Abstract
Objective
Telemedicine-based approaches to health care service delivery improve access to care. It was recognized that adults with inflammatory arthritis (IA) living in remote areas had limited access to patient education and could benefit from the 1-day Prescription for Education (RxEd) program. The program was delivered by extended role practitioners with advanced training in arthritis care. Normally offered at one urban center, RxEd was adapted for videoconference delivery through two educator development workshops that addressed telemedicine and adult education best practices. This study explores the feasibility of and participant satisfaction with telemedicine delivery of the RxEd program in remote communities.
Materials and methods
Participants included adults with IA attending the RxEd program at one of six rural sites. They completed post-course program evaluations and follow-up interviews. Educators provided post-course feedback to identify program improvements that were later implemented.
Results
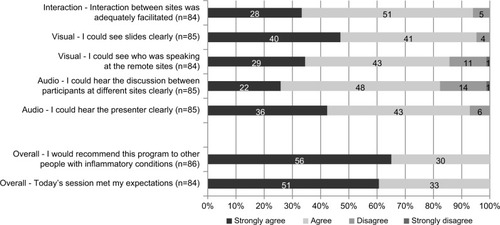
In total, 123 people (36 in-person and 87 remote, across 6 sites) participated, attending one of three RxEd sessions. Remote participants were satisfied with the quality of the video-conference (% agree/strongly agree): could hear the presenter (92.9%) and discussion between sites (82.4%); could see who was speaking at other remote sites (85.7%); could see the slides (95.3%); and interaction between sites adequately facilitated (94.0%). Educator and participant feedback were consistent. Suggested improvements included: use of two screens (speaker and slides); frontal camera angles; equal interaction with remote sites; and slide modifications to improve the readability on screen. Interview data included similar constructive feedback but highlighted the educational and social benefits of the program, which participants noted would have been inaccessible if not offered via telemedicine.
Conclusion
Study findings confirm the feasibility of delivering the RxEd program to remote communities by using telemedicine. Future research with a focus on the sustainability of this and other models of technology-supported patient education for adults with IA across Ontario is warranted.
Introduction
Inflammatory arthritis (IA) is a growing burden in Canada.Citation1 It is estimated to affect more than 1 millionCitation2 of the 36 million Canadians.Citation3 The number of individuals with rheumatoid arthritis (RA), the most common inflammatory condition, has well surpassed the capacity of rheumatologists in Ontario to effectively care for these patients.Citation4 Although new models of arthritis care continue to advance in rural areas,Citation5,Citation6 adults with IA still represent a significantly undertreated and growing population.Citation1,Citation5 Patient education is well recognized as an essential component of specialized arthritis care models.Citation1,Citation7–Citation10 However, access to care, and importantly, to patient education is lacking in remote areas in Ontario.
Arthritis patient education can take many forms and, depending on the program, is associated with improvements in disease knowledge,Citation11–Citation17 disease self-management,Citation18,Citation19 and coping ability.Citation20–Citation24 These outcomes are known to reduce health care utilization and costs to the health care system and, importantly, improve quality of life for people living with chronic disease.Citation18,Citation19,Citation25 However, there remains a gap between the education required to successfully manage a chronic condition and the education that primary care practitioners, and even physician specialists, can provide in treatment-focused care. The targeted education that is available to patients in larger urban centers is often inaccessible to those living in rural Ontario.
Offering an education program, such as the “Prescription for Education” (RxEd) program, to individuals with IA, in their communities, is one way to address this gap. The effectiveness of the RxEd program was validated in 2011.Citation26 A pilot, wait-listed controlled study demonstrated that a 1-day IA education program delivered by an interprofessional arthritis care team was feasible and improved arthritis self-efficacy and other secondary outcomes in people with arthritis. This was apparent in people with different stages of the disease and with disease duration ranging from newly diagnosed to 48 years. The program was expanded to include telemedicine delivery when Advanced Clinician Practitioner in Arthritis Care (ACPAC)-trained clinicians working in rural and suburban areas across Ontario recognized the potential benefits of the RxEd program for people with IA in their communities. Delivering program content via telemedicine technology (videoconferencing) is an accessible, learner-centered approach to education that supports disease self-management.
A number of studies have explored the use of telemedicine for patient education and self-management among individuals with chronic diseases. They have determined that telemedicine is indeed a feasible method of delivery. Jaglal et alCitation27 evaluated the delivery of a 6-week chronic disease self-management program, comparing two telemedicine formats, point-to-point videoconferencing and multipoint conference design. This study concluded that the self-management program could be successfully delivered by using telemedicine and showed that outcomes were similar across the two groups (improved self-efficacy, positive health behaviors, and health status). Another group explored the feasibility and efficacy of a telehealth stroke self-management program for rural participants and found this program to be well received by all participants and was associated with improvement in patient outcomes, compared to a wait-listed control group.Citation28,Citation29 In addition, several studies have explored the feasibility and effectiveness of using a variety of telemedicine technologies for diabetes education.Citation30–Citation33 These studies reported improvements in clinical outcomes, and they report assisting patients with the management of their disease. However, only a few have directly compared telemedicine to in-person delivery. As with our prospective study comparing the effectiveness of telemedicine and in-person delivery of RxEd,Citation34 they found similar trends in outcomes over time when comparing different modes of delivery.Citation27,Citation29
This project sets out to achieve two objectives: first, to understand the feasibility of using videoconferencing to deliver the RxEd program, reported herein, and second, to compare telemedicine delivery of RxEd with face-to-face (in-person) delivery. In a separate publication,Citation34 we report on the two modes of delivery in terms of patient outcomes including arthritis self-efficacy, arthritis knowledge, coping efficacy, illness intrusiveness, and effective consumer.
The purpose of the present study was to explore the feasibility of and participant satisfaction with telemedicine delivery of the RxEd program by triangulating quantitative and qualitative feedback from RxEd participants at remote sites with input from the ACPAC-trained educators and facilitators.
Materials and methods
The RxEd program
The RxEd program, a 1-day education session for adults with IA, was developed in response to a recognized gap in arthritis care. Patients’ knowledge of their disease, and in turn, their ability to manage it, was lacking. The RxEd curriculum was developed in collaboration with arthritis care professionals, a person with arthritis, and an adult learning specialistCitation26 and based on the results of a patient-centred needs assessment.
The content of the program focuses on helping participants better understand their arthritis and manage the pain and other challenges associated with this chronic disease. The session is delivered by an interprofessional arthritis care team and includes short presentations, panel discussions, time for questions and answers, and interactive small group, facilitator-led activities. Each remote site has a local extended role practitioner (trained through the ACPAC program)Citation35 who provides in-person facilitation.
Telemedicine delivery of RxEd
In order to adapt the RxEd Program for telemedicine delivery, two professional development workshops were offered to both the interprofessional educators in Toronto and the facilitators at the remote sites. The workshops focused on videoconferencing fundamentals and the use of videoconferencing specifically for patient education. They incorporated videoconferencing technology, linking various sites, and simulated the RxEd learning experience. Emphasis was placed on the importance of applying sound patient education and adult learning principles in this unique virtual environment. The workshops demonstrated that technology can be manipulated to optimize the sense of social presence by using set camera positions and multiple microphones. Guidelines for slide presentations were also shared. Most importantly, the workshop modeled effective teaching strategies to actively engage remote participants.
The RxEd program was delivered to learners in Toronto (in-person) and via videoconferencing technology to participants at six remote sites, including Thunder Bay, Sault Ste. Marie, Sudbury, Timmins, Orangeville, and Brampton. Didactic presentations, as well as the panel discussions, were transmitted to the remote sites. One local ACPAC-trained physiotherapist or occupational therapist led small group activities at each site, answered participants’ questions, managed the videoconferencing technology, and facilitated participants’ interactions with the other sites.
Recruitment
Participants included RxEd program attendees (patients), as well as the RxEd program faculty (this included the educators delivering the content at the in-person site and the local facilitators at each of the remote sites).
Patients were recruited from arthritis care clinics at an urban teaching hospital (in-person site), as well as through six ACPAC extended role practitioners working across six rural and remote Ontario communities (remote sites). Program attendees who were eligible to participate included adults (aged ≥18 years) with IA attending one of three full-day RxEd education sessions held in the fall of 2012, spring of 2013, or fall of 2013. Attendees had to have been diagnosed, by a clinician, with one of the following IA-related disorders: RA, psoriatic arthritis (PsA), systemic lupus erythematosus (SLE), inflammatory bowel disease (IBD), or gout. Participants at remote sites who consented to be contacted for follow-up research were invited to participate in the qualitative interviews. Attendees who could not complete the survey or interview in English were excluded.
All RxEd program attendees were invited to participate in the program evaluation. They each received a study introduction package, including evaluation forms prior to the beginning of the 1-day session. Following the RxEd session, attendees were asked to indicate, in writing, their willingness to be contacted for the purposes of follow-up research. Approximately 1 week after the session, a research coordinator called those individuals who agreed to be contacted over the phone. Attendees were provided with details of the research study and asked whether they were willing to participate. If they agreed, they were mailed a study consent form for review. About 1 week after mailing the consent form, the research coordinator called the attendee to answer any questions and, if appropriate, obtain consent to participate. The research coordinator obtained verbal consent using a structured, approved consent checklist. This study received ethics approval from St. Michael’s Hospital Research Ethics Board.
Immediate post-program participant feedback
RxEd attendees completed a paper-based program evaluation immediately following their education session. Following each session, local facilitators returned participants’ anonymous evaluation forms to the research coordinator by secure courier. The evaluation included demographic information including age, sex, education, living situation, as well as diagnosis, disease duration, disease activity, and disability.
Disease activity was measured by using the rapid assessment of disease activity index,Citation36 and an abbreviated, eight-item, version of the Health Assessment Questionnaire (HAQ-8) was used to measure disability.Citation37,Citation38
The evaluation included 16 items rated on a 4-point scale (ie, strongly agree, agree, disagree, and strongly disagree). Items addressed participants’ overall impressions and more specifically their perceptions of the quality of the videoconferencing, presentations, and facilities as well as an open-ended space for comments. Because the present study was focusing on the feasibility of telemedicine delivery of RxEd, it reports on participants’ overall impressions (whether or not the session met expectations; willingness to recommend the program to someone else with IA) and their views on the quality of the videoconferencing (ability to hear the presenter, ability to hear participants at other sites, ability to see who was speaking at the remote sites, ability to see the presentation slides, and adequate facilitation of interaction between sites).
Post-program faculty (educator/facilitator) feedback
Following each session, faculty were asked to complete a 2-page feedback form (). The form included open-ended comment boxes addressing 1) the quality of the videoconference including audio, visual, and other technical considerations; 2) the quality of interaction between sites; 3) the small group learning activities including timing, task completion, and group dynamics; and 4) any other feedback. Feedback was discussed at a debriefing meeting, and action items were compiled and implemented in the following session(s) in keeping with quality improvement methodology.Citation39
Table 1 Feedback form content: Prescription for Education (RxEd) telemedicine post-session reflection sheet for faculty
Follow-up participant interviews
Semi-structured interviews were conducted over the phone by the research coordinator and digitally audio-recorded for verbatim transcription. Two members of the research team independently coded the transcripts and conducted a thematic analysis. The interviews were based on a topic guide addressing two main issues: 1) the usefulness of the RxEd program (participants’ expectations of the program, whether their expectations were met, usefulness of the information provided, and perceived benefits of the program), and 2) the quality of the videoconferencing (ability to see and hear the presenters, ability to hear the discussion between sites, and usefulness of the interaction between sites).
Results
In order to examine the feasibility of delivering RxEd via telemedicine, the present study reports primarily on the characteristics and perceptions of those participating remotely. lists the characteristics of in-person participants for comparison.
Table 2 Characteristics of participants by group
Immediate post-program participant feedback
In total, 123 program attendees participated in one of three sessions delivered over six sites. Eighty-two percent (36 in-person and 87 remote) completed the post-program evaluation. There were no significant differences between groups in age, sex, diagnosis, disease activity, disease duration, or disability (). On average, remote participants were 58.6 years old (standard deviation [SD]=13.3), and most were female (n=76; 87.4%), had a postsecondary education (n=45, 52.3%), and lived with at least one other person (n=67; 78.8%). The majority of these participants had been diagnosed with RA (n=60, 85.7%), either on its own or in conjunction with PsA, SLE, or IBD. Disease duration varied with a mean of 7.9 years (SD=11.2). Mean disease activity was 4.7 (SD=1.8) and HAQ score 0.6 (SD=0.4), indicating little disability.
The vast majority of participants reported (% who agreed or strongly agreed) that they could hear the presenter (n=79, 92.9%) as well as the discussion between sites (n=70, 82.4%). Most could see who was speaking at the other remote sites (n=72, 85.7%), and they could see the presenters’ slides (n=81, 95.3%). Most felt that interaction between sites was adequately facilitated (n=79, 94.0%). Overall, 100% of respondents reported that the session met their expectations and, similarly, that they would recommend the program to other people with IA ().
Post-program faculty (educator/facilitator) feedback
Between four and ten educators/facilitators submitted reflective feedback after the three RxEd sessions. Depending on their availability, a subset of the educators, facilitators, and the research team participated in each of the three debriefing meetings.
Educator and facilitator feedback validated the program evaluation data. Feedback suggested that having local facilitators to manage the videoconference technology was essential and that the overall coordination of the program content, technology, and flow of the day were very important and well managed. Facilitators noted that, for the most part, they and the attendees could see and hear the presenters well. They noted some challenges hearing comments from other sites and, as such, acknowledged the importance of the educators repeating questions posed at other sites. Facilitators also requested that educators “treat the video camera as if it’s a person,” to encourage eye contact with the camera and therefore the remote participants. Some facilitators even took the opportunity to share their appreciation for being involved; they noted the psychological benefits of the program to remote attendees thanks to participant interaction, the expert content, and having their questions and fears addressed.
Follow-up participant interviews
Six participants from across the remote sites completed follow-up interviews. Demographics are not reported due to the small sample size. The six semi-structured interviews were conducted between 2 and 6 weeks after participants had attended the RxEd program. Interviews ranged in length from 5 to 15 min.
Remote participants reflected on the value of the program, delivery via videoconference, and the impact or potential impact of RxEd. They noted that the program goes beyond the education that physicians and individual health care professionals can offer in a clinical setting:
… when it comes to arthritis [my doctor is] pretty vague … I knew absolutely nothing about what to expect
…… [the program] was very content-rich … Having the different experts talk about their perspective and their ability to input on treatment was quite useful in understanding … It’s an issue that has to be looked at from many perspectives …
Remote participants note that the program is a good starting point and may be particularly valuable for those newly diagnosed:
… I’ve had arthritis for 10 years and I would have loved to have participated in this at the beginning. I went through a lot and this would have really helped me …
Specific to the videoconference delivery of the program, remote participants noted that they would not have attended if the session was not offered in their community:
… I would have found it difficult to get [to Toronto]. I would have had to not attend just because of the drive … The fact that it was available in the outlying areas … was excellent for us and we so appreciate having the opportunity to participate …
The small group setting and on-site facilitators supported learning:
… You probably could have sat at home and watched it on your computer. But I don’t think it would have had the same opportunity for reinforcement, either by the facilitator or by the other people in the group
…… you felt connected with your little group … [That] removed some of the isolation …
And while some participants felt included:
… I think that it was good that they allowed all the viewers to ask questions and provide feedback if they wanted to. It wasn’t like you just sat and watched people. You were encouraged to participate … I thought that was helpful …
Others would have liked to see more discussion and interaction between the remote sites:
… we had to cover so much information in such a short time that I didn’t feel like there was much of a time for … discussion …
Overall, participants reported that the facilitators were very competent with the technology:
… [The facilitator was] so encouraging for everybody and very comfortable with operating the equipment. There were no issues there
…… [The facilitator] at our end … was excellent … Everything [was] organized and running smoothly … There [were] no hang ups at all …
The immediate and short-term impacts of the program were evident. Participants benefited from the peer interaction:
… I think it’s always very positive to be with other people that have arthritis, in the same room … you see different ages, you see people that don’t look like they have arthritis
… and it’s kind of interesting to hear … what they’ve gone through. It’s very satisfying to have that experience …
… the greatest value I got out of it was being there with people who were further down the path than I was who were saying ‘it’s going to get better’ …
The knowledge they gained positively impacted how they felt about their disease and its treatment:
… I came away feeling better about my meds and understanding why I’m taking what I’m taking and not feeling devastated … And understanding how important the inflammatory drugs are to me …
And some had made decisions about their care:
… I actually went there because I really needed to know more about this medication they were putting me on. I was really scared to go on it. After listening to all these things they had to say, I decided I would try it …
Discussion
Patient education empowers individuals living with arthritis, as it helps them understand their chronic disease, and also offers strategies to self-manage their symptomsCitation1,Citation7–Citation10 Unfortunately, there are many barriers, including distance and a lack of qualified health care human resources, which prevent patients from accessing appropriate, comprehensive education. In the present study, the issue of access was addressed by offering the RxEd program to individuals with IA, in their communities. Delivering the education program, via videoconferencing technology, with the support of specialized arthritis facilitators was feasible, well-received, and as effective as in-person delivery of the content.Citation34 Participants provided rich feedback addressing the technology, the immediate and short-term impacts of the program, and the unanticipated benefits associated with peer interaction and the presence of the facilitators.
Of note, all the respondents reported that they would recommend the program to other people with IA. Educator and facilitator feedback aligned with the strengths and weaknesses of the program and the technology identified by the participants. Program modifications between sessions addressed weaknesses where possible and reinforced the use of a quality improvement approach to meet participants’ needs. Finally, in addition to some constructive feedback about sound quality and remote site inclusion, interview data focused on the value of the program, including the knowledge gained, social support, and the benefits of education, which would have been wholly inaccessible if not offered via telemedicine.
This study had some limitations. First, the number of qualitative interviews was low. Additional participant feedback and more responses from each site would strengthen the conclusions drawn. Another limitation of this work is the potential bias associated with the educator and facilitator feedback. Some of the educators and facilitators are also members of the research team. Finally, the exclusion of individuals who could not provide data in English is also a limitation. The present study recognized that people with chronic conditions who are living in remote areas and whose first language is not English are a highly vulnerable population. They utilize the health care system at a disproportionately high rate and would very likely benefit from accessible, targeted, culturally sensitive patient education. It is hoped that the model of telemedicine delivery that has been used can serve as the foundation for the development of other such arthritis education programs. This is an opportunity for future research.
The strengths of this study include the strong response rate (program evaluation: 82%) and representation from across sites in the qualitative interview data. The present study has three rich sources of data from different stakeholders and time points that allowed for triangulation of study findings. This mixed-methods approach validated previous and early findings and uncovered new information about the impact of the RxEd Program when delivered remotely. Finally, an iterative approach to program improvement grounded in quality improvement methodology was taken. Addressing participant feedback from one session to the next allowed later attendees to benefit from ongoing modifications and encouraged attendees and educators/facilitators to generate new improvement ideas over the course of the three sessions.
The use of videoconferencing for distance education makes the delivery of educational opportunities more accessible to health care professionals living and working in remote areas. Compared to other distance learning modalities – online learning and webinars – videoconferencing is considered the richest media because the technology allows for the conveyance of communication cues (eg, vocal inflection and gestures) and real-time communication.Citation40,Citation41 While videoconferencing has become more commonplace, educators are still challenged to use the medium effectively. As a result, the technology can interfere with the learning experience. The artificiality of videoconferencing technology is often blamed for an unsatisfactory learning experience. However, the way the course is planned, and a lack of knowledge, on the part of the adult educator, about how to engage the remote audience can adversely affect the quality of the virtual educational experience as well.Citation42 Lecture format, in particular, has been shown to leave remote participants feeling excluded from discussions, emotionally isolated, and reluctant to ask questions or to discuss issues.Citation42 The literature suggests that the introduction of a more participatory pedagogy is better suited to this interactive medium.Citation43,Citation44 In the present study, the videoconferencing professional development workshops were an effective intervention that prepared the educators to embrace the media-rich features of the technology. The workshops supported them to integrate participatory education practices in order to ensure that all learners were immersed in the learning experience.
Conclusion
Our study showed that it is feasible to deliver an effective RxEd workshop by using multipoint videoconferencing. Participants and educators saw value in offering RxEd to remote sites using telemedicine. By taking full advantage of the functionality of the videoconferencing medium, the educators were able to encourage active participation and effectively engage learners regardless of their geographical location. The creation of the virtual learning environment made it possible for remote participants to gain new knowledge about their condition from specialized, interprofessional health care providers and, importantly, gave them an opportunity to interact with and learn from their peers.
Future directions
Although the present study demonstrated that it was feasible to use interactive videoconferencing to deliver an effective patient education program, it was acknowledged that facilitation of day-long workshops for targeted communities poses logistical challenges, is costly and time-intensive, and may be exclusionary. As our population ages, the prevalence of chronic diseases, such as IA, is anticipated to increase, as will be the demand for accessible, high-quality patient education. This raises a number of questions related to the reach and sustainability of programs such as RxEd. Future research should further examine: curriculum design (such as shortening the workshop or offering the program as a series of sessions); alternative formats developed as an adjunct (such as web-based learning: eLearning, webcasting); a blended learning approach combining in-person or video-based peer interaction and self-selected, asynchronous, online education as an even more accessible and sustainable option; whether a blended learning approach would achieve similar outcomes; and finally whether tailored, needs-based patient education would improve self-efficacy and health status in this population as in others.Citation45
There are innumerable opportunities for future study. While leveraging the expertise of ACPAC-trained health care providers, the lived experience and recommendations of patients and clinicians in remote areas, and the benefits of ever-advancing technology, RxEd has the potential to benefit a significant number of individuals with IA. Ideally, the RxEd program will continue to grow and adapt, based on patient needs, within a sustainable framework.
The need for patient education among adults with IA will continue to grow. Delivering the RxEd program via telemedicine offers a feasible and effective solution to this growing demand in remote areas across Ontario.
Acknowledgments
This work was supported by CIORA (Canadian Initiative for Outcomes in Rheumatology Care), 2012–2013 funding cycle. The authors thank (time, program delivery, intellectual contribution): St. Michael’s Hospital RxEd team: Dr. Louise Perlin, Angelo Papachristos, Rosaleen Crooks, Caroline Jones, Maureen Riley, Melissa Heidebrecht, Sasha Miles, Donna Scaffidi, Josie Rockman, Catherine Walther, Kevin Curley; Rural/Remote Ontario sites: Jocelyne Murdoch, Mary Ellen Marcon, Tiffany Larsen, Anne MacLeod, Lisa Denning; and St. Michael’s Telemedicine team: Mark Kinach, Rashmi Bhide.
Disclosure
Preliminary findings from this paper were presented at the following meetings as a conference talk:
e-Health 2015: Making Connections, Toronto, Ontario. The presentation is posted at http://www.e-healthconference.com/pastpresentations/2015/201571077557/1931Cflewelling_RxEdTelemed_2015_COACH.pdf?AF=Download&AA=202,1502&AD=DlFile
2nd Annual Sunnybrook Education Conference 2013: Digital Learning, Toronto, Ontario. Abstracts/presentations from this meeting were not published or posted.
e-Health 2013: Accelerating Change, Toronto, Ontario. Abstracts/presentations from this meeting were not published or posted.
Preliminary findings from this paper were presented at the following meetings as a poster presentation:
Canadian Rheumatology Association/Arthritis Health Professions Association Annual Scientific Meeting 2014, Whistler, British Columbia. The poster’s abstract (#72) was posted at https://rheum.ca/images/documents/2014_Poster_Presentations_for_JRheum.pdf
American College of Rheumatology/Association of Rheumatology Health Professionals (ACR/ARHP) Annual Meeting 2013, San Diego, California, USA. The poster’s abstract (#986) was published in the 2013 Annual Meeting Abstract Supplement. Arthritis & Rheumatism, 65: S420 (abstract #986). doi: 10.1002/art.38216. http://www.acrannualmeeting.org/wp-content/uploads/2014/01/2013-ACR_ARHP-Annual-Meeting-Abstract-Supplement.pdf
The authors report no other conflicts of interest in this work.
References
- BombardierCHawkerGMosherDThe impact of arthritis in Canada: today and over the next 30 yearsArthritis alliance of Canada2011 Available from: www.arthritisalliance.ca/images/PDF/eng/…/20111022_2200_impact_of_arthritis.pdfAccessed September 9, 2016
- The Arthritis SocietyFacts and figures2015 Available from: http://arthritis.ca/getmedia/43e83e3e-1a54-4fda-81d5-042ffaf9983f/Arthritis-Facts-Figures-EN.pdfAccessed September 8, 2016
- Statistics CanadaPopulation by sex and age group2016 Available from: http://www.statcan.gc.ca/tables-tableaux/sum-som/l01/cst01/demo31a-eng.htmAccessed October 17, 2016
- WiddifieldJPatersonJMBernatskySThe rising burden of rheumatoid arthritis surpasses rheumatology supply in OntarioCan J Public Health2013104e450e45524495819
- MacKayCVeinotPBadleyEMCharacteristics of evolving models of care for arthritis: a key informant studyBMC Health Serv Res2008814718625070
- GillisKAugrusoACoeTPhysiotherapy extended-role practitioner for individuals with hip and knee arthritis: patient perspectives of a rural/urban partnershipPhysiother Can201466253224719505
- AlbanoMGGiraudet-Le QuintrecJSCrozetCd’IvernoisJFCharacteristics and development of therapeutic patient education in rheumatoid arthritis: analysis of the 2003-2008 literatureJoint Bone Spine20107740541020381401
- CombeBLandeweRLukasCEULAR recommendations for the management of early arthritis: report of a task force of the European Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT)Ann Rheum Dis200766344516396980
- National Institute for Health and Care Excellence (NICE)Rheumatoid arthritis: the management of rheumatoid arthritis in adults2009 Available from: https://www.nice.org.uk/guidance/cg79Accessed September 9, 2016
- ZangiHANdosiMAdamsJEULAR recommendations for patient education for people with inflammatory arthritisAnn Rheum Dis20157495496225735643
- BarlowJHPenningtonDCBishopPEPatient education leaflets for people with rheumatoid arthritis: a controlled studyPsychol Health Med19972221235
- BellMJLinekerSCWilkinsALGoldsmithCHBadleyEMA randomized controlled trial to evaluate the efficacy of community based physical therapy in the treatment of people with rheumatoid arthritisJ Rheumatol1998252312379489812
- BranchVLipskyKNiemanTLipskyPPositive impact of an intervention by arthritis patient educators on knowledge and satisfaction of patients in a rheumatology practiceArthritis Care Res199912375
- HelliwellPSO’HaraMHoldsworthJHesseldenAKingTEvansPA 12-month randomized controlled trial of patient education on radiographic changes and quality of life in early rheumatoid arthritisRheumatology (Oxford)19993830330810378705
- LindrothYBrattstromMBellmanIA problem-based education program for patients with rheumatoid arthritis: evaluation after three and twelve monthsArthritis Care Res1997103253329362599
- LorigKFeigenbaumPReganCUngEChastainRLHolmanHRComparison of lay-taught and professional-taught arthritis self-management coursesJ Rheumatol1986137637673772925
- TaalERiemsmaRPBrusHLMSeydelERRaskerJJWiegmanOGroup education for patients with rheumatoid arthritisPatient Educ Couns1993201771878337194
- LorigDRMazonsonPDHolmanHREvidence suggesting that health education for self-management in patients with chronic arthritis has sustained health benefits while reducing health care costsArthritis Rheum1993364394468457219
- LorigKRLubeckDKrainesRGSeleznickMHolmanHROutcomes of self-help education for patients with arthritisArthritis Rheum198528685
- LeibingEPfingstenMBartmannURuegerUSchuesslerGCognitive-behavioral treatment in unselected rheumatoid arthritis outpatientsClin J Pain199915586610206568
- ParkerJCSmarrKLBuckelewSPEffects of stress management on clinical outcomes in rheumatoid arthritisArthritis Rheum199538180718188849353
- SavelkoulMDe WitteLPVan der BorneBHWVan derTHEffects of a coping intervention on patients with rheumatic diseases: results of a randomized controlled trialArthritis Rheum200145697611308064
- ScholtenCBrodowiczTGraningerWPersistent functional and social benefit 5 years after a multidisciplinary arthritis training programArch Phys Med Rehabil1999801282128710527088
- SharpeLSenskyTTimberlakeNRyanBBrewinCRAllardSA blind, randomized, controlled trial of cognitive-behavioural intervention for patients with recent onset rheumatoid arthritis: preventing psychological and physical morbidityPain20018927528311166484
- BodenheimerTLorigKHolmanHGrumbachKPatient self-management of chronic disease in primary careJAMA20022882469247512435261
- KennedyCABeatonDEWarmingtonKShupakRJonesCHogg-JohnsonSPrescription for education: development, evaluation, and implementation of a successful interprofessional education program for adults with inflammatory arthritisJ Rheumatol2011382247225721765108
- JaglalSBHarounVASalbachNMIncreasing access to chronic disease self-management programs in rural and remote communities using telehealthTelemed J E Health20131946747323570277
- HuijbregtsMPJMcEwenSTaylorDExploring the feasibility and efficacy of a telehealth stroke self-management programme: a pilot studyPhysiother Can20096121022020808482
- TaylorDMCameronJIWalshLExploring the feasibility of videoconference delivery of a self-management program to rural participants with strokeTelemed J E Health20091564665419694589
- IzquierdoREKnudsonPEMeyerSKearnsJPloutz-SnyderRWeinstockRSA comparison of diabetes education administered through telemedicine versus in personDiabetes Care2003261002100712663564
- KearnsJWBowermanDKemmisKIzquierdoREWadeMWeinstockRSGroup diabetes education administered through telemedicine: tools used and lessons learnedTelemed J E Health20121834735322468984
- TimmerbergBDWurstJPattersonJSpauldingRJBelzNEFeasibility of using videoconferencing to provide diabetes education: a pilot studyJ Telemed Telecare200915959719246610
- WestSPLaguaCTriefPMIzquierdoRWeinstockRSGoal setting using telemedicine in rural underserved older adults with diabetes: experiences from the informatics for diabetes education and telemedicine projectTelemed J E Health20101640541620507198
- KennedyCAWarmingtonKFlewellingCA prospective comparison of telemedicine versus in-person delivery of an interprofessional education program for adults with inflammatory arthritisJ Telemed Telecare Published online before print372016
- LundonKShupakRSunstrum-MannLGaletDSchneiderRLeading change in the transformation of arthritis care: development of an inter-professional academic-clinical education training modelHealthc Q2008116268
- FransenJStuckiGvan RielPLCMRheumatoid arthritis measures: Disease Activity Score (DAS), Disease Activity Score-28 (DAS28), Rapid Assessment of Disease Activity in Rheumatology (RADAR), and Rheumatoid Arthritis Disease Activity Index (RADAI)Arthritis Care Res200349S214S224
- FriesJFSpitzPWKrainesRGHolmanHRMeasurement of patient outcome in arthritisArthritis Rheum1980231371457362664
- Stanford School of MedicineResearch instruments developed, adapted or used by the Stanford Patient Education Research CenterPaolo Alto, CAStandford School of Medicine2010 [cited October 14, 2010]. Available from: http://patienteducation.stanford.edu/research/Accessed September 8, 2016
- Health Quality OntarioQuality Improvement Guide2012 Available from: http://www.hqontario.ca/portals/0/documents/qi/qi-quality-improve-guide-2012-en.pdfAccessed September 8, 2016
- DaftRLLengelRHOrganizational information requirements, media richness and structural designManag Sci198632554571
- DennisARKinneySDTesting media richness theory in the new media: the effects of cues, feedback and task equivocalityISR19869256274
- KnipeDLeeMThe quality of teaching and learning via videoconferencingBritish J Educ Technol200233301311
- FritzwYNordkvelleYTComparing lectures: effects of the technological context of the studioEduc and Info Technol20038327343
- SclaterKAlagiakrishnanKSclaterAAn investigation of videoconferenced geriatric medicine grand rounds in AlbertaJ Telemed Telecare20041010410715068647
- NdosiMJohnsonDYoungTEffects of needs-based patient education on self-efficacy and health outcomes in people with rheumatoid arthritis: a multicentre, single blind, randomised controlled trialAnn Rheum Dis2016751126113226162769