Abstract
Fibromyalgia (FM) syndrome is a chronic condition causing pain, affecting approximately 0.5%–6% of the developed countries’ population, and on average, 2% of the worldwide population. Despite the large amount of scientific literature available, the FM etiology is still uncertain. The diagnosis is based on the clinical presentation and the severity of the symptomatology. Several studies pointed out pathological alterations within the central nervous system, suggesting that FM could originate from a central sensitization of the pain processing centers. Research supports the thesis of a peripheral neuropathic component, with the finding of axonal damages. The fibromyalgia patient has many myofascial system abnormalities, such as pain and fatigue, impairing the symptomatic profile. This paper revises the myopathic compensations, highlighting the possible role of the fascia in generating symptoms, being aware of the new information about the fascia’s activity in stimulating inflammation and fat cell production.
Introduction
Fibromyalgia (FM) syndrome is a chronic condition causing pain, affecting approximately 0.5%–6% of the developed countries’ population, and on average, 2% of the worldwide population.Citation1–Citation3 Caucasian and the middle-aged females are at higher risk of FM, as well as those who have family members affected by the disorder.Citation1
FM is characterized by various symptomatological manifestations such as widespread chronic pain (allodynia), hyperalgesia, morning stiffness, altered sensory perception (light, sounds, temperature, touch, smell), sleep disorders, mood disturbances (anxiety and depression), general fatigue, memory loss, irritable bowel, restless leg, migraine, cognitive difficulties, dysmenorrhea, and temporomandibular joint disorder.Citation1–Citation6
Despite the large amount of scientific literature available, FM etiology is still uncertain. The diagnosis is based on the clinical presentation and the severity of the symptomatology.Citation7
In 2010 and 2011, the 1990 American College of Rheumatology established diagnostic criteria for the FM. The scale rating the Symptom Severity (SS) has been added to be used along with the Widespread Pain Index (WPI), while the previous routine manual exam checking the tender points’ presence has been removed.Citation7 According to the American College of Rheumatology, an FM diagnosis is based on these two scales’ scores. A patient must have a WPI ≥7 and an SS score ≥5, or an evaluation of WPI ranging from 3 to 6 and an SS score ≥9.7. The duration of the symptomatology has been estimated to be ≥3 months without a cause justifying the pain.Citation7 Several studies highlighted pathological alterations within the central nervous system, leading to the hypothesis that the FM could originate from a central sensitization of the pain processing centers.Citation8 A thalamocortical dysrhythmia, due to a lower threshold for the action of calcium in the thalamus, could contribute to a constant pain processing in the cortical somatosensory system, leading to the chronicity of the disorder.Citation8 A recent study pointed out an increase in theta oscillations within the prefrontal cortex, which could cause persistent central sensitization.Citation8 Furthermore, another recent research demonstrated a decrease in the cortical presence of dopamine receptors, which are involved in modulating nociceptive perceptions, but further insights are needed in order to make certain assertions about the FM and the dopaminergic role.Citation9 A study with 126 patients affected by FM recently demonstrated the presence, in some subjects, of a functional polymorphic genetic alteration, affecting the frontoparietal control network, which plays an important role in assessing and anticipating the pain sensation.Citation10 Neurosteroids act as modulators of the synaptic transmission, facilitating or inhibiting the GABA-A receptor response, and affecting the perception of pain, mood, and cognition; the serotoninergic tone will act as a weighing needle for the neurosteroid stimulation or inhibition. An increase of neurosteroids is linked to the activation of glial cells, due to a higher concentration in mitochondrial membrane proteins; this happens in the case of chronic psychiatric and pain conditions, highlighting a cerebral inflammatory disease.Citation10 Recent revisions still point fingers at central nervous causes. Other genetic differences (immunomodulator and purinergic, nociceptive and stress mediators, mitochondrial DNA mutation) between healthy subjects and patients affected by FM have been highlighted; the reasons are unknown.Citation11,Citation12 It has been documented that fibromyalgia patients have high level of central glutamate (posterior cingulate gyrus, posterior insula, ventrolateral prefrontal cortex, amygdala), which has an excitatory role on the function of neural cells, lowering the pain threshold.Citation11 Hypotheses have been advanced about vitamin D and its role with the pain’s central modulation: hypovitaminosis findings have been reported, but not in all patients.Citation11 Magnetic resonance studies show alterations in the morphology and activity of some brain areas. Cortical white matter reduction occurs in areas (left side anterior cortex, left lateral orbitofrontal cortex) that are important for the output of the pain modulation mechanisms.Citation12 Gray matter undergoes both a decrease in volume (superior temporal gyrus, thalamus, amygdala, periaqueductal gray, insula, putamen) and an increase in volume (orbitofrontal cortex, cerebellum, basal ganglia, cingulate cortex).Citation12 These alterations are not fully understood. Brain activity seems to be increased especially in cerebellar areas, insula, cortical area, thalamus, and amygdala, probably explaining behavioral alterations related to the pain perception in patients with FM.Citation12 In FM, a peripheral neuropathic component has been noticed. The epidermal nerve fibers’ density is a sign of so-called “small fibrous neuropathy”, a painful neuropathic disorder.Citation13 Reduction in epidermal nerve fiber density can also occur in other conditions, such as in fibromyalgia. The origin could be immune-mediated, and it has been reported in patients affected by FM.Citation13 The hypothesis supporting a peripheral origin of the FM is due to some data pointing to the presence of peripheral polyneuropathy (demyelinating lesions and axonopathy large nerve lesions).Citation13 The spinal cord and brain pathway (that process sensory information) sensitivity is increased by the action of the peripheral system whose afferent nerve fibers detect noxious stimuli (C and A-delta fibers) and movement (mechanoreceptors) in patients with FM. This is probably due to the modulation of the NMDAR which, once activated thanks to the presence of glutamate and glycine, causes the depolarization of the medullary neural cells.Citation14
The presence of peripheral neuropathy and inflammatory elements could decrease the activity-dependent slowing of C-fibers, with a decrease in the latency time to pain, facilitating the medullary mechanism of the summation of the afferential electrical input.Citation15 The decreased activity-dependent slowing compromises the C-fibers activation threshold and their spontaneous activation.
The peripheral neuropathic pain could also be related to the constant activity of the spinal cordial microglia: these are immune cells of the nervous system, releasing proinflammatory substances, whose characteristics are linked to those of the macrophage cells.Citation16 These are highly dynamic and mobile cells (minutes/seconds), characteristics that allow them to be able to repair damaged areas, under constant surveillance of the bone marrow precursor.Citation16 The activation of microglial cells by a nerve’s peripheral damage leads to a bone marrow neuroplasticity with consequent pain hypersensitivity. The damaged peripheral nervous tissue releases CSF1, linking to its glial receptor with a retrograde transport to the marrow. This will activate a membrane protein (DAP12), which will stimulate microglial genes upregulation associated with nociceptive hypersensitivity (Irf8 and Irf5), neuropathic pain, allodynia, and myalgia.Citation16–Citation18 The fibromyalgia patient is characterized by peripheral abnormalities affecting the myofascial system.Citation2,Citation19 It is known that in some chronic conditions, such as congestive heart failure (CHF) and airway obstruction (chronic obstructive pulmonary disease), there is no clear correlation between the clinical presentation and the instrumental evaluation (echocardiography and spirometry, respectively). It is the myopathic chronic adaptation, with the visceral disease as a background, that highly impairs the symptomatology, such as dyspnea, fatigue, and pain.Citation20,Citation21 This paper explains the myopathic adaptations in the fibromyalgia patient, highlighting the possible contribution of the fascia to the fibromyalgia’s symptomatology, being aware of the new information about the fascial role in the production of fat and inflammatory cells.
Myofascial system’s compensation in patients with FM
The fascial tissue is equally distributed throughout the entire body, creating various layers at different depths and forming a three-dimensional metabolic and mechanical matrix. The following four fascial planes can be distinguished: the superficial fascia, the axial/appendicular fascia or myofascia, the meningeal fascia, and the visceral fascia.Citation22 The myofascial continuum, the axial fascia, extends in depth through the body, surrounding the contractile areas, the vessels, and the nerves. This fascia includes the epimysium, perimysium and endomysium, the periosteum, the tissue covering tendons and ligaments, as well as joint capsules.Citation22 Muscle tissue is an integral part of the fascial system (myofascial), having the same embryonic origin.Citation21 DNA fragmentations can be noticed within the muscle fibers, without apoptotic signs or obvious evidence of inflammatory processes.Citation23–Citation27 Type I fibers (slow) are more likely to be lysed and consumed, while atrophy processes frequently occur within the Type II (fast) fibers.Citation23,Citation24,Citation27–Citation30 Anomalous lipid, subsarcolemmal glycogen deposits, and lipofuscin are found within the contractile fibers.Citation23,Citation29,Citation31,Citation32 The latter is considered to be one of the aging pigments, as it is formed by the oxidative degradation, and is known to be inversely proportional to longevity.Citation33 Mitochondrial function is altered along with morphological (wider) and functional changes; aerobic metabolism seems to be deficient in both building up and using energy.Citation23,Citation31 There is a reduction in phosphate production, both under strain and at rest.Citation23,Citation24,Citation34 There is an unbalanced relationship between inorganic phosphorus production and the presence of ATP, indicating one of the possible causes of muscular fatigue.Citation35 In the case of excessive inorganic phosphorus levels, the phosphate binds with calcium favoring an inorganic phosphate precipitation, which in turn prevents the fundamental link with the actin for the muscular contraction to take place, as a result of the cross-bridge cycle.Citation36 There seems to be a greater use of anaerobic muscle metabolism, probably due to a dysregulation of the vasoconstrictive mechanism, along with hypoperfusion occurring within the fibers.Citation27,Citation37 There are vasospasms of the capillary architecture, causing low levels of constant ischemia and low levels of oxygen release to the contractile cell.Citation31,Citation38–Citation40 Often, the endothelial cells are swollen and disorganized, with a greater thickness and a lower permeability.Citation31 The capillary density, ie, the number of capillaries per area and per square millimeter, is decreased as a result.Citation28,Citation41 The blood flow to the muscle cells is reduced, both at rest and in activity.Citation38
This ischemia, though of low magnitude, may relate to the phenomenon of pain and altered nociceptive perception. The vascular hypoperfusion stimulates greater local production of iNOS, an enzyme involved in the synthesis of NO.Citation42,Citation43 In proper dosage, it is essential for muscle regeneration and perfusion, but NO’s abnormal quantities can lead to cellular oxidative stress.Citation43 The oxidative stress, due to an overload of free radicals within the system, damages the structural integrity of the fiber.Citation42 The nociceptive pain perception also occurs as a result of a constant ischemia–reperfusion, related to the activity of ASIC3 that is involved in type III and IV somatosensory afferents (mechanosensitive component), as well as the presence of lactate and protons within the muscles.Citation44,Citation45 Latent ischemia seems to produce an inflammatory systemic response allowing IL-1β cytokine to activate its receptor on III/IV (IL-1r1), thus increasing ASIC3’s expression. This cascade of events, probably through the use of JNK pathway, would modulate myalgic afferent impulse activity, resulting in a lower pain threshold.Citation44 There are alterations in the connective tissue metabolism, although it is not yet possible to find out about the causes.Citation46 According to some studies, a decrease in the density of perimysium and endomysium, along with a build-up of connective tissue on the nerve pathways crossing the muscles, has been hypothesized.Citation47,Citation48 This fascial remodeling could alter the muscles afferent-related response, reducing pain perception.Citation48
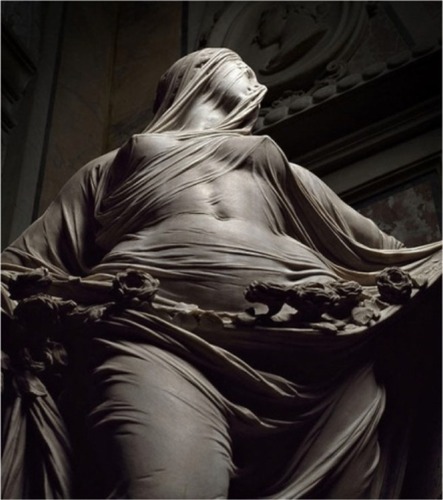
The electrical activity of motor neurons seems to be altered, due to a higher electric conductivity that coordinates the contraction of the muscle.Citation27 As a result, the nerve undergoes morphological remodeling superficially. A less dense lamellar structure is pointed out within the perineurium and endoneurium (fascial tissue), along with functional alterations.Citation49 If the nerve sliding through soft tissues, such as muscles, is impaired because of myofascial stiffness or restriction (eg, in case of remodeling muscle tissue), nervi nervorum are activated, triggering movement-related pain.Citation50 They play a fundamental role in regulating the metabolic nerve background.Citation51 If a nerve runs into an inflamed area, such as muscle fibers, despite the fact that its nociceptors are intact, the axon may get inflamed and more sensitive to mechanical variations, causing pain.Citation51 The fascia is not just about contractile bundles’ subdivision or the attachment to bones, but everything that surrounds the perimysium, thus connecting every part of the body. One needs only to consider the lumbar fascia or the several fascicles favoring the muscles’ tension transmission to the whole body.Citation52 This fascial continuum is crucial for proper motor coordination and the final movement to take place.Citation52,Citation53 Everyday movements of the body are possible thanks to the presence of the fascial tissues and their inseparable interconnection, which allows the sliding of the muscular framework and the sliding of nerves and vessels between/around contractile fields and joints, the same way all the organs can slide and move among each other, influenced by the position of the body (). An alteration of the bodily movements would have a negative influence on neural, peripheral, and central processes, which would induce modifications in the motor patterns.Citation52 An alteration of the function and structure of the lumbar fascia could cause disturbances to the whole back, shoulders, neck, and motor imbalances of the muscular area of the abdomen and thorax.Citation52
Figure 1 Sculpture of veiled woman by Antonio Corradini, 1668–1752.
The fascial changes that have been recorded in several studies are thought to be among the causes of muscular incoordination observed in patients with FM.Citation54–Citation56
Adipocytes and fascia
A lot of scientific evidence has shown an existing link between FM patients and overweight/obesity, with an average of approximately 30% and 40%, respectively.Citation57 Possible causes could be related to sleep disorders, cognitive and behavioral disorders, and/or decreased physical activity. All these reasons do not necessarily concern the total calorie intake or the diet quality.Citation57,Citation58 It has been shown that there is an increase in intramuscular adiposity, probably due to decreased mitochondrial density and function, along with disorders of the hypothalamic–pituitary–adrenal axis.Citation59 Body fat composition seems to influence a higher level of nociceptive factors as well as a low but constant inflammatory status.Citation59 Adipose tissue secretes proinflammatory cytokines, playing a role in generating and perpetuating pain in FM.Citation60,Citation61 Adipose tissue is composed of adipocytes embedded in the loose connective tissue, preadipocytes, and immune cells; it is innervated and vascularized.Citation62 Adipocytes have the ability to secrete different cytokines, including high molecular weight adipokines. The latter stimulate inflammation along with increase in IL-6 levels.Citation62 The hormone leptin, secreted by the adipose tissue, is responsible for weight gain and inflammatory stuatus.Citation62 Adipose tissue also secretes chemokines, being stimulated by an already existing inflammatory process, thus contributing to perpetuation of the event.Citation61 Their function is to manage leukocyte traffic through the interaction with specific seven-transmembrane-spanning G protein-coupled receptors that are involved in development, inflammation and cancer.Citation63
The corticotropin-releasing factor (CRF) is secreted by the central nervous system, released by the hypothalamus’ neurons, with the ability to reach peripheral tissues through the sensory afferent nerve fibers. This neuropeptide binds to the immune cells expressing its receptors (CRF1R and CRF2R) such as macrophages, neutrophils, mast cells, monocytes, and other cell types.Citation64,Citation65 This system is also seen in the adipose tissue where CRF could play a role in the development of a constant but low-level inflammation and contribute to peripheral pain modulation.Citation65 Adipocytes are thought to originate from four tissues: stromal vascular cells, pericytes, adipose tissue endothelial cells, and/or hematopoietic stem cells within the bone marrow.Citation66 Recently, the ability to synthesize adipose tissue starting from the superficial subcutaneous fascial system has been discovered in animals.Citation67 Fascial preadipocytes are unable to be converted into other cell types (myocytes or osteocytes), but they end up differentiating into adipose cells.Citation67 In the rat’s superficial fascial tissue, there is a parallel growth of fat (adipogenesis) and vascular pathways feeding the adipocytes (angiogenesis).Citation67 In the future, many questions will have to be answered. Does the adipose superficial fascia influence the inflammatory status? Can the fascial system as a whole (superficial and deep, somatic, visceral, and meningeal) stimulate adipogenesis and inflammation? Does the fascial adipose tissue influence FM symptomatology?
Conclusion
It is known that there is central sensitization and peripheral neurological alterations with FM. Evidences link fibromyalgia with overweight/obesity, which is associated with greater peripheral pain perception. Recently, in animal models, the adipogenic capacity of the subcutaneous superficial fascia has been uncovered. This paper discussed the possible involvement of the fascial system in this chronic pathology. The fascial system can produce inflammatory substances which could negatively influence the inflammatory environment. New questions are now opening up about the fascial continuum as a whole, whether it is capable of producing adipocytes, and whether this contributes to the painful symptomatology in patients affected by FM.
Disclosure
The authors report no conflicts of interest in this work.
References
- FeinbergTSambamoorthiULillyCInnesKKPotential mediators between fibromyalgia and C-reactive protein: results from a Large U.S. Community SurveyBMC Musculoskelet Disord201718129428687081
- FaveroGTraplettiVBonominiFOral supplementation of melatonin protects against fibromyalgia-related skeletal muscle alterations in reserpine-induced myalgia ratsInt J Mol Sci2017187 pii:E1389
- BäckrydETanumLLindALLarssonAGordhTEvidence of both systemic inflammation and neuroinflammation in fibromyalgia patients, as assessed by a multiplex protein panel applied to the cerebrospinal fluid and to plasmaJ Pain Res20171051552528424559
- KosekEAltawilRKadetoffDEvidence of different mediators of central inflammation in dysfunctional and inflammatory pain--interleukin-8 in fibromyalgia and interleukin-1 β in rheumatoid arthritisJ Neuroimmunol2015280495525773155
- AblinJNeumannLBuskilaDPathogenesis of fibromyalgia – a reviewJoint Bone Spine200875327327918375167
- SayılırSÇulluNDecreased olfactory bulb volumes in patients with fibromyalgia syndromeClin Rheumatol201736122821282428744789
- TaylorAGFischer-WhiteTGAndersonJGStress, Inflammation and pain: a potential role for monocytes in fibromyalgia-related symptom severityStress Health201632550351327925450
- FallonNChiuYNurmikkoTStancakAAltered theta oscillations in resting EEG of fibromyalgia syndrome patientsEur J Pain2018221495728758313
- AlbrechtDSMacKiePJKarekenDADifferential dopamine function in fibromyalgiaBrain Imaging Behav201610382983926497890
- KosekEMartinsenSGerdleBThe translocator protein gene is associated with symptom severity and cerebral pain processing in fibromyalgiaBrain Behav Immun20165821822727448744
- TalottaRBazzichiLDi FrancoMOne year in review 2017: fibromyalgiaClin Exp Rheumatol201735 Suppl 1053612
- SawaddirukPPaiboonworachatSChattipakornNChattipakornSCAlterations of brain activity in fibromyalgia patientsJ Clin Neurosci201738132228087191
- CaroXJWinterEFThe role and importance of small fiber neuropathy in fibromyalgia painCurr Pain Headache Rep201519125526497568
- LittlejohnGGuymerEModulation of NMDA receptor activity in fibromyalgiaBiomedicines20175215
- DickieACMcCormickBLukitoVWilsonKLTorsneyCInflammatory pain reduces c fiber activity-dependent slowing in a sex-dependent manner, amplifying nociceptive input to the spinal cordJ Neurosci201737276488650228576935
- MapplebeckJCBeggsSSalterMWMolecules in pain and sex: a developing storyMol Brain2017101928270169
- GaoYJJiRRChemokines, neuronal-glial interactions, and central processing of neuropathic painPharmacol Ther20101261566820117131
- YasuiMYoshimuraTTakeuchiSA chronic fatigue syndrome model demonstrates mechanical allodynia and muscular hyperalgesia via spinal microglial activationGlia20146291407141724852223
- LiptanGLFascia: a missing link in our understanding of the pathology of fibromyalgiaJ Bodyw Mov Ther201014131220006283
- BordoniBMarelliFMorabitoBSacconiBManual evaluation of the diaphragm muscleInt J Chron Obstruct Pulmon Dis2016111949195627574419
- BordoniBMarelliFThe fascial system and exercise intolerance in patients with chronic heart failure: hypothesis of osteopathic treatmentJ Multidiscip Healthc2015848949426586951
- BordoniBMarelliFMorabitoBSacconiBThe indeterminable resilience of the fascial systemJ Integr Med201715533734328844209
- SprottHSalemiSGayREIncreased DNA fragmentation and ultrastructural changes in fibromyalgic muscle fibresAnn Rheum Dis200463324525114962957
- StaudRRodriguezMEMechanisms of disease: pain in fibromyalgia syndromeNat Clin Pract Rheumatol200622909816932662
- BanicBPetersen-FelixSAndersenOKEvidence for spinal cord hypersensitivity in chronic pain after whiplash injury and in fibromyalgiaPain20041071–271514715383
- FlodgrenGMCrenshawAGAlfredsonHGlutamate and prostaglandin E2 in the trapezius muscle of female subjects with chronic muscle pain and controls determined by microdialysisEur J Pain20059551151516139179
- GerdleBOstlundNGrönlundCRoeleveldKKarlssonJSFiring rate and conduction velocity of single motor units in the trapezius muscle in fibromyalgia patients and healthy controlsJ Electromyogr Kinesiol200818570771617459728
- BengtssonAThe muscle in fibromyalgiaRheumatology (Oxford)200241772172412096218
- PongratzDESpäthMMorphologic aspects of fibromyalgiaZ Rheumatol199857Suppl 2475110025082
- YunusMBKalyan-RamanUPKalyan-RamanKMasiATPathologic changes in muscle in primary fibromyalgia syndromeAm J Med1986813A38423464207
- Le GoffPIs fibromyalgia a muscle disorder?Joint Bone Spine200673323924216488643
- YunusMBKalyan-RamanUPMasiATAldagJCElectron microscopic studies of muscle biopsy in primary fibromyalgia syndrome: a controlled and blinded studyJ Rheumatol1989161971012716012
- NakaeYStowardPJKashiyamaTEarly onset of lipofuscin accumulation in dystrophin-deficient skeletal muscles of DMD patients and mdx miceJ Mol Histol200435548949915571326
- VøllestadNKMengshoelAMRelationships between neuromuscular functioning, disability and pain in fibromyalgiaDisabil Rehabil2005271266767316012059
- SprottHRzannyRReichenbachJRKaiserWAHeinGSteinG31P magnetic resonance spectroscopy in fibromyalgic muscleRheumatology (Oxford)200039101121112511035133
- FittsRHThe cross-bridge cycle and skeletal muscle fatigueJ Appl Physiol (1985)2008104255155818162480
- KatzDLGreeneLAliAFaridiZThe pain of fibromyalgia syndrome is due to muscle hypoperfusion induced by regional vasomotor dysregulationMed Hypotheses200769351752517376601
- ElvinASiösteenAKNilssonAKosekEDecreased muscle blood flow in fibromyalgia patients during standardised muscle exercise: a contrast media enhanced colour Doppler studyEur J Pain200610213714416310717
- MorfSAmann-VestiBForsterAMicrocirculation abnormalities in patients with fibromyalgia – measured by capillary microscopy and laser fluxmetryArthritis Res Ther200572R209R21615743467
- SrikueaRSymonsTBLongDEAssociation of fibromyalgia with altered skeletal muscle characteristics which may contribute to postexertional fatigue in postmenopausal womenArthritis Rheum201365251952823124535
- LindhMJohanssonGHedbergMHenningGBGrimbyGMuscle fiber characteristics, capillaries and enzymes in patients with fibromyalgia and controlsScand J Rheumatol199524134377863276
- KasikciogluEDinlerMBerkerEReduced tolerance of exercise in fibromyalgia may be a consequence of impaired microcirculation initiated by deficient action of nitric oxideMed Hypotheses200666595095216412581
- McIverKLEvansCKrausRMIspasLSciottiVMHicknerRCNO-mediated alterations in skeletal muscle nutritive blood flow and lactate metabolism in fibromyalgiaPain20061201–216116916376018
- RossJLQuemeLFCohenERMuscle IL1β drives ischemic myalgia via ASIC3-mediated sensory neuron sensitizationJ Neurosci201636266857687127358445
- QuemeLFRossJLLuPHudginsRCJankowskiMPDual modulation of nociception and cardiovascular reflexes during peripheral ischemia through P2Y1 receptor-dependent sensitization of muscle afferentsJ Neurosci2016361193026740646
- Ribel-MadsenSChristgauSGronemannSTBartelsEMDanneskiold-SamsøeBBliddalHUrinary markers of altered collagen metabolism in fibromyalgia patientsScand J Rheumatol200736647047718092271
- GronemannSTRibel-MadsenSBartelsEMDanneskiold-SamsoeBBliddalHCollagen and muscle pathology in fibromyalgia patientsRheumatology (Oxford)2004431273112867573
- SprottHMüllerAHeineHCollagen crosslinks in fibromyalgiaArthritis Rheum1997408145014549259425
- Ribel-MadsenSGronemannSTBartelsEMDanneskiold-SamsøeBBliddalHCollagen structure in skin from fibromyalgia patientsInt J Tissue React2005273758216372472
- BordoniBBordoniGReflections on osteopathic fascia treatment in the peripheral nervous systemJ Pain Res2015873574026586962
- BoveGMEpi-perineurial anatomy, innervation, and axonal nociceptive mechanismsJ Bodyw Mov Ther200812318519019083672
- BordoniBZanierEClinical and symptomatological reflections: the fascial systemJ Multidiscip Healthc2014740141125258540
- ChoiHWKimYEEffect of lumbar fasciae on the stability of the lower lumbar spineComput Methods Biomech Biomed Engin201720131431143728836460
- Pérez-de-Heredia-TorresMHuertas-HoyasEMartínez-PiédrolaRBalance deficiencies in women with fibromyalgia assessed using computerised dynamic posturography: a cross-sectional study in SpainBMJ Open201777e016239
- Heredia-JimenezJOrantes-GonzalezESoto-HermosoVMVariability of gait, bilateral coordination, and asymmetry in women with fibromyalgiaGait Posture201645414426979881
- MutoLHSauerJFYuanSLSousaAMangoPCMarquesAPPostural control and balance self-efficacy in women with fibromyalgia: are there differences?Eur J Phys Rehabil Med201551214915424755776
- de AraújoTAMotaMCCrispimCAObesity and sleepiness in women with fibromyalgiaRheumatol Int201535228128725056401
- SlimMCalandreEPGarcia-LeivaJMThe effects of a gluten-free diet versus a hypocaloric diet among patients with fibro-myalgia experiencing gluten sensitivity-like symptoms: a pilot, open-label randomized clinical trialJ Clin Gastroenterol201751650050727548732
- GerdleBForsgrenMFBengtssonADecreased muscle concentrations of ATP and PCR in the quadriceps muscle of fibromyalgia patients – a 31P-MRS studyEur J Pain20131781205121523364928
- SlukaKAClauwDJNeurobiology of fibromyalgia and chronic widespread painNeuroscience201633811412927291641
- IgnacioRMGibbsCRLeeESSonDSDifferential chemokine signature between human preadipocytes and adipocytesImmune Netw201616318919427340388
- PeterlinBLSaccoSBerneckerCScherAIAdipokines and migraine: a systematic reviewHeadache201656462264427012149
- KabirSMLeeESSonDSChemokine network during adipogenesis in 3T3-L1 cells: differential response between growth and proinflammatory factor in preadipocytes vs. adipocytesAdipocyte2014329710624719782
- KempurajDThangavelRSelvakumarGPBrain and peripheral atypical inflammatory mediators potentiate neuroinflammation and neurodegenerationFront Cell Neurosci20171121628790893
- DermitzakiEVenihakiMTsatsaniCThe multi-faceted profile of Corticotropin-Releasing Factor (CRF) family of neuropeptides and of their receptors on the paracrine/local regulation of the inflammatory responseCurr Mol Pharmacol2018111395028103784
- CawthornWPSchellerELMacDougaldOAAdipose tissue stem cells meet preadipocyte commitment: going back to the futureJ Lipid Res201253222724622140268
- SuXLyuYWangWFascia origin of adipose cellsStem Cells20163451407141926867029
