ajcn/65.2.626S
- Badrov M, Bartol C, Millar PJ, McNevin NH. Effects of isometric handgrip training dose on resting blood pressure and resistance vessel endothelial function in normotensive women. Eur J Appl Physiol. 2013;113:2091–2100. doi:10.1007/s00421-013-2644-523588257
- Devereux GR, Wiles JD, Swaine I. Markers of isometric training intensity and reductions in resting blood pressure. J Sports Sci. 2011;29(7):715–724. doi:10.1080/02640414.2011.55211321400346
- Howden R, Lightfoot JT, Brown SJ, Swaine IL. The effects of isometric exercise training on resting blood pressure and orthostatic tolerance in humans. Exp Physiol. 2002;87(4):507–515. doi:10.1111/j.1469-445X.2002.tb00064.x12392115
- Bentley DC, Nguyen CHP, Thomas SG. High-intensity handgrip training lowers blood pressure and increases heart rate complexity among postmenopausal women : a pilot study. Blood press Monit. 2018;23(2):71–78. DOI:10.1097/MBP.0000000000000313
- Zona health. Zona health Inc. Zona Health Inc website.
- Dunne FP, Barry DG, Ferriss JB, Grealy G, Murphy D. Changes in blood pressure during the normal menstrual cycle. ClinicalScience. 1991;81:515–518. doi:10.1089/10799900260100150
- Greenberg G, Imeson JD, Thompson SG, Meade TW. Blood pressure and the menstrual cycle. Br J Obstet Gynaecol. 1985;92(10):1010–1014. doi:10.1111/j.1471-0528.1985.tb02995.x4052342
